Peer-review started: July 10, 2016
First decision: September 12, 2016
Revised: November 16, 2016
Accepted: November 27, 2016
Article in press: November 29, 2016
Published online: January 26, 2017
Processing time: 194 Days and 22.3 Hours
Vitamin D deficiency is a prevalent condition, cutting across all ethnicities and among all age groups, and occurring in about 30%-50% of the population. Besides vitamin D established role in calcium homeostasis, its deficiency is emerging as a new risk factor for coronary artery disease. Notably, clinical investigations have suggested that there is an association between hypovitaminosis D and acute myocardial infarction (AMI). Not only has it been linked to incident AMI, but also to increased morbidity and mortality in this clinical setting. Moreover, vitamin D deficiency seems to predispose to recurrent adverse cardiovascular events, as it is associated with post-infarction complications and cardiac remodeling in patients with AMI. Several mechanisms underlying the association between vitamin D and AMI risk can be involved. Despite these observational and mechanistic data, interventional trials with supplementation of vitamin D are controversial. In this review, we will discuss the evidence on the association between vitamin D deficiency and AMI, in terms of prevalence and prognostic impact, and the possible mechanisms mediating it. Further research in this direction is warranted and it is likely to open up new avenues for reducing the risk of AMI.
Core tip: Vitamin D deficiency is a prevalent condition and it is emerging as a new risk factor for coronary artery disease. Notably, hypovitaminosis D has been reported to be common in patients with acute myocardial infarction, and preliminary studies indicate a possible association with short-term and long-term morbidity and mortality. Although these observational initial proofs, interventional trials with supplementation of vitamin D have yielded controversial results. We herein discuss the current evidence suggesting an association between acute myocardial infarction and vitamin D deficiency, in terms of prevalence and prognostic impact, and the possible underlying mechanisms.
- Citation: Milazzo V, De Metrio M, Cosentino N, Marenzi G, Tremoli E. Vitamin D and acute myocardial infarction. World J Cardiol 2017; 9(1): 14-20
- URL: https://www.wjgnet.com/1949-8462/full/v9/i1/14.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i1.14
Cardiovascular disease, and specifically acute myocardial infarction (AMI), is the main cause of morbidity and mortality in western countries, despite current preventive and therapeutic strategies[1,2].
Besides the traditional, most recognized risk factors for AMI development, new risk factors are emerging with potential relevant therapeutic implications. Among them, hypovitaminosis D has been the focus of recent interest. It is well known that vitamin D insufficiency, or deficiency, is highly prevalent in the general population[3-7]. Traditionally, the most characterized consequences of vitamin D depletion have involved bone metabolism and calcium homeostasis[8]. However, its close association with major cardiovascular risk factors, such as diabetes, hypertension, and chronic kidney disease, and the detection of nuclear vitamin D receptors (VDR) on vascular endothelial cells and cardiomyocytes have paved the way to studies investigating the intriguing link between hypovitaminosis D and cardiac disease[9-11].
Deficiency of vitamin D was shown to be common in AMI, and preliminary studies indicate a possible association with their short-term and long-term prognosis[12-14]. Indeed, vitamin D deficiency seems to predispose to in-hospital and recurrent adverse cardiac events, since it is associated with the number of affected coronary arteries, AMI complications, and cardiac remodeling in patients with AMI[12-14].
In this review, we provide an overview on the currently available evidence supporting the relationship between hypovitaminosis D and AMI, its prognostic relevance, and the possible underlying mechanisms. Finally, we will try to identify challenges and future investigative perspectives in this field.
There are two major forms of vitamin D: Vitamin D2, which is contained in plants and fortified foods, and vitamin D3, which is obtained from aliments or through the conversion of dehydrocholesterol in the skin[11,15]. Of note, the cutaneous synthesis of vitamin D3 from sunlight exposure is the main source of vitamin D in humans. Vitamin D undergoes hydroxylation in the liver to 25-hydroxyvitamin D - its main circulating form in the blood - and then in the kidney to 1,25-dihydroxyvitamin D. The 1,25(OH) vitamin D3 reaches the nucleus where, by binding to its receptors, it regulates the transcription and function of more than 200 genes[16,17]. The VDR, which are expressed in enterocytes, osteoblasts, parathyroid glands, distal renal tubule cells, regulate calcium homeostasis and bone metabolism. Recent investigations have also demonstrated their presence on endothelial cells, lymphocytes, macrophages, smooth vascular muscle cells, beta-pancreatic cells and cardiomyocytes, through which vitamin D3 mediates cardiovascular effects[18-20].
There is no consensus on how to define vitamin D deficiency, and this introduces significant difficulties in conducting epidemiological studies in this field[21-24]. The most widely accepted definition for normal vitamin D serum levels, according to the United States Endocrine Society guideline recommendations, is ≥ 30 ng/mL. Vitamin D insufficiency is characterized by levels of 21-29 ng/mL, while its deficiency by levels ≤ 20 ng/mL[25]. Vitamin D deficiency is the most common nutritional deficiency worldwide in both children and adults[26]. In the United States and Europe, > 40% of the adult population has low vitamin D levels[26]. The Third National Health and Examination Survey (NHANES III) reports a high prevalence of vitamin D deficiency and its rapid increase, going from 55% in the period 1988-1994 to 77% in the years 2001-2004[27,28]. The main causes of vitamin D deficiency are listed in Table 1.
| Age |
| Increased distance from the equator |
| Winter season |
| Darkly pigmented skin |
| Institutionalized/housebound |
| Sunscreens and cover-up clothing |
| Air pollution |
| Smoking |
| Obesity |
| Physical inactivity |
| Malabsorption |
| Chronic kidney disease |
| Liver disease |
| Drugs (glucocorticoids, antirejection medications, human immunodeficiency virus medications, antiepileptic drugs, etc.) |
A growing amount of data has highlighted the potential link between vitamin D and cardiovascular disease. Firstly, VDR have been found in the myocardium, as well as in vascular cells[18,29,30]. Secondly, epidemiological studies demonstrated that the incidence of coronary artery disease, diabetes, hypertension, and hypovitaminosis D, increase in proportion to distance from the equator[31]. Cardiac death and prevalence of vitamin D deficiency have also been reported to be at their highest during periods of decreased sunlight exposure (i.e., winter months)[32]. Thirdly, new evidence suggests that vitamin D deficiency has a role in the development of different cardiovascular risk factors, in particular hypertension[33,34], metabolic syndrome[35], and diabetes mellitus[36-38]. Finally, patients with conditions known to be associated with vitamin D deficiency, such as chronic kidney disease and primary hyperparathyroidism, die more frequently from cardiovascular causes than from those related to their underlying disease[39].
Taken together, these findings strongly support the notion that vitamin D is involved in cardiac risk factor development, finally leading to an increased burden in coronary artery disease and to a worse short-term and long-term outcome in AMI patients.
An initial Danish report in 1978 examined vitamin D levels in 75 patients with stable angina, in 53 patients with AMI, and in 409 healthy subjects, and it found that vitamin D levels were significantly lower in patients with angina or AMI than in controls[40]. In 1990, a case control study showed that AMI patients had lower vitamin D levels than controls, and this difference was more pronounced in the winter-spring period[41]. Of note, the relative risk of AMI decreased across increasing quartiles of vitamin D, suggesting an inverse correlation between vitamin D levels and AMI risk[41]. These figures have also been confirmed in more contemporary cohorts. Among 1739 Framingham Offspring Study healthy participants, the rates of major cardiovascular events were 50% and 80% higher in those with vitamin D insufficiency and deficiency, respectively[42]. In particular, subjects with no history of coronary artery disease and vitamin D levels < 10 ng/mL experienced a hazard ratio of 1.8 for developing a first cardiovascular event during a 5-year follow-up compared with subjects with levels > 15 ng/mL[43]. Finally, in 18225 men in the Health Professionals Follow-up Study, low vitamin D levels were associated with a higher risk of AMI, even after controlling for other cardiovascular risk factors and, at 10-year follow-up, subjects with normal vitamin D levels (> 30 ng/mL) had approximately half the risk of AMI[43]. These findings have been recently confirmed in a large meta-analysis that showed an adjusted pooled relative risk of 1.52 for total cardiovascular events when comparing the lowest to the highest categories of baseline circulating vitamin D concentration[44]. Thus, there is growing evidence suggesting that vitamin D deficiency represents a novel risk factor for AMI.
In agreement with these epidemiological data, prospective reports have found a high prevalence of vitamin D deficiency in patients hospitalized with AMI. A multicenter study performed in 239 acute coronary syndrome patients showed that 96% of them had vitamin D levels < 30 ng/mL at hospital presentation[45]. In line with this, Ng et al[13] demonstrated that 74% of AMI patients had low vitamin D levels and, of note, 36% of them had a severe deficiency. Correia et al[46] reported a median serum concentration of vitamin D of 18.5 ng/mL in a cohort of 206 AMI patients (7% with STEMI), and a severe deficiency in 10% of the sample analyzed. Similar findings were also observed by De Metrio et al[12] and Aleksova et al[14], who reported a prevalence of hypovitaminosis D in AMI patients of 89% and 68%, respectively.
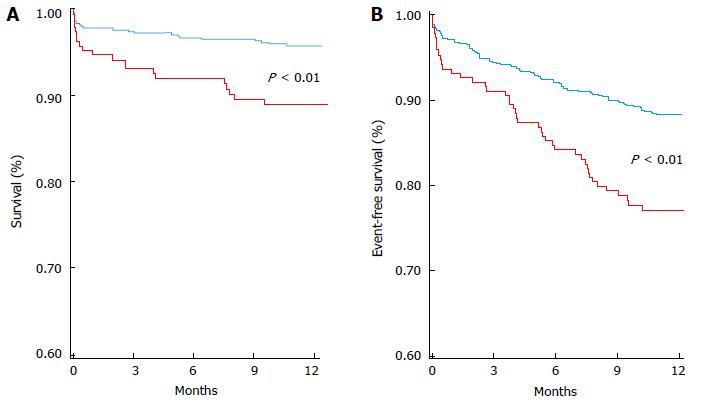
Low vitamin D levels seem to be not only a prevalent independent risk factor for AMI, but also to be associated with a worse outcome when it occurs (Table 2). Correia et al[46] provided the first evidence of the potential independent association between severe deficiency of vitamin D and in-hospital mortality in patients with acute coronary syndromes. Indeed, patients with vitamin D levels < 10 ng/mL had a 24% in-hospital cardiovascular mortality rate, significantly higher than that observed in the remaining patients (4.9%, with a relative risk 4.3). A possible association between hypovitaminosis D and higher in-hospital mortality was also reported by Khalili et al[47] in 139 STEMI patients. However, the study was underpowered to show statistically significant difference in in-hospital mortality between patients with normal and low vitamin D[48]. More robust data have been provided on the long-term clinical implications of low vitamin D levels in AMI. Thus far, the largest study assessing vitamin D and prognosis in 1259 acute coronary syndrome patients is that by Ng et al[13]. In their study, the lowest vitamin D quartile (< 7.3 ng/mL) was associated with long-term major adverse cardiovascular events. Notably, the association was predominantly with re-hospitalization for acute decompensated heart failure or for successive acute coronary syndrome[13]. In agreement with these findings, in our cohort of AMI patients, the lowest quartile of vitamin D was a strong predictor of 1-year mortality (Figure 1)[12]. Of note, vitamin D deficiency was again a borderline independent predictor of in-hospital mortality, possibly due to the relatively low in-hospital mortality rate of our population, and it was associated with the highest risk of several in-hospital major adverse cardiac events. Interestingly, the lowest vitamin D quartile was associated with a higher incidence of bleeding requiring transfusion, although similar baseline hemoglobin values[12]. This is a crucial issue in the setting of AMI, as potent antithrombotic therapy is the mainstay of treatment, and bleeding and transfusions have a detrimental role on outcomes. We also found an association between the lowest vitamin D quartile and acute respiratory insufficiency rate[12]. The higher occurrence of these threatening complications might have contributed to the higher in-hospital mortality risk found in AMI patients and low vitamin D levels.
