Copyright
©The Author(s) 2021.
World J Gastrointest Pathophysiol. May 22, 2021; 12(3): 25-39
Published online May 22, 2021. doi: 10.4291/wjgp.v12.i3.25
Published online May 22, 2021. doi: 10.4291/wjgp.v12.i3.25
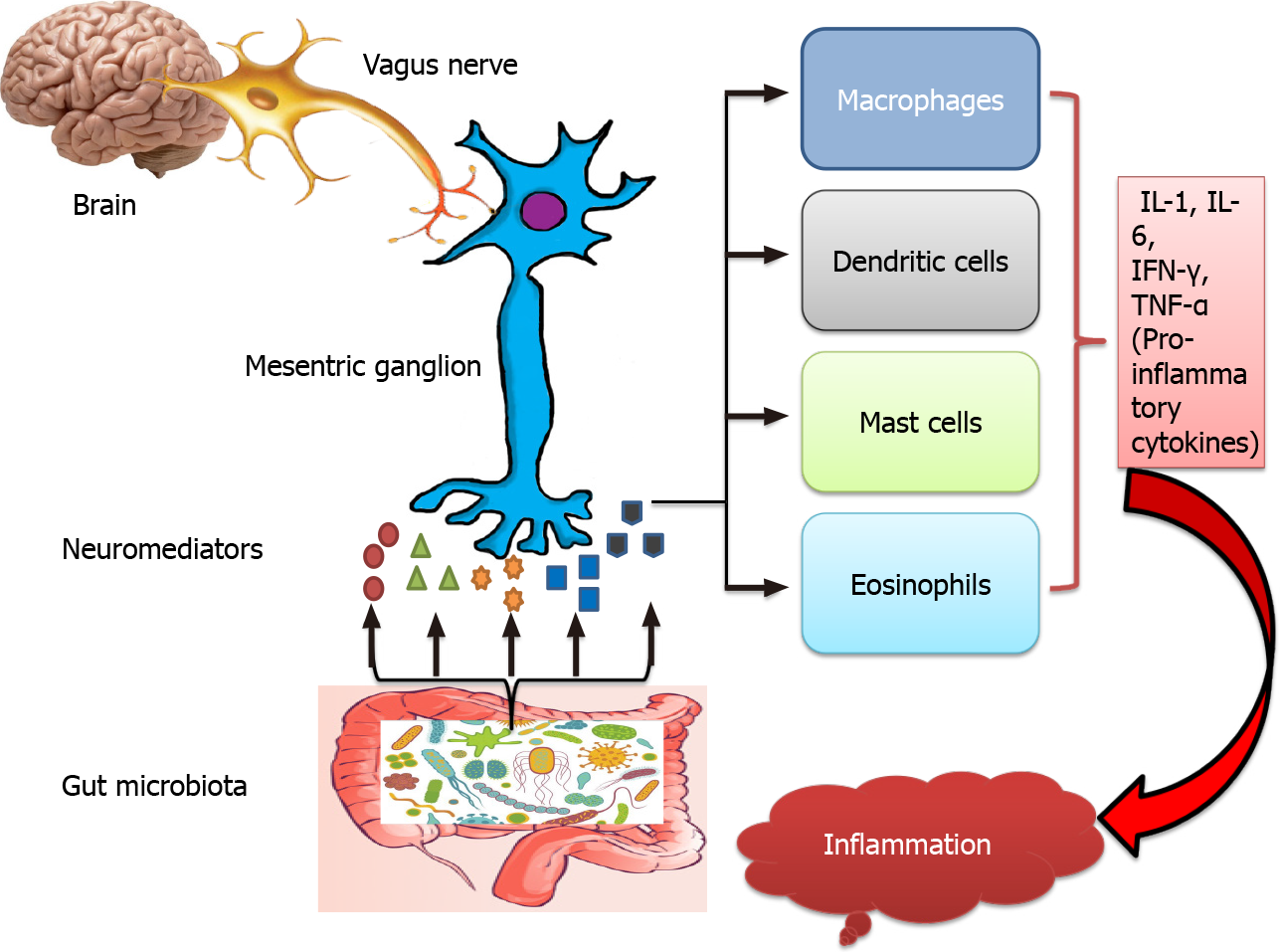
Figure 1 Modulation of cross-talk between the enteric nervous system and the enteric immune system via gut bacteria.
