Published online Mar 5, 2025. doi: 10.4292/wjgpt.v16.i1.97918
Revised: October 29, 2024
Accepted: December 10, 2024
Published online: March 5, 2025
Processing time: 263 Days and 18.1 Hours
The exact worldwide prevalence of gastroesophageal reflux disease (GERD) re
Core Tip: Globally, the prevalence of gastroesophageal reflux disease (GERD) and GERD symptoms vary depending from country to country and region to region. Defining GERD and pinpointing its prevalence are problematic due to its diagnostic issues. However, understanding the differences in prevalence will help us identify the differences in associated risk factors, such as genetics and diet, that lead to an individual’s susceptibility to suffering from GERD and its symptoms.
- Citation: Wickramasinghe N, Devanarayana NM. Insight into global burden of gastroesophageal reflux disease: Understanding its reach and impact. World J Gastrointest Pharmacol Ther 2025; 16(1): 97918
- URL: https://www.wjgnet.com/2150-5349/full/v16/i1/97918.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v16.i1.97918
Effortless reflux of gastric contents into the esophagus is a normal physiological process termed gastroesophageal reflux. However, when such reflux occurs frequently and for a prolonged duration, it can lead to symptoms such as heartburn and regurgitation. Gastroesophageal reflux can lead to complications such as esophagitis or strictures. This is termed gastroesophageal reflux disease (GERD)[1,2]. GERD is a multifactorial disease with a complex pathophysiology, usually simplified to a malfunctioning lower esophageal sphincter[3]. It is linked with many genetic and behavioral risk factors such as diet, obesity, mental stress, and medications[4-9]. It is discussed extensively as a common condition[10]. How
GERD gives rise to a wide range of unpleasant symptoms, both gastrointestinal and extraintestinal. The most common symptoms of GERD are listed in Table 1. Of them, heartburn is recognized as the commonest symptom and the strongest indicator of GERD[11,12]. While heartburn is defined in the Montreal consensus as “a burning sensation in the retrosternal area”[13], the interpretation of “heartburn” and its perception vary in each culture, country, and language, as there are no direct translations of the term “heartburn” in many languages[14]. This issue can confound research[15]. Some non-English speaking populations and Asian cultures like Chinese do not have a term equivalent to heartburn, and dyspeptic symptoms can be counted as part of the diagnosis. Heartburn can also be due to several disorders other than GERD, such as heart disease, gallstones, and eosinophilic esophagitis[16-18]. Despite such issues, heartburn is said to have a 78% sensitivity and 60% specificity[19]. The second commonly described symptom is regurgitation[20], which is defined as the “perception of the flow of refluxed gastric content to the mouth or hypopharynx” or can simply be described as the feeling of a sour taste inside the mouth or fluid moving up in the chest[13,20]. This symptom can also be present in other disorders such as achalasia cardia and rumination syndrome[13,21,22].
| Ref. | Symptom |
| [97] | Non cardiac chest pain |
| [11] | Heartburn |
| [20] | Regurgitation |
| [98] | Dysphagia |
| [99] | Globus sensation |
| [13] | Epigastric pain |
| [100] | Dyspepsia |
| [101] | Belching |
| [102] | Gall bladder disease |
| [33] | Nausea |
| [103] | Headache |
| [104] | Disturbance of sleep |
| [13] | Dental erosions |
| [105] | Increased salivation |
| [106] | Temporomandibular dysfunction |
| [107] | Chronic cough |
| [108] | Laryngitis |
| [109] | Asthma |
| [110] | Chronic otitis media |
| [111] | Chronic sinusitis |
| [112,113] | Taste and smell changes |
| [114] | Asymptomatic |
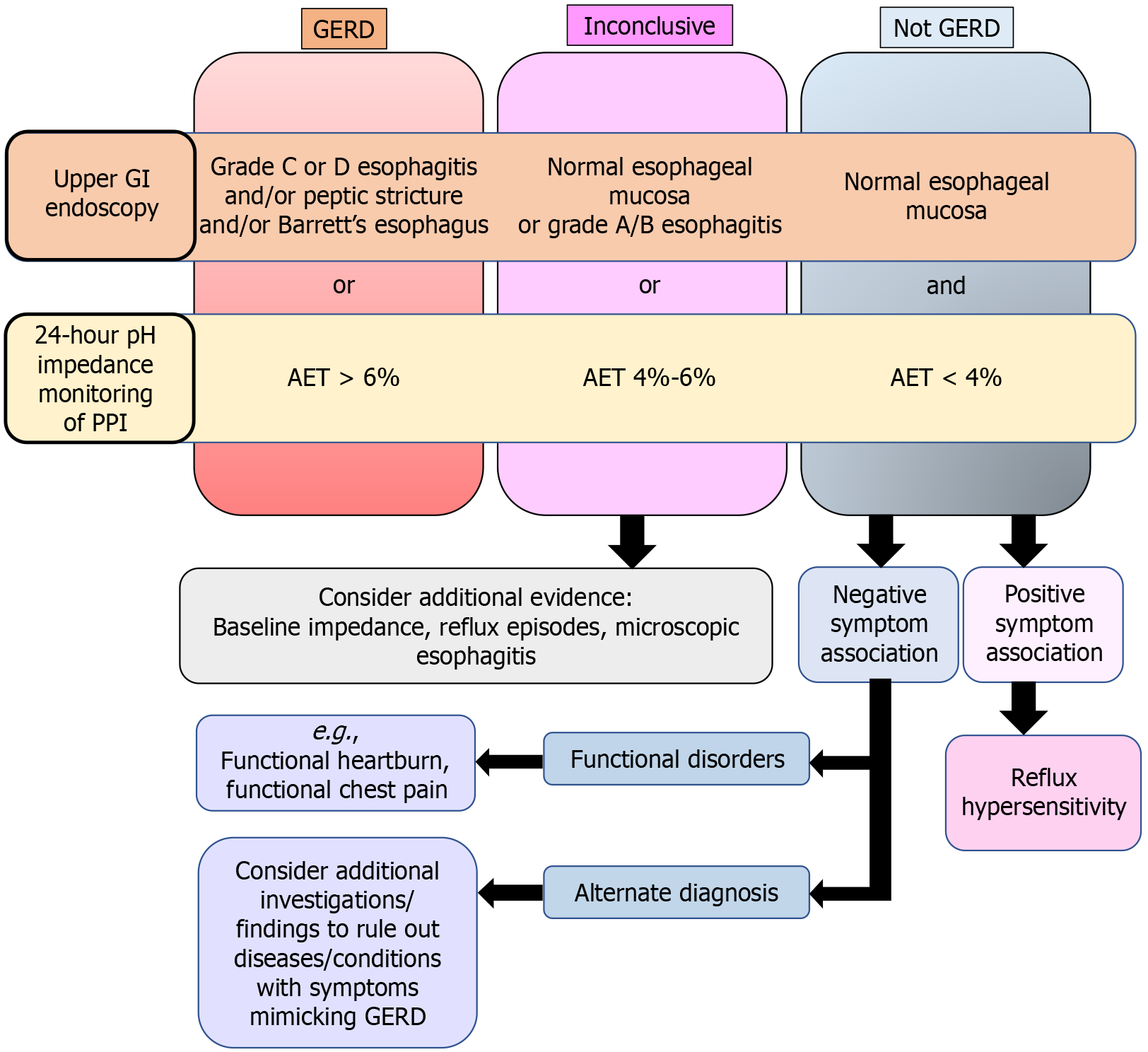
GERD can be classified as erosive reflux disease (ERD) and non-ERD (NERD)[23]. When reflux-induced esophageal inflammation/ulceration is noted on endoscopy, it is diagnosed as esophagitis[23]. Esophagitis is graded based on the Los Angeles classifications A, B, C, and D[24], with only Grades C and D considered ERD (Table 2)[25]. Patients with NERD have no endoscopic changes but still show abnormal acid exposure time (AET) in 24-hour multichannel intra
| Grade | Criteria |
| A | One or more mucosal breaks < 5 mm that do not extend between the tops of two mucosal folds |
| B | One or more mucosal breaks > 5 mm that do not extend between the tops of two mucosal folds |
| C | One or more mucosal breaks that are continuous between the tops of two or more mucosal folds but that involve < 75% of the circumference |
Many diseases can mimic GERD. Some of these conditions are listed in Table 3. Two important differential diagnoses of GERD presenting with symptoms of heartburn and regurgitation are reflux hypersensitivity (RH), where normal physiological refluxes elicit symptoms and functional heartburn (FH), where there is no evidence either on the ambulatory pH monitoring or endoscopy, but the patient still complains of heartburn[27,28]. A further problem is that RH and FH can overlap with GERD, as patients can continue to suffer from symptoms despite improvement of reflux and esophagitis[29].
| Ref. | Diseases with overlapping symptoms |
| [115] | Eosinophilic esophagitis |
| [116] | Infectious esophagitis |
| Esophageal candidiasis | |
| Herpes and cytomegalovirus esophagitis | |
| [117] | Drug-induced esophagitis |
| [118] | Achalasia and esophageal motility disorders |
| [119] | Pharyngeal and esophageal diverticula, rings, and webs |
| [120] | Disorders of gastric motility/ gastroparesis |
| [121] | Gastritis & peptic ulcer disease |
| [122] | Gluten-related disorders |
| [123] | Functional gastrointestinal disorders: Functional chest pain, functional heartburn, reflux hypersensitivity, globus sensation, functional dysphagia, functional dyspepsia, postprandial distress syndrome, epigastric pain syndrome, belching disorders, and rumination syndrome |
| [124] | Functional abdominal bloating/distension and esophageal and gastric carcinoma |
| [125] | Cardiac disease |
| [126] | Gall bladder and pancreatic diseases |
The initial diagnosis of GERD is usually symptom-based but can be confirmed by upper gastrointestinal endoscopy or combined multichannel intraluminal impedance and pH monitoring (MII-pH)[30].
Clinical history plays a large part in the first-time diagnosis of GERD and is also the main tool used in epidemiological studies[13]. Since investigations used to confirm GERD are invasive and uncomfortable, the symptom criteria play a very significant role in the diagnosis of this condition. From the vast array of symptoms, heartburn and/or regurgitation have a somewhat higher sensitivity and specificity for the diagnosis of GERD and are considered “typical” symptoms[13]. However, diagnosing GERD by clinical history alone is inaccurate since some patients with GERD are asymptomatic or have atypical symptoms other than typical symptoms such as heartburn and regurgitation[31,32]. The Diamond Study findings showed that even a history taken by an expert (e.g., a gastroenterologist) has a sensitivity and specificity of just 70% and 67%, respectively, compared with pH impedance testing or endoscopy[33].
The lack of universally recognized criteria to grade the severity of GERD is another major issue in assessing the burden of this condition. Vakil et al[13], in the Montreal classification with 44 content experts, defined patients with GERD as those who have mild symptoms occurring on ≥ 2 days of the week or those having moderate to severe symptoms occur
| Tool or questionnaire | Abbreviation |
| Gastroesophageal reflux disease questionnaire | GerdQ |
| Reflux Disease Questionnaire | RDQ |
| Carlsson-Dent Questionnaire | CDQ |
| Bowel Disease Questionnaire | BDQ |
| Frequency Scale for the Symptoms of GERD | FSSG |
| General Health Questionnaire-28 | GHQ-28 |
| Gastrointestinal Symptom Rating Scale | GSRS |
| Domestic/International Gastroenterology Surveillance Study | DIGEST |
| Subjective Symptom Assessment Profile | SSA-P |
| GERD Symptom and Medication Questionnaire | GERD-SMQ |
| Chest Pain Questionnaire | CPQ |
| Quality of Life and Utility Evaluation Survey Technology | QUEST |
| Infant Gastro-Esophageal Reflux Questionnaire | I-GERQ |
| GERD Activity Index | GRACI |
| Esophageal Symptom Questionnaire | |
| Standardized Esophageal Symptom Questionnaire | |
| Ulcer Esophagitis Subjective Symptoms Scale | UESS |
| GERD Activity Index | GRACI |
| Digestive Health Status Instrument | DHSI |
| Modified Bowel Disease Questionnaire | BDQ |
| GERD Symptom Assessment Scale | GSAS |
| GERD Screener |
One of the most used questionnaires worldwide is the GerdQ[35]. This is utilized worldwide and has been translated into many languages[36]. It questions the frequency of heartburn and regurgitation as well as sleep disturbance and use of medication for those two symptoms for the past week and gives positive marks, while non-cardiac chest pain and nausea give negative points. GERD is diagnosed if the marks are equal or more than 8[36]. One of the eight questions in GerdQ is “How often does a patient use medication for heartburn or reflux other than what the doctor prescribed?” In countries where the prescribing is not streamlined, self-medication is common, and the ability to buy “prescription drugs” over the counter without a doctor’s prescription is rampant, this question might not be relevant. Despite all the criticisms of decreased sensitivity and specificity, diagnosis of GERD based on usual symptoms is practical and affordable, and many international guidelines support it[1].
Endoscopy: Endoscopy can identify erosive esophagitis and its complications[23]. Erosive esophagitis is the most common endoscopic manifestation seen in GERD and is reported in 3%-16% of patients, with most having mild esophagitis[37]. However, most GERD patients do not have visible mucosal lesions. Patients with a negative result on endoscopy are recommended to undergo pH impedance testing to confirm the diagnosis of NERD.
24-hour pH impedance: MII-pH can identify the retrograde bolus movement, number of reflux events, total reflux time, the association between symptoms and reflux episodes, and acidic, weakly acidic, and alkaline refluxes[38]. Thus, it is the most sensitive and specific investigation in diagnosing GERD[38]. It can also differentiate GERD from FH and RH. There are many controversies in using 24-hour pH impedance in diagnosing GERD. The Lyon consensus in 2018 proposed that an AET of less than 4% for 24 hours be considered normal and that those above 6% are definitively abnormal and considered GERD. Those within 4% to 6% are recommended to have an adjunctive measure to prove GERD. The consen
MII-pH also had many regional differences which were further complicated by the different analytic systems and software used in different countries[41]. Cut-offs and normal values for MII-pH are further controversial due to other reasons as well. One is that their values rely on very small cohorts of healthy volunteers from only a few countries[42,43]. Another reason is that there is significant inter-reviewer variability due to technical issues related to analysis such as artifacts and subjective identification of reflux events[44]. Thus, it is problematic that despite all these differences related to different systems and regional differences, the GERD categorization is still related to the Lyon consensus with a fixed cut-off[25]. Furthermore, different systems were used to detect MII-pH metrics, and a significant number of false-positive refluxes in automated analyses of these systems were identified[45,46]. Some experts now recommend lower AET values to diagnose GERD than the Lyon consensus, going as low as 3.2%[47].
High-resolution manometry of the esophagus: High-resolution manometry (HRM) is not a diagnostic test for GERD and most GERD patients have a normal manometric study. However, there can be abnormalities in the LES or the esophageal body that can be detected by HRM[25]. It is recommended in patients with treatment-resistant GERD as it can identify conditions such as achalasia, hiatal hernia, abnormal LES pressures, and esophageal dysmotility that can give rise to GERD symptoms[48]. Manometry also helps identify the exact location of the LES, which helps with the accurate placement of pH sensors[48]. Combined impedance and HRM can also differentiate GERD from rumination[49].
Figure 1 summarizes the currently accepted GERD diagnostic guidelines published by leading authorities in gastroenterology, including the Lyon consensus, Porto consensus, British society, and American College of Gastroenterology guidelines[1,25,50,51].
The global prevalence of GERD remains unclear, despite its frequent mention as a common condition. This uncertainty primarily arises from the absence of a universally accepted definition of GERD. A key issue is that the gold standard for diagnosing GERD, the combined pH impedance testing (MII-pH), is underutilized. This limitation is due to both the invasive nature of the procedure and the limited availability of facilities equipped to perform it. MII-pH as well as endoscopy is cumbersome and cannot be carried out in a practical setup to identify the community prevalence of a country or region. Furthermore, despite endoscopy being more widely utilized than ambulatory pH studies, with its inability to identify NERD[53], it cannot be utilized to identify community prevalence, especially in pediatric age groups. Thus, most of the studies on the epidemiology of GERD used various questionnaires as screening tools to assess the symptoms of GERD. The symptoms of GERD can be both esophageal and extraesophageal with much variation, with also an added component of asymptomatic patients[54].
These account for the wide variety of prevalence estimates presented, ranging from 5% to 25% worldwide[6]. Some systematic reviews by experts have used heartburn and or regurgitation at least once weekly as their cut-off for GERD when going through studies worldwide[55]. The latest comprehensive systematic review and meta-analysis on GERD was conducted by Nirwan et al[34] in 2020. The definition was “having heartburn and/or regurgitation at least once weekly”. However, this does not represent the other multitude of GERD patients who might be asymptomatic or have other symptoms other than heartburn or regurgitation as well as those who fit into other differential diagnoses of GERD such as RH and FH.
The recent systematic review conducted by Nirwan et al[34], reported a global prevalence of 13.98%, using 102 studies. The highest pooled prevalence of GERD is reported in Turkey (22.4%). The lowest GERD prevalence has been reported in China (4.16%). The prevalence of GERD in North America and Europe is 19.55% and 14.12%, respectively[34]. Pooled prevalence was not calculated in some regions such as Asia in this systematic review. Even though several few South Asian studies (from Bangladeshi and India) were cited in this systematic review, the pooled prevalence was not calculated for this region[34]. When the definition of heartburn and/or regurgitation at least once a week was used, the prevalence of GERD in Bangladeshi was 5.25%[56] and in Indian studies it was 7.6%[57] and 23.6%[58], respectively. A recent study from Sri Lanka in 2024[59], using the same definition as that used by Nirwan et al[34], reported a country-wide prevalence of 25.3%, which is higher than that of Turkey, the country with the highest pooled prevalence reported by Nirwan et al[34]. Table 5 shows the data on regional and country GERD prevalences around the world updated with the latest data using the definition used by Nirwan et al[34].
| Geographical location | Number of studies used for calculation by Nirwan et al[34], 2020 | Number of participants | GERD prevalence, % |
| Global | |||
| Overall | 102 | 469899 | 13.98 |
| Male | 50 | 122849 | 15.69 |
| Female | 50 | 138435 | 17.17 |
| Hemisphere | |||
| Western | 10-20[6,55] | ||
| Eastern | 2-7[6,127] | ||
| Continents | |||
| Asia | 54 | 240451 | 12.92 |
| Europe | 29 | 90057 | 14.12 |
| North America | 9 | 20525 | 19.55 |
| Latin America and the Caribbean | 4 | 12756 | 12.88 |
| Oceania | 4 | 3760 | 13.78 |
| Africa | 2 | 2350 | NA |
| Countries | |||
| China | 10 | 36887 | 4.16 |
| Japan | 7 | 27912 | 13.81 |
| South Korea | 7 | 43897 | 5.84 |
| Taiwan | 1 | 1238 | NA |
| Indonesia | 1 | 278 | NA |
| Bangladesh | 1 | 2000 | 5.25[56] |
| India | 3 | 6296 | NA |
| Iran | 16 | 102295 | 18.43 |
| Turkey | 4 | 13332 | 22.4 |
| Israel | 2 | 3008 | NA |
| Saudi Arabia | 2 | 3308 | NA |
| Poland | 1 | 850 | NA |
| Romania | 1 | 184 | NA |
| Russia | 2 | 8877 | NA |
| Albania | 1 | 845 | NA |
| Italy | 2 | 2032 | NA |
| Greece | 1 | 700 | NA |
| Spain | 3 | 5365 | NA |
| Switzerland | 2 | 7736 | NA |
| Netherlands | 1 | 502 | NA |
| France | 2 | 46377 | NA |
| Germany | 1 | 268 | NA |
| Sweden | 4 | 8120 | 16.15 |
| Finland | 1 | 1700 | NA |
| Norway | 1 | 44997 | NA |
| United Kingdom | 4 | 12467 | 14.53 |
| Denmark | 1 | 48027 | NA |
| United States | 8 | 19489 | 21.04 |
| Canada | 1 | 1036 | NA |
| Argentina | 1 | 839 | NA |
| Brazil | 1 | 3934 | NA |
| Uruguay | 1 | 1141 | NA |
| Colombia | 1 | 6842 | NA |
| Australia | 3 | 2982 | 12[62], 9.2[63] |
| New Zealand | 1 | 778 | NA |
| Nigeria | 1 | 410 | NA |
| Côte d’Ivoire | 1 | 1940 | NA |
| Sri Lanka | 1 | 1200 | 23.5[59] |
When one moves away from the definition of GERD as heartburn and/or regurgitation once a week and analyzes the studies done with other questionnaires, the prevalence is even more variable. The Western hemisphere has a higher prevalence of GERD, with prevalence rates of 27.8% in North America, 25.9% in Europe, and 23% in South America given as examples[6,60]. A prevalence of 19.55% was noted in the North American region[34], with at least 30% of the United States population having GERD symptoms at least one time in their life[61]. An Australian study reported a prevalence of GERD symptoms of 12% in their subjects[62], while another estimated it at 9.2%[63]. Studies done in Latin America have shown that GERD prevalence is around 11.9% and 31.3%[64].
GERD was reported traditionally as being less common in Asian countries, with the prevalence ranging around 2% to 7%[6,37,65,66]. But over the last decades, it has been noted to be increasing in Asia, most probably due to the westernization of diets[14,67]. In Eastern Asian countries, the prevalence, which was around 2.5% to 4.8% in 2005 increased to 5.2% and 8.5% in 2010. This rise is seen higher in Southeast and Western Asian countries where in 2010 the prevalence was noted to be around 6.3% to 18.3%[65]. This rise is also noted by many studies done in China where the current estimate is pooled at 4.16%[34,68]. While the above-quoted number is quite small, surprisingly studies done in neighboring Taiwan meanwhile showed a prevalence of around 25%[69]. Far Eastern countries such as China, Japan, and South Korea had a prevalence that was very much lower, while in the Middle Eastern region, the quoted prevalence rates are quite higher[6]. A study done in Saudi Arabia showed the prevalence of GERD at 45.4%[70], while a study done in Iran quoted 43.07% as the percentage of the population having GERD symptoms[71]. The prevalence studies done in India show varying percentages ranging from 10%[72] to 19%[73], and even 22.2% in South India[74].
Except for heartburn or regurgitation, which are the typical GERD symptoms, the others are considered atypical GERD symptoms[13]. We compared various aspects of the symptom profile of studies done around the world using the same GERD definition used by Nirwan et al[34]. The prevalence of symptoms other than heartburn and regurgitation in those with GERD was wide and varied among studies worldwide[75]. For instance, a study from Sri Lanka found that bloating, affecting 55.6% of GERD patients, was the most troublesome symptom after heartburn and regurgitation[59]. This finding contrasts with a Korean study, where only 15.2% of GERD patients reported bloating[76]. In Turkey, dysphagia affected 11.9% of those with GERD[77], whereas a study from China reported a significantly higher dysphagia rate of 35.7% among GERD patients[78].
Even the prevalence of those who suffer from daily heartburn and regurgitation differs from country to country. In a study in Turkey, which has a similar sample size (n = 1345) and a similar GERD prevalence (19.3%) as the study con
Due to the unavailability of conducting endoscopy and pH-impedance testing to diagnose and identify GERD in the general population, the prevalence of confirmed GERD is still not available as of now. The global age-standardized prevalence of GERD in 2017 was calculated to be 8819 cases per 100000 population (95% confidence interval: 7781-9863). This prevalence has been stabled from 1990 to 2017, but with increased prevalence in older age groups and increased years lived with disability[80]. The Global Burden of Diseases Study 2019 calculated that from 1990 to 2019, the total number of prevalent cases and incident cases increased by 77.53% (from 441.57 million in 1990 to 783.95 million in 2019) and 74.79%, respectively[81].
GERD has many associated factors as well as risk factors[5]. These are summarized in Table 6. These factors, especially diet, could be the reason for the wide variations of prevalence in countries worldwide.
| Factor | Evidence |
| Age | With increasing age, the elasticity of the pharyngoesophageal membrane reduces, progressively leading to hiatal hernias, predisposing to GERD[128]; the prevalence of GERD symptoms is highest in those aged 40 to 59 years in the systematic review by Nirwan et al[34] |
| Gender | Females had a slightly higher prevalence of GERD than males in systematic reviews by Nirwan et al[34] and Friedland et al[128] |
| Education level | Those with the lowest education level had the highest GERD prevalence, whilst those with the highest level of education had the lowest GERD prevalence[34,129] |
| Ethnicities | Ethnicities can play a role in development of GERD even in the same country[14], though some studies did not find any significant difference[59] |
| Economic strata | Lower-income groups are reported to have a significantly higher prevalence of GERD[34,128] |
| Urban or rural | GERD is reported to be higher in urban populations[34,74,130] |
| Obesity | Obesity is an identified risk factor for GERD[34,131,132] |
| Mental stress | Mental stress is shown to increase GERD symptoms[9,133] |
| Diet | Common food items associated with GERD are: Spices[10], carbonated beverages[134], wheat products[135], tea[136], coffee[137], sour and acidic food[138], alcohol[78], chocolate[139], dietary sugar[140] |
| Habits | Habits associated with GERD include: Large meals[141], sleeping after eating a meal[142], eating a meal fast[135], habit of midnight snacks[143], skipping meals[143], inadequate sleep[134], exercise[142,144], smoking[145] |
| Diseases and treatments | Some diseases such as asthma[146], diabetes mellitus[147], and different medications[148-151] are known to be associated with GERD symptoms |
The United States is estimated to spend more than 10 billion dollars per year on the diagnosis and treatment of GERD[25], with an estimated number of up to 4663644 annual hospital visits made for GERD and reflux esophagitis just for the year 2016[82]. A mean ± SD of dollars 6955 ± 35880 was estimated to be the annual disease-related cost per patient for GERD in the United States for the year 2020[83]. Another study in the United States noted that a mean incremental cost of 3355 dollars per employee was associated with GERD, with 17% of it accounting for prescription drug costs and 19% for indirect costs[84]. Increasing severity and complications of the GERD spectrum towards dysplasia and carcinoma result in further expenses as well[83]. The average monthly medical costs for proton pump medications were estimated to be approximately 163 dollars in South Korea[85].
GERD affects the quality of life (QoL) of its sufferers. The Global Burden of Diseases Study 2019 has calculated that between the years 1990 and 2019, the estimated years lived in disability has increased by 77.19%[81]. Patients with GERD have lower physical and mental health scores, increased work absenteeism, reduced percent productivity, increased healthcare utilization, and more concomitant diseases. The QoL parameters invariably deteriorate if the severity of GERD increases[86]. Due to its effect on daily life, several QoL questionnaires have been developed alongside screening tools and diagnostic questionnaires[87,88]. Studies using these questionnaires have shown that the QoL of GERD sufferers become worse with increasing age and obesity[89].
GERD leads to many complications such as reflux esophagitis, Barret’s esophagus, and strictures[90,91]. The damage to the esophagus that leads to esophagitis and dysplasia was initially thought to be due to the chemical injury caused by refluxed stomach acid, bile salts, and other erosive and noxious materials in gastric secretions[92]. But now the school of thought is more toward acid-mediated inflammation through cytokines than direct injury[93]. Receptors mediating nociception such as protease-activated receptor-2, also cause inflammation of the mucosa through cytokines such as interleukin-8 (IL-8)[94]. Its levels increase with the progression of the disease, while they decrease with treatment[95]. IL-1β and IL-6 are other cytokines noted to be expressed at high levels in the esophageal mucosa of GERD patients[96]. This inflammatory process of the mucosa of the esophagus is what causes reflux esophagitis or ERD[24].
Continuous inflammation can sometimes change the normal esophageal stratified squamous epithelium into a metaplastic columnar epithelium, leading to Barrett’s esophagus (BE). BE is diagnosed if the columnar epithelium is more than 1 cm proximal to the gastroesophageal junction, together with confirmation from biopsies. BE is a concerning situation, as there could be a progression from metaplastic to dysplastic epithelium and even to carcinoma[91]. Mucosal damage and chronic inflammatory changes can also cause fibrosis, scarring, and loss of esophageal distensibility, leading to an esophageal stricture with dysphagia as a symptom[90].
GERD is a common disorder with high worldwide prevalence. Its burden on some regions of the world is still not clear due to a lack of research and variations in screening tools and diagnostic criteria. When studied, the prevalence is estimated using GERD symptoms, and the exact prevalence of confirmed GERD (using endoscopy and gastrointestinal physiology investigations) is unknown. Accurate knowledge on GERD prevalence is crucial for allocating resources effectively. This includes ensuring access to gastroenterology specialists and diagnostic tools such as endoscopy, pH impedance testing, and esophageal manometry, as well as medications and facilities for surgical treatment options like fundoplication. GERD is a lifelong debilitating disorder with poor QoL, high health care costs, and multiple complications. Early diagnosis and effective treatment are essential to reduce the burden of this disease on the healthcare system and to improve the QoL. A global consensus must be reached to develop highly sensitive symptomatic diagnostic criteria for screening GERD patients as well as for effective management of this cumbersome and complicated disease.
| 1. | Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022;117:27-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 463] [Article Influence: 154.3] [Reference Citation Analysis (1)] |
| 2. | Sontag SJ. Defining GERD. Yale J Biol Med. 1999;72:69-80. [PubMed] |
| 3. | Belhocine K, Galmiche JP. Epidemiology of the complications of gastroesophageal reflux disease. Dig Dis. 2009;27:7-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 4. | Ayazi S, Hagen JA, Chan LS, DeMeester SR, Lin MW, Ayazi A, Leers JM, Oezcelik A, Banki F, Lipham JC, DeMeester TR, Crookes PF. Obesity and gastroesophageal reflux: quantifying the association between body mass index, esophageal acid exposure, and lower esophageal sphincter status in a large series of patients with reflux symptoms. J Gastrointest Surg. 2009;13:1440-1447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Argyrou A, Legaki E, Koutserimpas C, Gazouli M, Papaconstantinou I, Gkiokas G, Karamanolis G. Risk factors for gastroesophageal reflux disease and analysis of genetic contributors. World J Clin Cases. 2018;6:176-182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (3)] |
| 6. | Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1256] [Cited by in RCA: 1261] [Article Influence: 63.1] [Reference Citation Analysis (0)] |
| 7. | Moraes-Filho JP, Chinzon D, Eisig JN, Hashimoto CL, Zaterka S. Prevalence of heartburn and gastroesophageal reflux disease in the urban Brazilian population. Arq Gastroenterol. 2005;42:122-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Sontag SJ. Rolling review: gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 1993;7:293-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Wickramasinghe N, Thuraisingham A, Jayalath A, Wickramasinghe D, Samarasekara N, Yazaki E, Devanarayana NM. The association between symptoms of gastroesophageal reflux disease and perceived stress: A countrywide study of Sri Lanka. PLoS One. 2023;18:e0294135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Nebel OT, Fornes MF, Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976;21:953-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 540] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 11. | Rothman M, Farup C, Stewart W, Helbers L, Zeldis J. Symptoms associated with gastroesophageal reflux disease: development of a questionnaire for use in clinical trials. Dig Dis Sci. 2001;46:1540-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Dent J, Brun J, Fendrick A, Fennerty M, Janssens J, Kahrilas P, Lauritsen K, Reynolds J, Shaw M, Talley N. An evidence-based appraisal of reflux disease management--the Genval Workshop Report. Gut. 1999;44 Suppl 2:S1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 547] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 13. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900-20; quiz 1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2368] [Cited by in RCA: 2451] [Article Influence: 129.0] [Reference Citation Analysis (2)] |
| 14. | Sharma P, Wani S, Romero Y, Johnson D, Hamilton F. Racial and geographic issues in gastroesophageal reflux disease. Am J Gastroenterol. 2008;103:2669-2680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Spechler SJ, Jain SK, Tendler DA, Parker RA. Racial differences in the frequency of symptoms and complications of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2002;16:1795-1800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 113] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 16. | Kia L, Hirano I. Distinguishing GERD from eosinophilic oesophagitis: concepts and controversies. Nat Rev Gastroenterol Hepatol. 2015;12:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Diehl AK. Symptoms of gallstone disease. Baillieres Clin Gastroenterol. 1992;6:635-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Simpson FG, Kay J, Aber CP. Chest pain--indigestion or impending heart attack? Postgrad Med J. 1984;60:338-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Klauser AG, Schindlbeck NE, Müller-Lissner SA. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990;335:205-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 457] [Article Influence: 13.1] [Reference Citation Analysis (2)] |
| 20. | Kahrilas PJ. Regurgitation in patients with gastroesophageal reflux disease. Gastroenterol Hepatol (N Y). 2013;9:37-39. [PubMed] |
| 21. | Jung DH, Park H. Is Gastroesophageal Reflux Disease and Achalasia Coincident or Not? J Neurogastroenterol Motil. 2017;23:5-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Talley NJ. Rumination syndrome. Gastroenterol Hepatol (N Y). 2011;7:117-118. [PubMed] |
| 23. | Martínek J, Benes M, Hucl T, Drastich P, Stirand P, Spicák J. Non-erosive and erosive gastroesophageal reflux diseases: No difference with regard to reflux pattern and motility abnormalities. Scand J Gastroenterol. 2008;43:794-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ, Tytgat GN, Wallin L. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1518] [Cited by in RCA: 1653] [Article Influence: 63.6] [Reference Citation Analysis (1)] |
| 25. | Gyawali CP, Kahrilas PJ, Savarino E, Zerbib F, Mion F, Smout AJPM, Vaezi M, Sifrim D, Fox MR, Vela MF, Tutuian R, Tack J, Bredenoord AJ, Pandolfino J, Roman S. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351-1362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 672] [Cited by in RCA: 944] [Article Influence: 134.9] [Reference Citation Analysis (0)] |
| 26. | El-Serag HB. Epidemiology of non-erosive reflux disease. Digestion. 2008;78 Suppl 1:6-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Sawada A, Sifrim D, Fujiwara Y. Esophageal Reflux Hypersensitivity: A Comprehensive Review. Gut Liver. 2023;17:831-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 28. | Fass R, Tougas G. Functional heartburn: the stimulus, the pain, and the brain. Gut. 2002;51:885-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 165] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 29. | Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Functional Esophageal Disorders. Gastroenterology. 2016;150:1368-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 374] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 30. | Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308-28; quiz 329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1136] [Cited by in RCA: 1119] [Article Influence: 93.3] [Reference Citation Analysis (0)] |
| 31. | Fass R, Dickman R. Clinical consequences of silent gastroesophageal reflux disease. Curr Gastroenterol Rep. 2006;8:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Fass R. Symptom assessment tools for gastroesophageal reflux disease (GERD) treatment. J Clin Gastroenterol. 2007;41:437-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Dent J, Vakil N, Jones R, Bytzer P, Schöning U, Halling K, Junghard O, Lind T. Accuracy of the diagnosis of GORD by questionnaire, physicians and a trial of proton pump inhibitor treatment: the Diamond Study. Gut. 2010;59:714-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 251] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 34. | Nirwan JS, Hasan SS, Babar ZU, Conway BR, Ghori MU. Global Prevalence and Risk Factors of Gastro-oesophageal Reflux Disease (GORD): Systematic Review with Meta-analysis. Sci Rep. 2020;10:5814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 182] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 35. | Bolier EA, Kessing BF, Smout AJ, Bredenoord AJ. Systematic review: questionnaires for assessment of gastroesophageal reflux disease. Dis Esophagus. 2015;28:105-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 36. | Bai Y, Du Y, Zou D, Jin Z, Zhan X, Li ZS, Yang Y, Liu Y, Zhang S, Qian J, Zhou L, Hao J, Chen D, Fang D, Fan D, Yu X, Sha W, Nie Y, Zhang X, Xu H, Lv N, Jiang B, Zou X, Fang J, Fan J, Li Y, Chen W, Wang B, Zou Y, Li Y, Sun M, Chen Q, Chen M, Zhao X; Chinese GerdQ Research Group. Gastroesophageal Reflux Disease Questionnaire (GerdQ) in real-world practice: a national multicenter survey on 8065 patients. J Gastroenterol Hepatol. 2013;28:626-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 37. | Goh KL. Changing epidemiology of gastroesophageal reflux disease in the Asian-Pacific region: an overview. J Gastroenterol Hepatol. 2004;19 Suppl 3:S22-S25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Bredenoord AJ, Weusten BL, Timmer R, Conchillo JM, Smout AJ. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy. Am J Gastroenterol. 2006;101:453-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 39. | Kahrilas PJ, Quigley EM. Clinical esophageal pH recording: a technical review for practice guideline development. Gastroenterology. 1996;110:1982-1996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 313] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 40. | Savarino E, Tutuian R, Zentilin P, Dulbecco P, Pohl D, Marabotto E, Parodi A, Sammito G, Gemignani L, Bodini G, Savarino V. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: study using combined impedance-pH off therapy. Am J Gastroenterol. 2010;105:1053-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 178] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 41. | Sifrim D, Roman S, Savarino E, Bor S, Bredenoord AJ, Castell D, Cicala M, de Bortoli N, Frazzoni M, Gonlachanvit S, Iwakiri K, Kawamura O, Krarup A, Lee YY, Soon Ngiu C, Ndebia E, Patcharatraku T, Pauwels A, Pérez de la Serna J, Ramos R, Remes-Troche JM, Ribolsi M, Sammon A, Simren M, Tack J, Tutuian R, Valdovinos M, Xiao Y, Zerbib F, Gyawali CP. Normal values and regional differences in oesophageal impedance-pH metrics: a consensus analysis of impedance-pH studies from around the world. Gut. 2020;70:1441-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 42. | Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 620] [Cited by in RCA: 604] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 43. | Zerbib F, Roman S, Bruley Des Varannes S, Gourcerol G, Coffin B, Ropert A, Lepicard P, Mion F; Groupe Français De Neuro-Gastroentérologie. Normal values of pharyngeal and esophageal 24-hour pH impedance in individuals on and off therapy and interobserver reproducibility. Clin Gastroenterol Hepatol. 2013;11:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 131] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 44. | Tenca A, Campagnola P, Bravi I, Benini L, Sifrim D, Penagini R. Impedance pH Monitoring: Intra-observer and Inter-observer Agreement and Usefulness of a Rapid Analysis of Symptom Reflux Association. J Neurogastroenterol Motil. 2014;20:205-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Koop AH, Francis DL, DeVault KR. Visual and Automated Computer Analysis Differ Substantially in Detection of Acidic Reflux in Multichannel Intraluminal Impedance-pH Monitoring. Clin Gastroenterol Hepatol. 2018;16:979-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 46. | Hemmink GJ, Bredenoord AJ, Aanen MC, Weusten BL, Timmer R, Smout AJ. Computer analysis of 24-h esophageal impedance signals. Scand J Gastroenterol. 2011;46:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 47. | Frazzoni L, Frazzoni M, de Bortoli N, Tolone S, Martinucci I, Fuccio L, Savarino V, Savarino E. Critical appraisal of Rome IV criteria: hypersensitive esophagus does belong to gastroesophageal reflux disease spectrum. Ann Gastroenterol. 2018;31:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 48. | Chen X, Wang F. Refractory Gastroesophageal Reflux Disease (GERD) Symptoms. In: Gastroesophageal Reflux Disease - Theory and Research. London: IntechOpen, 2019. [DOI] [Full Text] |
| 49. | Martos Vizcaino E, Canga Rodriguez-Valcárcel F, Ciriza de Los Ríos C. Rumination Syndrome: Unknown Pathology Easy to Diagnose With High-resolution Impedance Manometry. J Neurogastroenterol Motil. 2018;24:503-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 50. | Savarino E, Bredenoord AJ, Fox M, Pandolfino JE, Roman S, Gyawali CP; International Working Group for Disorders of Gastrointestinal Motility and Function. Expert consensus document: Advances in the physiological assessment and diagnosis of GERD. Nat Rev Gastroenterol Hepatol. 2017;14:665-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 142] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 51. | Trudgill NJ, Sifrim D, Sweis R, Fullard M, Basu K, McCord M, Booth M, Hayman J, Boeckxstaens G, Johnston BT, Ager N, De Caestecker J. British Society of Gastroenterology guidelines for oesophageal manometry and oesophageal reflux monitoring. Gut. 2019;68:1731-1750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 52. | Rossi P, Isoldi S, Mallardo S, Papoff P, Rossetti D, Dilillo A, Oliva S. Combined multichannel intraluminal impedance and pH monitoring is helpful in managing children with suspected gastro-oesophageal reflux disease. Dig Liver Dis. 2018;50:910-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 53. | Hershcovici T, Fass R. Nonerosive Reflux Disease (NERD) - An Update. J Neurogastroenterol Motil. 2010;16:8-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 54. | Schneider H. Gastro-oesophageal reflux disease: The Montreal definition and classification. S Afr Fam Pract. 2007;49:19-26. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 55. | El-Serag HB. Time trends of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2007;5:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 306] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 56. | Shaha M, Perveen I, Alamgir MJ, Masud MH, Rahman MH. Prevalence and risk factors for gastro-esophageal reflux disease in the North-Eastern part of Bangladesh. Bangladesh Med Res Counc Bull. 2012;38:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 57. | Bhatia SJ, Reddy DN, Ghoshal UC, Jayanthi V, Abraham P, Choudhuri G, Broor SL, Ahuja V, Augustine P, Balakrishnan V, Bhasin DK, Bhat N, Chacko A, Dadhich S, Dhali GK, Dhawan PS, Dwivedi M, Goenka MK, Koshy A, Kumar A, Misra SP, Mukewar S, Raju EP, Shenoy KT, Singh SP, Sood A, Srinivasan R. Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2011;30:118-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 58. | Kumar S, Shivalli S. Prevalence, Perceptions and Profile of Gastroesophageal Reflux Disease in A Rural Population of North Bihar. Natl J Community Med. 2014;5:214-218. |
| 59. | Wickramasinghe N, Thuraisingham A, Jayalath A, Wickramasinghe D, Samarasekera DN, Yazaki E, Devanarayana NM. Gastroesophageal reflux disease in Sri Lanka: An island-wide epidemiological survey assessing the prevalence and associated factors. PLOS Glob Public Health. 2024;4:e0003162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 60. | El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1057] [Cited by in RCA: 1263] [Article Influence: 114.8] [Reference Citation Analysis (2)] |
| 61. | Katz PO. Lessons learned from intragastric pH monitoring. J Clin Gastroenterol. 2001;33:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 62. | Watson DI, Lally CJ. Prevalence of symptoms and use of medication for gastroesophageal reflux in an Australian community. World J Surg. 2009;33:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Knox SA, Harrison CM, Britt HC, Henderson JV. Estimating prevalence of common chronic morbidities in Australia. Med J Aust. 2008;189:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 64. | Salis G. [Systematic review: Epidemiology of gastroesophageal reflux disease in Latin America]. Acta Gastroenterol Latinoam. 2011;41:60-69. [PubMed] |
| 65. | Jung HK. Epidemiology of gastroesophageal reflux disease in Asia: a systematic review. J Neurogastroenterol Motil. 2011;17:14-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 174] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 66. | Wu JC. Gastroesophageal reflux disease: an Asian perspective. J Gastroenterol Hepatol. 2008;23:1785-1793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 67. | Song HJ, Shim KN, Yoon SJ, Kim SE, Oh HJ, Ryu KH, Ha CY, Yeom HJ, Song JH, Jung SA, Yoo K. The prevalence and clinical characteristics of reflux esophagitis in koreans and its possible relation to metabolic syndrome. J Korean Med Sci. 2009;24:197-202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 68. | He J, Ma X, Zhao Y, Wang R, Yan X, Yan H, Yin P, Kang X, Fang J, Hao Y, Li Q, Dent J, Sung JJ, Zou D, Wallander MA, Johansson S, Liu W, Li Z. A population-based survey of the epidemiology of symptom-defined gastroesophageal reflux disease: the Systematic Investigation of Gastrointestinal Diseases in China. BMC Gastroenterol. 2010;10:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 69. | Hung LJ, Hsu PI, Yang CY, Wang EM, Lai KH. Prevalence of gastroesophageal reflux disease in a general population in Taiwan. J Gastroenterol Hepatol. 2011;26:1164-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 70. | Almadi MA, Almousa MA, Althwainy AF, Altamimi AM, Alamoudi HO, Alshamrani HS, Alharbi OR, Azzam NA, Sadaf N, Aljebreen AM. Prevalence of symptoms of gastroesopahgeal reflux in a cohort of Saudi Arabians: a study of 1265 subjects. Saudi J Gastroenterol. 2014;20:248-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 71. | Karimian M, Nourmohammadi H, Salamati M, Hafezi Ahmadi MR, Kazemi F, Azami M. Epidemiology of gastroesophageal reflux disease in Iran: a systematic review and meta-analysis. BMC Gastroenterol. 2020;20:297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 72. | Bhatia S, Gupta DK, Vennalaganti P. Epidemiology of Gastroesophageal Reflux in Asia. In: Sharma P, Bhatia S, Goh K. The Rise of Acid Reflux in Asia. New Delhi: Springer, 2018. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 73. | Kumar S, Sharma S, Norboo T, Dolma D, Norboo A, Stobdan T, Rohatgi S, Munot K, Ahuja V, Saraya A. Population based study to assess prevalence and risk factors of gastroesophageal reflux disease in a high altitude area. Indian J Gastroenterol. 2011;30:135-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 74. | Wang HY, Leena KB, Plymoth A, Hergens MP, Yin L, Shenoy KT, Ye W. Prevalence of gastro-esophageal reflux disease and its risk factors in a community-based population in southern India. BMC Gastroenterol. 2016;16:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 75. | Pourhoseingholi A, Pourhoseingholi MA, Moghimi-Dehkordi B, Barzegar F, Safaee A, Vahedi M, Dulaimi DA, Prabhakaran S. Epidemiological features of gastro-esophageal reflux disease in Iran based on general population. Gastroenterol Hepatol Bed Bench. 2012;5:54-59. [PubMed] |
| 76. | Min BH, Huh KC, Jung HK, Yoon YH, Choi KD, Song KH, Keum B, Kim JW; Functional Dyspepsia Study Group of Korean Society of Neurogastroenterology and Motility. Prevalence of uninvestigated dyspepsia and gastroesophageal reflux disease in Korea: a population-based study using the Rome III criteria. Dig Dis Sci. 2014;59:2721-2729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 77. | Yönem Ö, Sivri B, Özdemir L, Nadir I, Yüksel S, Uygun Y. Gastroesophageal reflux disease prevalence in the city of Sivas. Turk J Gastroenterol. 2013;24:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 78. | Wang JH, Luo JY, Dong L, Gong J, Tong M. Epidemiology of gastroesophageal reflux disease: a general population-based study in Xi'an of Northwest China. World J Gastroenterol. 2004;10:1647-1651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 113] [Cited by in RCA: 117] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 79. | Ma XQ, Cao Y, Wang R, Yan X, Zhao Y, Zou D, Wallander MA, Johansson S, Liu W, Gu Z, Zhao J, He J. Prevalence of, and factors associated with, gastroesophageal reflux disease: a population-based study in Shanghai, China. Dis Esophagus. 2009;22:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 80. | GBD 2017 Gastro-oesophageal Reflux Disease Collaborators. The global, regional, and national burden of gastro-oesophageal reflux disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:561-581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 97] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 81. | Zhang D, Liu S, Li Z, Wang R. Global, regional and national burden of gastroesophageal reflux disease, 1990-2019: update from the GBD 2019 study. Ann Med. 2022;54:1372-1384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 94] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 82. | Peery AF, Crockett SD, Murphy CC, Jensen ET, Kim HP, Egberg MD, Lund JL, Moon AM, Pate V, Barnes EL, Schlusser CL, Baron TH, Shaheen NJ, Sandler RS. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022;162:621-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 475] [Article Influence: 158.3] [Reference Citation Analysis (1)] |
| 83. | Sharma P, Falk GW, Bhor M, Ozbay AB, Latremouille-Viau D, Guerin A, Shi S, Elvekrog MM, Limburg P. Healthcare Resource Utilization and Costs Among Patients With Gastroesophageal Reflux Disease, Barrett's Esophagus, and Barrett's Esophagus-Related Neoplasia in the United States. J Health Econ Outcomes Res. 2023;10:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 84. | Brook RA, Wahlqvist P, Kleinman NL, Wallander MA, Campbell SM, Smeeding JE. Cost of gastro-oesophageal reflux disease to the employer: a perspective from the United States. Aliment Pharmacol Ther. 2007;26:889-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 85. | Park S, Kwon JW, Park JM, Park S, Seo KW. Treatment Pattern and Economic Burden of Refractory Gastroesophageal Reflux Disease Patients in Korea. J Neurogastroenterol Motil. 2020;26:281-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 86. | Wahlqvist P, Karlsson M, Johnson D, Carlsson J, Bolge SC, Wallander MA. Relationship between symptom load of gastro-oesophageal reflux disease and health-related quality of life, work productivity, resource utilization and concomitant diseases: survey of a US cohort. Aliment Pharmacol Ther. 2008;27:960-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 87. | Jurkowska G, Świdnicka-siergiejko A, Łagoda K, Sierżantowicz R, Dąbrowski A. Quality of life in patients with gastroesophageal reflux disease following pharmacotherapeutic, endoscopic, and surgical treatment. Studia Medyczne. 2016;4:299-306. [DOI] [Full Text] |
| 88. | Kleinman L, Nelson S, Kothari-Talwar S, Roberts L, Orenstein SR, Mody RR, Hassall E, Gold B, Revicki DA, Dabbous O. Development and psychometric evaluation of 2 age-stratified versions of the Pediatric GERD Symptom and Quality of Life Questionnaire. J Pediatr Gastroenterol Nutr. 2011;52:514-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 89. | Alshammari SA, Alabdulkareem AM, Aloqeely KM, Alhumud MI, Alghufaily SA, Al-Dossare YI, Alrashdan NO. The Determinants of the Quality of Life of Gastroesophageal Reflux Disease Patients Attending King Saud University Medical City. Cureus. 2020;12:e9505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 90. | Triggs JR, Pandolfino JE. Esophageal Strictures. 2nd ed. In: Kuipers EJ. Encyclopedia of Gastroenterology. Elsevier, 2020. [DOI] [Full Text] |
| 91. | Eluri S, Shaheen NJ. Barrett's esophagus: diagnosis and management. Gastrointest Endosc. 2017;85:889-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 92. | Spechler SJ. Carcinogenesis at the gastroesophageal junction: free radicals at the frontier. Gastroenterology. 2002;122:1518-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 93. | Dunbar KB, Agoston AT, Odze RD, Huo X, Pham TH, Cipher DJ, Castell DO, Genta RM, Souza RF, Spechler SJ. Association of Acute Gastroesophageal Reflux Disease With Esophageal Histologic Changes. JAMA. 2016;315:2104-2112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 177] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 94. | Vergnolle N, Bunnett NW, Sharkey KA, Brussee V, Compton SJ, Grady EF, Cirino G, Gerard N, Basbaum AI, Andrade-Gordon P, Hollenberg MD, Wallace JL. Proteinase-activated receptor-2 and hyperalgesia: A novel pain pathway. Nat Med. 2001;7:821-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 364] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 95. | Yoshida N, Imamura Y, Baba Y, Baba H. Pathogenesis of acute gastroesophageal reflux disease might be changing. Transl Cancer Res. 2016;5:S645-S647. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 96. | Rieder F, Cheng L, Harnett KM, Chak A, Cooper GS, Isenberg G, Ray M, Katz JA, Catanzaro A, O'Shea R, Post AB, Wong R, Sivak MV, McCormick T, Phillips M, West GA, Willis JE, Biancani P, Fiocchi C. Gastroesophageal reflux disease-associated esophagitis induces endogenous cytokine production leading to motor abnormalities. Gastroenterology. 2007;132:154-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 108] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 97. | Shim KN, Hong SJ, Sung JK, Park KS, Kim SE, Park HS, Kim YS, Lim SH, Kim CH, Park MJ, Yim JY, Cho KR, Kim D, Park SJ, Jee SR, Kim JI, Park JY, Song GA, Jung HY, Lee YC, Kim JG, Kim JJ, Kim N, Park SH, Jung HC, Chung IS; H. pylori and GERD Study Group of Korean College of Helicobacter and Upper Gastrointestinal Research. Clinical spectrum of reflux esophagitis among 25,536 Koreans who underwent a health check-up: a nationwide multicenter prospective, endoscopy-based study. J Clin Gastroenterol. 2009;43:632-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 98. | Kidambi T, Toto E, Ho N, Taft T, Hirano I. Temporal trends in the relative prevalence of dysphagia etiologies from 1999-2009. World J Gastroenterol. 2012;18:4335-4341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 71] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 99. | Jones D, Prowse S. Globus pharyngeus: an update for general practice. Br J Gen Pract. 2015;65:554-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 100. | Gerson LB, Kahrilas PJ, Fass R. Insights into gastroesophageal reflux disease-associated dyspeptic symptoms. Clin Gastroenterol Hepatol. 2011;9:824-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 101. | Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Air swallowing, belching, and reflux in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2006;101:1721-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 102. | Morton JM, Bowers SP, Lucktong TA, Mattar S, Bradshaw WA, Behrns KE, Koruda MJ, Herbst CA, McCartney W, Halkar RK, Smith CD, Farrell TM. Gallbladder function before and after fundoplication. J Gastrointest Surg. 2002;6:806-10; discussion 810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 103. | Aamodt AH, Stovner LJ, Hagen K, Zwart JA. Comorbidity of headache and gastrointestinal complaints. The Head-HUNT Study. Cephalalgia. 2008;28:144-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 53] [Reference Citation Analysis (1)] |
| 104. | Jung HK, Choung RS, Talley NJ. Gastroesophageal reflux disease and sleep disorders: evidence for a causal link and therapeutic implications. J Neurogastroenterol Motil. 2010;16:22-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 105. | Yandrapu H, Marcinkiewicz M, Poplawski C, Han K, Zbroch T, Goldin G, Sarosiek I, Namiot Z, Sarosiek J. Role of saliva in esophageal defense: implications in patients with nonerosive reflux disease. Am J Med Sci. 2015;349:385-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 106. | Gharaibeh TM, Jadallah K, Jadayel FA. Prevalence of temporomandibular disorders in patients with gastroesophageal reflux disease: a case-controlled study. J Oral Maxillofac Surg. 2010;68:1560-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 107. | Irwin RS, Corrao WM, Pratter MR. Chronic persistent cough in the adult: the spectrum and frequency of causes and successful outcome of specific therapy. Am Rev Respir Dis. 1981;123:413-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 82] [Reference Citation Analysis (0)] |
| 108. | Fraser AG. Review article: gastro-oesophageal reflux and laryngeal symptoms. Aliment Pharmacol Ther. 1994;8:265-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 109. | Mallah N, Turner JM, González-Barcala FJ, Takkouche B. Gastroesophageal reflux disease and asthma exacerbation: A systematic review and meta-analysis. Pediatr Allergy Immunol. 2022;33:e13655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 110. | Miura MS, Mascaro M, Rosenfeld RM. Association between otitis media and gastroesophageal reflux: a systematic review. Otolaryngol Head Neck Surg. 2012;146:345-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 111. | Lin YH, Chang TS, Yao YC, Li YC. Increased Risk of Chronic Sinusitis in Adults With Gastroesophgeal Reflux Disease: A Nationwide Population-Based Cohort Study. Medicine (Baltimore). 2015;94:e1642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 112. | Liu J, Wang W, Wang Y, Wu D, Sun C, Lv C, Wu D, Yu Y. Subjective Changes of Taste and Smell in Conjunction With Anxiety and Depression Are Associated With Symptoms in Globus Patients Without Evidence of Pathologic Acid Reflux. J Clin Gastroenterol. 2022;56:505-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 113. | Kabadi A, Saadi M, Schey R, Parkman HP. Taste and Smell Disturbances in Patients with Gastroparesis and Gastroesophageal Reflux Disease. J Neurogastroenterol Motil. 2017;23:370-377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 114. | Wang FW, Tu MS, Chuang HY, Yu HC, Cheng LC, Hsu PI. Erosive esophagitis in asymptomatic subjects: risk factors. Dig Dis Sci. 2010;55:1320-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 115. | Spechler SJ, Genta RM, Souza RF. Thoughts on the complex relationship between gastroesophageal reflux disease and eosinophilic esophagitis. Am J Gastroenterol. 2007;102:1301-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 255] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 116. | Rosołowski M, Kierzkiewicz M. Etiology, diagnosis and treatment of infectious esophagitis. Prz Gastroenterol. 2013;8:333-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 117. | Zografos GN, Georgiadou D, Thomas D, Kaltsas G, Digalakis M. Drug-induced esophagitis. Dis Esophagus. 2009;22:633-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 118. | Spechler SJ, Souza RF, Rosenberg SJ, Ruben RA, Goyal RK. Heartburn in patients with achalasia. Gut. 1995;37:305-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 69] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 119. | Liu JJ, Kahrilas PJ. Pharyngeal and esophageal diverticula, rings, and webs. GI Motility Online. 2006;. [DOI] [Full Text] |
| 120. | Jehangir A, Parkman HP. Reflux Symptoms in Gastroparesis: Correlation With Gastroparesis Symptoms, Gastric Emptying, and Esophageal Function Testing. J Clin Gastroenterol. 2020;54:428-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 121. | Najm WI. Peptic ulcer disease. Prim Care. 2011;38:383-394, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 122. | Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DS, Schumann M, Ullrich R, Villalta D, Volta U, Catassi C, Fasano A. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012;10:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 809] [Cited by in RCA: 676] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 123. | Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016;150:1262-1279.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1366] [Cited by in RCA: 1383] [Article Influence: 153.7] [Reference Citation Analysis (1)] |
| 124. | Abbas G, Krasna M. Overview of esophageal cancer. Ann Cardiothorac Surg. 2017;6:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 159] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 125. | Tougas G, Spaziani R, Hollerbach S, Djuric V, Pang C, Upton AR, Fallen EL, Kamath MV. Cardiac autonomic function and oesophageal acid sensitivity in patients with non-cardiac chest pain. Gut. 2001;49:706-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 126. | Pera M, Trastek VF, Carpenter HA, Fernandez PL, Cardesa A, Mohr U, Pairolero PC. Influence of pancreatic and biliary reflux on the development of esophageal carcinoma. Ann Thorac Surg. 1993;55:1386-92; discussion 1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 127. | Goh KL, Chang CS, Fock KM, Ke M, Park HJ, Lam SK. Gastro-oesophageal reflux disease in Asia. J Gastroenterol Hepatol. 2000;15:230-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 101] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 128. | Friedland GW. Progress in radiology: historical review of the changing concepts of lower esophageal anatomy: 430 B.C.--1977. AJR Am J Roentgenol. 1978;131:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 37] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 129. | Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 437] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 130. | Seto KC, Fragkias M, Güneralp B, Reilly MK. A meta-analysis of global urban land expansion. PLoS One. 2011;6:e23777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1205] [Cited by in RCA: 552] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 131. | Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 828] [Cited by in RCA: 796] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 132. | Corley DA, Kubo A. Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Gastroenterol. 2006;101:2619-2628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 233] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 133. | Söderholm JD. Stress-related changes in oesophageal permeability: filling the gaps of GORD? Gut. 2007;56:1177-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 134. | Fass R, Quan SF, O'Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127:1658-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 126] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 135. | Song JH, Chung SJ, Lee JH, Kim YH, Chang DK, Son HJ, Kim JJ, Rhee JC, Rhee PL. Relationship between gastroesophageal reflux symptoms and dietary factors in Korea. J Neurogastroenterol Motil. 2011;17:54-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 136. | Gudjonsson H, McAuliffe TL, Kaye MD. [The effect of coffee and tea upon lower esophageal sphincteric function]. Laeknabladid. 1995;81:484-488. [PubMed] |
| 137. | Thomas FB, Steinbaugh JT, Fromkes JJ, Mekhjian HS, Caldwell JH. Inhibitory effect of coffee on lower esophageal sphincter pressure. Gastroenterology. 1980;79:1262-1266. [PubMed] [DOI] [Full Text] |
| 138. | Price SF, Smithson KW, Castell DO. Food sensitivity in reflux esophagitis. Gastroenterology. 1978;75:240-243. [PubMed] [DOI] [Full Text] |
| 139. | Murphy DW, Castell DO. Chocolate and heartburn: evidence of increased esophageal acid exposure after chocolate ingestion. Am J Gastroenterol. 1988;83:633-636. [PubMed] |
| 140. | Riegler M, Kristo I, Asari R, Rieder E, Schoppmann SF. Dietary sugar and Barrett's esophagus. Eur Surg. 2017;49:279-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 141. | Iwakiri K, Kobayashi M, Kotoyori M, Yamada H, Sugiura T, Nakagawa Y. Relationship between postprandial esophageal acid exposure and meal volume and fat content. Dig Dis Sci. 1996;41:926-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 142. | Parasher A, Ranjan K. The prevalence of gastroesophageal reflux disease and its association with various risk factors in a tertiary care centre in West Bengal. Int J Res Med Sci. 2021;9:780. [DOI] [Full Text] |
| 143. | Yamamichi N, Mochizuki S, Asada-Hirayama I, Mikami-Matsuda R, Shimamoto T, Konno-Shimizu M, Takahashi Y, Takeuchi C, Niimi K, Ono S, Kodashima S, Minatsuki C, Fujishiro M, Mitsushima T, Koike K. Lifestyle factors affecting gastroesophageal reflux disease symptoms: a cross-sectional study of healthy 19864 adults using FSSG scores. BMC Med. 2012;10:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 144. | Pandeya N, Green AC, Whiteman DC; Australian Cancer Study. Prevalence and determinants of frequent gastroesophageal reflux symptoms in the Australian community. Dis Esophagus. 2012;25:573-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 145. | Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut. 2004;53:1730-1735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 233] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 146. | Avidan B, Sonnenberg A, Schnell TG, Sontag SJ. Temporal associations between coughing or wheezing and acid reflux in asthmatics. Gut. 2001;49:767-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 147. | Sun XM, Tan JC, Zhu Y, Lin L. Association between diabetes mellitus and gastroesophageal reflux disease: A meta-analysis. World J Gastroenterol. 2015;21:3085-3092. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 44] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (2)] |
| 148. | Spence AD, Busby J, Murchie P, Kunzmann AT, McMenamin ÚC, Coleman HG, Johnston BT, O'Rorke MA, Murray LJ, Iversen L, Lee AJ, Cardwell CR. Medications that relax the lower oesophageal sphincter and risk of oesophageal cancer: An analysis of two independent population-based databases. Int J Cancer. 2018;143:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 149. | DiMarino AJ, Cohen S. The adrenergic control of lower esophageal sphincter function. An experimental model of denervation supersensitivity. J Clin Invest. 1973;52:2264-2271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 150. | Berquist WE, Rachelefsky GS, Kadden M, Siegel SC, Katz RM, Mickey MR, Ament ME. Effect of theophylline on gastroesophageal reflux in normal adults. J Allergy Clin Immunol. 1981;67:407-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 69] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 151. | Farrell RL, Roling GT, Castell DO. Stimulation of the incompetent lower esophageal sphincter. A possible advance in therapy of heartburn. Am J Dig Dis. 1973;18:646-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 28] [Article Influence: 0.5] [Reference Citation Analysis (0)] |