Published online Jun 28, 2016. doi: 10.4329/wjr.v8.i6.594
Peer-review started: October 27, 2015
First decision: February 2, 2016
Revised: February 13, 2016
Accepted: March 22, 2016
Article in press: March 23, 2016
Published online: June 28, 2016
Processing time: 238 Days and 15.9 Hours
AIM: To use perfusion-derived permeability-surface area product maps to predict hemorrhagic transformation following thrombolytic treatment for acute ischemic stroke.
METHODS: We retrospectively analyzed our prospectively kept acute stroke database over five consecutive months for patients with symptoms of acute ischemic stroke (AIS) who had computed tomography (CT) perfusion (CTP) done at arrival. Patients included in the analyses also had to have a follow-up CT. The permeability-surface area product maps (PS) was calculated for the side of the ischemia and/or infarction and for the contralateral unaffected side at the same level. The cerebral blood flow map was used to delineate the ischemic territory. Next, a region of interest was drawn at the centre of this territory on the PS parametric map. Finally, a mirror region of interest was created on the contralateral side at the same level. The relative permeability-surface area product maps (rPS) provided an internal control and was calculated as the ratio of the PS on the side of the AIS to the PS on the contralateral side. A student t-test was performed after log conversion of rPS between patients with and without hemorrhagic transformation. Log conversion was used to convert the data into normal distribution to use t-test. For the group of patients who experienced intracranial bleed, a student t-test was performed between those with only petechial hemorrhage and those with more severe parenchymal hematoma with subarachnoid haemorrhage.
RESULTS: Of 84 patients with AIS and CTP at admission, only 42 patients had a follow-up CT. The rPS derived using the normal side as the internal control was significantly higher (P = 0.003) for the 15 cases of hemorrhagic transformation (1.71 + 1.64) compared to 27 cases that did not have any (1.07 + 1.30). Patients with values above the overall mean rPS of 1.3 had an increased likelihood of subsequent hemorrhagic transformation. The sensitivity of using this score to predict hemorrhagic transformation was 71.4, the specificity was 78.6, with a positive predictive value of 62.5 and negative predictive value of 84.6. The accuracy was 76.2. The odds ratio of an event occurring with such an rPS was 9.2. Of the 15 cases of hemorrhagic transformation, there was no difference (P = 0.35) in the rPS between the eight cases of petechial and the seven cases of more severe hemorrhagic events.
CONCLUSION: Pretreatment PS can predict the occurrence of hemorrhagic transformation on follow-up of AIS patients with relatively high sensitivity, specificity, positive and negative predictive value.
Core tip: Hemorrhagic transformation is one of the most important complications following thrombolytic treatment of acute ischemic stroke (AIS). Predicting hemorrhagic complication at presentation can be useful to clinicians. Perfusion-derived permeability-surface area product maps (PS) may help in predicting hemorrhagic transformation. We investigated whether PS can predict hemorrhagic transformation on follow-up. We found that pretreatment PS can predict the occurrence of hemorrhagic transformation on follow-up of AIS patients with relatively high sensitivity, specificity, positive and negative predictive value. However, it cannot predict the degree of severity, which is critical in the decision to treat.
- Citation: Yen P, Cobb A, Shankar JJS. Does computed tomography permeability predict hemorrhagic transformation after ischemic stroke? World J Radiol 2016; 8(6): 594-599
- URL: https://www.wjgnet.com/1949-8470/full/v8/i6/594.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i6.594
Thrombolytic therapy is the current mainstay[1], and the most promising treatment, for acute ischemic stroke (AIS). The aim is to restore blood flow and reperfuse ischemic brain tissue at risk of disastrous progression towards irreversible infarction. Although it is well established that this therapy has made significant reduction in the overall morbidity and improved the quality of life for stroke patients[2], it is not without complications[1,2]. In the hours and days following therapy, there is always a risk of intracranial bleeding, which has resulted in increased deaths for this treated group[3,4]. Multiple factors are associated with hemorrhagic transformation, such as reperfusion into a large volume of severely ischemic tissue[5]. One source reports the risk of death from intracranial hemorrhage in thrombolyzed patients to be as high as 4.45%, compared to 0.74% in those who were not treated[6]. In addition, the occurrence of intracranial hemorrhage is associated with an 8 to 10 fold increased risk of death[7,8]. Predicting whether patients are at greater risk for hemorrhagic transformation if thrombolytic therapy is applied is useful for clinicians, who can take this risk into consideration when deciding whether to proceed with such therapy.