Gut microbiota and vagus nerve stimulate mesenteric ganglion (enteric neuron) to produce neuromediators. Neuromediators act on various immune cells and influence their ability to release pro-inflammatory cytokines. During inflammatory bowel disease, dysbiosis in gut microbiota and abnormality in the enteric nervous system affect the level of neuromediators that results in overproduction of pro-inflammatory cytokines and promote inflammation. IL: Interleukin; TNF-α: Tumour necrosis factor-α; IFN-γ: Interferon-γ.
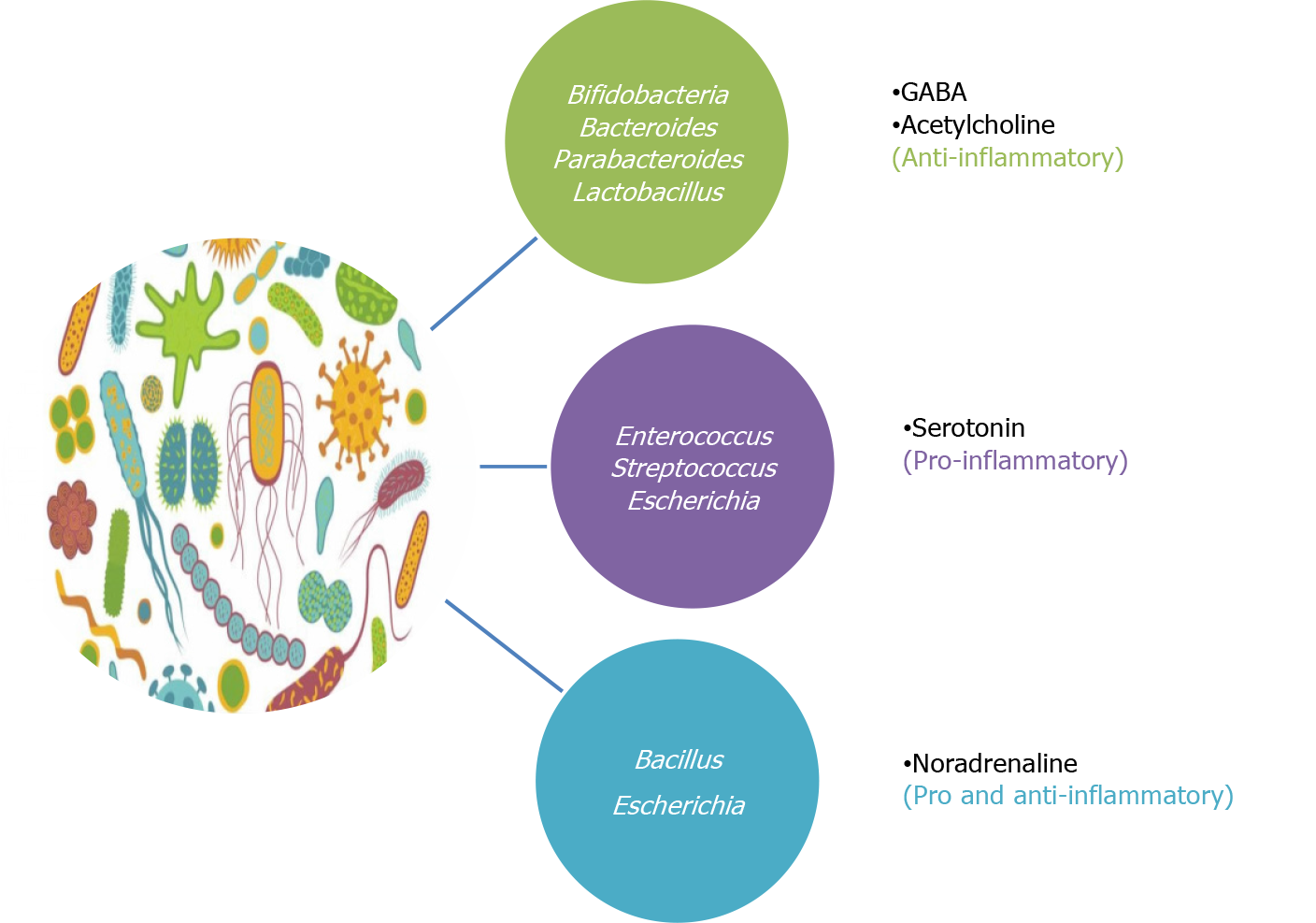
Figure 2 Inter-relation of diverse gut microbiota and their respective neuromediators with gut inflammation.
Bacteria used as probiotics in inflammatory bowel disease (IBD) (green box) produces anti-inflammatory neuromediators (γ-aminobutyric acid, acetylcholine), bacteria having a detrimental role in IBD (purple box) releases pro-inflammatory neuromediator (serotonin) and bacteria having a debatable role in IBD (blue box) secrete neuromediator (noradrenaline) having both pro and anti-inflammatory properties. GABA: γ-aminobutyric acid.
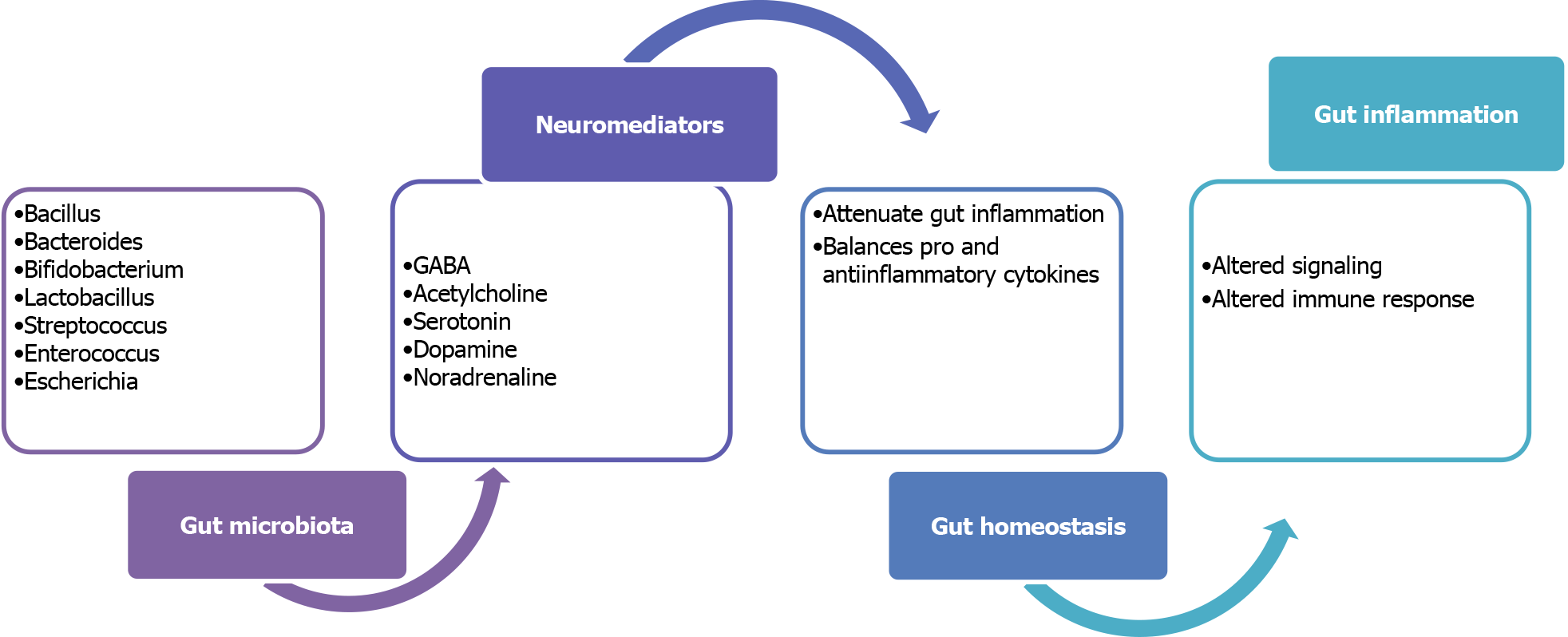
Figure 3 Role of neuromediators producing gut microbiota during gut inflammation.
Gut microbiota produces various neuromediators that attenuate the gut inflammation by balancing the pro and anti-inflammatory cytokines to maintain gut homeostasis. During inflammation, dysbiosis in gut microbiota leads to alteration in respective neuromediators which may lead to altered the host immune response. GABA: γ-aminobutyric acid.
- Citation: Aggarwal S, Ranjha R, Paul J. Neuroimmunomodulation by gut bacteria: Focus on inflammatory bowel diseases. World J Gastrointest Pathophysiol 2021; 12(3): 25-39
- URL: https://www.wjgnet.com/2150-5330/full/v12/i3/25.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v12.i3.25