INTRODUCTION
Today, most of clinical positron emission tomography (PET) scanners are sold as integrated PET-computer tomography (CT) units. The integrated CT data allow correct co-registration and fused imaging of anatomical and functional data. CT scan acquisition (transmission scan) is also used for attenuation correction of positron photon annihilation from radiotracer (18F) fluorodeoxyglucose (FDG). CT imaging in an integrated PET-CT scanner significantly decreases false positive results and improves specificity of the study in PET interpretation[1-3]. The advantage of PET/CT over PET alone can be attributed to the low anatomic resolution of PET and difficulty in lesion localization on PET[4,5].
Corresponding to abnormal FDG uptake on a whole body FDG PET/CT, a visible lesion or abnormality is often identified on the integrated CT in the same location. This co-registration of anatomic and functional imaging greatly increases confidence of nuclear radiologists in PET interpretation. Sometime, misalignment between PET and CT images may be present, usually resulting from either repositioning of the patient or the time interval between two scans for CT and PET[6]. The misalignment or mis-registration of PET and CT images is often noted in the lower thorax and upper abdomen, because of changes of organ positions during different breathing cycles between CT and PET acquisitions[7]. In general, this kind of PET/CT misalignment artifact can be solved without many difficulties in interpretation by checking adjacent upper and lower levels of the CT or PET slices when a FDG focus or CT lesion is identified.
It is not uncommon that markedly abnormal focal uptake is noted on FDG PET but no anatomic counterpart is visualized on the CT, which is bizarre and poses a dilemma in interpretation about the nature of uptake. Focal pattern and increased intensity of uptake can not be simply ignored or considered as an artifact in these cases. On the other hand, a diagnosis of the pathologic finding cannot be made with a lack of corresponding CT abnormality. What is this kind of hot spot? In this paper, we outline some common locations of abnormal focal uptake with the absence of corresponding CT finding on a whole body FDG PET-CT imaging. We also briefly discuss the interpretative pitfalls.
MOST COMMONLY SEEN FOCAL FLUORODEOXYGLUCOSE UPTAKE WITHOUT COMPUTER TOMOGRAPHY ABNORMALITY
Vocal cord uptake
Physiologic uptake in the vocal cords is mostly seen as symmetric. In some patients with known primary or metastatic malignancy of the head and neck, focal intense uptake may be noted in the unilateral true vocal cord, with no lesion or abnormality on CT images. In general, this uptake is secondary to the increased compensatory metabolic activity of the muscle in a normal true vocal cord responsible for the contralateral vocal cord paralysis as a result of damage or palsy of the recurrent laryngeal nerve (Figure 1). Lee et al[8] reported that all 15 patients with one-sided vocal cord uptake on FDG-PET had contralateral vocal cord paralysis on laryngoscopic examination. Therefore, when asymmetric intense uptake is seen in the unilateral vocal cord and no discrete lesion is appreciated on CT, clinical correlation including laryngoscopic examination is helpful to verify the nature of uptake.
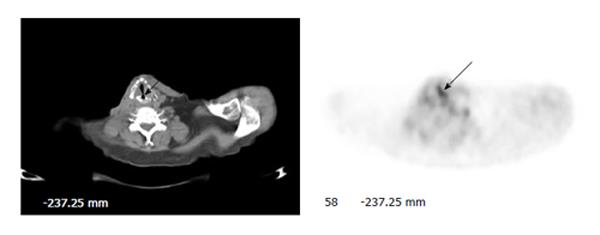
Figure 1 Unilateral vocal cord uptake.
A 59-year-old man with history of transglottic squamous cell carcinoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the neck shows intense unilateral uptake without a visible lesion on CT in the left true vocal cord (arrows). Subsequent laryngoscopic examination revealed paralysis of the right vocal cord.
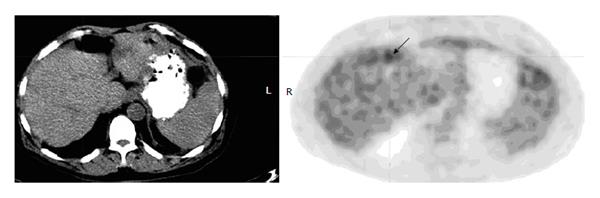
Iatrogenic uptake in the lung
Unlike other tissues or organs, normal lung parenchyma does not demonstrate notable FDG uptake on PET. Sometimes mild vague uptake may be noted in the vascular structures of the lungs. Evident FDG uptake in the lungs is always associated with abnormalities on CT, for example, nodule or mass, opacity or density, infiltrate, consolidation, etc. Abnormal uptake in the lung bases with no lung abnormality on CT may actually represent a lesion in the upper abdomen, for example the liver or spleen, because of mis-registration of PET and CT images secondary to the patient’s respiratory motion. But a real focus may be identified in any area of the lung without a visible corresponding abnormality on lung window of the CT (Figure 2).
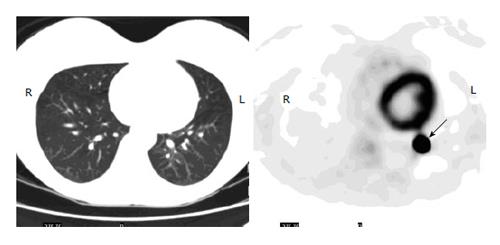
Figure 2 Iatrogenic uptake in the lung.
A 35-year-old woman with history of low grade serous ovarian cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Axial PET image of the lungs shows a focus of intense uptake in the left lower lobe (arrow), but no nodule or lesion is seen on CT. Subsequent diagnostic CT was negative as well for lung nodule. The uptake is likely secondary to microembolism due to a paravenous injection.
There are a few case reports in recent years about iatrogenic focal FDG accumulation in lung parenchyma without abnormal CT findings[9-12]. Observed foci in the lung parenchyma were in different areas with variable intensity of uptake, but they were typically peripheral in the location and very intense in uptake. A common characteristic in the most cases was partial paravenous injection of the radiotracer. A possible and the most likely explanation for these iatrogenic foci in the lungs could be micro-emboli secondary to paravenous injection. The damage to the vein endothelium during paravenous injection causes the formation of blood clots at the site of injury, which in turn detach from the vein, enter the small pulmonary vasculature and are seen as hot spots in the distal lung.
Axillary uptake
Although less reported, it is relatively common that small ipsilateral axillary lymph nodes, draining the region of tracer extravasation in the antecubital injection, demonstrate significant uptake on FDG-PET due to extravasation or partial subcutaneous injection[13]. The findings between PET and CT images are often discordant in the ipsilateral axilla following an infiltrated injection: small or no lymph node on CT, but intense uptake on PET (Figure 3). An interpretation of lymphadenopathy, especially metastasis, should be avoided in this situation when an infiltrated injection is present in the ipsilateral arm. In the most cases, the artefactual axillary lymph node uptake can be identified when linear superficial uptake in the ipsilateral arm is seen from the injection site to the axilla. To avoid confusion in interpretation of PET imaging for the breast, lung or chest wall lesion, the radiotracer should be always administered at the contralateral arm.
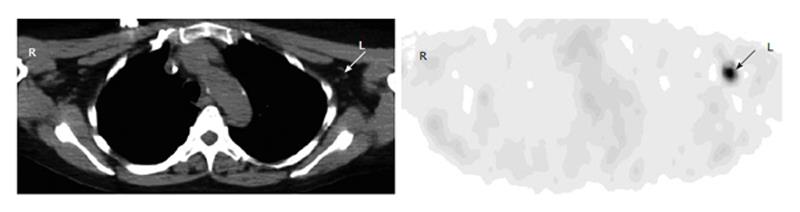
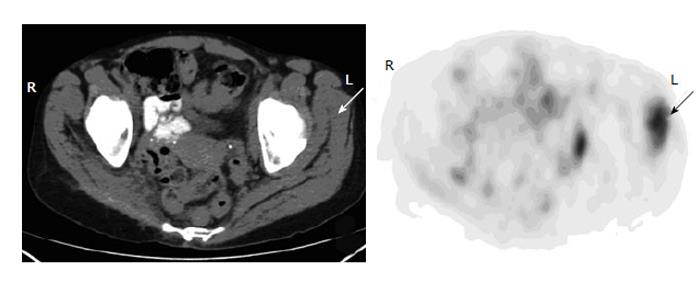
Figure 3 Axillary uptake.
A 63-year-old man with history of bladder cancer had fluorodeoxyglucose (FDG) positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the upper chest shows focal uptake in the left axilla (arrow). Corresponding to this focus, there is a small benign lymph node with fat lumen on CT (arrow). The uptake is secondary to infiltration of injected FDG at the antecubital site.
Noise uptake in the liver
Normal uptake of the liver is often inhomogeneous because of a relatively high and variable glucose-6-phosphatase activity. In our experience, so-called “noise artifact” in the liver on FDG-PET is not uncommon in a whole body imaging. Typically, this kind of noise artifact is displayed as ill defined, mildly increased uptake on PET without anatomic abnormality on CT (Figure 4). However, sometimes a discrete focus without corresponding CT abnormality may also represent the noise artifact in the liver. When a discrete focus is seen in the liver with the absence of a lesion on CT imaging of integrated PET/CT, a diagnosis can not be made about hepatic pathology; on the other hand, caution should also be exercised to exclude a lesion based on a negative finding on an integrated CT imaging only, because small hepatic lesions are often not well appreciated on the low dose, non-contrast CT. A diagnostic CT or magnetic resonance imaging (MRI) is necessary for correlation.
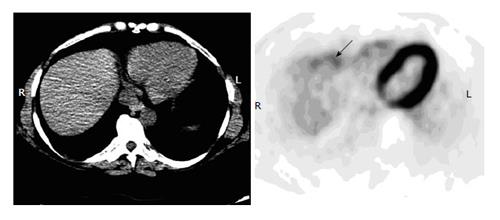
Figure 4 Noise artifact in the liver.
A 42-year-old man with history of cervical cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Axial PET image of the upper abdomen shows irregular uptake in the anterior margin (arrow) but without discrete lesions on an integrated CT, representing noise artifacts. Subsequent diagnostic CT was negative.
Increased hepatic uptake may be also seen on the anteromedial or posteromedial margin of the liver and adjacent to the hepatic flexure colon. If there is no corresponding hepatic lesion is identified on the CT, the uptake may represent colonic activity especially when the uptake is linear (Figure 5). Mal-location of the bowel uptake is due to patient’s motion or respiratory effect. The coronal and sagittal views are helpful to confirm the findings.
Figure 5 Colonic uptake abutting the margin of the liver.
A 59-year-old man with newly diagnosed pancreatic cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for staging. Axial PET image of the upper abdomen shows a small focus of increased uptake abutting the anterior margin of the liver (arrow). But there is no visible hepatic lesion on the integrated CT. A magnetic resonance imaging was also negative for any lesion in the liver. The uptake is from the adjacent transverse colon with slight motion artifact and mis-registration of PET and CT images.
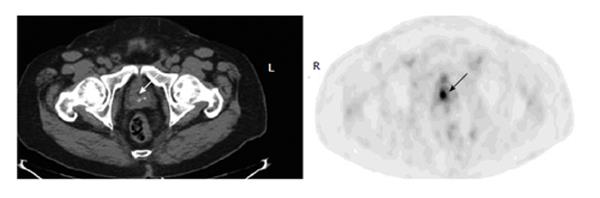
Focal urine activity
Focal urine activity in the ureter is easily identified by identifying the ureter on the integrated CT. Although some authors recommended re-acquisition following furosemide administration[14,15], it is not necessary in our experience. A focus in the urethra is more challenging in interpretation, especially in the prostatic urethra. For patients with prior trans-urethral resection of prostate, a focus is often seen in the dilated prostatic urethra, representing urine activity (Figure 6). If a focus is noted inferior to the urinary bladder and at the midline of the prostate, and no corresponding lesion is identified on CT, it is most likely urine activity as well, even though low density urine can not be seen on CT. In contrast, a real prostate lesion is often seen as either calcified or low density area with focal uptake in the peripheral prostate, rather than at the midline and location of the prostatic urethra (Figure 7).
Figure 6 Urine activity in the prostatic urethra.
A 65-year-old man with history of lung cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the lower pelvis shows a focus at the midline of the prostate, corresponding to the dilated urethra on CT (arrows). The finding represents urine retention in the urethra of previous trans-urethral prostate resection site.
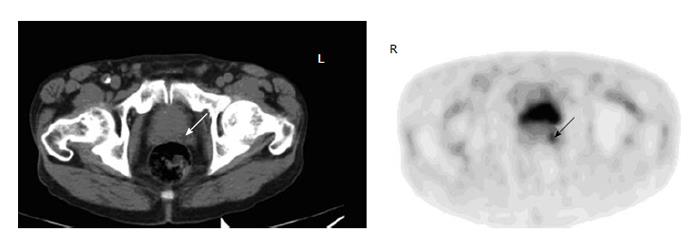
Figure 7 Uptake of prostate cancer.
A 63-year-old man with history of laryngeal cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging Axial PET image of the lower pelvis shows a focus corresponding to a hypodensity lesion on the CT in the left peripheral prostate (arrows). Biopsy confirmed prostate cancer.
Atypical brown fat or muscle uptake
Brown fat uptake is well known on FDG-PET, and is easily identified in well-defined patterns in the most cases. The most common location for brown fat is the neck and supraclavicular area, which is usually bilateral, linear or curvilinear[16-18]. Focal uptake of brown fat is often seen in the mediastinum, axillae, paravertebral areas and intercostals spaces[17,18]. However, brown fat uptake may be encountered anywhere as a focus or separate foci[19]. When focal uptake is seen on PET corresponding to “dark” low density rather than soft tissue on the integrated CT, it represents brown fat (Figure 8). HU measurement can be confirmative, fat tissue usually ranges -50 to -150 HU. A pitfall to identify brown fat uptake is to be aware of motion artifact or mismatch of PET and CT images. When a focus of uptake corresponds to low density fat on CT, it is always a good practice to carefully check the adjacent structures or tissues and exclude a real lesion on the CT images.
Figure 8 Focal brown fat uptake.
A 50-year-old woman with history of metastatic breast cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image shows a focus in the left supraclavicular region (arrow). On the integrated CT, there is no node or lesion except for fat tissue in this location. The uptake is from the brown fat.
Muscular uptake is often seen in anxious patients or due to stress induced muscle tension or secondary to motion after the FDG injection. Usually benign muscular uptake can be distinguished from malignant or metastatic disease due to its mostly symmetric pattern that matches the anatomy of the muscular groups, and the absence of a lesion on the integrated CT images. However, focal intense muscular uptake may be also seen with no corresponding CT lesion or abnormality (Figure 9). Whereas the uptake is mostly benign, further correlation with a MRI may be necessary because of limited value of the integrated CT for muscular pathology.
Figure 9 Muscular uptake.
A 45-year-old woman with history of leiomyosarcoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET-CT images of the pelvis show intense focal muscular uptake in the left gluteus maximus, gluteus minimus and obturator intermus, with no corresponding lesions on the CT (arrows). Two subsequent magnetic resonance images were unremarkable of the muscles.
Real lesion not seen on CT
Focal FDG uptake without a visible corresponding lesion on CT does not always indicate benign nature or an artifact. Caution should be exercised in some structures or tissues for example the gastrointestinal tract. The pattern rather than the intensity of uptake is more important in interpretation of the gastrointestinal tract. Physiologic or inflammatory uptake of the gastrointestinal tract is often diffuse and linear. Focal increased uptake may be frequently seen and mostly benign in some areas such as the gastroesophageal junction (Figure 10), the gastric wall, the rectal ampulla or the anal canal[20]. Less commonly seen focal uptake without a lesion on CT in the colon is most likely benign in nature as well, but a neoplasm should be excluded with colonoscopy since a small or superficial lesion may be not well appreciated on CT. Compared to that in the stomach and colon, focal uptake in the esophagus more likely represents a neoplastic process because physiologic esophageal uptake is very mild and linear, even though the integrated or diagnostic CT does not demonstrate discrete lesion or wall thickening (Figure 11). Endoscopic examination and biopsy may be warranted to diagnose or exclude an esophageal lesion if a discrete focus is noted on the esophageal wall. The false negative CT may be resulted from a small size of the tumor, lack of a discrete mass or mass effect and suboptimal sensitivity of CT for esophageal pathology due to poor distensibility of the esophagus[21].
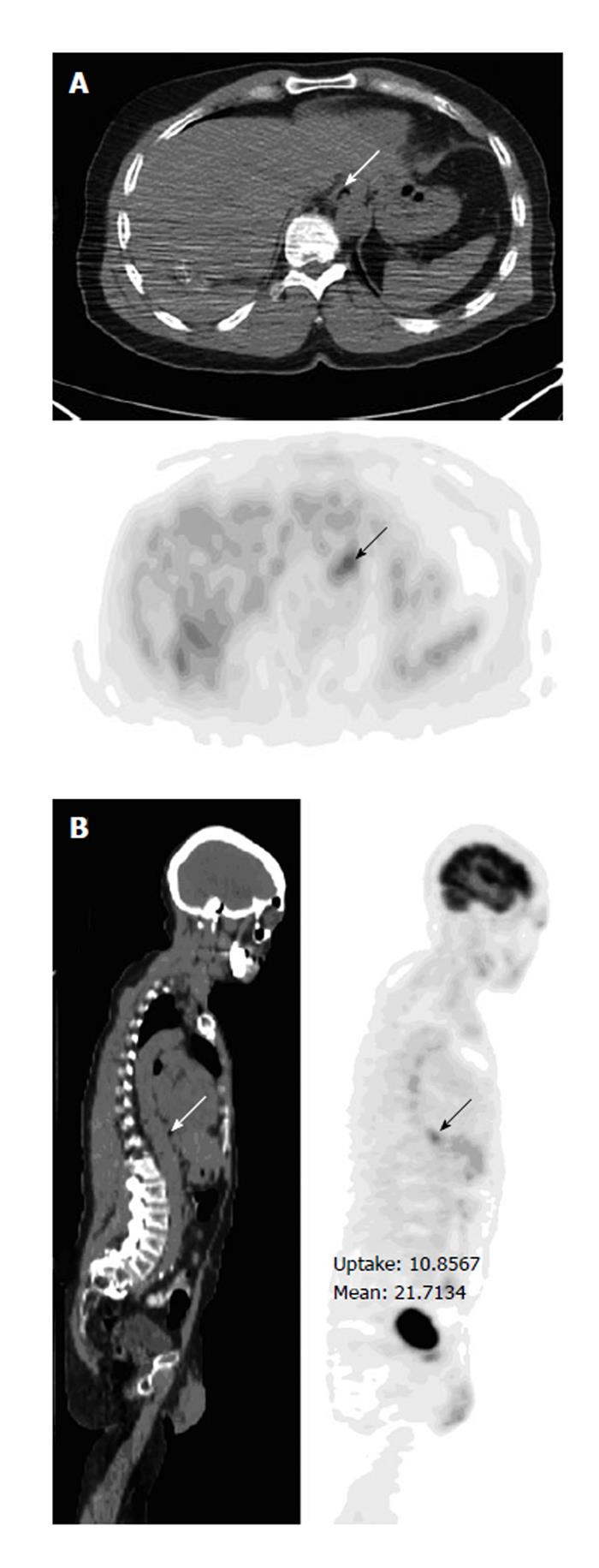
Figure 10 Prominent uptake in the gastroesophageal junction.
A 57-year-old man with history of osteosarcoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Axial (A) and sagittal (B) PET-CT images show focal uptake in the gastroesophageal junction (arrows), with no lesion on CT and stable over two years on follow-ups.
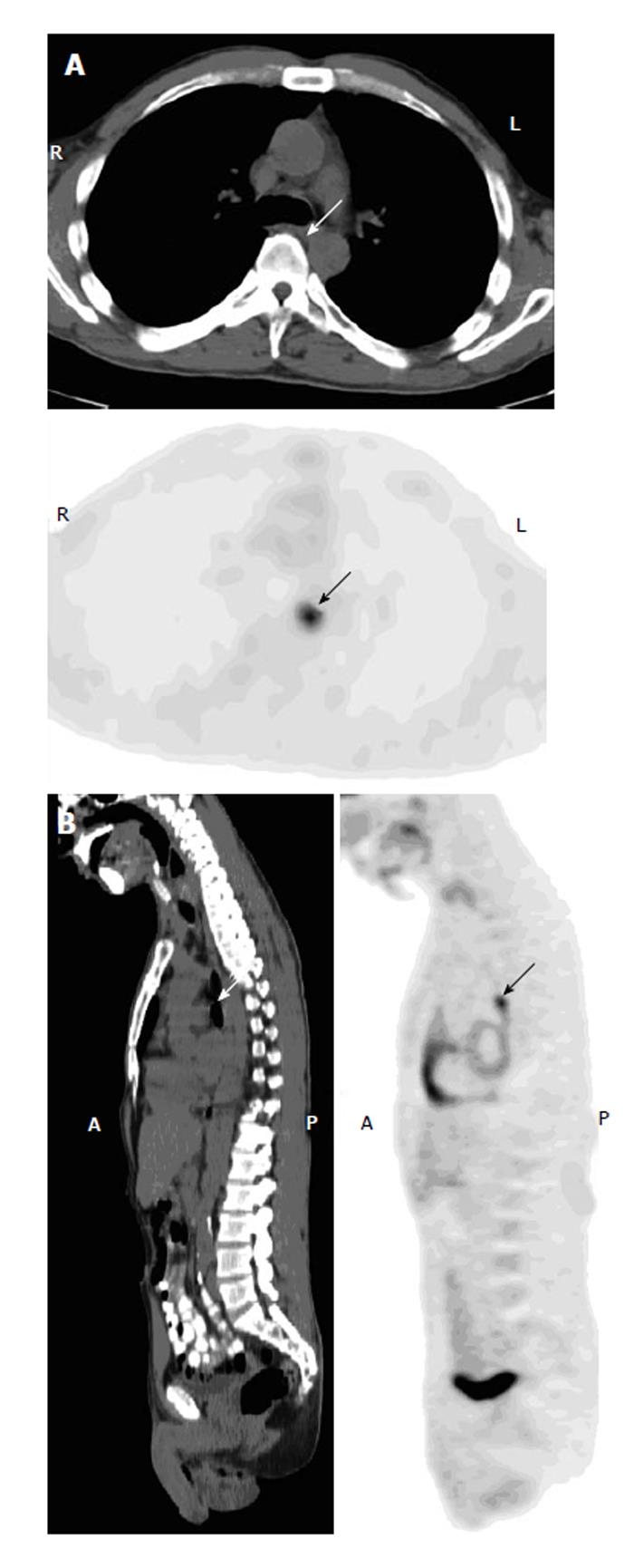
Figure 11 Uptake representing esophageal cancer.
A 49-year-old man with history of retromolar carcinoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial (A) and sagittal (B) PET-CT images show a focus in the mid esophagus at the subcarinal level (arrows), without a visible lesion or evident wall thickening on the integrated CT. Subsequent contrast CT was negative as well. An endoscopic biopsy revealed squamous cell carcinoma.
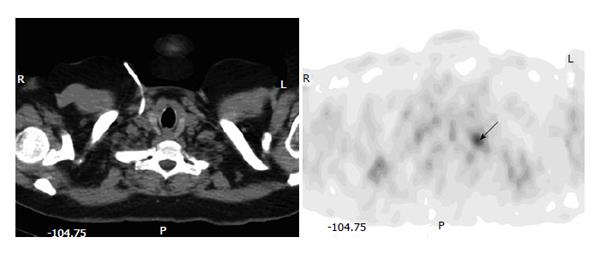
Focal osseous uptake is often seen on PET imaging with the absence of CT abnormality on bone window. Although a sclerotic or lytic bone lesion demonstrating abnormal FDG uptake is almost certainly diagnosed as a neoplasm or metastasis in an oncologic patient, focal uptake without a visible lesion on the integrated CT is potentially problematic in PET interpretation. Taira et al[22] reported that discordant findings between the PET and CT occurred in more than half of the bone lesions. While a CT noted osseous lesion lacking FDG uptake is most likely a benign or treated disease, abnormal osseous uptake with the absence of a lesion on CT more likely represents a metastasis[22,23]. When the examinations are discordant, PET is far more accurate than CT in the characterization of bone lesions[22,24]. In our experience, mild vague uptake may be secondary to some benign etiologies for example degenerative disease, but significant focal uptake in the bone is highly suspicious for metastatic disease in a patient with known malignancy even though the CT is negative (Figure 12). In addition, positive predictive value is significantly greater when multiple foci are seen in the bones compared to one solitary focus. It is not uncommon that in the cases with multiple osseous metastases, many foci of uptake have no discrete lesions on the integrated CT, because the metabolic change often precedes the anatomic change.
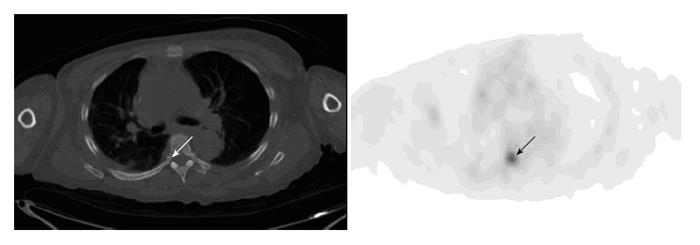
Figure 12 Osseous uptake.
A 55-year-old woman with history of metastatic breast cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the chest shows focal uptake at the right pedicle of the T6 (arrow). There is no visible corresponding bone lesion on the integrated CT (arrow). Repeat PET-CT three months after shows multiple bone metastases including worsening uptake in the right-sided T6.
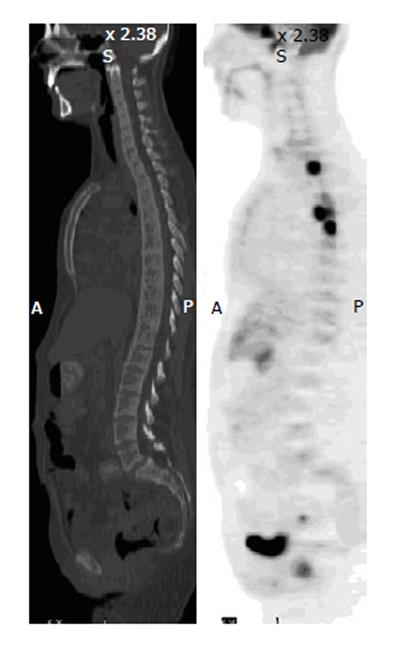
In lymphomatous disease of the bones, PET and CT findings may be discordant: intense FDG uptake but without significant CT abnormality on bone window (Figure 13). On CT, Bone lymphoma often demonstrates a permeative pattern with periosteal reaction, sequestra and absence of cortical destruction[25,26]. Therefore, early lymphomatous bone involvement or small bone lesions without marked bone destruction may only be visualized as increased FDG uptake on PET imaging only. In disseminated lymphomatous disease, FDG PET often reveals more osseous lesions than CT imaging.
Figure 13 Lymphomatous disease of bone.
A 28-year-old man with disseminated B-cell lymphoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Sagittal PET image shows foci of intense uptake in the vertebral bodies of the upper thoracic spine, but the CT is unremarkable in the corresponding sites. Repeated scan 3 mo after chemotherapy demonstrate resolution of uptake in the bones as well as lungs and lymph nodes.