Current imaging contraindication for thrombolytic therapy, according to the American Stroke Association, is greater than one-third of the hemisphere or multilobar involvement[9]. This guideline is quite crude and a method to evaluate the likelihood of hemorrhagic transformation on an individual basis could allow patients previously excluded due to the large volume of involved tissue to benefit from the therapy.
In addition to an unenhanced head computed tomography (CT), CT perfusion (CTP) is increasingly used in cases of suspected AIS to evaluate the tissue at risk. Data from the CTP can be used to generate information on the permeability of the blood-brain barrier as a function of ischemia-related vascular injury. This extracted permeability-surface area product map (PS) has been described by some studies as an independent predictor of future hemorrhagic transformation[10,11]. The primary purpose of this study is to assess whether PS can predict intracranial hemorrhage on follow-up scans in patients with acute ischemic stroke and, if so, whether the severity of the hemorrhagic event can be anticipated.
A retrospective review of a prospectively maintained acute stroke database at a tertiary care centre was performed on patients with symptoms of AIS during five consecutive months and in whom a CTP had been performed upon hospital arrival (Table 1). All patients with symptoms lasting less than 6 h were evaluated by the on-call neurologist and/or stroke neurologist and underwent routine stroke imaging protocol. Patients were treated according to standard institutional protocols, including intravenous or intra-arterial thrombolysis. This study was approved under an umbrella retrospective review of CT perfusion methodology by the institutional ethics committee.
| Patients (n = 42) | Age | Sex (M/F) | IV tPA | Mechanical | No tPA | Onset to CT (min) | Onset to therapy |
| No hemorrhage (27; 64.3%) | 70.1 ± 12.57 | 12/15 | 24 (88.9%) | 0 | 3 (11.1%) | 127 | 168 |
| Hemorrhage (15; 35.7%) | 69.9 ± 13.6 | 7/8 | 14 (92.9%) | 5 (33.3%) | 1 (6.7%) | 111 | 143 |
| P value | 0.89 | 0.83 | 0.7 | 0.07 |
During the study time period, 84 patients with symptoms of AIS received a CTP examination at admission. If tPA was then administered, a follow-up unenhanced CT was performed at 24 h. If tPA was deemed not clinically indicated, a follow-up CT was ordered at the neurologist’s discretion. Of these, a total of 42 patients received a follow-up CT, 32 patients were followed by magnetic resonance (MR), and the remainder received no follow-up. Within the group that received follow-up CT, there were 19 males and 23 females with an average age of 70.0 years (+ 12.9 year), ranging from 45 to 93 years old. Thirty-eight patients received IV thrombolytic therapy, five also received mechanical thrombus extraction, and four received neither treatment. Equal numbers of patients presented with symptoms on the left and right sides (17 and 18, respectively), six patients had transient ischemic attack, and one had cerebellar symptoms. In total, approximately one-third of the patients (n = 15) had intracranial hemorrhage.
All patients underwent a 9.6-cm coverage brain CTP protocol (80 kV, 100 mAs, 128 mm × 0.6 mm collimation, 9.6-cm scan volume in the Z-axis by using an adaptive spiral scanning technique (“shuttle mode”), CT dose index of 122.64 mGy, with 18 scans every 1.67 s, 5 scans every 3 s, and 4 scans every 15 s, resulting in a total scanning time of 105.06 s on the 128-section dual-energy CT scanner (Sensation Definition; Siemens Healthcare, Erlangen, Germany). A total of 40 mL of nonionic iodinated contrast media (iopamidol, Isovue-370; Bracco Diagnostic, Vaughan, Ontario, Canada) was injected at a rate of 5 mL/s, followed by a saline flush of 40-mL sodium chloride at 5 mL/s and a start delay of 5 s. Two sets of axial images with a section thickness of 1.5 mm for the computed tomography angiography (CTA) analysis and 5 mm for the perfusion analysis were reconstructed without overlap and sent to the Picture Archiving and Communication System (PACS). Sagittal and coronal multiplanar and maximum-intensity-projection images from the CTA data were reconstructed and also sent to the PACS. Perfusion analysis was performed with the vendor-supplied Neuro-VPCT software (Siemens Healthcare) based on the semiautomatic deconvolution algorithm “auto stroke”. Motion correction and bone segmentation were performed automatically. Automatic arterial and venous vessel identification, vessel segmentation threshold, and depiction of a healthy hemisphere for normalization were reviewed on all patient datasets by a single observer (AC). Gray-scale and colour-coded perfusion parameter maps for cerebral blood flow, cerebral blood volume, and time to peak were stored in a DICOM format.
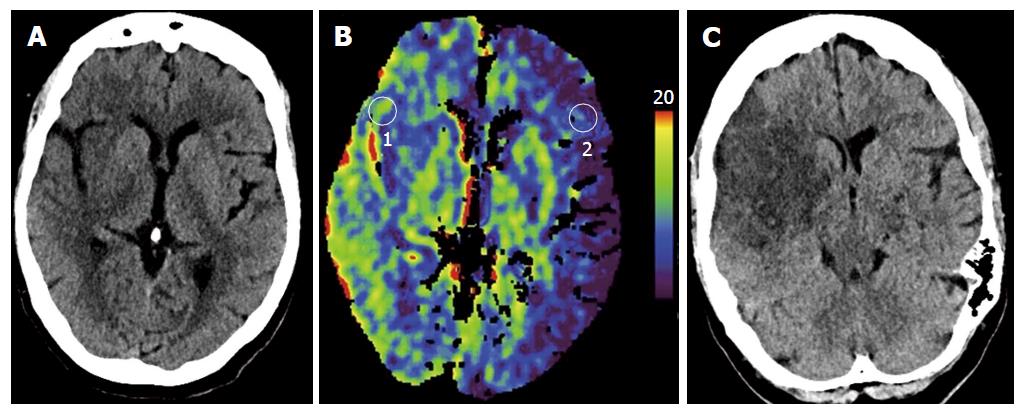
The PS was calculated for the side of the ischemia and/or infarction and for the contralateral unaffected side at the same level (Figure 1). The cerebral blood flow map was used to delineate the ischemic territory. Next, a region of interest (ROI) was drawn at the centre of this territory on the PS parametric map. Finally, a mirror ROI was created on the contralateral side at the same level. In cases of transient ischemic attack (n = 6) and cerebellar ischemia (n = 1), the ROI was placed over the basal ganglia and the affected and unaffected sides were compared. The PS scores were determined by the mean value within the ROI. The relative permeability-surface area product maps (rPS) acted as an internal control and was calculated as the ratio of the PS on the side of the AIS to the PS on the contralateral side.
For cases where intracranial hemorrhage occurred, one observer (JJSS), a fellowship-trained staff neuroradiologist, further classified the severity of the event. Events were classified as: (1) a petechial hemorrhage, which encompasses both the HI1 and HI2 (Hemorrhagic infarction) under the ECASS definition[12]; or (2) a more severe event with parenchymal hemorrhage, which includes both with and without mass effect. There was one case of subarachnoid hemorrhage, which was grouped together with parenchymal hemorrhage.
The data were arranged and analyzed using Excel (Microsoft Office 2007). The third author (JJSS) reviewed the statistical methods for this study. Patients were divided into two groups: Those who had and those who did not have hemorrhagic transformation. Quantitative variable results were expressed as means + standard deviations. Log conversion was used to convert the data into normal distribution to use t-test. A student t-test was performed to compare the degree of vascular permeability between the groups with and without hemorrhagic transformation. For the group of patients who experienced intracranial bleed, a student t-test was performed between those with only petechial hemorrhage and those with more severe parenchymal hematoma with subarachnoid hemorrhage. An alpha level of < 0.05 was considered significant. Next, a contingency table analysis of statistical measures including the sensitivity, specificity, positive and negative predictive values was derived.
The demographic information on our patients is summarized in Table 1. The average PS for the affected hemisphere in those who experienced any hemorrhagic transformation was not significantly (P = 0.26) higher (Mean + std: 3.06 + 1.81) compared to those who did not (2.47 + 1.75; Table 2). The average PS in the contralateral normal side was also not significantly different (P = 0.18) between those with hemorrhagic transformation (1.79 + 1.10) and those without (2.3 + 1.35; Table 2). The rPS derived using the normal side as the internal control was significantly higher (P = 0.003) in cases of hemorrhagic transformation (1.71 + 1.64) compared to those who did not have any (1.07 + 1.30; Table 2).
| Patients (n = 42) | Permeability surface area product | Relative permeability | ||
| Normal side | Affected side | P value | ||
| No hemorrhage (27; 64.3%) | 2.32 + 1.38 | 2.34 + 1.65 | 0.49 | 1.04 ± 0.53 |
| Hemorrhage (15; 35.7%) | 1.84 + 1.06 | 3.21 + 1.88 | 0.002 | 1.83 ± 0.78 |
| P value | 0.18 | 0.26 | 0.003 | |
Using the overall mean rPS of 1.3 as a cutoff, values above the threshold showed an increased likelihood of subsequent hemorrhagic transformation. The sensitivity of using this score to predict hemorrhagic transformation was 71.4, the specificity was 78.6, with a positive predictive value of 62.5 and negative predictive value of 84.6. The accuracy was determined at 76.2. The odds ratio of an event occurring with such an rPS was 9.2.
Of the 15 cases of hemorrhagic transformation, there was no statistically significant difference (P = 0.35) in the rPS between those with petechial or the more severe hemorrhagic events (Table 3).
| Patients (n = 15) | Permeability surface area product | Relative permeability | ||
| Normal side | Affected side | P value | ||
| Petechial hemorrhage (8; 53.3%) | 2.03 + 1.30 | 3.70 ± 2.28 | 0.02 | 1.78 ± 0.66 |
| Hematoma + SAH (7; 46.7%) | 1.61 ± 0.75 | 2.66 ± 1.23 | 0.06 | 1.89 ± 0.94 |
| P value | 0.92 | 0.74 | 0.35 | |
This retrospective study supports previous reports that showed a significant correlation between the measure of neurovascular injury (PS) and the propensity of patients to experience ipsilateral intracranial hemorrhage. In contrast to other studies, we did not find significantly increased permeability in the contralateral unaffected hemisphere. We postulate that because the average time from onset of symptoms to CT was well under 6 h, the inflammatory mediators and free radical products had not yet taken action on a global scale. Yang et al[13] showed also that the blood-brain barrier permeability was in the normal ranges for several hours after permanent middle cerebral artery occlusion and that BBB disruption occurs with late reperfusion. This is a global process and underscores the importance of using the contralateral PS as control.
Although PS has been shown here and elsewhere to be useful in predicting subsequent intracranial hemorrhage with relatively high specificity and sensitivity, it does not differentiate between mild petechial and the more severe parenchymal hemorrhagic events. A hemorrhagic event can range quite widely in the severity spectrum and can appear minor and asymptomatic with trivial hemorrhagic petechiae to large parenchymal hematoma with space-occupying effect. These imaging characteristics have been used as an indirect marker to predict the clinical outcome[14]. A post hoc analysis of the ECASS II data shows that only parenchymal hemorrhage affecting greater than 30% of the infarct and associated with mass effect leads to an early clinical deterioration and worsened long-term outcome, like death[11]. Thus, in practical terms, although the PS is quite good at evaluating the degree of blood-brain barrier damage that predisposes patients to further injury, it does not give clinicians a sense of who may proceed to catastrophic complication.
Ideally, a method would exist to, first, identify those who will develop symptomatic complications and to halt thrombolytic therapy in these patients. Second, the method would identify those who will develop only asymptomatic complications so that clinicians can extend thrombolytic therapy in this group, with the ultimate goal of individually customizing the time window for tPA administration. If PS cannot assess the true potential risk of thrombolytic therapy, we suggest that this method of stroke evaluation is not yet optimal for the treating physician. PS may prevent treatment in patients who may experience some minor petechial hemorrhage but, ultimately, can benefit from restoration of blood flow and recover from potential neurological deficits. Further research with a larger number of patients is required to develop more refined criteria that can help the treating clinician identify patients with potential serious hemorrhagic complications.
There are a few limitations to this study. First, only 42 of the 84 acute ischemic stroke patients received follow-up CT exam after therapy, which reduced the sample size and the statistical power associated with determination of severity. Second, this study focused solely on the CTP-derived PS. MR imaging has also been used to study blood-brain barrier breakdown and is superior for hemorrhage detection. In cases of acute stroke, however, it is often not feasible to obtain an MR exam within the treatment time window. Thus, development of an extended CT stroke protocol may be more practical in the acute setting because it is the modality of choice for the initial investigation.
Pre-treatment PS can predict the occurrence of hemorrhagic transformation in AIS patients with relatively high sensitivity, specificity, positive and negative predictive value. However, PS may not predict hemorrhagic transformation severity, which is critical in the decision to treat.
Hemorrhagic transformation is one of the most important complications following thrombolytic treatment of acute ischemic stroke (AIS). The ability to predict hemorrhagic complication at presentation can be useful to clinicians. Perfusion-derived permeability-surface area product maps (PS) have been suggested to be of utility in predicting hemorrhagic transformation. Herein, the authors aim to show whether PS can predict hemorrhagic transformation on follow-up. If so, can the magnitude of the score predict the event severity?
Previous reports showed a significant correlation between the measure of neurovascular injury (PS) and the propensity of patients to experience ipsilateral intracranial hemorrhage. They found that pre-treatment PS can predict the occurrence of hemorrhagic transformation in AIS patients with relatively high sensitivity, specificity, positive and negative predictive value.
Data from the computed tomography (CT) perfusion can be used to generate information on the permeability of the blood-brain barrier as a function of ischemia-related vascular injury. This extracted PS has been described by some studies as an independent predictor of future hemorrhagic transformation. Their results are consistent with those studies. However, PS may not predict hemorrhagic transformation severity, which is critical in the decision to treat.
This study suggests that PS is useful in predicting patient outcomes following AIS. However, the utility of PS is limited because it does not distinguish between mild petechial and the more severe parenchymal hemorrhagic events. If PS cannot assess the true potential risk of thrombolytic therapy, we suggest that this method of stroke evaluation is not yet optimal for the treating physician.
AIS: Acute ischemic stroke; PS: Permeability-surface area product maps; CTP: CT perfusion.
This article investigated the role of permeability-surface area product maps (PS) on CTP to predict HT in AIS patients. They concluded that pretreatment PS can predict the occurrence of HT on follow-up CT with reasonable accuracy. Overall it is a nicely written study.
P- Reviewer: Starke RM, Wang DJJ S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384:1929-1935. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1556] [Cited by in RCA: 1855] [Article Influence: 168.6] [Reference Citation Analysis (0)] |
| 2. | Balami JS, Chen RL, Grunwald IQ, Buchan AM. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333:1581-1587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8192] [Cited by in RCA: 8040] [Article Influence: 268.0] [Reference Citation Analysis (0)] |
| 3. | Balami JS, Chen RL, Grunwald IQ, Buchan AM. Neurological complications of acute ischaemic stroke. Lancet Neurol. 2011;10:357-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 174] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 4. | Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol. 2009;8:355-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1717] [Cited by in RCA: 1911] [Article Influence: 119.4] [Reference Citation Analysis (0)] |
| 5. | Souza LC, Payabvash S, Wang Y, Kamalian S, Schaefer P, Gonzalez RG, Furie KL, Lev MH. Admission CT perfusion is an independent predictor of hemorrhagic transformation in acute stroke with similar accuracy to DWI. Cerebrovasc Dis. 2012;33:8-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Wardlaw JM, Murray V, Berge E, Del Zoppo GJ. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev. 2009;CD000213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 163] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 7. | Heuschmann PU, Kolominsky-Rabas PL, Misselwitz B, Hermanek P, Leffmann C, Janzen RW, Rother J, Buecker-Nott HJ, Berger K; German Stroke Registers Study Group. Predictors of in-hospital mortality and attributable risks of death after ischemic stroke: The German Stroke Registers Study Group. Arch Intern Med. 2004;164:1761-1768. [PubMed] |
| 8. | Berger C, Fiorelli M, Steiner T, Schäbitz WR, Bozzao L, Bluhmki E, Hacke W, von Kummer R. Hemorrhagic transformation of ischemic brain tissue: asymptomatic or symptomatic? Stroke. 2001;32:1330-1335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 358] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 9. | Adams HP, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115:e478-e534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 693] [Cited by in RCA: 678] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 10. | Hom J, Dankbaar JW, Soares BP, Schneider T, Cheng SC, Bredno J, Lau BC, Smith W, Dillon WP, Wintermark M. Blood-brain barrier permeability assessed by perfusion CT predicts symptomatic hemorrhagic transformation and malignant edema in acute ischemic stroke. AJNR Am J Neuroradiol. 2011;32:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 129] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 11. | Aviv RI, d’Esterre CD, Murphy BD, Hopyan JJ, Buck B, Mallia G, Li V, Zhang L, Symons SP, Lee TY. Hemorrhagic transformation of ischemic stroke: prediction with CT perfusion. Radiology. 2009;250:867-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 12. | Trouillas P, von Kummer R. Classification and pathogenesis of cerebral hemorrhages after thrombolysis in ischemic stroke. Stroke. 2006;37:556-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 183] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 13. | Yang GY, Betz AL. Reperfusion-induced injury to the blood-brain barrier after middle cerebral artery occlusion in rats. Stroke. 1994;25:1658-1664; discussion 1664-1665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 249] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | Molina CA, Alvarez-Sabín J, Montaner J, Abilleira S, Arenillas JF, Coscojuela P, Romero F, Codina A. Thrombolysis-related hemorrhagic infarction: a marker of early reperfusion, reduced infarct size, and improved outcome in patients with proximal middle cerebral artery occlusion. Stroke. 2002;33:1551-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 184] [Article Influence: 8.0] [Reference Citation Analysis (0)] |