Copyright
©The Author(s) 2024.
World J Radiol. Sep 28, 2024; 16(9): 473-481
Published online Sep 28, 2024. doi: 10.4329/wjr.v16.i9.473
Published online Sep 28, 2024. doi: 10.4329/wjr.v16.i9.473
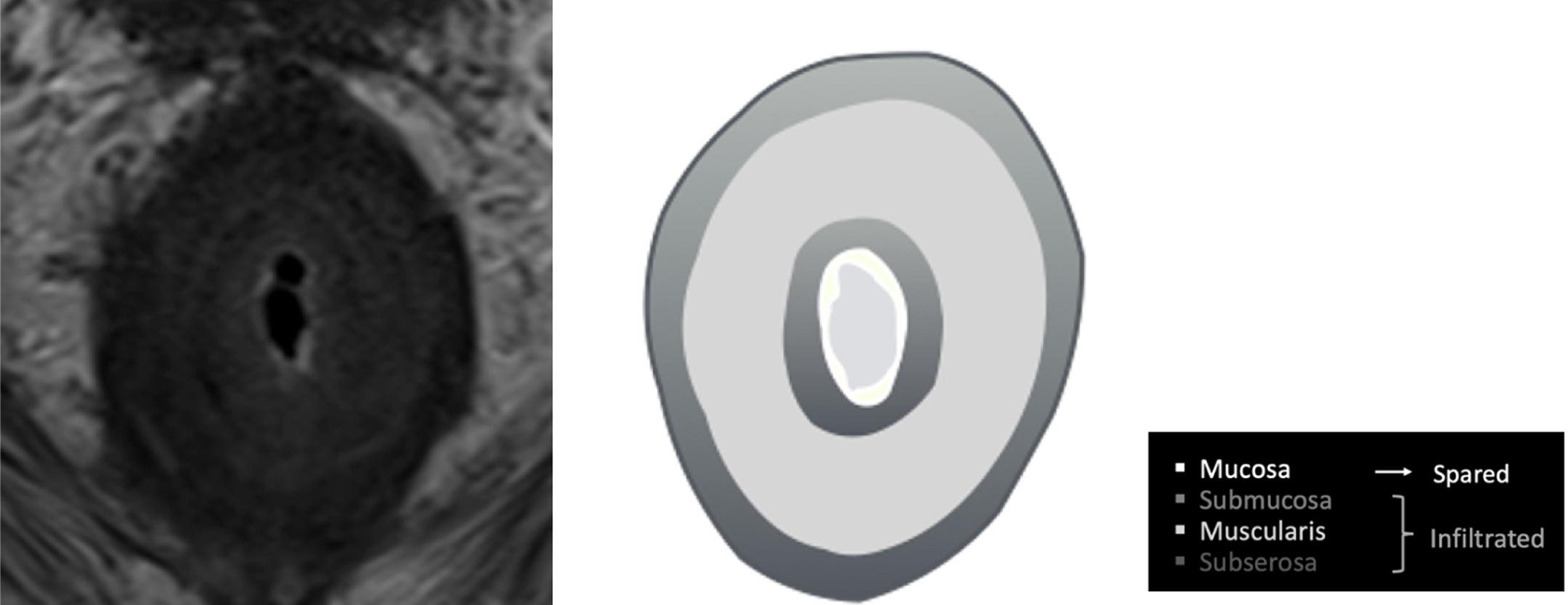
Figure 1 Illustration depicting the concentric "target-like" involvement of the rectal parietal wall due to secondary linitis plastica, with preservation of the mucosa.
Figure 2 The sigmoidoscopy reveals a narrowing of the rectal lumen accompanied by non-ulcerated underlying mucosa.
The preserved mucosa complicates endoscopic detection, emphasizing the importance of radiological evaluation for accurate diagnosis.
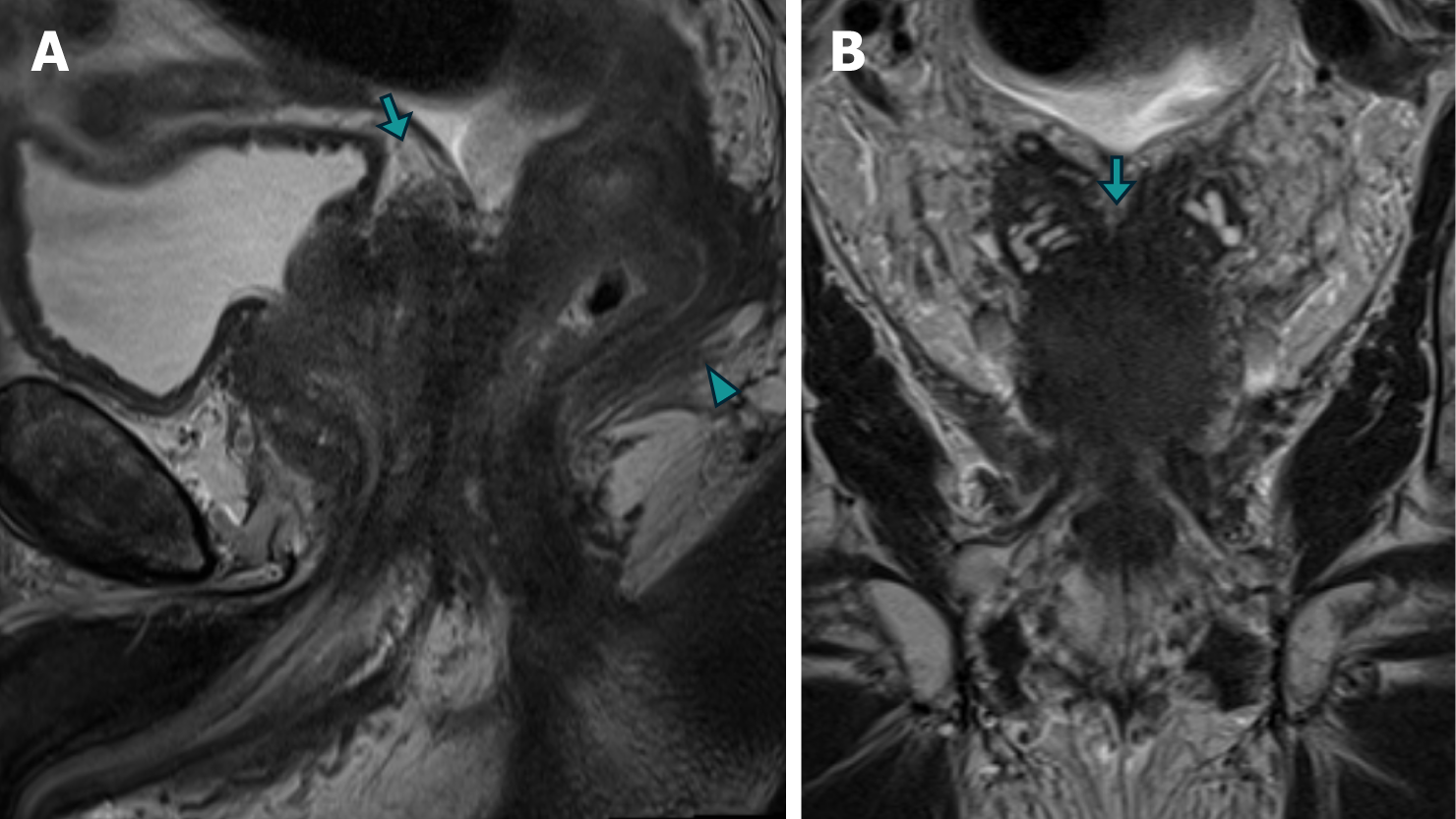
Figure 3 Magnetic resonance imaging images of case 1 demonstrating advanced prostate adenocarcinoma with rectal involvement.
A and B: The sagittal (A) and Coronal (B) T2 turbo spin echo images reveal diffuse neoplastic involvement of the prostatic parenchyma, with extension into the rectal wall (arrowhead) and base of the seminal vesicles (arrow).
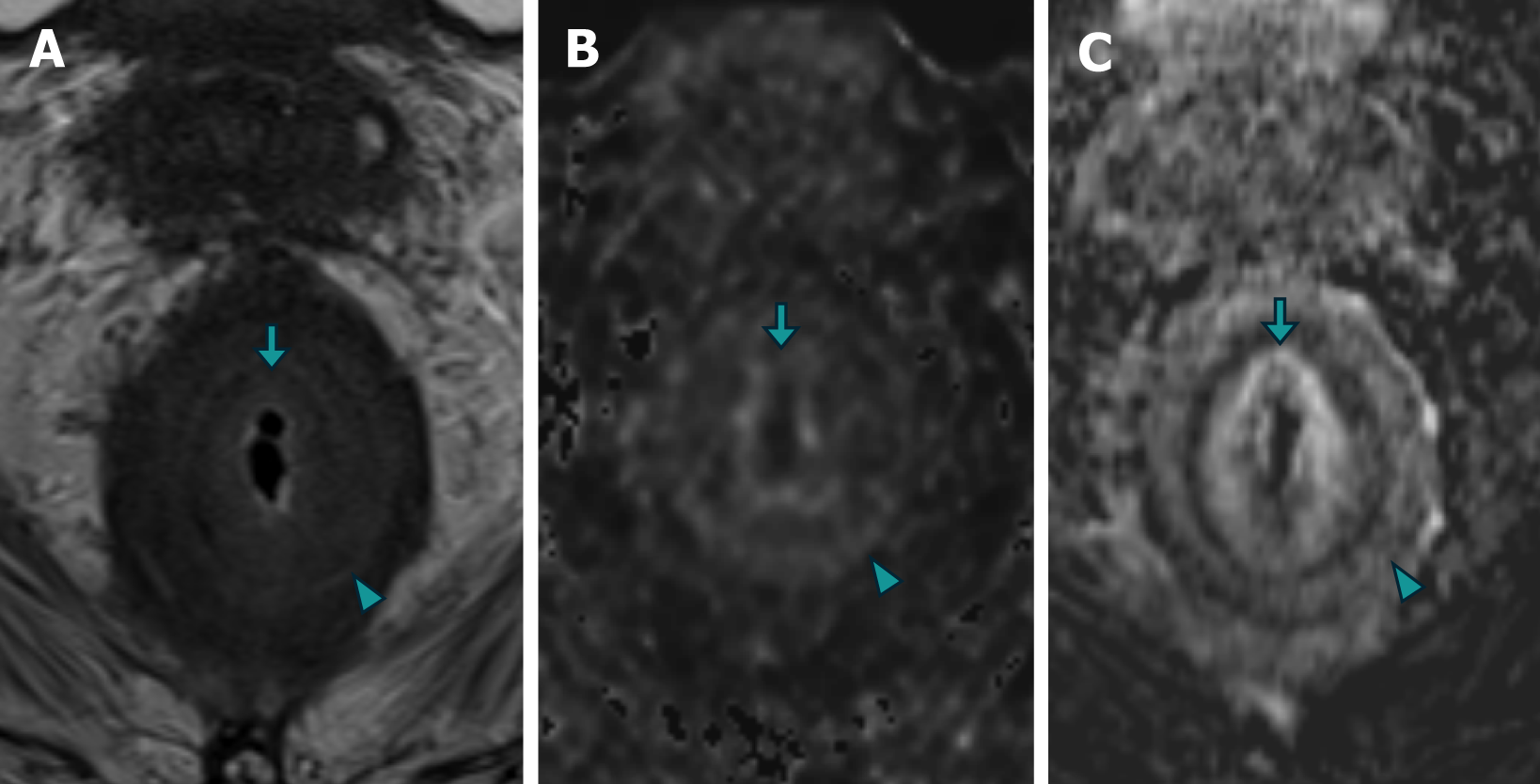
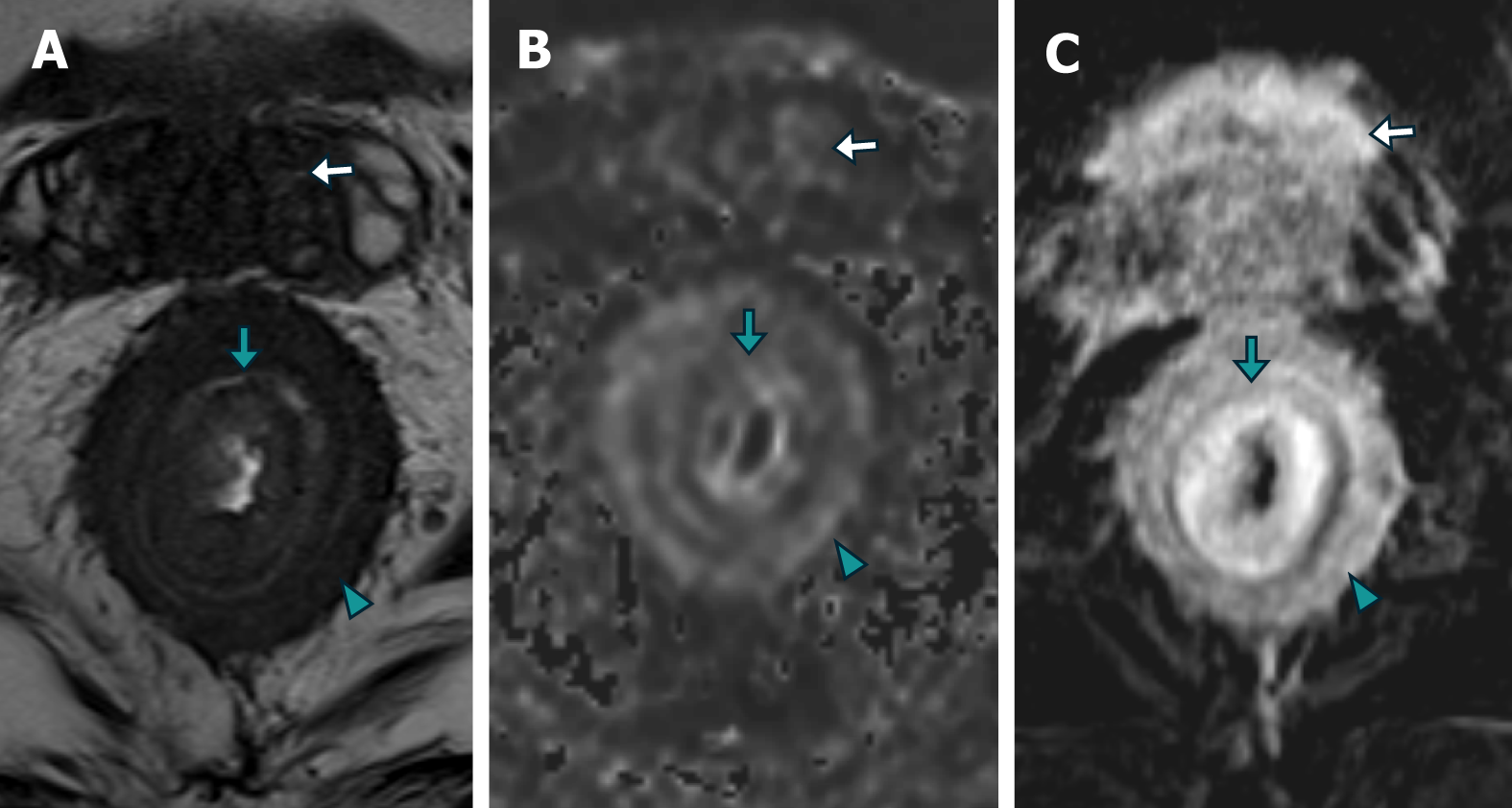
Figure 4 Magnetic resonance imaging images of case 1 demonstrating concentric "target-like" involvement of the rectal parietal wall due to secondary linitis plastica.
A: The axial images obtained from T2 turbo spin echo sequence; B: Diffusion-weighted imaging (DWI); C: T1 gradient recalled echo volumetric interpolated breath-hold examination with contrast-enhanced subtraction technique revealed a stratified parietal thickening of the rectal wall. This thickening displayed concentric areas of intermediate signal intensity on T2-weighted images, restricted diffusion on DWI, and enhancement on contrast-enhanced images, affecting both the submucosal (arrow) and muscular (arrowhead) layers.
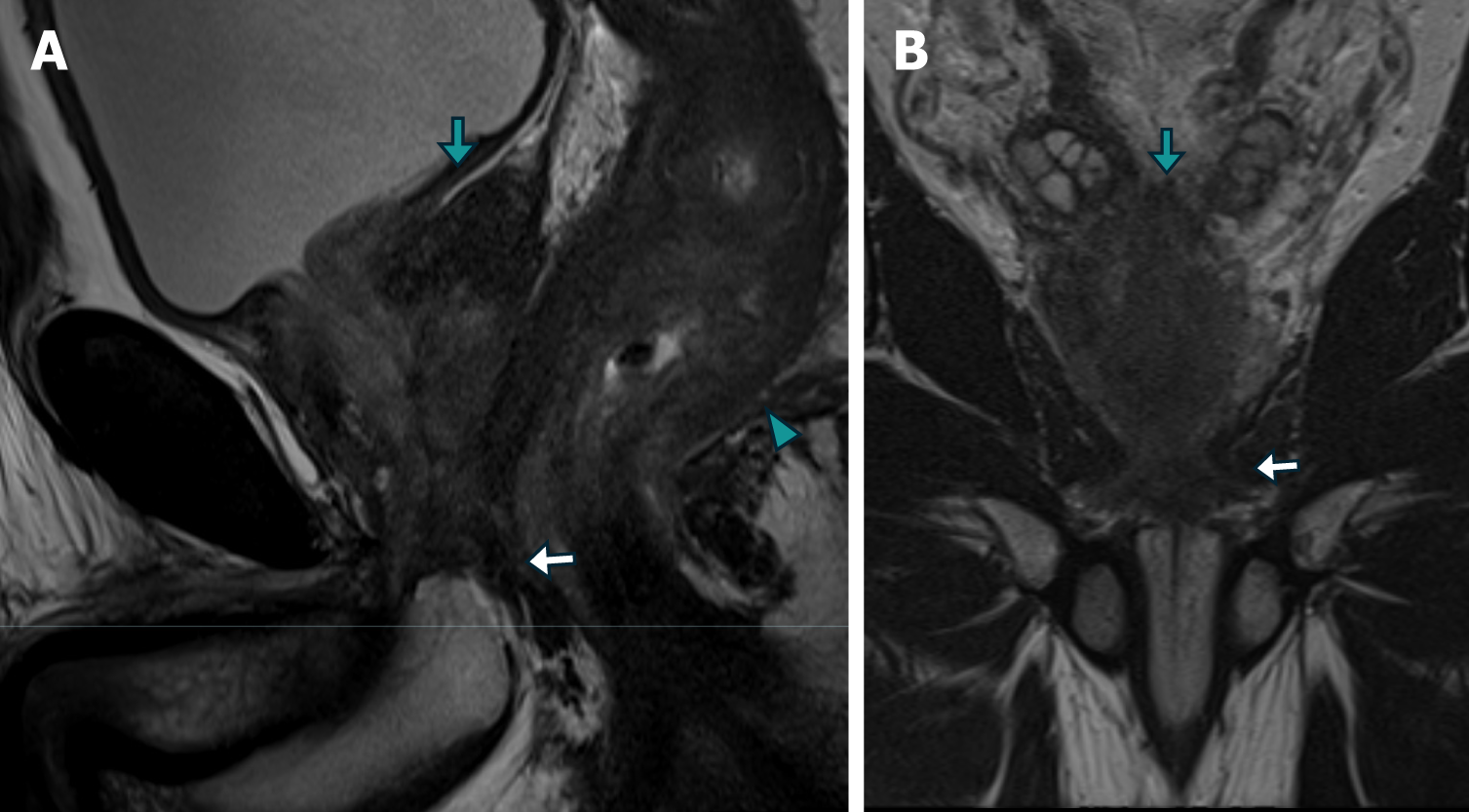
Figure 5 Magnetic resonance imaging images of case 2 demonstrating metastatic prostate adenocarcinoma.
A and B: The sagittal (A) and Coronal (B) T2-weighted turbo spin echo images demonstrate diffuse neoplastic involvement of the prostatic parenchyma, with extension to the rectal wall (arrowhead), base of the seminal vesicles (green arrow), and external urethral sphincter (white arrow).
Figure 6 Axial magnetic resonance imaging of case 2.
A-C: The imaging findings reveal a stratified parietal thickening of the rectal wall, characterized by concentric areas of intermediate signal intensity on T2-weighted imaging (A), restricted diffusion on diffusion-weighted imaging (B), and contrast enhancement on post-contrast T1-weighted volumetric interpolated breath-hold examination imaging with subtraction (C), affecting both the submucosal (green arrow) and muscular/subserosal planes (arrowhead) resembling a "linitis plastica" appearance. In addition, there is neoplastic involvement of the base of the seminal vesicles (white arrow).
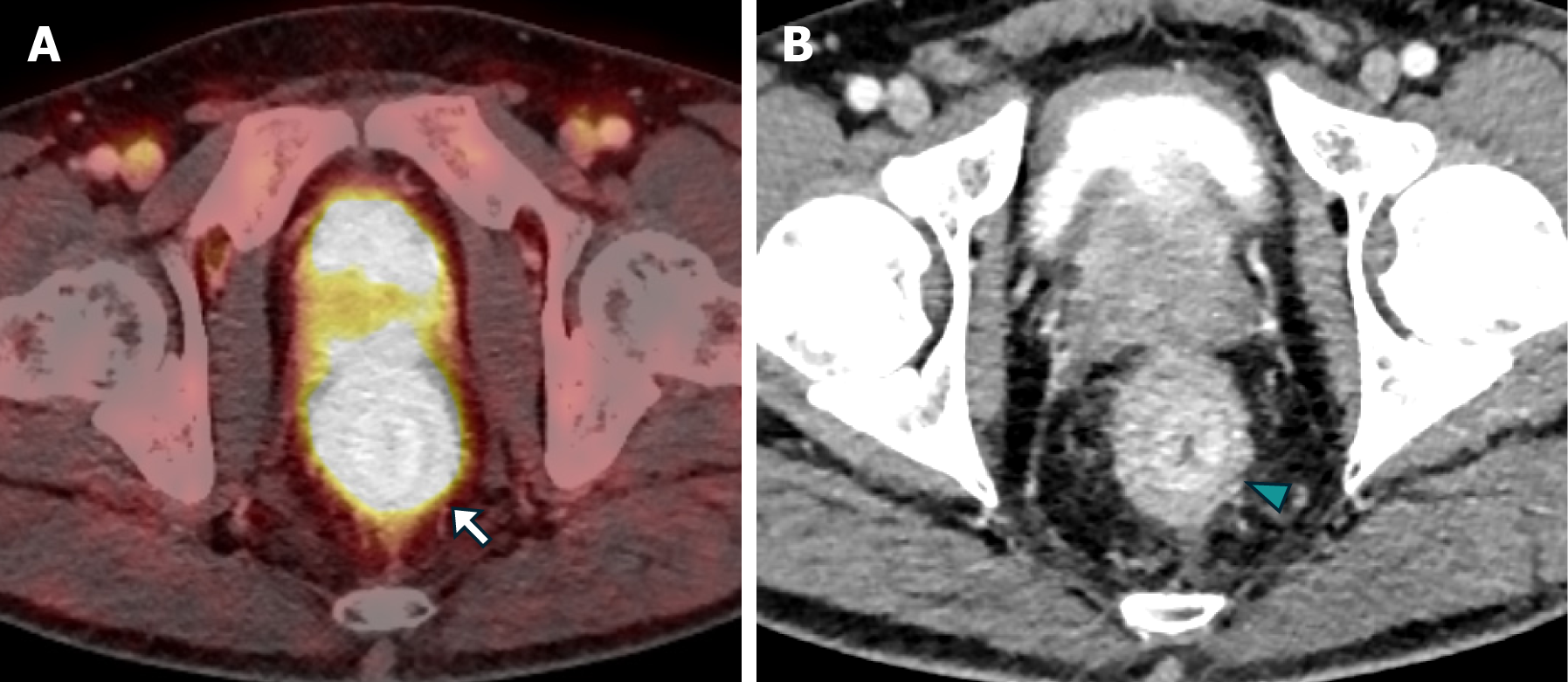
Figure 7 The positron emission tomography/computed tomography PSMA images in case 2.
A and B: Axial FUSION (A) and computed tomography (B) of abdomen and pelvis with intravenous contrast revealed a stratified parietal thickening of the rectal wall, displaying significant uptake of the radiotracer, thus confirming the prostatic origin of the neoplastic infiltration (white arrow). Furthermore, concentric impregnation with intravenous contrast (green arrowhead) was also observed.
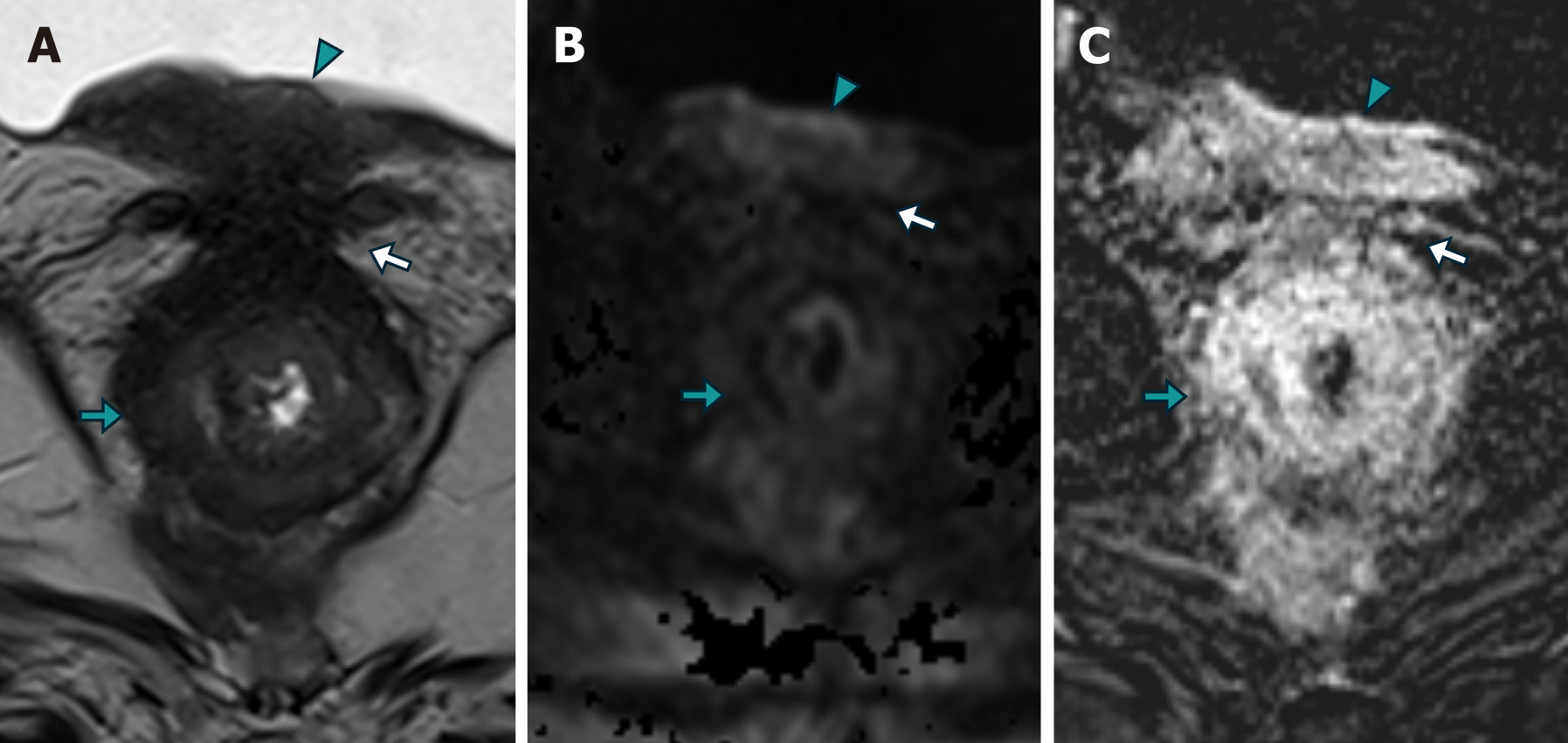
Figure 8 Magnetic resonance imaging findings in case 3.
A-C: T2-weighted turbo spin-echo axial imaging (A), diffusion-weighted axial imaging (B), and T1-weighted volumetric interpolated breath-hold examination imaging with contrast-enhanced subtraction (C). The imaging findings revealed a concentric neoplastic involvement of the rectal wall, characterized by areas of intermediate signal intensity on T2-weighted imaging (A), as well as restricted diffusion on diffusion-weighted imaging (correlating with a hypointense region on the apparent diffusion coefficient map, which was not shown; B), and a stratified enhancement pattern on contrast-enhanced imaging (green arrow; C). Notably, the imaging also showed neoplastic involvement of the vesico-rectal plane (white arrow) and the bladder floor wall (green arrowhead).
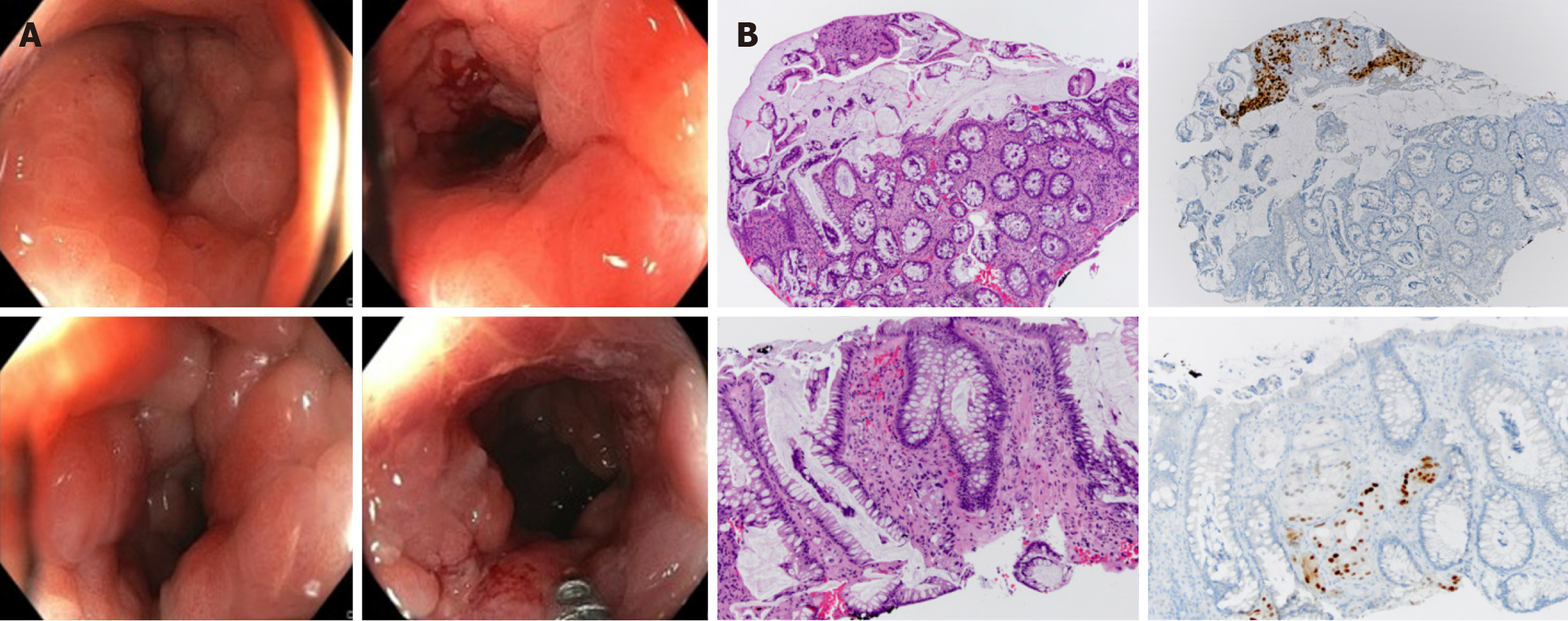
Figure 9 Colonoscopy and histological images of case 1 demostrating advanced metastatic prostate adenocarcinoma.
A: Colonoscopy image showing a reduced rectal lumen with congestive mucosa exhibiting increased consistency and loss of elasticity; B: Histological images of metastatic prostate adenocarcinoma utilizing Hematoxylin and Eosin staining in conjunction with immunohistochemical evaluation for the NKX marker. Groups of neoplastic cells arranged in nests and tubular structures. These cells exhibited atypical nuclei with prominent nucleoli and were positive for NKX, a highly specific marker for, albeit not exclusively indicative of, prostate origin.
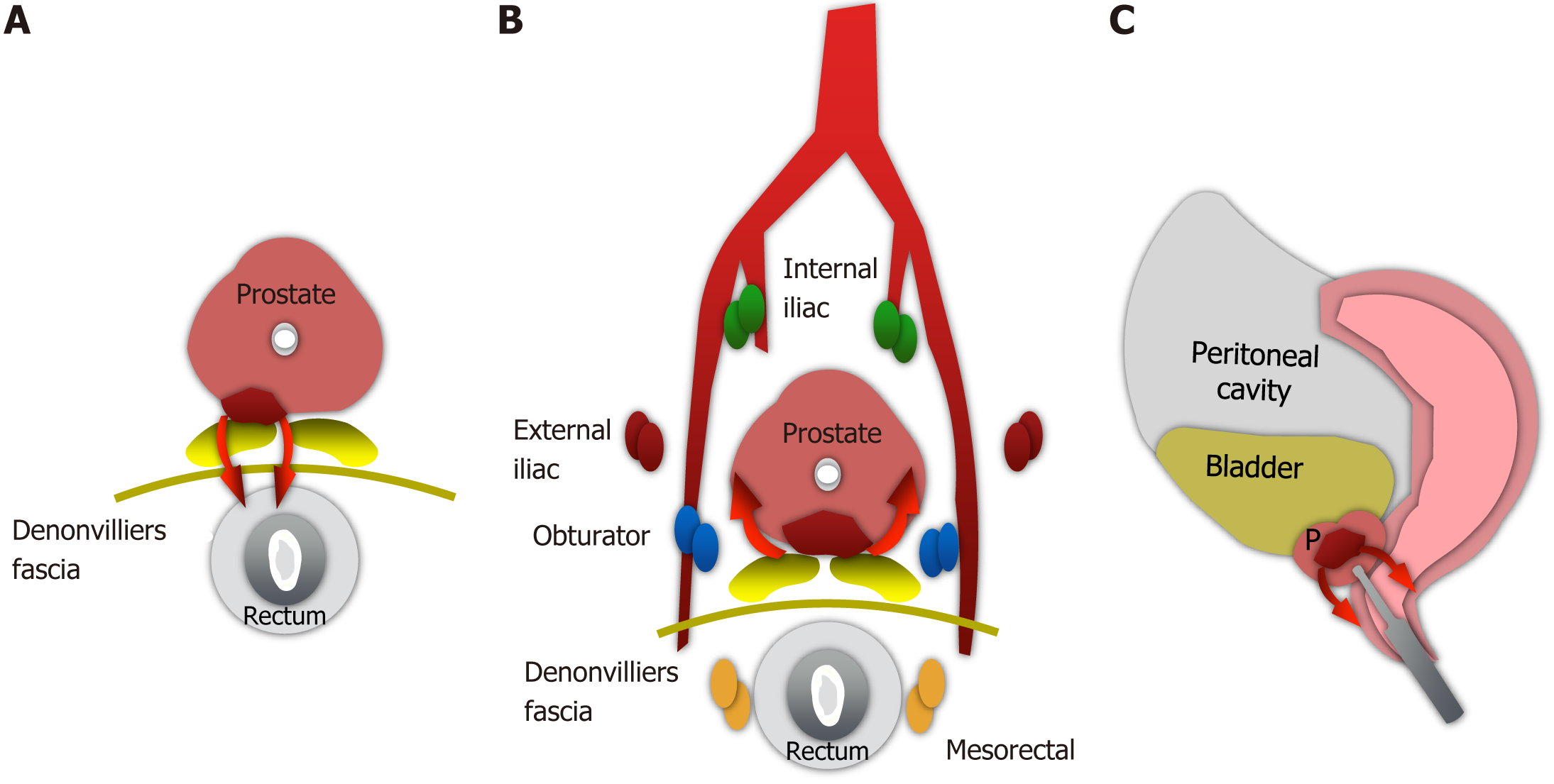
Figure 10 Postulated pathways of prostatic adenocarcinoma metastatic dissemination to the rectum.
These include direct extension through the rectoprostatic fascia or Denonvilliers' fascia (A), lymphatic and/or retrograde venous spread (B), and tumoral implantation (C) following transrectal prostate biopsy.
- Citation: Labra AA, Schiappacasse G, Cocio RA, Torres JT, González FO, Cristi JA, Schultz M. Secondary rectal linitis plastica caused by prostatic adenocarcinoma - magnetic resonance imaging findings and dissemination pathways: A case report. World J Radiol 2024; 16(9): 473-481
- URL: https://www.wjgnet.com/1949-8470/full/v16/i9/473.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i9.473