| Ref. | Study population (n) | Definitions of vitamin D levels (ng/mL) | Prevalence | End points considered | Major findings |
| Lee et al[45] | NSTEMI STEMI (n = 219) | Normal > 30 insufficiency 21-29 deficiency < 20 | 4% were normal 75% were insufficient 21% were deficient | Prevalence and vitamin D correlates | Vitamin D deficiency was more commonly observed in non-Caucasian patients, in diabetics patients, and in those with a higher body mass index |
| Khalili et al[47] | STEMI (n = 139) | Deficiency < 30 | 73% were deficient | In-hospital mortality correlation with MMP-9 levels at 72 h | Inverse correlation between vitamin D and MMP-9 levels |
| Correia et al[46] | UA NSTEMI STEMI (n = 206) | Severe deficiency < 10 | 10% were severely deficient | In-hospital mortality long-term mortality (mean FU 635 d) | A significant higher incidence of in-hospital and long-term mortality in patients with severe vitamin D deficiency |
| Ng et al[13] | NSTEMI STEMI (n = 1259) | Deficiency < 20 | 74% were deficient | long-term incidence of mortality and MACE (median FU 550 d) | A significant higher incidence of MACE in patients with deficient vitamin D levels |
| De Metrio et al[12] | NSTEMI STEMI (n = 814) | Normal > 30 Insufficiency 21-29 Deficiency < 20 | 11% were normal 19% were insufficient 70% were deficient | In-hospital mortality and in-hospital MACE 1-yr mortality and 1-yr re-admission for acute coronary syndrome and acute decompensated heart failure | A higher incidence of in-hospital mortality, mechanical ventilation, and major bleeding in patients with the lowest quartile of vitamin D levels A significant higher incidence of 1-yr mortality and re-hospitalization for acute decompensated heart failure in patients with the lowest quartile of vitamin D levels |
| Aleksova et al[14] | NSTEMI STEMI (n = 478) | Sufficient > 30 Insufficiency 21-30 Deficiency ≤ 20 | 10% were sufficient 22% were insufficient 68% were deficient | Independent predictors of vitamin D deficiency | Older age, female gender, higher body mass index, autumn/winter sampling, and lower GFR predicted vitamin D deficiency |
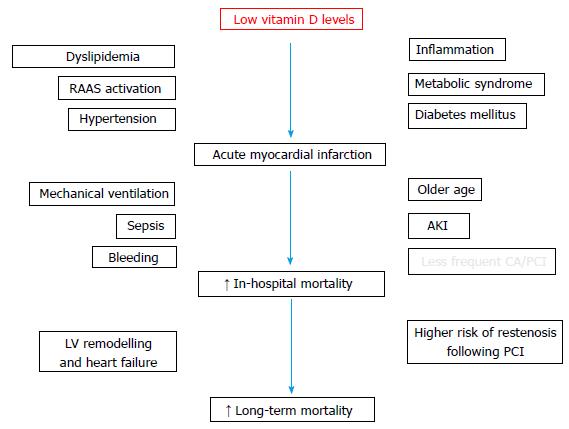
The causal relationship between vitamin D status and outcomes in AMI remains to be elucidated. Indeed, in more than 3000 patients undergoing coronary angiography, a significant association between hypovitaminosis D and lower left ventricular function was shown[49]. Of note, in this report, vitamin D deficiency was associated with deaths due to heart failure and with sudden cardiac deaths[50]. This highlights the possible relevance of vitamin D contribution to several aspects of AMI, such as acute ventricular dysfunction, heart failure progression, post-AMI ventricular remodeling, inflammation, thrombotic/bleeding balance and arrhythmias, which should be more deeply investigated through well-designed studies. Taking together, these considerations, along with older age, higher incidence of well-known cardiovascular risk factors, and lower rate of reperfusion strategy, might explain the worse outcome of AMI patients presenting with low vitamin D levels (Figure 2). A similar prognostic relevance has also been reported in critically ill patients, in whom a low vitamin D status was significantly associated with disease severity and mortality[50-52].
Although many studies suggest a higher cardiovascular risk associated with low vitamin D levels, the data regarding vitamin D supplementation are more sparse and controversial, in terms of primary prevention[53-57]. The potential benefit of vitamin D administration in the early phase of AMI has not been investigated yet. From a clinical point of view, vitamin D levels can be rapidly determined by blood testing and treated by supplementation. It has been demonstrated that a single oral ultra-high dose of vitamin D is able to restore normal levels in 2 d in critically ill patients, with no adverse effects, potentially providing an easy-to-administer dosing regimen for intervention trials in acute cardiovascular settings[58]. Although this evidence was not focused on AMI patients, it may pave the way for new investigations based on the use of a high oral loading dose regimen of vitamin D for restoration of adequate levels within few days. Notably, a dose-response association with cardiovascular risk and mortality has been demonstrated by Wang et al[44], and this was particularly true when short-term outcomes were considered.
Data on vitamin D supplementation in the setting of secondary prevention of AMI are also lacking. Yet, it has been recently demonstrated that high-dose vitamin D supplementation for 1-year in patients with chronic heart failure due to left ventricular systolic dysfunction and vitamin D deficiency, on contemporary optimal medical therapy, resulted in a significant improvement in left ventricular structure and function[59]. Of note, in almost 60% of these patients, the etiology was ischemic heart disease, suggesting a possible beneficial effect on post-AMI ventricular dysfunction[59].
Some studies have also proposed a possible association between low vitamin D and increased levels of cholesterol and of inflammatory markers, in particular C-reactive protein, in the setting of AMI[12,46]. Interestingly, 1-year atorvastatin treatment in patients with AMI determined a marked decrease in cholesterol and an unexpected increase in vitamin D levels, reinforcing the interplay among inflammation, low vitamin D and dyslipidemia[60,61].
Thus far, evidences in this field have been mainly driven by observational cohort studies, and these data are hypothesis-generating. Therefore, whether vitamin D is a risk factor or marker in this clinical setting cannot be inferred from the current literature. Larger studies are needed in order to shed lights on this issue. Because of their health status, frail patients with a high cardiovascular risk burden may spend mostly of their time indoors, which leads to low levels of vitamin D. This is also supported by the fact that such a similar observation has been found in patients with cancer, multiple sclerosis, and psychiatric diseases, potentially supporting the notion that hypovitaminosis D may be simply a marker of health[62]. However, even when adjusted for major confounders, vitamin D status still remains an independent risk factor, as it is significantly linked to incident AMI, worse short-term outcome, and recurrent major adverse cardiovascular events.
Whether vitamin D supplementation can counteract this increased risk in AMI patients is still an unanswered question, which should be investigated in large, well-designed, adequately powered interventional trials.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kettering K, Peteiro J, Petix NR, Sun Z S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5495] [Cited by in RCA: 5243] [Article Influence: 524.3] [Reference Citation Analysis (0)] |
| 2. | Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35:2950-2959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 684] [Cited by in RCA: 733] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 3. | Alkerwi A, Sauvageot N, Gilson G, Stranges S. Prevalence and Correlates of Vitamin D Deficiency and Insufficiency in Luxembourg Adults: Evidence from the Observation of Cardiovascular Risk Factors (ORISCAV-LUX) Study. Nutrients. 2015;7:6780-6796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Holick MF. The vitamin D deficiency pandemic: a forgotten hormone important for health. Public Health Reviews. 2010;32 267-283. |
| 5. | Vandevijvere S, Amsalkhir S, Van Oyen H, Moreno-Reyes R. High prevalence of vitamin D deficiency in pregnant women: a national cross-sectional survey. PLoS One. 2012;7:e43868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Lips P. Vitamin D status and nutrition in Europe and Asia. J Steroid Biochem Mol Biol. 2007;103:620-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 260] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 7. | Harinarayan CV. Prevalence of vitamin D insufficiency in postmenopausal south Indian women. Osteoporos Int. 2005;16:397-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 89] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Bouillon R, Suda T. Vitamin D: calcium and bone homeostasis during evolution. Bonekey Rep. 2014;3:480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 9. | Duplancic D, Cesarik M, Poljak NK, Radman M, Kovacic V, Radic J, Rogosic V. The influence of selective vitamin D receptor activator paricalcitol on cardiovascular system and cardiorenal protection. Clin Interv Aging. 2013;8:149-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Gouni-Berthold I, Krone W, Berthold HK. Vitamin D and cardiovascular disease. Curr Vasc Pharmacol. 2009;7:414-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Dusso AS, Brown AJ, Slatopolsky E. Vitamin D. Am J Physiol Renal Physiol. 2005;289:F8-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 907] [Cited by in RCA: 921] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 12. | De Metrio M, Milazzo V, Rubino M, Cabiati A, Moltrasio M, Marana I, Campodonico J, Cosentino N, Veglia F, Bonomi A. Vitamin D plasma levels and in-hospital and 1-year outcomes in acute coronary syndromes: a prospective study. Medicine (Baltimore). 2015;94:e857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Ng LL, Sandhu JK, Squire IB, Davies JE, Jones DJ. Vitamin D and prognosis in acute myocardial infarction. Int J Cardiol. 2013;168:2341-2346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Aleksova A, Belfiore R, Carriere C, Kassem S, La Carrubba S, Barbati G, Sinagra G. Vitamin D Deficiency in Patients with Acute Myocardial Infarction: An Italian Single-Center Study. Int J Vitam Nutr Res. 2015;85:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 15. | Calvo MS, Whiting SJ, Barton CN. Vitamin D intake: a global perspective of current status. J Nutr. 2005;135:310-316. [PubMed] |
| 16. | Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011;364:248-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 583] [Cited by in RCA: 579] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 17. | Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9399] [Cited by in RCA: 9428] [Article Influence: 523.8] [Reference Citation Analysis (1)] |
| 18. | Somjen D, Weisman Y, Kohen F, Gayer B, Limor R, Sharon O, Jaccard N, Knoll E, Stern N. 25-hydroxyvitamin D3-1alpha-hydroxylase is expressed in human vascular smooth muscle cells and is upregulated by parathyroid hormone and estrogenic compounds. Circulation. 2005;111:1666-1671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 263] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 19. | Zhou C, Lu F, Cao K, Xu D, Goltzman D, Miao D. Calcium-independent and 1,25(OH)2D3-dependent regulation of the renin-angiotensin system in 1alpha-hydroxylase knockout mice. Kidney Int. 2008;74:170-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 295] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 20. | Adams JS, Hewison M. Extrarenal expression of the 25-hydroxyvitamin D-1-hydroxylase. Arch Biochem Biophys. 2012;523:95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 195] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 21. | IOM (Institute of Medicine) Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press, 2011. [DOI] [Full Text] |
| 22. | SACN (Scientific Advisory Committee on Nutrition). Update on vitamin D. Position statement. London: The Stationary Office 2007; . |
| 23. | Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011;86:50-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 495] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 24. | Hilger J, Friedel A, Herr R, Rausch T, Roos F, Wahl DA, Pierroz DD, Weber P, Hoffmann K. A systematic review of vitamin D status in populations worldwide. Br J Nutr. 2014;111:23-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 487] [Cited by in RCA: 536] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 25. | Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6974] [Cited by in RCA: 6846] [Article Influence: 489.0] [Reference Citation Analysis (0)] |
| 26. | Hossein-nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc. 2013;88:720-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 720] [Cited by in RCA: 785] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 27. | Kendrick J, Targher G, Smits G, Chonchol M. 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis. 2009;205:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 288] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 28. | Kim DH, Sabour S, Sagar UN, Adams S, Whellan DJ. Prevalence of hypovitaminosis D in cardiovascular diseases (from the National Health and Nutrition Examination Survey 2001 to 2004). Am J Cardiol. 2008;102:1540-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 263] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 29. | Yao T, Ying X, Zhao Y, Yuan A, He Q, Tong H, Ding S, Liu J, Peng X, Gao E. Vitamin D receptor activation protects against myocardial reperfusion injury through inhibition of apoptosis and modulation of autophagy. Antioxid Redox Signal. 2015;22:633-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 132] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 30. | Kawashima H. Receptor for 1,25-dihydroxyvitamin D in a vascular smooth muscle cell line derived from rat aorta. Biochem Biophys Res Commun. 1987;146:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Fabsitz R, Feinleib M. Geographic patterns in county mortality rates from cardiovascular diseases. Am J Epidemiol. 1980;111:315-328. [PubMed] |
| 32. | Zipes DP. Warning: the short days of winter may be hazardous to your health. Circulation. 1999;100:1590-1592. [PubMed] |
| 33. | Forman JP, Giovannucci E, Holmes MD, Bischoff-Ferrari HA, Tworoger SS, Willett WC, Curhan GC. Plasma 25-hydroxyvitamin D levels and risk of incident hypertension. Hypertension. 2007;49:1063-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 598] [Cited by in RCA: 602] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 34. | Forman JP, Curhan GC, Taylor EN. Plasma 25-hydroxyvitamin D levels and risk of incident hypertension among young women. Hypertension. 2008;52:828-832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 255] [Cited by in RCA: 249] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 35. | Hyppönen E, Boucher BJ, Berry DJ, Power C. 25-hydroxyvitamin D, IGF-1, and metabolic syndrome at 45 years of age: a cross-sectional study in the 1958 British Birth Cohort. Diabetes. 2008;57:298-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 288] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 36. | Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care. 2004;27:2813-2818. [PubMed] |
| 37. | Chonchol M, Scragg R. 25-Hydroxyvitamin D, insulin resistance, and kidney function in the Third National Health and Nutrition Examination Survey. Kidney Int. 2007;71:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 170] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 38. | Mattila C, Knekt P, Männistö S, Rissanen H, Laaksonen MA, Montonen J, Reunanen A. Serum 25-hydroxyvitamin D concentration and subsequent risk of type 2 diabetes. Diabetes Care. 2007;30:2569-2570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 219] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 39. | Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7995] [Cited by in RCA: 8531] [Article Influence: 406.2] [Reference Citation Analysis (0)] |
| 40. | Lund B, Badskjaer J, Lund B, Soerensen OH. Vitamin D and ischaemic heart disease. Horm Metab Res. 1978;10:553-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Scragg R, Jackson R, Holdaway IM, Lim T, Beaglehole R. Myocardial infarction is inversely associated with plasma 25-hydroxyvitamin D3 levels: a community-based study. Int J Epidemiol. 1990;19:559-563. [PubMed] |
| 42. | Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, Benjamin EJ, D’Agostino RB, Wolf M, Vasan RS. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503-511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1750] [Cited by in RCA: 1652] [Article Influence: 97.2] [Reference Citation Analysis (0)] |
| 43. | Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008;168:1174-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 857] [Cited by in RCA: 811] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 44. | Wang L, Song Y, Manson JE, Pilz S, März W, Michaëlsson K, Lundqvist A, Jassal SK, Barrett-Connor E, Zhang C. Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: a meta-analysis of prospective studies. Circ Cardiovasc Qual Outcomes. 2012;5:819-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 470] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 45. | Lee JH, Gadi R, Spertus JA, Tang F, O’Keefe JH. Prevalence of vitamin D deficiency in patients with acute myocardial infarction. Am J Cardiol. 2011;107:1636-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 105] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 46. | Correia LC, Sodré F, Garcia G, Sabino M, Brito M, Kalil F, Barreto B, Lima JC, Noya-Rabelo MM. Relation of severe deficiency of vitamin D to cardiovascular mortality during acute coronary syndromes. Am J Cardiol. 2013;111:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 47. | Khalili H, Talasaz AH, Salarifar M. Serum vitamin D concentration status and its correlation with early biomarkers of remodeling following acute myocardial infarction. Clin Res Cardiol. 2012;101:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 48. | De Metrio M, Milazzo V, Marenzi G. Serum vitamin D concentration status and its correlation with early biomarkers of remodeling following acute myocardial infarction. Clin Res Cardiol. 2012;101:771-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 49. | Pilz S, März W, Wellnitz B, Seelhorst U, Fahrleitner-Pammer A, Dimai HP, Boehm BO, Dobnig H. Association of vitamin D deficiency with heart failure and sudden cardiac death in a large cross-sectional study of patients referred for coronary angiography. J Clin Endocrinol Metab. 2008;93:3927-3935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 383] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 50. | Perron RM, Lee P. Efficacy of high-dose vitamin D supplementation in the critically ill patients. Inflamm Allergy Drug Targets. 2013;12:273-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 51. | Braun AB, Litonjua AA, Moromizato T, Gibbons FK, Giovannucci E, Christopher KB. Association of low serum 25-hydroxyvitamin D levels and acute kidney injury in the critically ill. Crit Care Med. 2012;40:3170-3179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 52. | Moromizato T, Litonjua AA, Braun AB, Gibbons FK, Giovannucci E, Christopher KB. Association of low serum 25-hydroxyvitamin D levels and sepsis in the critically ill. Crit Care Med. 2014;42:97-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 140] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 53. | Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167:1730-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 741] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 54. | Wang L, Manson JE, Song Y, Sesso HD. Systematic review: Vitamin D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. 2010;152:315-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 332] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 55. | Avenell A, MacLennan GS, Jenkinson DJ, McPherson GC, McDonald AM, Pant PR, Grant AM, Campbell MK, Anderson FH, Cooper C. Long-term follow-up for mortality and cancer in a randomized placebo-controlled trial of vitamin D(3) and/or calcium (RECORD trial). J Clin Endocrinol Metab. 2012;97:614-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 187] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 56. | Hsia J, Heiss G, Ren H, Allison M, Dolan NC, Greenland P, Heckbert SR, Johnson KC, Manson JE, Sidney S. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115:846-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 458] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 57. | Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ. 2003;326:469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 880] [Cited by in RCA: 813] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 58. | Amrein K, Sourij H, Wagner G, Holl A, Pieber TR, Smolle KH, Stojakovic T, Schnedl C, Dobnig H. Short-term effects of high-dose oral vitamin D3 in critically ill vitamin D deficient patients: a randomized, double-blind, placebo-controlled pilot study. Crit Care. 2011;15:R104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 133] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 59. | Witte KK, Byrom R, Gierula J, Paton MF, Jamil HA, Lowry JE, Gillott RG, Barnes SA, Chumun H, Kearney LC. Effects of Vitamin D on Cardiac Function in Patients With Chronic HF: The VINDICATE Study. J Am Coll Cardiol. 2016;67:2593-2603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 164] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 60. | Pérez-Castrillón JL, Vega G, Abad L, Sanz A, Chaves J, Hernandez G, Dueñas A. Effects of Atorvastatin on vitamin D levels in patients with acute ischemic heart disease. Am J Cardiol. 2007;99:903-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 118] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 61. | Walter DH, Fichtlscherer S, Britten MB, Rosin P, Auch-Schwelk W, Schächinger V, Zeiher AM. Statin therapy, inflammation and recurrent coronary events in patients following coronary stent implantation. J Am Coll Cardiol. 2001;38:2006-2012. [PubMed] |
| 62. | Eren E, Ellidag HY, Yılmaz A, Aydın Ö, Yılmaz N. No association between vitamin D levels and inflammation markers in patients with acute coronary syndrome. Adv Med Sci. 2015;60:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |