Published online Jul 28, 2023. doi: 10.4329/wjr.v15.i7.226
Peer-review started: April 25, 2023
First decision: June 19, 2023
Revised: June 20, 2023
Accepted: July 7, 2023
Article in press: July 7, 2023
Published online: July 28, 2023
Processing time: 89 Days and 23.6 Hours
Irritable bowel syndrome (IBS) is one of the most frequently referred conditions to the gastrointestinal outpatient clinic. The pathophysiology of IBS has not been determined with certainty. Visceral hypersensitivity is indicated as one of the pathophysiologies. The sympathetic nervous system is primarily in charge of controlling the arteries, and its effect is vasospasm in the medium and large arteries, resulting in decreased blood flow.
To demonstrate, using Doppler evaluation of the brachial artery, that sympathetic activity impairs vasomotor performance due to autonomic neuropathy, which we believe is associated with IBS.
There were 58 participants in the study. The control group consisted of 29 healthy patients, while the remaining 29 patients had been diagnosed with IBS. Patients who met the Rome IV criteria and had IBS were included in the study. People with known polyneuropathy or non-IBS chronic conditions that can progress were excluded from the trial, as were those with essential hypertension, diabetes mellitus, cardiovascular disease, or peripheral arterial disease, and patients diagnosed with anxiety or depression. Those with moderate to severe carpal tunnel syndrome or a median nerve lesion due to trauma were also excluded from the trial. A Doppler probe was used to measure the baseline diameter and flow rates of the brachial artery from 2 cm superior to the antecubital fossa. The Doppler probe remained stationary throughout the experiment, allowing for continuous measurements. Then, to activate the sympathetic fibers, an electrical stimulus for 5 s with an intensity of 10 mA and a frequency of 1 Hz was applied to the median nerve at the wrist level via the bipolar stimulus electrode. The artery diameter and flow rates were measured again immediately following the fifth stimulus.
In healthy persons with no history of chronic illness, there was a statistically significant decrease in flow rate after stimulation (P < 0.001). In addition, stimulation resulted in a statistically significant reduction in the diameter of the brachial artery (P < 0.001). Patients diagnosed with IBS had statistically significant vasodilation and an increase in flow rate.
Sympathetic stimulation causes a reduction in vascular diameter and blood flow, whereas it has the reverse effect on IBS patients. In investigating the involvement of autonomic neuropathy in the development of IBS, significant changes in brachial artery Doppler parameters were observed before and after stimulation of the median nerve with low-current sensory stimulation. This method is thought to be more user-friendly and comfortable than other methods described in the literature.
Core Tip: It has been noted that the autonomic activity of individuals who suffer from irritable bowel syndrome (IBS) differs from that of healthy people. Colored Doppler ultrasonography can be utilized as a noninvasive diagnostic tool that can be performed at any age and at any age, is comfortable for the patient, and does not require further patient compliance to show autonomic dysfunction in patients with IBS.
- Citation: Kazci O, Ege F, Aydemir H, Kazci S, Aydin S. Can the change of vasomotor activity in irritable bowel syndrome patients be detected via color Doppler ultrasound? World J Radiol 2023; 15(7): 226-233
- URL: https://www.wjgnet.com/1949-8470/full/v15/i7/226.htm
- DOI: https://dx.doi.org/10.4329/wjr.v15.i7.226
Irritable bowel syndrome (IBS) is a common chronic disease that causes constipation, diarrhea, or both, as well as abdominal pain or cramps, and can significantly reduce quality of life and work productivity. The diagnosis can be made with confidence if organic diseases are ruled out and characteristic symptoms are present. Environmental factors such as stress, food intolerance, enteric infections, and antibiotics, as well as patient-related factors such as variability in pain perception, variability in brain-gut interaction, dysbiosis, increased intestinal permeability, increased intestinal mucosal immune activation, and visceral hypersensitivity, are considered potential etiologies[1,2]. The autonomic nervous system modulates visceral sensitivity, and the central nervous system influences gastrointestinal secretion and activity via the enteric nervous system and autonomic pathways[3,4].
Some studies have found differences in autonomic activity between IBS subgroups. In studies with IBS and control groups, in patients with IBS, in the study of Karling et al[5], the heart rate variability was evaluated in the supine position with the head 70° upwards; an increase in sympathetic nervous system activation was observed, but no significant change in parasympathetic nervous system activation was found[5]. Adeyemi et al[6] investigated heart rate variability under orthostatic stress, deep inspiration, and resting states and discovered an increase in sympathetic nervous system activation and a decrease in parasympathetic nervous system activation[6]. Van Orshoven et al[7] measured blood pressure, heart rate, heart rate variability, and muscle sympathetic nerve activity before, during, and after a standard meal. As a result, parasympathetic nervous system activation decreased while sympathetic nervous system activation increased. There was no discernible difference[7]. Tanaka et al[8] investigated fingertip blood flow during, before, and after cold stress and discovered an increase in sympathetic nervous system activation[8]. Spaziani et al[9] used baroreceptor sensitivity to assess heart rate and blood pressure variability before, during, and after rectal distension and found a decrease in baroreceptor sensitivity and an increase in blood pressure[9]. In a study by Yildirim et al[10], neuropathy tests (standing, Valsalva, deep inspiration, isometric exercise, and cold application) were evaluated, and it was discovered that sympathetic activity increased while parasympathetic activity decreased[10].
Doppler ultrasonography is a type of ultrasonographic imaging that is used to determine the morphology of vascular structures as well as the direction, amount, and shape of blood flow in them. The laser Doppler method is widely used to assess sympathetic vasoconstrictor function. In the literature, it is emphasized that continuous wave Doppler ultrasound is a valid alternative approach to laser Doppler flowmetry in healthy volunteers[11], as well as that it can be used to detect the normal and abnormal functioning of the peripheral sympathetic nervous system[12]. The benefits of using color Doppler ultrasonography include the fact that it has no known side effects, does not contain radiation, can be used at any time and age including pregnancy, is easy to apply, does not require additional patient compliance, and is a noninvasive diagnostic method.
Almost all research into autonomic dysfunction in IBS is out of date. The goal of this study was to determine if autonomic dysfunction can be demonstrated in IBS patients using this new color Doppler ultrasonography (CDUS)-based method, as well as to reevaluate the presence of autonomic dysfunction in IBS, which has been described in previous studies.
The participants signed a declaration form declaring that all participants and/or their legal guardians granted informed permission. The studies adhered to the most recent edition of the Declaration of Helsinki, and the Ankara City Hospital No. 2 Clinical Research Ethics Committee authorized the procedures.
Patients who met the Rome IV criteria and had IBS were included in the study. People with known polyneuropathy or non-IBS chronic conditions that can progress were excluded from the trial, as were those with essential hypertension, diabetes mellitus, cardiovascular disease, peripheral arterial disease, and patients diagnosed with anxiety or depression. Those with moderate to severe carpal tunnel syndrome or a median nerve lesion due to trauma were also excluded from the trial.
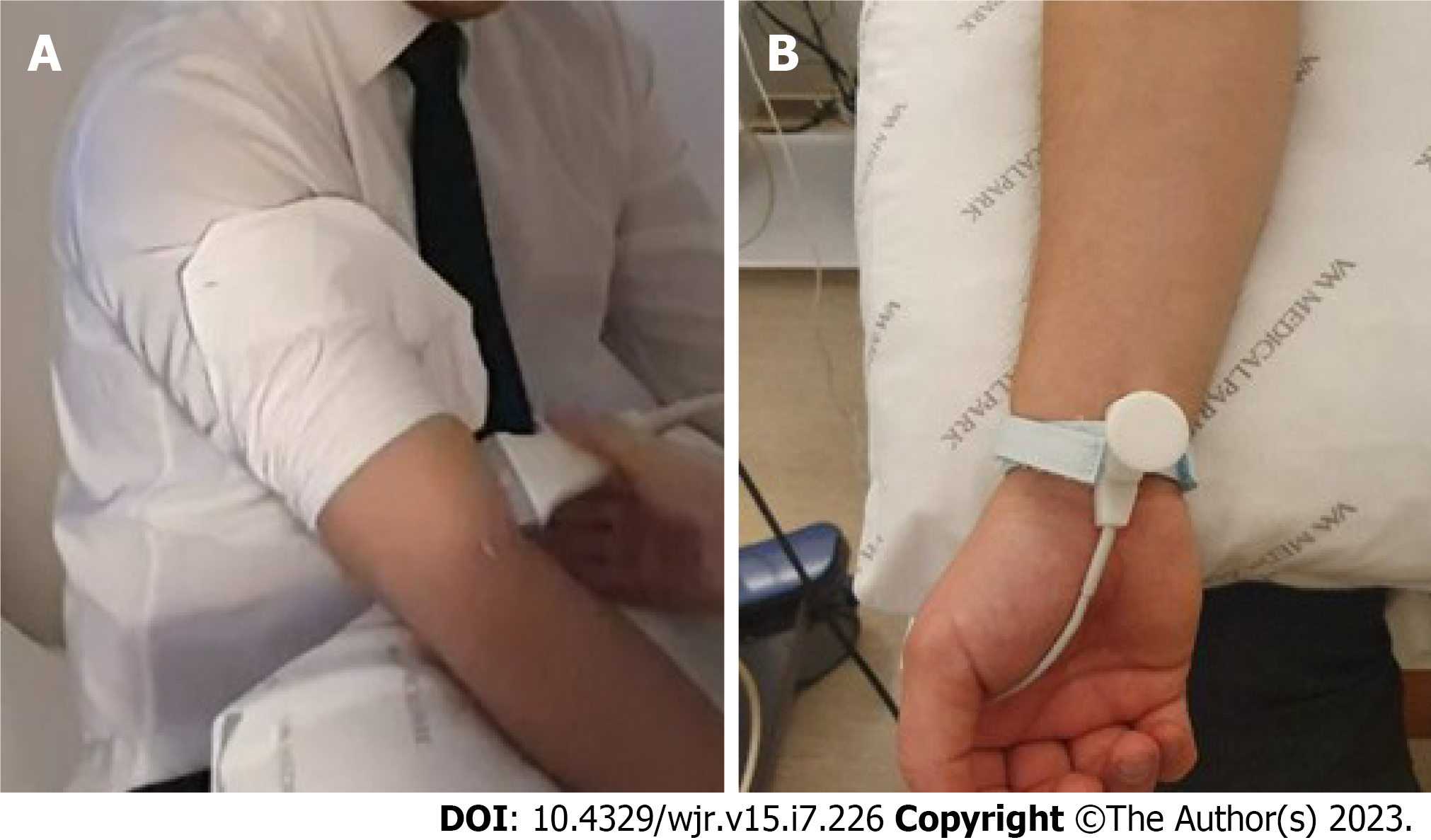
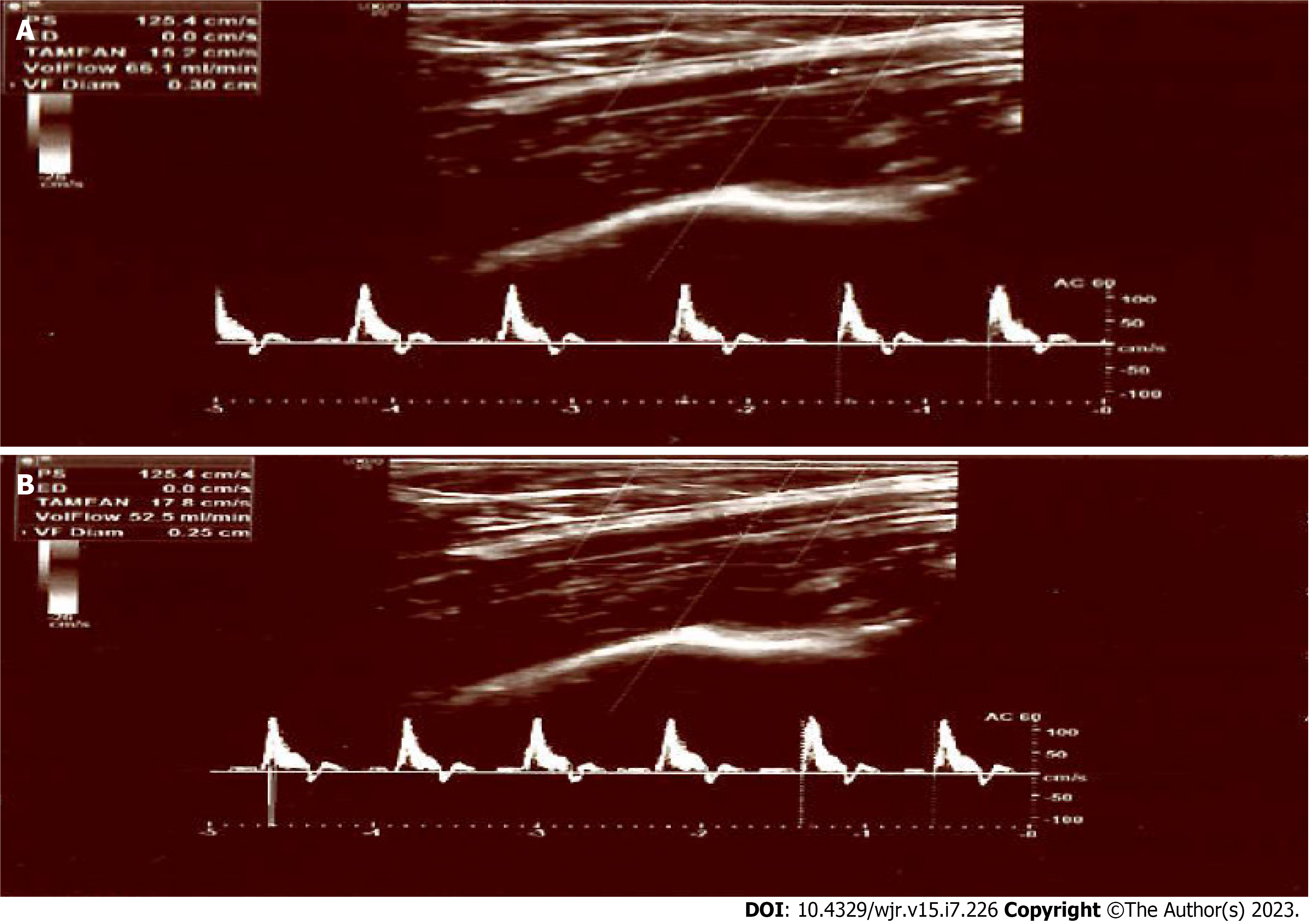
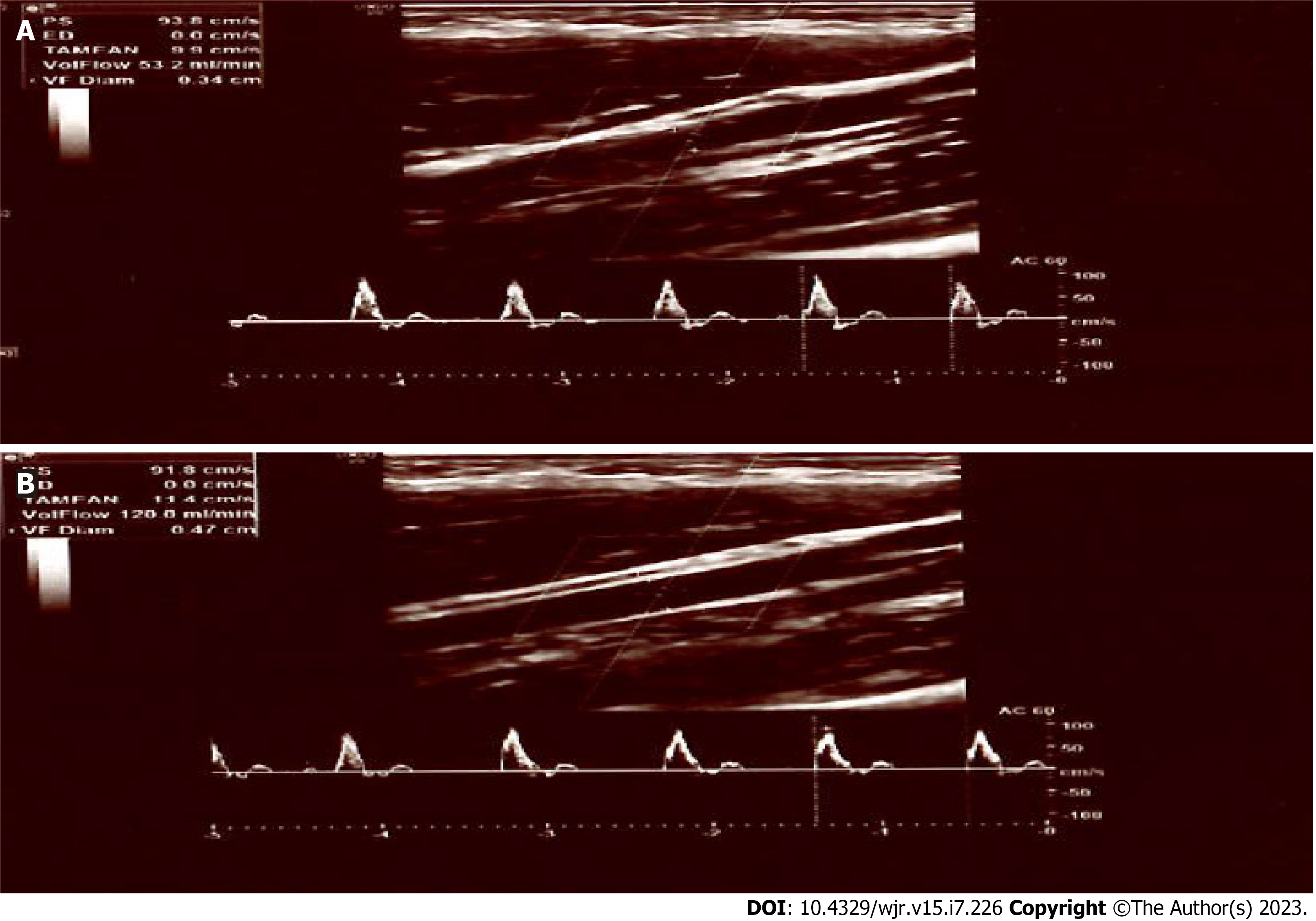
The technical models are associated with “studies on sensory nerve conduction.” These non-invasive approaches are utilized in routine clinical electrophysiological examinations to detect peripheral neuropathies. Four hours before the experiment, nicotine, caffeine, alcohol, and exercise were restricted. Before measuring the subjects' blood pressure, heart rate, and body temperature, they rested for 10 min in a seated position with their forearms supinated. The study was carried out at temperatures between 22 C and 24 C. Individuals were encouraged to remain as motionless as possible and were verbally informed at each test stage following a 10-min rest period (for example, before the Doppler measurement was performed and before the electrical stimulation began). The diameter and flow rates of the right brachial artery were measured from 2 cm above the antecubital fossa using a 9 Hz linear probe of the LOQIC P9 USG Doppler device (GE Healthcare, Chicago, IL, United States) (Figure 1A). A radiologist with 8 years of experience in Doppler took these readings. The Doppler sensor remained stationary during the experiment, allowing for continuous readings. Then an electrical stimulation of 10 mA intensity and 1 Hz frequency was applied to the median nerve at the level of the wrist for 5 s using the bipolar stimulus electrode of the Neuropack S1 MEB-9400A EMG/EP system (Nihon Kohden Co., Tokyo, Japan), in the direction of the sensory fibers (orthodromically) (Figure 1B). Immediately after the sixth stimulation, artery diameter and flow rates were measured again. Some demonstrative examinations can be seen in Figures 2 and 3.
In addition to sociodemographic data such as age and sex, the diameters and flow rates of the brachial arteries were recorded as final data before and after electrical stimulation in the healthy control group and IBS patients.
The variables were investigated using analytical methods (Kolmogorov-Smirnov/Shapiro-Wilk’s test) to determine whether they were normally distributed. Descriptive analyses were presented using frequencies and percentages for the categorical variables, mean ± SD for normally distributed variables, and median (25P-75P) for the non-normally distributed variables. The Student’s t-test or Mann–Whitney U test was used for the comparison of continuous variables in independent groups, and the paired samples t-test was used in dependent groups. P < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS (20.0; Armonk, NY, United States).
The study included 58 people, 29 of whom were diagnosed with IBS and 29 of whom were in the control group. Thirty (51.7%) of the 58 participants in the study were women, with a median age of 36 (min-max: 18-64). The female/male ratios (51.7%/48.3%) were the same in both groups (P = 1.000), and the median age of the IBS group [36 (min-max: 31-48)] was comparable to that of the control group [36 (min-max: 30-49)] (P = 0.864).
Table 1 shows brachial artery flow measurements before and after median nerve stimulation in IBS and control groups. While the median pre-stimulation flow rate in the IBS group was 60.2 mL/min, the post-stimulation flow rate was 78.1 mL/min. Mean flow rates before and after stimulation in the control group were 77.5 and 39.7 mL/min, respectively. The decrease in flow seen in the control group with median nerve stimulation could not be replicated in the IBS group.
| Pre-stimulation flow rate (mL/min), mean ± SD | Post-stimulation flow rate (mL/min), mean ± SD | P value | |
| IBS (n = 29) | 60.2 ± 28.8 | 78.1 ± 42.5 | 0.002 |
| Control (n = 29) | 77.5 ± 36.5 | 39.7 ± 19.1 | < 0.001 |
| P value | 0.05 | < 0.001 |
Before median nerve stimulation, the mean brachial artery diameter in the IBS group was 3.44 mm, while it was 3.43 mm in the control group. While the diameters measured before median stimulation in the IBS and control groups were not statistically different (P = 0.092), the diameters measured after stimulation were statistically significant (P < 0.001). While median nerve stimulation caused a decrease in diameter in the control group, it caused an increase in the IBS group (Table 2).
| Diameter before stimulus (mm), mean ± SD | Diameter after stimulus (mm), mean ± SD | P value | |
| IBS | 3.4 ± 0.5 | 3.7 ± 0.5 | 0.01 |
| Control | 3.4 ± 0.5 | 2.8 ± 0.6 | < 0.001 |
| P value | 0.92 | < 0.001 |
Before the stimulus, there was no significant difference in the flow rate and artery diameters between the control and study groups (Tables 1 and 2).
Table 3 shows the changes in brachial artery flow and diameter measurements after median nerve stimulation. While there was a median increase in brachial artery output of 9.10 (min-max: 0.00-33.70) mL/min and a median increase in brachial artery diameter of 0.20 (min-max: 0.00-0.40) mm in the IBS group, the changes in flow and diameter were decreased in the control group. Median brachial artery output was 33.00 (min-max: 24.20-42.50) mL/min, and median brachial artery diameter was 0.50 (min-max: 0.40-0.90) mm in the control group. The participants in the IBS and control groups had a significant difference in brachial artery flow rates (P < 0.001) and diameters (P < 0.001) before and after median nerve stimulation. The change in flow and diameter after stimulation was statistically significant in both the IBS and control groups (P < 0.001 for both sexes).
| Flow difference before and after stimulus (mL/min), median (25P-75P) | Diameter difference before and after stimulus (mm), median (25P-75P) | |
| IBS | 9.10 (0.00-33.70) | 0.20 (0.00-0.40) |
| Control | -33.00 (-42.50 to -24.20) | -0.50 (-0.90 to -0.40) |
| P value | < 0.001 | < 0.001 |
By evaluating the changes in brachial artery flow (Table 4) and diameter (Table 5) according to the presence of chronic disease in the male and female groups, statistical significance was maintained for both sexes. In other words, the change in flow and diameter following stimulation was statistically significant (P < 0.001 for both sexes) in both the IBS and control groups.
| The difference in flow rate between before and after a stimülation (mL/min), median (25P-75P) | P value | ||
| Female | IBS (n = 15) | 11.90 (0.00-35.70) | < 0.001 |
| Control (n = 15) | -25.50 (-39.40 to -21.60) | ||
| Male | IBS (n = 14) | 6.55 (-0.60-25.50) | < 0.001 |
| Control (n = 14) | -39.75 (-58.90 to -32.00) |
| The difference in diameter between before and after a stimulation (mm), median (25P-75P) | P value | ||
| Female | IBS (n = 15) | 0.20 (0.00-0.40) | < 0.001 |
| Control (n = 15) | -0.50 (-1.00 to -0.30) | ||
| Male | IBS (n = 14) | 0.30 (0.00-0.50) | < 0.001 |
| Control (n = 14) | -0.60 (-0.90 to -0.40) |
The primary goal of our research was to use CDUS to detect autonomic dysfunction in IBS patients. In our study, there was an increase in brachial artery diameter and flow rate in IBS patients measured with Doppler ultrasonography before and after median nerve stimulation, whereas there was a decrease in the control group.
Changes in flow and diameter after median nerve stimulation were found to be statistically significant in both IBS patients and the control group, regardless of sex. This is the first study to compare autonomic dysfunction in IBS patients based on age and sex, and to use CDUS to assess sympathetic autonomic functions in IBS patients.
Previously, Eicke et al[11] used continuous-wave Doppler ultrasound and laser Doppler flowmetry to detect blood flow changes in the radial artery during sympathetic stimulation (deep breathing and coughing) and compared the two methods. They discovered a decrease in flow in the radial artery after sympathetic stimulation using both continuous-wave Doppler ultrasound and laser Doppler flowmetry. As a result, they determined that continuous-wave Doppler ultrasound can be used in blood flow measurements after sympathetic stimulation as laser Doppler flowmetry[11].
Several studies have reported differences in sympathetic and parasympathetic autonomic activity in IBS patients. The majority of these studies looked at both sympathetic and parasympathetic activity.
Karling et al[5] investigated autonomic activity differences in their study, which included 18 patients with IBS and 36 control groups, by evaluating heart rate variability in the supine position with the head 70° upwards. When compared to healthy people, IBS patients showed an increase in sympathetic nervous system activation but no significant change in parasympathetic nervous system activation[5].
Adeyemi et al[6] investigated autonomic activity differences in 35 patients with IBS and 18 control groups in a study that included orthostatic stress, deep inspiration, and resting-state heart rate variability. In the study, IBS patients had an increase in sympathetic nervous system activation at rest and a decrease in parasympathetic nervous system activation under orthostatic stress and deep inspiration compared to healthy individuals[6].
Van Orshoven et al[7] investigated autonomic activity differences and muscle sympathetic nerve activity in 18 patients with IBS and 19 control groups by evaluating blood pressure, heart rate, and heart rate variability during, before, and after consumption of a standard meal. When IBS patients were compared to healthy people, there was no decrease in parasympathetic nervous system activation, an increase in sympathetic nervous system activation, or a significant change in muscle sympathetic nerve activity[7].
The study group and control group were monitored, and autonomic neuropathy tests (standing posture, Valsalva, deep inspiration, isometric exercise, and cold application) were used in the study conducted by Yildirim et al[10], which included 50 patients with IBS and 49 control groups. The study discovered that when IBS patients were compared to healthy people, sympathetic activity increased while parasympathetic activity decreased[10].
There are also studies that only assessed sympathetic system dysfunction.
Tanaka et al[8] investigated autonomic activity differences in 59 patients with IBS and 40 control groups by measuring fingertip blood flow during, before, and after cold stress. In the study, IBS patients had higher levels of sympathetic nervous system activation than healthy people[8].
Spaziani et al[9] used baroreceptor sensitivity to assess heart rate and blood pressure variability before, during, and after rectal distension in 39 patients with IBS and 98 control groups. In the study, IBS patients were found to have lower baroreceptor sensitivity and a higher increase in blood pressure after rectal distension when compared to healthy individuals[9].
We have demonstrated, as in previous studies, that autonomic dysfunction exists in IBS patients. The method we used in our study is low-cost, simple, and comfortable for the patient, and it does not necessitate additional patient compliance. We described a novel method for demonstrating sympathetic autonomic dysfunction in IBS patients.
Our research had some limitations. The fact that CDUS measurements of brachial artery diameter and flow are user-dependent adds to the measurement's subjectivity. A single researcher measured everything in a single session. As a result, interobserver and intraobserver variability cannot be shown. Furthermore, the study's limitations include the relatively small study population and the fact that IBS subtypes were not evaluated separately. Another limitation of the current study was the lack of investigation into parasympathetic autonomic functions.
Our findings show that a new CDUS-based method can successfully detect sympathetic autonomic dysfunction in IBS patients. This method is thought to be more user-friendly and comfortable than other methods described in the literature.
Irritable bowel syndrome (IBS) is one of the most common illnesses referred to the gastrointestinal outpatient clinic. The pathophysiology of IBS is not completely understood. One of the pathophysiologies is visceral hypersensitivity. The sympathetic nervous system is primarily responsible for managing the arteries, and its consequence is vasospasm in the medium and large arteries, which results in decreased blood flow.
Our impetus came from our study's adoption of a novel approach to assess changes in vasomotor activity in IBS patients.
We wanted to employ a different way to determine the change in vasomotor activity in persons with IBS in our study.
The diameter and flow velocities of the brachial artery were determined using a probe with Doppler examination at the diameter of the antecubital fossa. To activate the sympathetic fibers, bipolar stimulation was applied to the median nerve at the wrist. Brachial artery diameter and flow velocities were assessed again immediately after the fifth stimulation.
In our study, a statistically significant decrease was found in brachial artery flow velocity and diameter after sympathetic stimulation in healthy individuals without a history of chronic disease. In patients with IBS, a statistically significant increase was found in brachial artery flow velocity and diameter after sympathetic stimulation.
As a result, sympathetic activation reduces artery width and blood flow in healthy people. In people with IBS, it has the opposite effect. Detection of changes in brachial artery diameter and flow velocity by Doppler examination is thought to be more useful and comfortable than other methods described in the literature.
It has been discovered that the autonomic activity of persons suffering from IBS differs from that of healthy people. Colored Doppler ultrasonography can be used as a noninvasive diagnostic method that can be conducted at any age, is comfortable for the patient, and does not require additional patient compliance in patients with IBS.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baeg MK, South Korea; Lv L, China S-Editor: Li L L-Editor: Filipodia P-Editor: Zhao S
| 1. | Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313:949-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 629] [Cited by in RCA: 740] [Article Influence: 74.0] [Reference Citation Analysis (0)] |
| 2. | Camilleri M. Diagnosis and Treatment of Irritable Bowel Syndrome: A Review. JAMA. 2021;325:865-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 180] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 3. | Iovino P, Azpiroz F, Domingo E, Malagelada JR. The sympathetic nervous system modulates perception and reflex responses to gut distention in humans. Gastroenterology. 1995;108:680-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 93] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Gibbons CH. Basics of autonomic nervous system function. Handb Clin Neurol. 2019;160:407-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 103] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 5. | Karling P, Nyhlin H, Wiklund U, Sjöberg M, Olofsson BO, Bjerle P. Spectral analysis of heart rate variability in patients with irritable bowel syndrome. Scand J Gastroenterol. 1998;33:572-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Adeyemi EO, Desai KD, Towsey M, Ghista D. Characterization of autonomic dysfunction in patients with irritable bowel syndrome by means of heart rate variability studies. Am J Gastroenterol. 1999;94:816-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | van Orshoven NP, Andriesse GI, van Schelven LJ, Smout AJ, Akkermans LM, Oey PL. Subtle involvement of the parasympathetic nervous system in patients with irritable bowel syndrome. Clin Auton Res. 2006;16:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Tanaka T, Manabe N, Hata J, Kusunoki H, Ishii M, Sato M, Kamada T, Shiotani A, Haruma K. Characterization of autonomic dysfunction in patients with irritable bowel syndrome using fingertip blood flow. Neurogastroenterol Motil. 2008;20:498-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Spaziani R, Bayati A, Redmond K, Bajaj H, Mazzadi S, Bienenstock J, Collins SM, Kamath MV. Vagal dysfunction in irritable bowel syndrome assessed by rectal distension and baroreceptor sensitivity. Neurogastroenterol Motil. 2008;20:336-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Yildirim AE, Korkmaz M, Altun R, Sandikçi SC, Ocal S, Selçuk H. Is there any association between irritable bowel syndrome subgroups and autonomous dysfunction. Eur Rev Med Pharmacol Sci. 2016;20:1315-1322. [PubMed] |
| 11. | Eicke BM, Milke K, Schlereth T, Birklein F. Comparison of continuous wave Doppler ultrasound of the radial artery and laser Doppler flowmetry of the fingertips with sympathetic stimulation. J Neurol. 2004;251:958-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Kazci O, Ege F. Evaluation of Sympathetic Vasomotor Activity of the Brachial Arteries Using Doppler Ultrasound. Med Sci Monit. 2023;29:e939352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |