Copyright
©2013 Baishideng Publishing Group Co.
World J Radiol. Dec 28, 2013; 5(12): 460-467
Published online Dec 28, 2013. doi: 10.4329/wjr.v5.i12.460
Published online Dec 28, 2013. doi: 10.4329/wjr.v5.i12.460
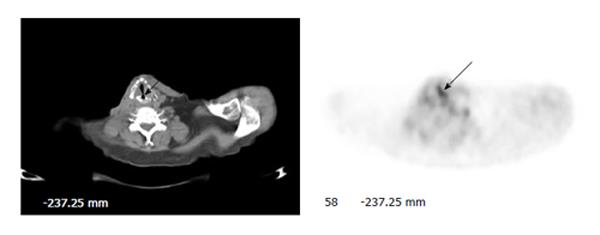
Figure 1 Unilateral vocal cord uptake.
A 59-year-old man with history of transglottic squamous cell carcinoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the neck shows intense unilateral uptake without a visible lesion on CT in the left true vocal cord (arrows). Subsequent laryngoscopic examination revealed paralysis of the right vocal cord.
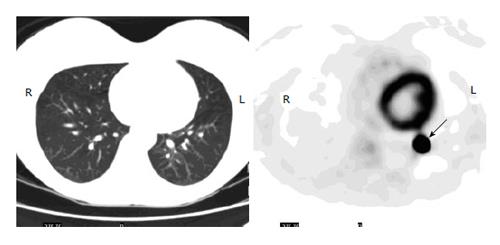
Figure 2 Iatrogenic uptake in the lung.
A 35-year-old woman with history of low grade serous ovarian cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Axial PET image of the lungs shows a focus of intense uptake in the left lower lobe (arrow), but no nodule or lesion is seen on CT. Subsequent diagnostic CT was negative as well for lung nodule. The uptake is likely secondary to microembolism due to a paravenous injection.
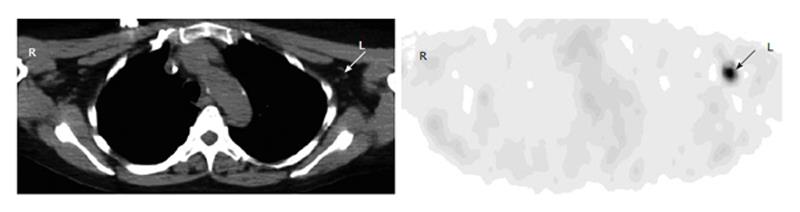
Figure 3 Axillary uptake.
A 63-year-old man with history of bladder cancer had fluorodeoxyglucose (FDG) positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the upper chest shows focal uptake in the left axilla (arrow). Corresponding to this focus, there is a small benign lymph node with fat lumen on CT (arrow). The uptake is secondary to infiltration of injected FDG at the antecubital site.
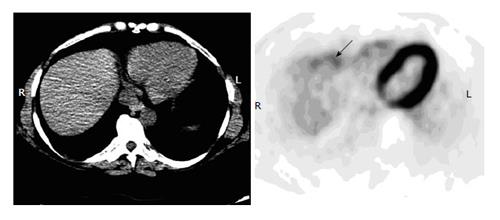
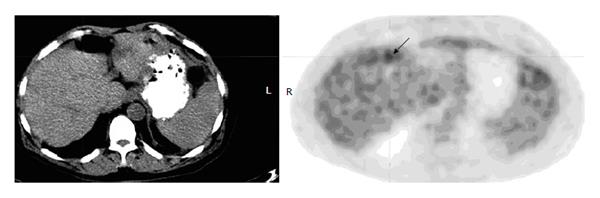
Figure 4 Noise artifact in the liver.
A 42-year-old man with history of cervical cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Axial PET image of the upper abdomen shows irregular uptake in the anterior margin (arrow) but without discrete lesions on an integrated CT, representing noise artifacts. Subsequent diagnostic CT was negative.
Figure 5 Colonic uptake abutting the margin of the liver.
A 59-year-old man with newly diagnosed pancreatic cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for staging. Axial PET image of the upper abdomen shows a small focus of increased uptake abutting the anterior margin of the liver (arrow). But there is no visible hepatic lesion on the integrated CT. A magnetic resonance imaging was also negative for any lesion in the liver. The uptake is from the adjacent transverse colon with slight motion artifact and mis-registration of PET and CT images.
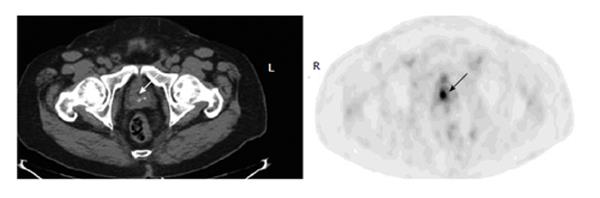
Figure 6 Urine activity in the prostatic urethra.
A 65-year-old man with history of lung cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the lower pelvis shows a focus at the midline of the prostate, corresponding to the dilated urethra on CT (arrows). The finding represents urine retention in the urethra of previous trans-urethral prostate resection site.
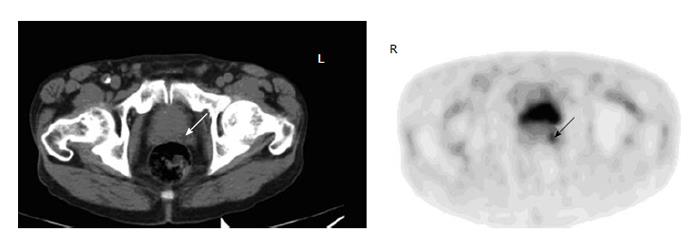
Figure 7 Uptake of prostate cancer.
A 63-year-old man with history of laryngeal cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging Axial PET image of the lower pelvis shows a focus corresponding to a hypodensity lesion on the CT in the left peripheral prostate (arrows). Biopsy confirmed prostate cancer.
Figure 8 Focal brown fat uptake.
A 50-year-old woman with history of metastatic breast cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image shows a focus in the left supraclavicular region (arrow). On the integrated CT, there is no node or lesion except for fat tissue in this location. The uptake is from the brown fat.
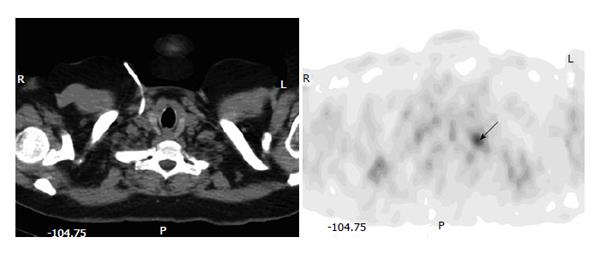
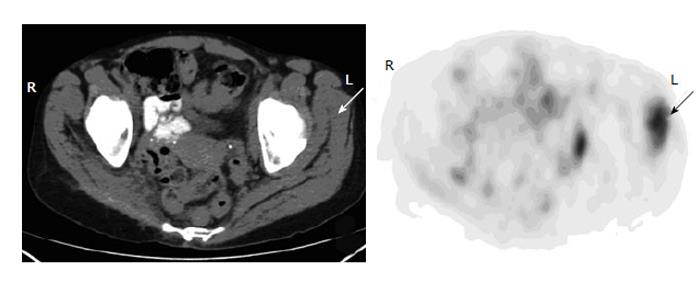
Figure 9 Muscular uptake.
A 45-year-old woman with history of leiomyosarcoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET-CT images of the pelvis show intense focal muscular uptake in the left gluteus maximus, gluteus minimus and obturator intermus, with no corresponding lesions on the CT (arrows). Two subsequent magnetic resonance images were unremarkable of the muscles.
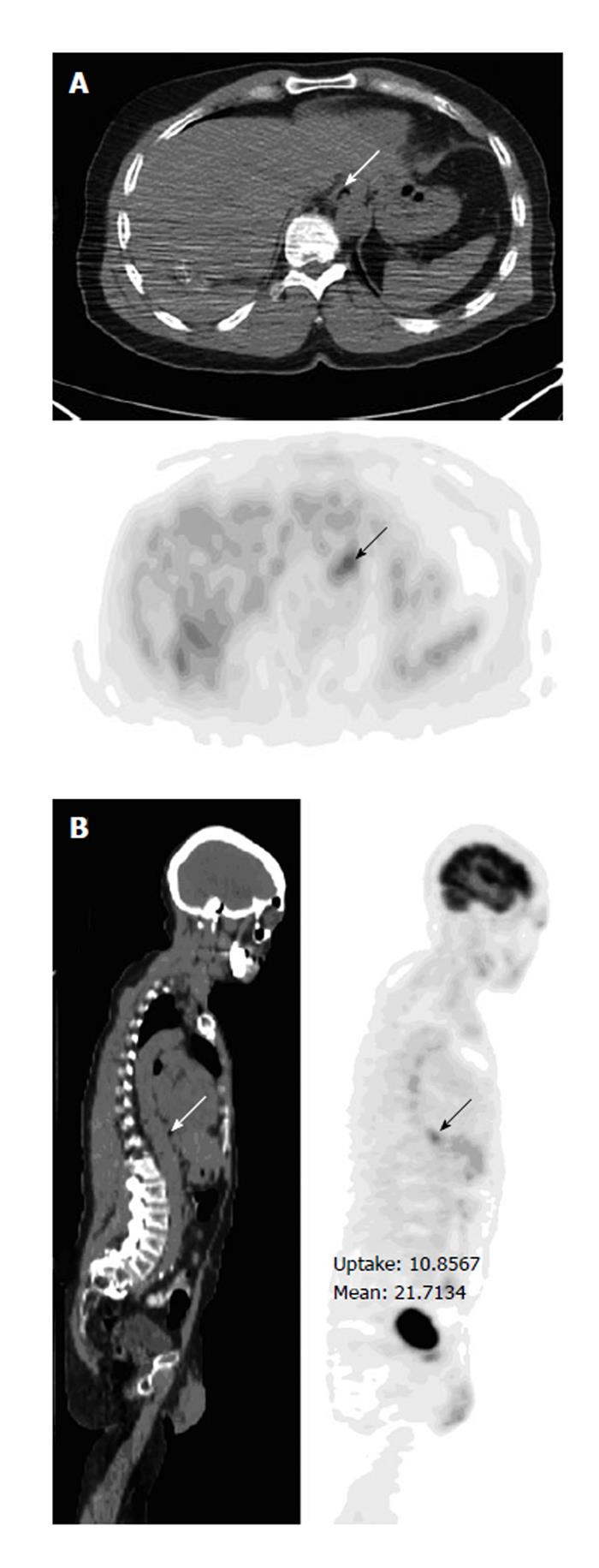
Figure 10 Prominent uptake in the gastroesophageal junction.
A 57-year-old man with history of osteosarcoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Axial (A) and sagittal (B) PET-CT images show focal uptake in the gastroesophageal junction (arrows), with no lesion on CT and stable over two years on follow-ups.
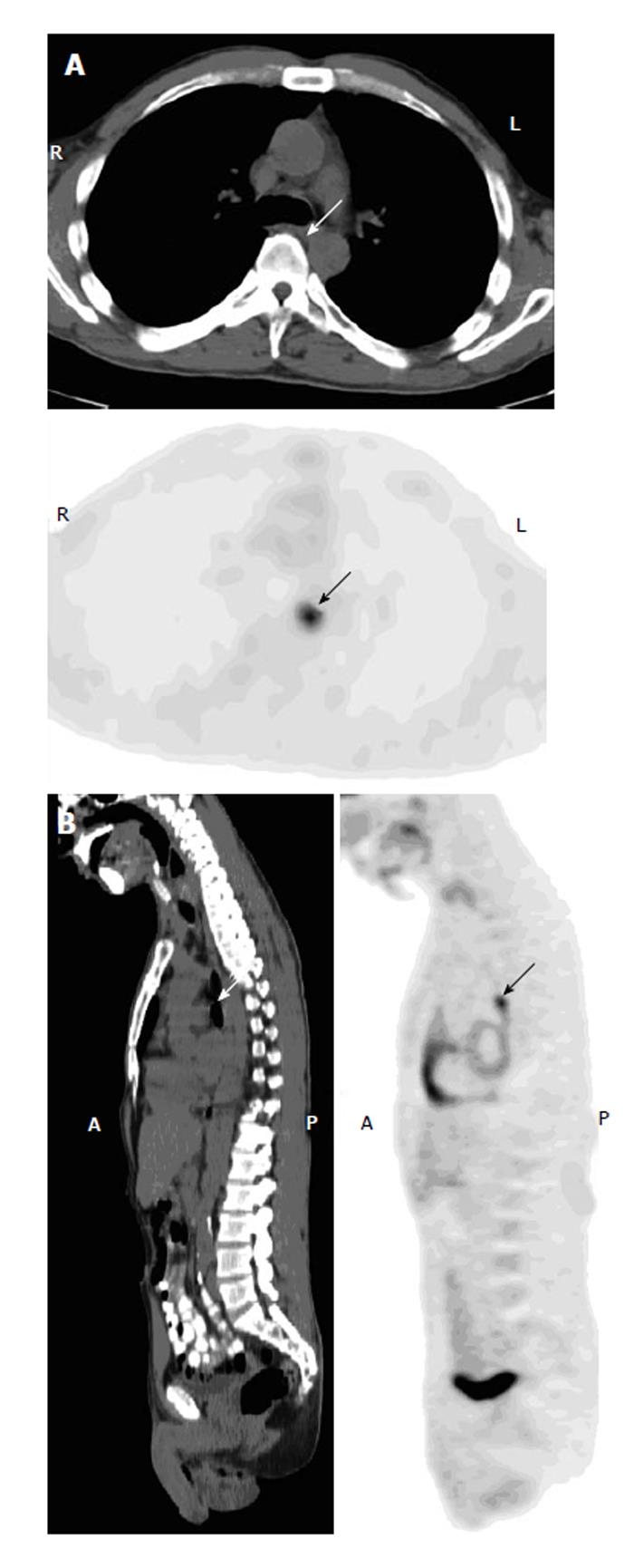
Figure 11 Uptake representing esophageal cancer.
A 49-year-old man with history of retromolar carcinoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial (A) and sagittal (B) PET-CT images show a focus in the mid esophagus at the subcarinal level (arrows), without a visible lesion or evident wall thickening on the integrated CT. Subsequent contrast CT was negative as well. An endoscopic biopsy revealed squamous cell carcinoma.
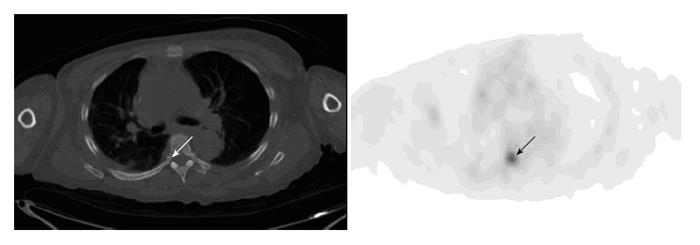
Figure 12 Osseous uptake.
A 55-year-old woman with history of metastatic breast cancer had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for restaging. Axial PET image of the chest shows focal uptake at the right pedicle of the T6 (arrow). There is no visible corresponding bone lesion on the integrated CT (arrow). Repeat PET-CT three months after shows multiple bone metastases including worsening uptake in the right-sided T6.
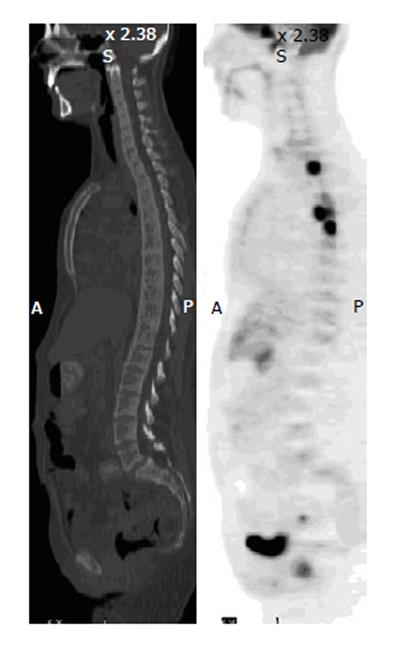
Figure 13 Lymphomatous disease of bone.
A 28-year-old man with disseminated B-cell lymphoma had fluorodeoxyglucose positron emission tomography-computer tomography (PET-CT) for initial staging. Sagittal PET image shows foci of intense uptake in the vertebral bodies of the upper thoracic spine, but the CT is unremarkable in the corresponding sites. Repeated scan 3 mo after chemotherapy demonstrate resolution of uptake in the bones as well as lungs and lymph nodes.
- Citation: Liu Y. Fluorodeoxyglucose uptake in absence of CT abnormality on PET-CT: What is it? World J Radiol 2013; 5(12): 460-467
- URL: https://www.wjgnet.com/1949-8470/full/v5/i12/460.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i12.460