Published online Sep 28, 2024. doi: 10.4329/wjr.v16.i9.466
Revised: August 7, 2024
Accepted: August 28, 2024
Published online: September 28, 2024
Processing time: 103 Days and 15.4 Hours
Primary hyperparathyroidism is typically caused by a single parathyroid adeno
The patient had a history of parathyroidectomy 10 years prior but developed recurrent hyperparathyroidism with symptoms of pruritus and cough with sputum during a period of routine dialysis. Radiographic imaging revealed multiple nodules in both lungs, with the largest measuring approximately 1.35 cm. Surgical histopathology confirmed the presence of hyperplastic parathyroid glands within the pulmonary tissue. After tumor resection surgery via video-assisted thoracic surgery with wedge resection, the patient was discharged in stable condition and in follow-up her symptoms showed improvement.
This article describes hyperparathyroidism presenting as pulmonary nodules in a patient undergoing post-parathyroidectomy HD, highlighting diagnostic challenges and a positive outcome from tumor resection surgery.
Core Tip: This case highlights a rare occurrence of hyperplastic parathyroid gland seeding in pulmonary tissue in a patient with end-stage renal disease and recurrent hyperparathyroidism. The study underscores the diagnostic challenge posed by atypical presentations of hyperparathyroidism in patients undergoing dialysis, emphasizing the crucial role of comprehensive imaging and histopathological examination. Surgical resection proved effective in alleviating symptoms, suggesting its therapeutic utility in managing such complex cases. Further research is needed to refine management strategies and improve outcomes for similar clinical scenarios.
- Citation: Chiang PH, Ko KH, Peng YJ, Huang TW, Tang SE. Hyperparathyroidism presented as multiple pulmonary nodules in hemodialysis patient status post parathyroidectomy: A case report. World J Radiol 2024; 16(9): 466-472
- URL: https://www.wjgnet.com/1949-8470/full/v16/i9/466.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i9.466
There are many conditions that can cause hyperparathyroidism. In primary hyperparathyroidism, 85% of cases are caused by a single parathyroid adenoma[1] and are almost always due to benign overgrowth of parathyroid tissue as a single gland (80% of cases) or as a multiple gland disorder (15%-20% of cases)[2]. Ectopic parathyroid adenomas are occasionally found in the mediastinum (28% paraesophageal, 26% in the mediastinum, 24% intrathymic, 11% intrathy
Herein, we describe a rare case of a patient undergoing hemodialysis (HD) who was diagnosed with hyperparathyroidism presenting as multiple pulmonary nodules.
A 50-year-old female patient presented with complaints of itchy skin and cough with sputum experienced during routine HD.
The symptoms of itching skin and cough with sputum had persisted for several months during the routine HD treatment for pre-existing severe renal failure due to chronic kidney disease, which had been diagnosed decades previously with dialysis initiated in 1987. The persistence of these symptoms had caused her to seek help at our thoracic medicine outpatient department. A chest x-ray taken at admission revealed bilateral opacities over her lungs, prompting admission for further evaluation and treatment.
The patient had a decades-long history of hypertension (the precise start-date was lost to time) and end-stage renal disease which initiated in 1987. She developed tertiary hyperparathyroidism post-parathyroidectomy under regular HD.
The patient reported no abnormal past medical or family history.
Skin turgor was normal with no skin rash or ecchymosis. There was no jugular vein engorgement, lymph node enlargement, or palpable goiter in the neck region. Lung inspection showed symmetrical and full expansion with bilateral rales detected on auscultation but no wheezing. Overall, no abnormal findings were noted upon physical examination at admission.
The complete blood count and differential blood count results were normal. Other relevant blood tests revealed the following abnormal results: (1) Creatinine at 8.4 mg/dL (normal range: 0.5-0.9 mg/dL); (2) Serum parathyroid hormone at 1891 pg/mL (normal range: 10-69 pg/dL); and (3) Calcium at 10.3 mg/dL (normal range: 8.6-10.2 mg/dL). The following tests were performed and results were found to be in the normal range: (1) Thyroid stimulating hormone at 0.49 IU/mL (normal range: 0.25-5.00 IU/mL); (2) Free-T4 at 1.12 ng/mL (normal range: 0.89-1.78 ng/mL); and (3) Thyroglobulin at 20.06 ng/mL (normal range: 0-25.00 ng/mL). These results indicated that the patient had hyperparathyroidism, though the underlying cause had yet to be determined.
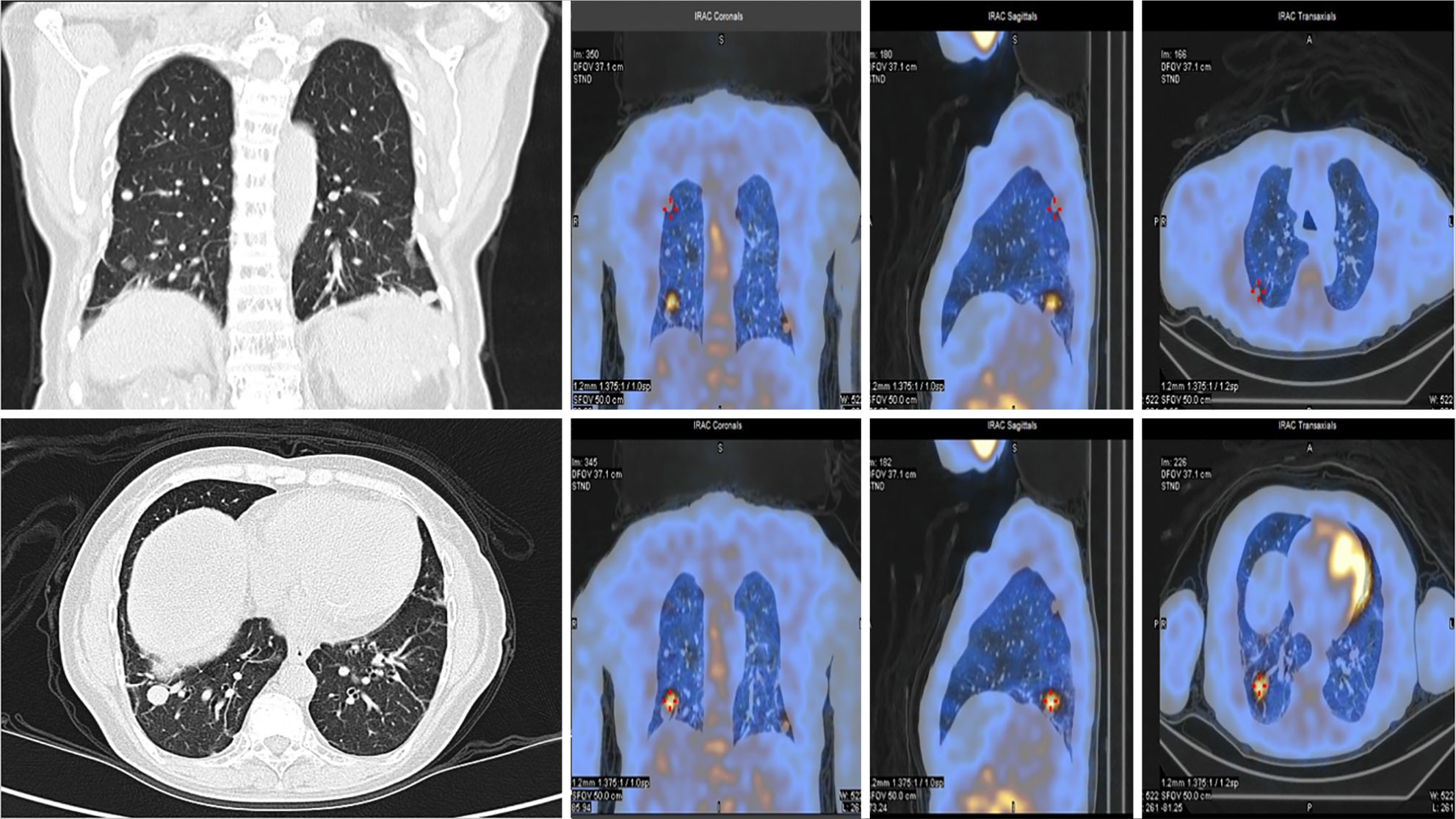
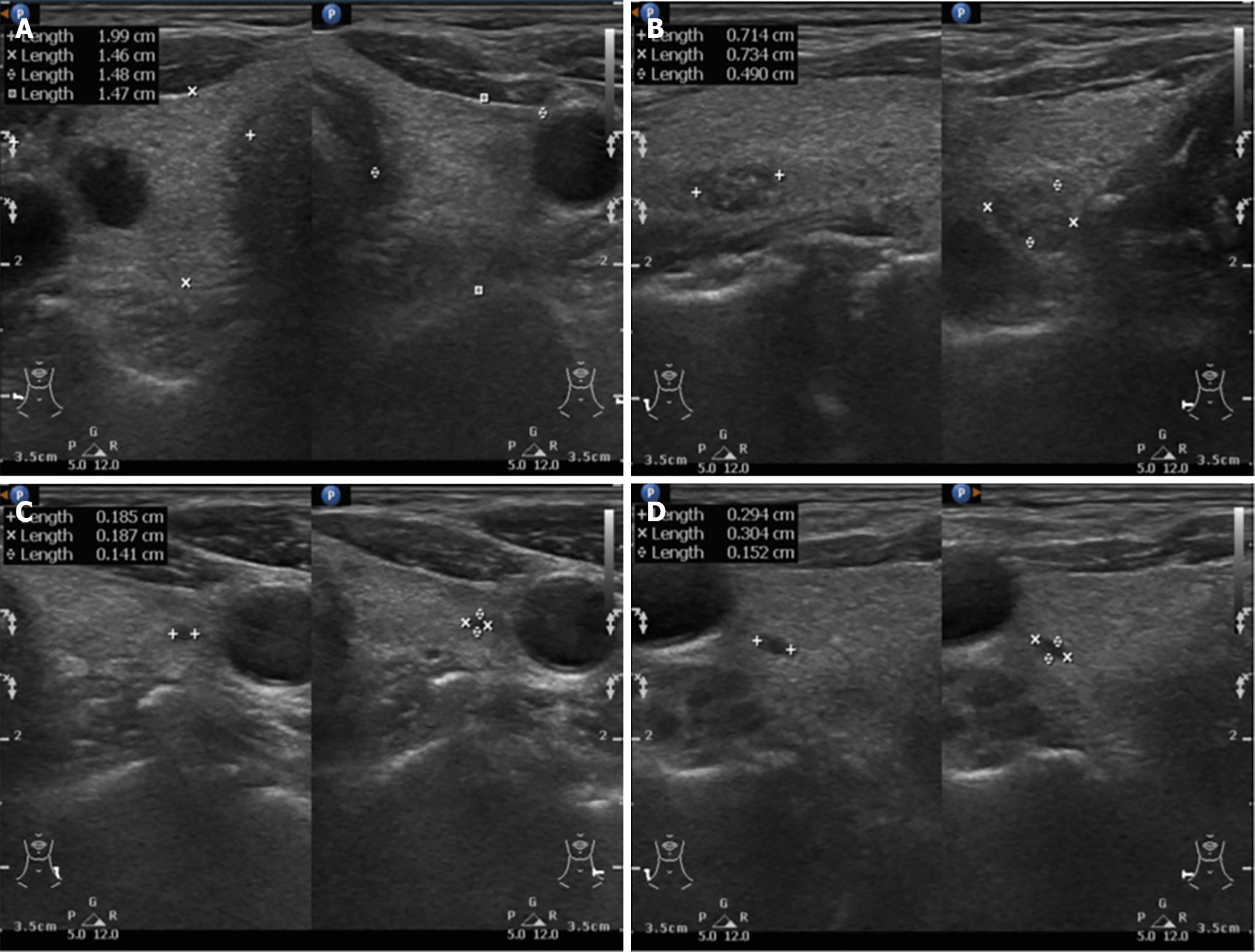
The chest x-ray revealed several bilateral opacities in the lungs. A contrast-enhanced computed tomography (CT) scan of the chest identified multiple nodules in both lungs, with the largest nodule measuring approximately 1.35 cm (Figure 1). A methoxyisobutyl-isonitrile (MIBI) scan was performed and did not reveal any significant abnormalities except for the presence of multiple pulmonary nodules with dominant MIBI uptake in the lung regions (Figure 1). These findings suggested the possibility of pulmonary malignancy or metastases. A neck ultrasound revealed a normally sized thyroid gland with a multinodular goiter (Figure 2). A CT scan of the neck did not clearly identify the parathyroid glands.
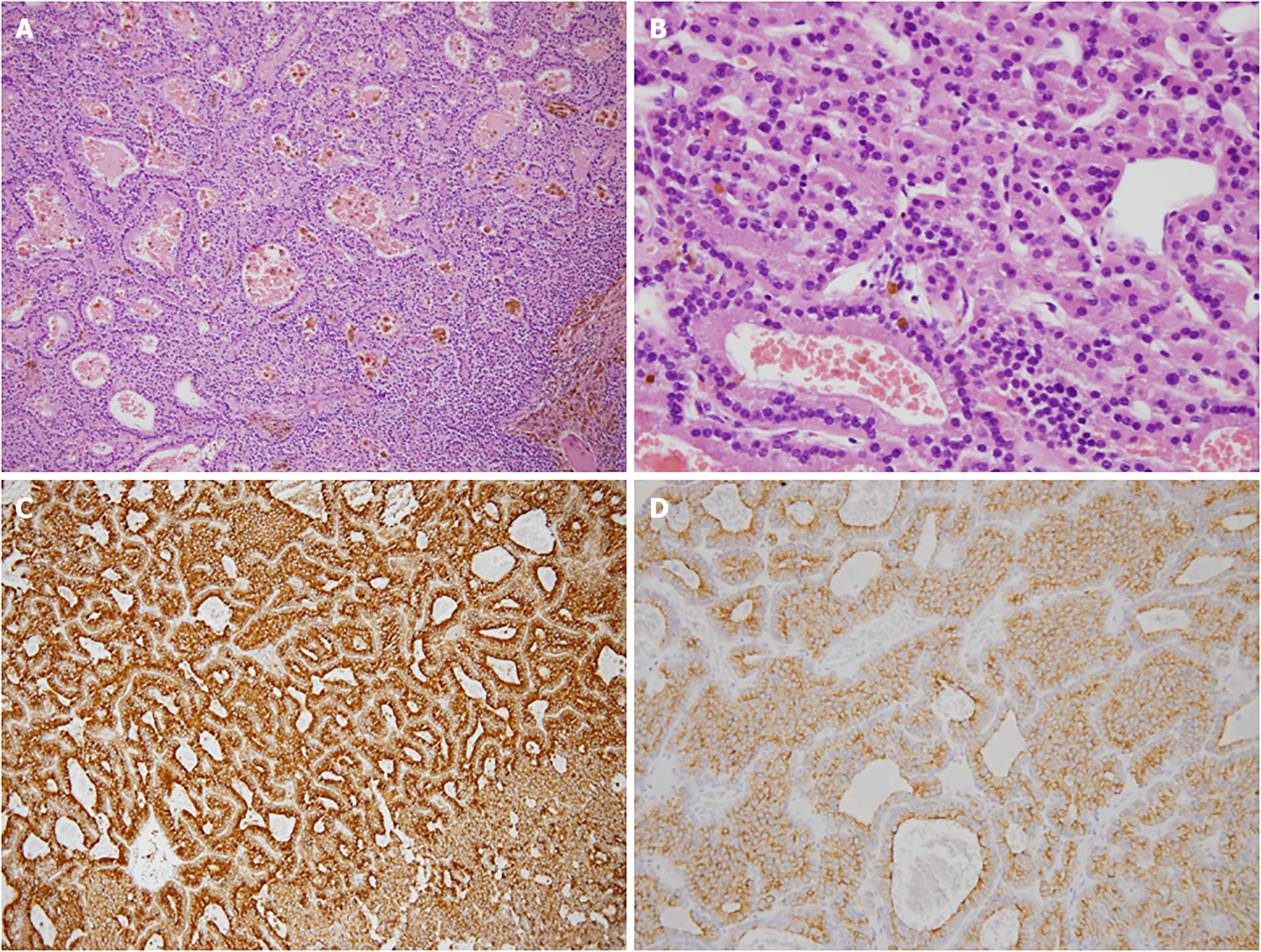
The tentative diagnosis was multiple pulmonary nodules in bilateral lungs with the nature of the nodules unknown (Figure 3). Surgical intervention was required to obtain pathological evidence to inform the final diagnosis. After surgery, the final diagnosis was hyperparathyroidism presenting with multiple pulmonary nodules.
Video-assisted thoracic surgery [commonly referred to as video-assisted thoracic surgery (VATS)] with wedge resection was performed on the right side to remove the ectopic hyperplastic parathyroid gland tissue and to obtain samples for diagnosis. After the two nodules were resected from the right side, the one nodule on the other side was left intact.
At 14 days after surgery, the patient was discharged from the hospital in stable condition. The 14-day postoperative recovery was favorable with a noticeable improvement in symptoms, which continued throughout the 3 years of follow-up. Surgical intervention allowed for the acquisition of valuable tissue samples that contributed to the final diagnosis and management of her condition. The patient was advised on follow-up care (wound care) and monitoring (outpatient department blood exams) to ensure continued recovery and to address any further needs as part of her treatment plan.
Before surgery, imaging studies were conducted to locate the lesion. A chest x-ray revealed multiple nodules in the lung area, with the largest measuring approximately 1.35 cm. These nodules appeared round and well-defined. Additionally, 99mTc-MIBI scintillation scans indicated the accumulation of radioactive isotopes in the suspected right lower lobe lung tumor (Figure 1). Previous studies demonstrated that some lesions such as primary lung cancers show an accumulation of MIBI[5,6], and others have suggested that 99mTc-MIBI could be useful to differentiate between benign and malignant lesions for solitary pulmonary nodules[7,8]. Under the impression that the patient had multiple pulmonary bilateral nodules in the lungs, we arranged VATS with wedge resection of the right lung for pathological confirmation and to remove the nodule tissue. Surprisingly, the postoperative pathological results were hyperplastic parathyroid gland with pulmonary seeding. Within 14 days after the operation, the patient’s symptoms subsided.
Differential diagnosis included ectopic parathyroid glands and malignant carcinoma. However, ectopic adenomas are usually located in the paraesophageal area or mediastinum as a single lesion[9]. To the best of our knowledge, there are only a few reports of ectopic parathyroid glands in lung tissue[9]. However, it is difficult to make a precise pathological distinction between benign and malignant parathyroid tumors by microscopic appearance alone. To distinguish between malignant and benign parathyroid nodules, the proliferation marker Ki-67 is widely used in pathology laboratories. A labeling index > 5% indicates an increased risk for malignancy, as Ki-67 expression is significantly higher in carcinomas than in adenomas and hyperplasia[10]. In this case, the labeling index was < 2%, and we did not identify any significant nuclear atypia or surrounding tissue invasion. Taken together, our findings indicated that the nodules were benign. While not performed in our case, additional tests have been suggested to distinguish between benign and malignant parathyroid tumors. For example, telomerase reverse transcriptase (hTERT) expression is uniquely limited to parathyroid carcinoma and not observed in benign tumors[11]. Therefore, it is possible that immunostaining against hTERT could distinguish parathyroid carcinoma from benign tumors[11]. Moreover, immunohistochemistry for parafibromin or sequencing of the CDC73 gene can distinguish parathyroid carcinoma from benign tumors. However, these tests are not widely performed in clinical practice and cannot alone be recommended as a definitive screening method for parathyroid malignancy. Therefore, a clinical analysis is essential to interpret potential malignancy.
Hyperparathyroidism is characterized by excessive production of parathyroid hormone, which results in elevated blood calcium levels. It can manifest as primary, secondary, or tertiary forms. Primary hyperparathyroidism arises from gland cell hyperplasia of unknown etiology, small benign tumors, or parathyroid adenomas. Secondary hyperparathyroidism occurs due to chronic hypocalcemia or reduced vitamin D levels resulting from other diseases or HD, whereas tertiary hyperparathyroidism develops from prolonged secondary hyperparathyroidism.
As evidenced by this case, surgical resection is an important aspect of treatment for hyperparathyroidism. Parathyroidectomy with bilateral neck exploration has been the standard of care for treating parathyroid hyperplasia[12]. A 10-year study of surviving patients undergoing HD showed that 64.8% of patients eventually underwent parathyroidectomy due to hyperparathyroidism[13]. In fact, parathyroidectomy is the only effective treatment for primary hyperparathyroidism[14]. However, in this case, resection of lesions on the right side only was sufficient to alleviate the patient’s symptoms. To the best of our knowledge, there are only a few case reports about parathyroid hyperplasia or adenomas extending to the lung region. More evidence is needed for the indication of surgical resection of both lesions (Table 1)[15,16].
| Case report title | Year | Lesion | Treatment | Outcome |
| Persistent hyperparathyroidism secondary to ectopic parathyroid adenoma in lung: Case report[15] | 2022 | Right side | Video-assisted thoracic surgery | Symptom improved |
| Recurrent hyperparathyroidism due to parathyroid and pulmonary tumors showing features of parathyroid adenoma[9] | 2020 | Right side | Surgically removed | Symptom improved |
| A patient with lung ectopic parathyroid coexistent with primary hyperparathyroidism and end-stage renal diseases[16] | 2014 | Mono-side | Surgically removed | Symptom improved |
It was challenging to determine whether our patient's hyperparathyroidism stems from secondary hyperparathyroidism or from parathyroid seeding in the lung. Typically, secondary hyperparathyroidism does not correlate with elevated blood calcium levels. However, blood tests revealed that our patient had hypercalcemia, suggesting that hyperparathyroidism presenting as multiple pulmonary nodules in a HD patient is likely.
In conclusion, we present a rare case of hyperparathyroidism stemming from multiple hyperplastic parathyroid glands with pulmonary seeding. This underscores the importance of comprehensive evaluation in HD patients presenting with hyperparathyroidism. Diagnostic measures such as neck ultrasound and chest CT should be employed to assess the possibility of parathyroid hyperplasia or adenomas extending to the lungs. If there is a chance of hyperplastic parathyroid glands with pulmonary seeding, surgical removal could be a good option for symptom improvement and to confirm pathological findings. Moreover, integrating clinical data with imaging findings is crucial for gauging the malignant potential of tumors, apart from pathological findings. It is important to always keep in mind that patients’ conditions should be followed after treatment.
| 1. | Colognesi A, de Tullio D, Messina F, Ferrocci G, Stano R, Azzena G. Primary hyperparathyroidism related to a parathyroid adenoma: the dramatic clinical evolution of a misdiagnosed patient and its surgical solution. Minerva Chir. 2006;61:51-56. [PubMed] |
| 2. | Bilezikian JP, Bandeira L, Khan A, Cusano NE. Hyperparathyroidism. Lancet. 2018;391:168-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 323] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 3. | Shen W, Düren M, Morita E, Higgins C, Duh QY, Siperstein AE, Clark OH. Reoperation for persistent or recurrent primary hyperparathyroidism. Arch Surg. 1996;131:861-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 145] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Lau WL, Obi Y, Kalantar-Zadeh K. Parathyroidectomy in the Management of Secondary Hyperparathyroidism. Clin J Am Soc Nephrol. 2018;13:952-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 5. | Santini M, Fiorello A, Mansi L, Rambaldi PF, Vicidomini G, Busiello L, Messina G, Nargi P. The role of technetium-99m hexakis-2-methoxyisobutyl isonitrile in the detection of neoplastic lung lesions. Eur J Cardiothorac Surg. 2009;35:325-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Abdel-Dayem HM, Scott A, Macapinlac H, Larson S. Tracer imaging in lung cancer. Eur J Nucl Med. 1994;21:57-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Nikoletic K, Lucic S, Peter A, Kolarov V, Zeravica R, Srbovan D. Lung 99mTc-MIBI scintigraphy: impact on diagnosis of solitary pulmonary nodule. Bosn J Basic Med Sci. 2011;11:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Zhang S, Liu Y. Diagnostic Performances of 99mTc-Methoxy Isobutyl Isonitrile Scan in Predicting the Malignancy of Lung Lesions: A Meta-Analysis. Medicine (Baltimore). 2016;95:e3571. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Miyauchi R, Yamada T, Kumano R, Aida Y, Takagi M. Recurrent hyperparathyroidism due to parathyroid and pulmonary tumors showing features of parathyroid adenoma. Radiol Case Rep. 2020;15:1289-1294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Erickson LA, Jin L, Wollan P, Thompson GB, van Heerden JA, Lloyd RV. Parathyroid hyperplasia, adenomas, and carcinomas: differential expression of p27Kip1 protein. Am J Surg Pathol. 1999;23:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 72] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Osawa N, Onoda N, Kawajiri H, Tezuka K, Takashima T, Ishikawa T, Miyauchi A, Hirokawa M, Wakasa K, Hirakawa K. Diagnosis of parathyroid carcinoma using immunohistochemical staining against hTERT. Int J Mol Med. 2009;24:733-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Lebastchi AH, Donovan PI, Udelsman R. Paradigm shift in the surgical management of multigland parathyroid hyperplasia: an individualized approach. JAMA Surg. 2014;149:1133-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Neff MS, Eiser AR, Slifkin RF, Baum M, Baez A, Gupta S, Amarga E. Patients surviving 10 years of hemodialysis. Am J Med. 1983;74:996-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Yu N, Leese GP, Smith D, Donnan PT. The natural history of treated and untreated primary hyperparathyroidism: the parathyroid epidemiology and audit research study. QJM. 2011;104:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Valizadeh M, Ebadinejad A, Amouzegar A, Zakeri A. Persistent hyperparathyroidism secondary to ectopic parathyroid adenoma in lung: Case report. Front Endocrinol (Lausanne). 2022;13:988035. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |