Published online Jul 26, 2014. doi: 10.4330/wjc.v6.i7.610
Revised: February 21, 2014
Accepted: May 14, 2014
Published online: July 26, 2014
Processing time: 235 Days and 10.9 Hours
Post-myocardial infarction (MI), the left ventricle (LV) undergoes a series of events collectively referred to as remodeling. As a result, damaged myocardium is replaced with fibrotic tissue consequently leading to contractile dysfunction and ultimately heart failure. LV remodeling post-MI includes inflammatory, fibrotic, and neovascularization responses that involve regulated cell recruitment and function. Stem cells (SCs) have been transplanted post-MI for treatment of LV remodeling and shown to improve LV function by reduction in scar tissue formation in humans and animal models of MI. The promising results obtained from the application of SCs post-MI have sparked a massive effort to identify the optimal SC for regeneration of cardiomyocytes and the paradigm for clinical applications. Although SC transplantations are generally associated with new tissue formation, SCs also secrete cytokines, chemokines and growth factors that robustly regulate cell behavior in a paracrine fashion during the remodeling process. In this review, the different types of SCs used for cardiomyogenesis, markers of differentiation, paracrine factor secretion, and strategies for cell recruitment and delivery are addressed.
Core tip: Stem cell (SC)-based therapies hold promise to improve damaged myocardium repair and regeneration and thereby restore normal tissue function post-MI. In addition to the potential of SCs to regenerate myocardium, intrinsic properties of SCs such as their ability to home to areas of tissue damage make them an attractive tool for drug delivery. SCs, specifically mesenchymal stem cells, secrete multiple factors that can act in an autocrine and paracrine manner to regulate cell activation, recruitment, and survival during myocardium repair and regeneration.
- Citation: Zamilpa R, Navarro MM, Flores I, Griffey S. Stem cell mechanisms during left ventricular remodeling post-myocardial infarction: Repair and regeneration. World J Cardiol 2014; 6(7): 610-620
- URL: https://www.wjgnet.com/1949-8462/full/v6/i7/610.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i7.610
In the United States alone, it is estimated that a myocardial infarction (MI) occurs every 35 s and approximately 20% of patients that experience a first-MI develop heart failure (HF) within 5 years[1]. An MI is consensually defined as the death of cardiomyocytes after a prolonged period of ischemia causing a progressive decline in cardiac function that ultimately results in HF[2]. Although the mortality associated with acute MI continues to decline as a result of revascularization, the morbidity and mortality caused by HF is on the rise[3,4].
Current post-MI pharmacological therapies such as ACE inhibitors and beta-blockers improve cardiac repair and slow down the progression to HF. However, the growing interest in stem cell (SC) therapies which not only promote repair but also hold promise to regenerate damaged myocardium has sparked a tremendous effort aimed at the development of an effective paradigm for ventricular remodeling post-MI. The possibility that SC therapies can restore cardiac function post-MI and increased evidence that the heart contains resident SCs niches has also contributed to this growing interest[5-7].
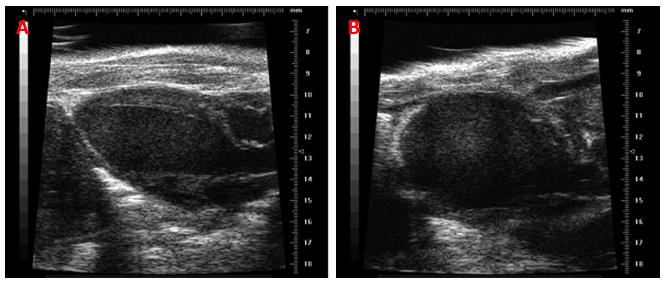
Post-MI, the LV undergoes a remodeling process that results in the replacement of damaged myocardium with a collagen scar[8-10]. During the remodeling process, the normal elliptical shape of the LV (Figure 1A) changes to spherical (Figure 1B) as illustrated by the echocardiogram of the murine heart following MI induced by permanent ligation of the left anterior descending coronary artery. Along with the architectural and structural changes, LV contractile function declines[10].
The magnitude of LV contractile dysfunction is dependent on the extent of the infarct and the wound healing response that follows which includes cardiomyocyte death, inflammatory response, granulation tissue synthesis and granulation tissue maturation and remodeling. Historically, the use of stem cells has automatically been associated with direct replacement of dead cardiomyocytes; however, more recent research has indicated that stem cells possess intricate properties that can regulate other aspects of myocardium repair post-MI. In this review we will focus on the application of stem cells as a therapeutic tool for treatment of myocardial damage post-acute MI and discuss the role of stem cells during cardiac repair and regeneration.
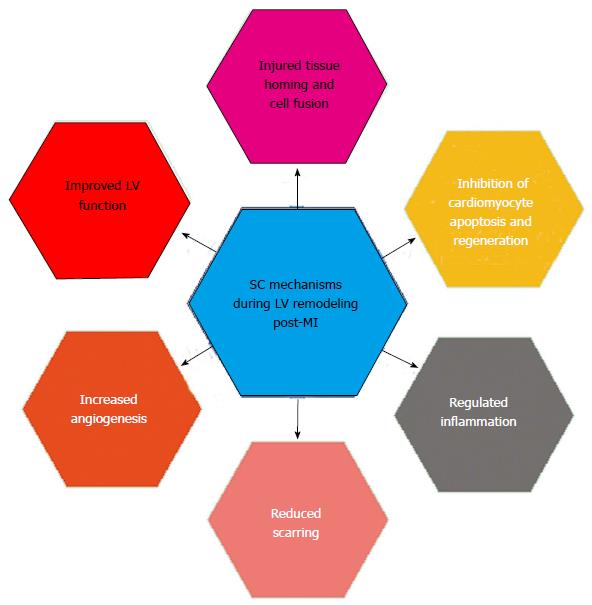
SCs are sophisticated cells with multifunctional properties that can orchestrate the wound healing process post-MI leading to restoration of normal tissue function (Figure 2). One of these properties is the ability to home to areas of injury which has led to the investigation of stem cells for targeted drug delivery[11-13]. Post-MI, SC transplantations have been shown to rescue apoptotic cardiomyocytes and give rise to mature cardiomyocytes through cell fusion[14,15]. In addition, multiple SC types have the capability of differentiating into functional cardiomyocytes which suggest that SCs can be used to replace necrotic or apoptotic cells post-MI. Further, SC transplantations have been shown to regulate the inflammatory response, reduce scarring, and promote angiogenesis through the paracrine effects, all of which lead to improved cardiac function in humans and animal models post-MI.
A major mechanism of action of SC transplantation post-MI that contributes to cardiac repair and regeneration is achieved through cell fusion. Using a combination of in vitro cell culture models and in vivo animal models of MI, fusion rates of SCs with injured cardiomyocytes were shown to significantly increase[14,15]. As a result, there was a decrease in cardiomyocyte apoptosis and an increase in the generation of mature cardiomyocytes[14-16]. Interestingly, inhibition of apoptosis was also achieved through paracrine effects using in vitro co-culture models through activation of the anti-apoptotic AKT/PKB pathway[15,16].
One of the primary goals of SC therapies post-MI is the replacement of dead cardiomyocytes. The current challenge in this regard is to identify the optimal SC for cardiomyocyte replacement. SCs are broadly classified based on their tissue of origin including embryonic vs adult, hematopoietic vs non-hematopoietic, and are further subcategorized by their differentiation potential. Stem cell differentiation potential is their ability to differentiate into specialized cells. By definition, a SC is not committed to one specific lineage and must therefore be given the appropriate differentiation signals if the paradigm calls for a cardiac progenitor or cardiomyocyte-differentiated cell. In Table 1, SCs that have been differentiated into a cardiogenic lineage and the methods of differentiation are listed.
| Cell type | Method of differentiation | Ref. |
| ESCs | EB-mediated differentiation | [17,18] |
| iPS | Transdifferentiation of iPS cell factor-based reprogrammed cardiac fibroblasts using EB-based method + transwell CM co-culture system | [19] |
| Direct reprogramming of cardiac fibroblasts in vivo by local delivery of GMT | [21] | |
| Suspension EB-mediated differentiation of reprogrammed adult fibroblasts | [22,23] | |
| Bone marrow MSC | In vitro differentiation induced by treatment with 5-azacytadine | [27,28] |
| In vivo differentiation of stem cells transplanted and mobilized to damaged myocardium | [29] | |
| In vivo differentiation of stem cells engrafted into the myocardium | [30] | |
| Differentiation using a cardiomyogenic differentiation medium containing insulin, DMSO, and ascorbic acid | [31] | |
| Adipose-derived MSC | Co-culture in direct contact with contracting cardiomyocytes | [37] |
| DMSO at 0.1% for 48 h | [38] | |
| Amniotic fluid SCs | In vivo differentiation of cells transplanted into myocardium | [33] |
| In vitro differentiation through EB formation | [35] | |
| Umbilical cord blood SCs | Co-culture with primary rat neonatal ventricular myocytes | [32] |
| Co-culture with mouse neonatal cardiomyocytes | [34] | |
| Wharton's Jelly MSCs | In vitro differentiation induced by treatment with 5-azacytadine or by culture in cardiomyocyte CM | [36] |
| CS | Co-culture with neonatal rat cardiomyocytes | [41] |
| CSP | Treatment with oxytocin or trichostatin A | [48] |
Embryonic stem cells (ESCs) have been differentiated into cardiomyocytes in vitro and in vivo. Expression of transcription factors GATA-4, myocyte-specific enhancer factors (MEF) 1 and 2C, and Nkx2.5 are commonly used for assessment of cardiomyocyte differentiation. Other factors such as atrial natriuretic factor, myosin light chain (MLC)-2v, myosin heavy chain (MHC), and phospholamban have also been used[16-18].
Human induced pluripotent stem (iPS) cells from various sources, including reprogrammed cardiac fibroblasts, have been differentiated into functional cardiomyocytes[19-23]. Early cardiac lineage differentiation markers include GATA-4, GATA6, Nkx2-5, the T-box 5 (Tbx5), insulin gene enhancer protein-1 (Isl1), and LIM homeodomain transcription factor[20].
To date, the most commonly used SCs for cardiac tissue regeneration have been derived from adult bone marrow. In 2001, Orlic et al[24] demonstrated that c-kit positive cells derived from bone marrow were able to generate de novo myocardium indicating that these cells might be ideal for treatment post-MI. Expansion of this study has demonstrated that bone marrow hematopoietic SCs give rise to cardiomyocytes through cell fusion rather than differentiation. Expression of α-actin, cardiac troponin T, and connexin-43 has been used for cardiac lineage differentiation[25]. In addition to c-kit positive cells, the bone marrow contains fibroblast-like, mesenchymal stromal cells (MSCs) also known as mesenchymal stem cells[26,27]. Studies using bone marrow MSCs have demonstrated that transplanted MSCs mobilize from the bone marrow into the ischemic myocardium post-MI. Consequently, these cells differentiate into cardiomyocytes suggesting that these cells play important roles in repair and regeneration post-MI[27-29]. Expression of α-actin, cardiac titin, cardiac troponin T, desmin, MHC, MEF 2A and 2D, and phospholamban have been used as markers for MSC cardiomyocyte differentiation[27,30,31].
Human-derived adipose MSCs, amniotic fluid SCs, umbilical cord blood hematopoietic cells and MSCs, and Wharton’s Jelly MSCs have also been differentiated to cardiomyocytes. Expression of α-actin, cardiac troponin I, GATA4, MHC, N-cadherin, Nkx2.5, and Tbx5 have been used for cardiac lineage differentiation characterization[32-38].
Interestingly, cardiac tissue homeostasis and regenerative potential has been shown to involve resident cardiac SCs and progenitor cells which have been isolated and expanded from adult human and mouse heart tissue biopsies[39-41]. At least four different types of resident cardiac SCs have been isolated and shown to differentiate into cardiomyocytes[41-47]. Interestingly, three of the four types of resident cardiac SCs identified so far have the ability to form cardiospheres (CS)[41,47]. α-actin and MEF2C are expressed by cardiomyocyte progenitors and developing cardiomyocytes. In addition to cardiosphere-derived cells, cardiac side population cells isolated from neonatal rat hearts have also been differentiated into beating cardiomyocytes by treatment with oxytocin or trichostatin A. In vivo, cardiac side specific cells demonstrated a superb ability to home to injured heart and differentiate into cardiomyocytes. Expression of cardiac transcription factors GATA-4, Nkx2.5 and MEF 2C as well as contractile proteins MHC and MLC-2v have been used for SP cell cardiomyocyte differentiation[48].
In addition to the ability of SCs to potentially replace dead cardiomyocytes, SCs provide a rich source of cytokines and growth factors that can act in an autocrine, paracrine, or endocrine fashion to regulate cell behavior during the inflammatory reaction post-MI[49].
The inflammatory response that follows an MI is necessary and plays a crucial role in proper healing and ventricular remodeling. Post-MI, myocardial necrosis initiates an inflammatory response that includes a cascade of cytokines and chemokines followed by recruitment of neutrophils and macrophages[50,51]. As summarized by Frangogiannis et al[51], the inflammatory reaction clears the damaged myocardium of cellular and matrix debris and activates the reparative process[51]. A prolonged inflammatory reaction leads to adverse remodeling and ventricular dysfunction due to untimely resolution of the acute inflammatory response, increased cardiomyocyte loss and resultant negative downstream effects to extracellular matrix (ECM) metabolism and neovascularization[50].
The most commonly used SC for transplantations post-MI are bone marrow-derived MSCs. The paracrine effects of MSCs have received far more recognition than their ability to replace dead cardiomyocytes. One of the therapeutic goals post-MI is to minimize cardiomyocyte loss. Transplantation of bone marrow MSCs has been shown to reduce cardiomyocyte loss through activation of the cell survival gene Akt[52]. Further, other anti-apoptotic effects of MSCs are postulated to include inhibition of nuclear factor κβ (NF-κB) activity, reduced production of tumor necrosis factor α (TNF-α) and interleukin 6 (IL-6) as well as increased expression of IL-10[53-55].
As part of their involvement in the inflammatory response post-MI, polymorphonuclear granulocytes (PMNs; neutrophils) leave the circulation, infiltrate into the injured myocardium, secrete proteolytic enzymes and reactive oxygen species, and clear cellular and ECM debris[56,57]. Increased production of IL-6 by MSC’s has been shown to prevent apoptosis by activated neutrophils thereby increasing the lifespan of neutrophils through STAT3 transcription factors[58-60]. In addition, the increased production of IL-6 regulates neutrophil activation by attenuation of the respiratory burst[59,60].
Macrophages in the injured myocardium undergo a biphasic activation that begins with a pro-inflammatory phase (also known as M1 or classically activated) that is followed by an overlapping anti-inflammatory phase (also known as M2 or alternatively activated)[61,62]. The macrophage polarization switch from M1 to M2 is a key event in myocardium repair[51,63]. MSC transplantations post-MI increase the number of M2 macrophages[64]. While the mechanism is still unclear, it is likely mediated through paracrine effects that include CCL2, galectin-1, interferon-γ, IL-1β, indoleamine-2,3-dioxygenase, IL-4, IL-6, IL-10, IL-13, prostaglandin-E2, TNF-α, NF-κB, nitric oxide, heme oxygenase-1, hepatocyte growth factor, transforming growth factor-b1, and Human Leukocyte Antigen-G5[53,64,65].
MSC paracrine factors have also been shown to suppress T cell, natural killer cell, and B cell proliferation and attenuate the maturation of dendritic cells through paracrine factors as listed in Table 2[60,66-68].
| Factor | Outcome | Ref. |
| ↑Akt | Reduction cardiomyocyte loss | [52] |
| ↓ NF-κβ | Anti-apoptotic effects | [53-55] |
| ↓ TNF-α | Anti-apoptotic effects | [53-55] |
| ↓ IL-6 | Anti-apoptotic effects | [53-55] |
| ↑ IL-10 | Anti-apoptotic effects | [53-55] |
| ↑ IL-6 | Prevention activated neutrophil apoptosis via Stat3; regulation of neutrophil activation | [56-60] |
| ↑ IL-10, ↑TNF-α, and ↑ IL-6 | Macrophage M2 polarization | [53,61-65] |
| ↓ Collagen I and III, ↓ TIMP-1 and ↓TGF-β | Reduction in fibrosis and scar size | [55,69-76] |
| ↑ VEGF | Promote angiogenesis; improved contractile function | [77-86] |
| ↑ IL-6 | DC maturation inhibition | [60,66-68] |
| ↑ IDO and ↑PGE2 | Reduced T cell activation | [60,66-68] |
| ↑ IDO and ↑PGE2 | Decreased NK proliferation | [60] |
| Factor to be identified | B-Cell arrest | [60] |
Post-MI, necrotic cardiomyocytes are replaced with a fibrous scar. The extent of damaged tissue degradation and subsequent production of a provisional ECM affects scar thickness which in turn influences contractility of the surrounding myocardium. An increased degradation of ECM results in wall thinning and the development of aneurysms and LV rupture while an increased production of ECM results in fibrosis and can predispose the LV to HF[69]. Interestingly, SC transplantations post-MI have been shown to regulate scar formation post-MI and improve ventricular function.
Transplantation of beating cardiomyocytes produced in vitro from ESCs has been shown to attenuate scar thinning and increase fractional shortening post-MI[70]. iPS cell therapy in the mouse permanent ligation model has also been shown to reduce wall thinning post-MI[71]. Additionally, MSC transplantations have been shown to reduce fibrosis and scar size[55,72-74]. Studies by Xu and colleagues demonstrated that MSC transplantations in rats post-MI regulate LV remodeling by decreasing mRNA expression and protein levels of TGF-β, type I and type III collagens, and tissue inhibitor of metalloproteinase (TIMP)-1[75]. Interestingly, in sheep, MSC progenitor cell-injections into the border zone altered collagen dynamics in a cell concentration-dependent manner as a result of spatial changes in matrix metalloproteinases (MMPs) and TIMPs. MMPs -1, - 2, -3, -7, -9, -13, MT1-MMP, and TIMPs -1, -2, -4 were differentially altered in the remote, border zone, and infarct zones post-injection[76].
Angiogenesis is essential for myocardium repair and scar formation post-MI, and paracrine factors released following SC transplantations promote angiogenesis[77,78]. MSCs that engraft after transplantation post MI have been shown to express endothelial cell markers[79,80]. Consistent with these findings, MSCs have also been shown to secrete significantly elevated levels of vascular endothelial growth factor (VEGF). Concomitantly, capillary density increases in the infarct region contributing to improved regional and contractile function[81-83]. It is important to note that MSCs, preconditioned under hypoxic conditions, have an enhanced capacity to stimulate vascularization compared to MSCs cultured under normoxic conditions due to increased expression of VEGF, angiopoietin-1, and survival post-transplantation[84-86].
Several strategies have been used for SC therapeutic applications post-MI. These include cell infusion intravenously, intramyocardial injections, intracoronary applications, endocardial applications, and engineered delivery methods such as cardiac patches[87,88]. For SC recruitment, identification of chemoattractants that are responsible for SCs homing to damaged myocardium has shown an improvement in repair and ventricular function post-MI. Overexpression of stromal cell-derived factor-1 by transfected fibroblasts injected into the peri-infarct zone increased hematopoietic SC homing and improved fractional shortening in the rat MI model[89]. Monocyte chemotactic protein-3 also delivered in a similar fashion via transfected fibroblasts was shown to increase MSC engraftment. Although no significant regeneration of cardiomyocytes was observed, fractional shortening increased and LV end diastolic dimensions decreased[90]. In the porcine MI model, the combination of insulin growth factor-1 and hepatocyte growth factor activated endogenous cardiac SCs resulting in regeneration of cardiomyocytes and angiogenesis as well as improved cardiac function[91]. Interestingly, thymosin β4 has also been shown to play important roles in epicardial progenitor cell mobilization in the mouse heart for neovascularization[92,93].
For delivery, biological and synthetic scaffolds used as vehicles for SC transplantations have shown improvement in cell survival, engraftment and cardiomyogenesis. In the rat MI model, transplanted cardiac SCs using nano-topographical hydrogel patches that mimicked the native cardiac ECM improved cell integration, retention and myocardium regeneration[94]. Similarly, cardiac patches containing adipose stromal vascular cells increased coronary blood flow and significantly improved ejection fraction post-MI[95,96]. The combination of a hydrogel patch with encapsulation of MSCs, as designed by Levit and colleagues, improves cell survival and takes full advantage of MSC paracrine factors. In addition to significantly reduced scar size, delivery of encapsulated MSCs increased peri-infarct microvasculature and improved ejection fraction in the rat MI model[97].
Although numerous studies in humans and animal models have demonstrated that SC transplantations post-MI are safe and can improve cardiac healing and function, several common limitations associated with SC transplantations have been reported. The most common issues with SC transplantations for ventricular remodeling post-MI include reduced cell survival and engraftment which ultimately result in diminished cardiac regeneration and limited functional benefits. In human clinical trials, 3.2% of bone marrow SCs remained 24 h post-infusion, and in agreement with this outcome, other studies report less than 10% SC retention in human and animal studies[97-102]. Further, SCs that do engraft may differentiate into other lineages such as endothelial cells and fibroblasts rather than cardiomyocytes[103-105]. With regard to delivery methods, intravenous infusions may have decreased efficacy due to entrapment of cells in non-target tissues and organs such as bone marrow, lungs, liver and spleen[106,107]. Similarly, intracoronary and intramyocardial delivered cell retention is also limited and may reduce the efficacy of the transplanted cells due to the hostile milieu of the damaged heart[108,109]. Other reported issues with SC delivery methods include the potential for microembolism formation (intravenously and intracoronary), and the potential to induce arrhythmias (intracoronary and intramyocardial)[87,88].
The ultimate goal of SC applications is the translation of what has been learned in the laboratory to the production of safe and effective therapies for attenuation of adverse LV remodeling. In Table 3, the results from the most recently published clinical trials of SC therapies in treatment of myocardial damage post-acute MI are listed. In addition to the feasibility of cell delivery, the safety associated with SC transplantations continues to evolve in clinical trials. Conversely, common issues such as standardization of methodology (including cell dosing, cell product formulation, and timing of transplantation) and the innate heterogeneity of study populations which include other clinical factors such as advanced aging and diabetes hinder interpretation of trial outcomes resulting in the need for a larger-scale study[100-114]. On this front, it is very encouraging to see a significant increase in the number of clinical trials being performed across the globe. The Alliance for Regenerative Medicine annual report for 2012-2013 indicates there were 326 industry-sponsored cell therapy trials ongoing in early 2013. The report further indicates that the number of early to mid-stage cell therapy trials in cardiovascular-related diseases ranks second only to cell therapy studies involving cancer[115].
| Clinical trial | Outcome | Ref. | |
| 2010 | Influence of bone marrow stem cells on left ventricular perfusion and ejection fraction in patients with acute myocardial infarction of anterior wall: Randomized clinical trial | Slight improvement of myocardial profusion | [109] |
| 2011 | HEBE trial | No significant improvement on regional or global function | [110] |
| 2011 | Late TIME trial | No improvement on global or regional function at 6 mo | [111] |
| 2012 | Stem cell treatment for acute myocardial infarction | Reduced LVESV, LVEDV, and infarct size | [109] |
| 2012 | CADUCEUS trial | Reduced scar mass, increased myocardium viability, regional contractility and wall thickness | [112] |
| 2012 | Enhanced mobilization of the bone marrow-derived circulating progenitor cells by intracoronary freshly isolated bone marrow cells transplantation in patients with acute myocardial infarction | Feasibility, safety, and improvement on recovery of LV contractility | [113] |
| 2013 | The C-CURE trial | Feasibility, safety and improved LV ejection fraction | [114] |
A more specific review of acute MI clinical trials reveals that there were 36 open studies registered under “acute myocardial infarction and stem cells”. For congestive heart disease clinical trials the search revealed that there were 48 open studies registered under “congestive heart failure and stem cells” as of the writing of this review. Of these studies, there were 16 listed in phase 1 trials, 25 phase 2 trials, and 9 phase 3 trials (note that some studies are listed in overlapping phases). The majority of these studies are being conducted in the European Union and the United States with 15 and 12 registered studies, respectively[116].
The results from post-MI SC transplantations in animal models and humans have provided promising results in reducing scar formation and improved LV function which are achieved primarily through paracrine effects. While a great deal of information has been obtained in the past two decades on the roles SCs play in the post-MI setting, additional studies are needed to improve the efficacy of stem cell transplantations post-MI. Further, a consensus on the best time to initiate treatment, dosage, and delivery method is needed.
In summary, we have reviewed the current literature on the roles SCs play during LV remodeling post-MI. This evaluation includes different types of SCs with cardiomyogenic potential, markers of differentiation, trophic effects for the inflammatory, fibrotic and vascularization responses as well as strategies for cell homing and delivery post-MI.
The authors would like to thank Dr. Merry L. Lindsey for kindly providing the echocardiograms for the murine permanent ligation MI model.
P- Reviewer: Dominguez-Rodriguez A, Grignola JC, Gong KZ, Shah R S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS. Executive summary: heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:188-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 912] [Cited by in RCA: 950] [Article Influence: 73.1] [Reference Citation Analysis (0)] |
| 2. | Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3050] [Cited by in RCA: 2990] [Article Influence: 119.6] [Reference Citation Analysis (0)] |
| 3. | Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS. Executive summary: heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 971] [Cited by in RCA: 955] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 4. | Pocock SJ, Wang D, Pfeffer MA, Yusuf S, McMurray JJ, Swedberg KB, Ostergren J, Michelson EL, Pieper KS, Granger CB. Predictors of mortality and morbidity in patients with chronic heart failure. Eur Heart J. 2006;27:65-75. [PubMed] |
| 5. | Beltrami AP, Urbanek K, Kajstura J, Yan SM, Finato N, Bussani R, Nadal-Ginard B, Silvestri F, Leri A, Beltrami CA. Evidence that human cardiac myocytes divide after myocardial infarction. N Engl J Med. 2001;344:1750-1757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1046] [Cited by in RCA: 919] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 6. | Bearzi C, Rota M, Hosoda T, Tillmanns J, Nascimbene A, De Angelis A, Yasuzawa-Amano S, Trofimova I, Siggins RW, Lecapitaine N. Human cardiac stem cells. Proc Natl Acad Sci USA. 2007;104:14068-14073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 776] [Cited by in RCA: 704] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 7. | Ellison GM, Vicinanza C, Smith AJ, Aquila I, Leone A, Waring CD, Henning BJ, Stirparo GG, Papait R, Scarfò M. Adult c-kit(pos) cardiac stem cells are necessary and sufficient for functional cardiac regeneration and repair. Cell. 2013;154:827-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 404] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 8. | Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990;81:1161-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | St John Sutton M, Lee D, Rouleau JL, Goldman S, Plappert T, Braunwald E, Pfeffer MA. Left ventricular remodeling and ventricular arrhythmias after myocardial infarction. Circulation. 2003;107:2577-2582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Sutton MG, Sharpe N. Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation. 2000;101:2981-2988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1182] [Cited by in RCA: 1278] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 11. | Aboody K, Capela A, Niazi N, Stern JH, Temple S. Translating stem cell studies to the clinic for CNS repair: current state of the art and the need for a Rosetta stone. Neuron. 2011;70:597-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 148] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 12. | Aboody KS, Najbauer J, Danks MK. Stem and progenitor cell-mediated tumor selective gene therapy. Gene Ther. 2008;15:739-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 215] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 13. | Aboody KS, Najbauer J, Metz MZ, D’Apuzzo M, Gutova M, Annala AJ, Synold TW, Couture LA, Blanchard S, Moats RA. Neural stem cell-mediated enzyme/prodrug therapy for glioma: preclinical studies. Sci Transl Med. 2013;5:184ra59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 182] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 14. | Alvarez-Dolado M, Pardal R, Garcia-Verdugo JM, Fike JR, Lee HO, Pfeffer K, Lois C, Morrison SJ, Alvarez-Buylla A. Fusion of bone-marrow-derived cells with Purkinje neurons, cardiomyocytes and hepatocytes. Nature. 2003;425:968-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1199] [Cited by in RCA: 1160] [Article Influence: 52.7] [Reference Citation Analysis (0)] |
| 15. | Yang WJ, Li SH, Weisel RD, Liu SM, Li RK. Cell fusion contributes to the rescue of apoptotic cardiomyocytes by bone marrow cells. J Cell Mol Med. 2012;16:3085-3095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Rosenberg M, Lutz M, Kuhl C, Will R, Eckstein V, Krebs J, Katus HA, Frey N. Coculture with hematopoietic stem cells protects cardiomyocytes against apoptosis via paracrine activation of AKT. J Transl Med. 2012;10:115. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Boheler KR, Czyz J, Tweedie D, Yang HT, Anisimov SV, Wobus AM. Differentiation of pluripotent embryonic stem cells into cardiomyocytes. Circ Res. 2002;91:189-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 514] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 18. | Boheler KR, Crider DG, Tarasova Y, Maltsev VA. Cardiomyocytes derived from embryonic stem cells. Methods Mol Med. 2005;108:417-435. [PubMed] |
| 19. | Jiang B, Dong H, Li Q, Yu Y, Zhang Z, Zhang Y, Wang G, Zhang Z. Differentiation of reprogrammed mouse cardiac fibroblasts into functional cardiomyocytes. Cell Biochem Biophys. 2013;66:309-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Mummery CL, Zhang J, Ng ES, Elliott DA, Elefanty AG, Kamp TJ. Differentiation of human embryonic stem cells and induced pluripotent stem cells to cardiomyocytes: a methods overview. Circ Res. 2012;111:344-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 550] [Article Influence: 42.3] [Reference Citation Analysis (0)] |
| 21. | Qian L, Huang Y, Spencer CI, Foley A, Vedantham V, Liu L, Conway SJ, Fu JD, Srivastava D. In vivo reprogramming of murine cardiac fibroblasts into induced cardiomyocytes. Nature. 2012;485:593-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1000] [Cited by in RCA: 1029] [Article Influence: 79.2] [Reference Citation Analysis (0)] |
| 22. | Zwi-Dantsis L, Huber I, Habib M, Winterstern A, Gepstein A, Arbel G, Gepstein L. Derivation and cardiomyocyte differentiation of induced pluripotent stem cells from heart failure patients. Eur Heart J. 2013;34:1575-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Zwi L, Caspi O, Arbel G, Huber I, Gepstein A, Park IH, Gepstein L. Cardiomyocyte differentiation of human induced pluripotent stem cells. Circulation. 2009;120:1513-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 307] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 24. | Orlic D, Kajstura J, Chimenti S, Bodine DM, Leri A, Anversa P. Bone marrow stem cells regenerate infarcted myocardium. Pediatr Transplant. 2003;7 Suppl 3:86-88. [PubMed] |
| 25. | Nygren JM, Jovinge S, Breitbach M, Säwén P, Röll W, Hescheler J, Taneera J, Fleischmann BK, Jacobsen SE. Bone marrow-derived hematopoietic cells generate cardiomyocytes at a low frequency through cell fusion, but not transdifferentiation. Nat Med. 2004;10:494-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 766] [Cited by in RCA: 719] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 26. | Friedenstein AJ, Chailakhjan RK, Lalykina KS. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 1970;3:393-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Makino S, Fukuda K, Miyoshi S, Konishi F, Kodama H, Pan J, Sano M, Takahashi T, Hori S, Abe H. Cardiomyocytes can be generated from marrow stromal cells in vitro. J Clin Invest. 1999;103:697-705. [PubMed] |
| 29. | Kawada H, Fujita J, Kinjo K, Matsuzaki Y, Tsuma M, Miyatake H, Muguruma Y, Tsuboi K, Itabashi Y, Ikeda Y. Nonhematopoietic mesenchymal stem cells can be mobilized and differentiate into cardiomyocytes after myocardial infarction. Blood. 2004;104:3581-3587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 445] [Cited by in RCA: 411] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 30. | Toma C, Pittenger MF, Cahill KS, Byrne BJ, Kessler PD. Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation. 2002;105:93-98. [PubMed] |
| 31. | Shim WS, Jiang S, Wong P, Tan J, Chua YL, Tan YS, Sin YK, Lim CH, Chua T, Teh M. Ex vivo differentiation of human adult bone marrow stem cells into cardiomyocyte-like cells. Biochem Biophys Res Commun. 2004;324:481-488. [PubMed] |
| 32. | Avitabile D, Crespi A, Brioschi C, Parente V, Toietta G, Devanna P, Baruscotti M, Truffa S, Scavone A, Rusconi F. Human cord blood CD34+ progenitor cells acquire functional cardiac properties through a cell fusion process. Am J Physiol Heart Circ Physiol. 2011;300:H1875-H1884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Fang CH, Jin J, Joe JH, Song YS, So BI, Lim SM, Cheon GJ, Woo SK, Ra JC, Lee YY. In vivo differentiation of human amniotic epithelial cells into cardiomyocyte-like cells and cell transplantation effect on myocardial infarction in rats: comparison with cord blood and adipose tissue-derived mesenchymal stem cells. Cell Transplant. 2012;21:1687-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 34. | Orlandi A, Pagani F, Avitabile D, Bonanno G, Scambia G, Vigna E, Grassi F, Eusebi F, Fucile S, Pesce M. Functional properties of cells obtained from human cord blood CD34+ stem cells and mouse cardiac myocytes in coculture. Am J Physiol Heart Circ Physiol. 2008;294:H1541-H1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Wang H, Chen S, Cheng X, Dou Z, Wang H. [Differentiation of human amniotic fluid stem cells into cardiomyocytes through embryonic body formation]. Shengwu Gongcheng Xuebao. 2008;24:1582-1587. [PubMed] |
| 36. | Wang HS, Hung SC, Peng ST, Huang CC, Wei HM, Guo YJ, Fu YS, Lai MC, Chen CC. Mesenchymal stem cells in the Wharton’s jelly of the human umbilical cord. Stem Cells. 2004;22:1330-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 946] [Cited by in RCA: 916] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 37. | Choi YS, Dusting GJ, Stubbs S, Arunothayaraj S, Han XL, Collas P, Morrison WA, Dilley RJ. Differentiation of human adipose-derived stem cells into beating cardiomyocytes. J Cell Mol Med. 2010;14:878-889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 38. | Okura H, Matsuyama A, Lee CM, Saga A, Kakuta-Yamamoto A, Nagao A, Sougawa N, Sekiya N, Takekita K, Shudo Y. Cardiomyoblast-like cells differentiated from human adipose tissue-derived mesenchymal stem cells improve left ventricular dysfunction and survival in a rat myocardial infarction model. Tissue Eng Part C Methods. 2010;16:417-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 39. | Chimenti I, Gaetani R, Barile L, Forte E, Ionta V, Angelini F, Frati G, Messina E, Giacomello A. Isolation and expansion of adult cardiac stem/progenitor cells in the form of cardiospheres from human cardiac biopsies and murine hearts. Methods Mol Biol. 2012;879:327-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Gaetani R, Ledda M, Barile L, Chimenti I, De Carlo F, Forte E, Ionta V, Giuliani L, D’Emilia E, Frati G. Differentiation of human adult cardiac stem cells exposed to extremely low-frequency electromagnetic fields. Cardiovasc Res. 2009;82:411-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 85] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 41. | Messina E, De Angelis L, Frati G, Morrone S, Chimenti S, Fiordaliso F, Salio M, Battaglia M, Latronico MV, Coletta M. Isolation and expansion of adult cardiac stem cells from human and murine heart. Circ Res. 2004;95:911-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1137] [Cited by in RCA: 1024] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 42. | Beltrami AP, Barlucchi L, Torella D, Baker M, Limana F, Chimenti S, Kasahara H, Rota M, Musso E, Urbanek K. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell. 2003;114:763-776. [PubMed] |
| 43. | Laugwitz KL, Moretti A, Lam J, Gruber P, Chen Y, Woodard S, Lin LZ, Cai CL, Lu MM, Reth M. Postnatal isl1+ cardioblasts enter fully differentiated cardiomyocyte lineages. Nature. 2005;433:647-653. [PubMed] |
| 44. | Martin CM, Meeson AP, Robertson SM, Hawke TJ, Richardson JA, Bates S, Goetsch SC, Gallardo TD, Garry DJ. Persistent expression of the ATP-binding cassette transporter, Abcg2, identifies cardiac SP cells in the developing and adult heart. Dev Biol. 2004;265:262-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 460] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 45. | Matsuura K, Nagai T, Nishigaki N, Oyama T, Nishi J, Wada H, Sano M, Toko H, Akazawa H, Sato T. Adult cardiac Sca-1-positive cells differentiate into beating cardiomyocytes. J Biol Chem. 2004;279:11384-11391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 453] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 46. | Oh H, Bradfute SB, Gallardo TD, Nakamura T, Gaussin V, Mishina Y, Pocius J, Michael LH, Behringer RR, Garry DJ. Cardiac progenitor cells from adult myocardium: homing, differentiation, and fusion after infarction. Proc Natl Acad Sci USA. 2003;100:12313-12318. [PubMed] |
| 47. | Torella D, Ellison GM, Méndez-Ferrer S, Ibanez B, Nadal-Ginard B. Resident human cardiac stem cells: role in cardiac cellular homeostasis and potential for myocardial regeneration. Nat Clin Pract Cardiovasc Med. 2006;3 Suppl 1:S8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 113] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 48. | Tripathi R, Dutta GP, Vishwakarma RA. Comparison of antimalarial efficacy of alpha, beta, and alpha/beta arteether against Plasmodium cynomolgi B infection in monkeys. Am J Trop Med Hyg. 1991;44:560-563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 253] [Cited by in RCA: 218] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 49. | Ting WC. Massive blood transfusion. Singapore Med J. 1991;32:24-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 575] [Cited by in RCA: 633] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 50. | Frangogiannis NG, Smith CW, Entman ML. The inflammatory response in myocardial infarction. Cardiovasc Res. 2002;53:31-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1464] [Cited by in RCA: 1510] [Article Influence: 65.7] [Reference Citation Analysis (0)] |
| 51. | Frangogiannis NG. Regulation of the inflammatory response in cardiac repair. Circ Res. 2012;110:159-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 757] [Cited by in RCA: 899] [Article Influence: 69.2] [Reference Citation Analysis (0)] |
| 52. | Uemura R, Xu M, Ahmad N, Ashraf M. Bone marrow stem cells prevent left ventricular remodeling of ischemic heart through paracrine signaling. Circ Res. 2006;98:1414-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 487] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 53. | Du YY, Zhou SH, Zhou T, Su H, Pan HW, Du WH, Liu B, Liu QM. Immuno-inflammatory regulation effect of mesenchymal stem cell transplantation in a rat model of myocardial infarction. Cytotherapy. 2008;10:469-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 54. | Jiang CY, Gui C, He AN, Hu XY, Chen J, Jiang Y, Wang JA. Optimal time for mesenchymal stem cell transplantation in rats with myocardial infarction. J Zhejiang Univ Sci B. 2008;9:630-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 55. | Li Q, Turdi S, Thomas DP, Zhou T, Ren J. Intra-myocardial delivery of mesenchymal stem cells ameliorates left ventricular and cardiomyocyte contractile dysfunction following myocardial infarction. Toxicol Lett. 2010;195:119-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 56. | Bell D, Jackson M, Nicoll JJ, Millar A, Dawes J, Muir AL. Inflammatory response, neutrophil activation, and free radical production after acute myocardial infarction: effect of thrombolytic treatment. Br Heart J. 1990;63:82-87. [PubMed] |
| 57. | Ma Y, Yabluchanskiy A, Lindsey ML. Neutrophil roles in left ventricular remodeling following myocardial infarction. Fibrogenesis Tissue Repair. 2013;6:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 156] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 58. | Raffaghello L, Bianchi G, Bertolotto M, Montecucco F, Busca A, Dallegri F, Ottonello L, Pistoia V. Human mesenchymal stem cells inhibit neutrophil apoptosis: a model for neutrophil preservation in the bone marrow niche. Stem Cells. 2008;26:151-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 348] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 59. | van den Akker F, Deddens JC, Doevendans PA, Sluijter JP. Cardiac stem cell therapy to modulate inflammation upon myocardial infarction. Biochim Biophys Acta. 2013;1830:2449-2458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 60. | van den Akker F, de Jager SCA, Sluijter JPG. Mesenchymal Stem Cell Therapy for Cardiac Inflammation: Immunomodulatory Properties and the Influence of Toll-Like Receptors. Mediators of Inflammation. 2013;2013:1-13. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 86] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 61. | Nahrendorf M, Pittet MJ, Swirski FK. Monocytes: protagonists of infarct inflammation and repair after myocardial infarction. Circulation. 2010;121:2437-2445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 653] [Cited by in RCA: 625] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 62. | Zamilpa R, Ibarra J, de Castro Brás LE, Ramirez TA, Nguyen N, Halade GV, Zhang J, Dai Q, Dayah T, Chiao YA. Transgenic overexpression of matrix metalloproteinase-9 in macrophages attenuates the inflammatory response and improves left ventricular function post-myocardial infarction. J Mol Cell Cardiol. 2012;53:599-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 63. | Swirski FK, Nahrendorf M. Macrophage-stem cell crosstalk after myocardial infarction. J Am Coll Cardiol. 2013;62:1902-1904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 64. | Ben-Mordechai T, Holbova R, Landa-Rouben N, Harel-Adar T, Feinberg MS, Abd Elrahman I, Blum G, Epstein FH, Silman Z, Cohen S. Macrophage subpopulations are essential for infarct repair with and without stem cell therapy. J Am Coll Cardiol. 2013;62:1890-1901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 212] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 65. | Bernardo ME, Fibbe WE. Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell. 2013;13:392-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 903] [Cited by in RCA: 1056] [Article Influence: 96.0] [Reference Citation Analysis (0)] |
| 66. | Nauta AJ, Kruisselbrink AB, Lurvink E, Willemze R, Fibbe WE. Mesenchymal stem cells inhibit generation and function of both CD34+-derived and monocyte-derived dendritic cells. J Immunol. 2006;177:2080-2087. [PubMed] |
| 67. | Pradier A, Passweg J, Villard J, Kindler V. Human bone marrow stromal cells and skin fibroblasts inhibit natural killer cell proliferation and cytotoxic activity. Cell Transplant. 2011;20:681-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 68. | Glennie S, Soeiro I, Dyson PJ, Lam EW, Dazzi F. Bone marrow mesenchymal stem cells induce division arrest anergy of activated T cells. Blood. 2005;105:2821-2827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 825] [Cited by in RCA: 832] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 69. | Zamilpa R, Lindsey ML. Extracellular matrix turnover and signaling during cardiac remodeling following MI: causes and consequences. J Mol Cell Cardiol. 2010;48:558-563. [PubMed] |
| 70. | Leor J, Gerecht S, Cohen S, Miller L, Holbova R, Ziskind A, Shachar M, Feinberg MS, Guetta E, Itskovitz-Eldor J. Human embryonic stem cell transplantation to repair the infarcted myocardium. Heart. 2007;93:1278-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 140] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 71. | Yamada S, Nelson TJ, Kane GC, Martinez-Fernandez A, Crespo-Diaz RJ, Ikeda Y, Perez-Terzic C, Terzic A. Induced pluripotent stem cell intervention rescues ventricular wall motion disparity, achieving biological cardiac resynchronization post-infarction. J Physiol. 2013;591:4335-4349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 72. | Berry MF, Engler AJ, Woo YJ, Pirolli TJ, Bish LT, Jayasankar V, Morine KJ, Gardner TJ, Discher DE, Sweeney HL. Mesenchymal stem cell injection after myocardial infarction improves myocardial compliance. Am J Physiol Heart Circ Physiol. 2006;290:H2196-H2203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 504] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 73. | Fazel S, Chen L, Weisel RD, Angoulvant D, Seneviratne C, Fazel A, Cheung P, Lam J, Fedak PW, Yau TM. Cell transplantation preserves cardiac function after infarction by infarct stabilization: augmentation by stem cell factor. J Thorac Cardiovasc Surg. 2005;130:1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 74. | Williams AR, Suncion VY, McCall F, Guerra D, Mather J, Zambrano JP, Heldman AW, Hare JM. Durable scar size reduction due to allogeneic mesenchymal stem cell therapy regulates whole-chamber remodeling. J Am Heart Assoc. 2013;2:e000140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 75. | Xu X, Xu Z, Xu Y, Cui G. Effects of mesenchymal stem cell transplantation on extracellular matrix after myocardial infarction in rats. Coron Artery Dis. 2005;16:245-255. [PubMed] |
| 76. | Dixon JA, Gorman RC, Stroud RE, Bouges S, Hirotsugu H, Gorman JH, Martens TP, Itescu S, Schuster MD, Plappert T. Mesenchymal cell transplantation and myocardial remodeling after myocardial infarction. Circulation. 2009;120:S220-S229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 77. | Barandon L, Couffinhal T, Dufourcq P, Ezan J, Costet P, Daret D, Deville C, Duplàa C. Frizzled A, a novel angiogenic factor: promises for cardiac repair. Eur J Cardiothorac Surg. 2004;25:76-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 78. | Zhao T, Zhao W, Chen Y, Ahokas RA, Sun Y. Vascular endothelial growth factor (VEGF)-A: role on cardiac angiogenesis following myocardial infarction. Microvasc Res. 2010;80:188-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 79. | Boomsma RA, Geenen DL. Mesenchymal stem cells secrete multiple cytokines that promote angiogenesis and have contrasting effects on chemotaxis and apoptosis. PLoS One. 2012;7:e35685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 253] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 80. | Nagaya N, Kangawa K, Itoh T, Iwase T, Murakami S, Miyahara Y, Fujii T, Uematsu M, Ohgushi H, Yamagishi M. Transplantation of mesenchymal stem cells improves cardiac function in a rat model of dilated cardiomyopathy. Circulation. 2005;112:1128-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 81. | Tomita S, Li RK, Weisel RD, Mickle DA, Kim EJ, Sakai T, Jia ZQ. Autologous transplantation of bone marrow cells improves damaged heart function. Circulation. 1999;100:II247-II256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 482] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 82. | Tomita S, Mickle DA, Weisel RD, Jia ZQ, Tumiati LC, Allidina Y, Liu P, Li RK. Improved heart function with myogenesis and angiogenesis after autologous porcine bone marrow stromal cell transplantation. J Thorac Cardiovasc Surg. 2002;123:1132-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 227] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 83. | Zhang S, Jia Z, Ge J, Gong L, Ma Y, Li T, Guo J, Chen P, Hu Q, Zhang P. Purified human bone marrow multipotent mesenchymal stem cells regenerate infarcted myocardium in experimental rats. Cell Transplant. 2005;14:787-798. [PubMed] |
| 84. | Hu X, Yu SP, Fraser JL, Lu Z, Ogle ME, Wang JA, Wei L. Transplantation of hypoxia-preconditioned mesenchymal stem cells improves infarcted heart function via enhanced survival of implanted cells and angiogenesis. J Thorac Cardiovasc Surg. 2008;135:799-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 466] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 85. | Imanishi Y, Saito A, Komoda H, Kitagawa-Sakakida S, Miyagawa S, Kondoh H, Ichikawa H, Sawa Y. Allogenic mesenchymal stem cell transplantation has a therapeutic effect in acute myocardial infarction in rats. J Mol Cell Cardiol. 2008;44:662-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 86. | Roy R, Brodarac A, Kukucka M, Kurtz A, Becher PM, Jülke K, Choi YH, Pinzur L, Chajut A, Tschöpe C. Cardioprotection by placenta-derived stromal cells in a murine myocardial infarction model. J Surg Res. 2013;185:70-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 87. | Wu KH, Han ZC, Mo XM, Zhou B. Cell delivery in cardiac regenerative therapy. Ageing Res Rev. 2012;11:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 88. | Donndorf P, Strauer BE, Haverich A, Steinhoff G. Stem cell therapy for the treatment of acute myocardial infarction and chronic ischemic heart disease. Curr Pharm Biotechnol. 2013;14:12-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 89. | Askari AT, Unzek S, Popovic ZB, Goldman CK, Forudi F, Kiedrowski M, Rovner A, Ellis SG, Thomas JD, DiCorleto PE. Effect of stromal-cell-derived factor 1 on stem-cell homing and tissue regeneration in ischaemic cardiomyopathy. Lancet. 2003;362:697-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 984] [Cited by in RCA: 942] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 90. | Schenk S, Mal N, Finan A, Zhang M, Kiedrowski M, Popovic Z, McCarthy PM, Penn MS. Monocyte chemotactic protein-3 is a myocardial mesenchymal stem cell homing factor. Stem Cells. 2007;25:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 193] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 91. | Ellison GM, Torella D, Dellegrottaglie S, Perez-Martinez C, Perez de Prado A, Vicinanza C, Purushothaman S, Galuppo V, Iaconetti C, Waring CD. Endogenous cardiac stem cell activation by insulin-like growth factor-1/hepatocyte growth factor intracoronary injection fosters survival and regeneration of the infarcted pig heart. J Am Coll Cardiol. 2011;58:977-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 183] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 92. | Smart N, Risebro CA, Melville AA, Moses K, Schwartz RJ, Chien KR, Riley PR. Thymosin beta4 induces adult epicardial progenitor mobilization and neovascularization. Nature. 2007;445:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 551] [Cited by in RCA: 507] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 93. | Smart N, Dubé KN, Riley PR. Epicardial progenitor cells in cardiac regeneration and neovascularisation. Vascul Pharmacol. 2013;58:164-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 94. | Kim DH, Kshitiz RR, Kim P, Ahn EH, Kim HN, Marbán E, Suh KY, Levchenko A. Nanopatterned cardiac cell patches promote stem cell niche formation and myocardial regeneration. Integr Biol (Camb). 2012;4:1019-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 95. | Leblanc AJ, Touroo JS, Hoying JB, Williams SK. Adipose stromal vascular fraction cell construct sustains coronary microvascular function after acute myocardial infarction. Am J Physiol Heart Circ Physiol. 2012;302:H973-H982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 96. | Leblanc AJ, Nguyen QT, Touroo JS, Aird AL, Chang RC, Ng CK, Hoying JB, Williams SK. Adipose-derived cell construct stabilizes heart function and increases microvascular perfusion in an established infarct. Stem Cells Transl Med. 2013;2:896-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 97. | Levit RD, Landázuri N, Phelps EA, Brown ME, García AJ, Davis ME, Joseph G, Long R, Safley SA, Suever JD. Cellular encapsulation enhances cardiac repair. J Am Heart Assoc. 2013;2:e000367. [PubMed] |
| 98. | Assis AC, Carvalho JL, Jacoby BA, Ferreira RL, Castanheira P, Diniz SO, Cardoso VN, Goes AM, Ferreira AJ. Time-dependent migration of systemically delivered bone marrow mesenchymal stem cells to the infarcted heart. Cell Transplant. 2010;19:219-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 117] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 99. | Clifford DM, Fisher SA, Brunskill SJ, Doree C, Mathur A, Watt S, Martin-Rendon E. Stem cell treatment for acute myocardial infarction. Cochrane Database Syst Rev. 2012;2:CD006536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 100. | Goussetis E, Manginas A, Koutelou M, Peristeri I, Theodosaki M, Kollaros N, Leontiadis E, Theodorakos A, Paterakis G, Karatasakis G. Intracoronary infusion of CD133+ and CD133-CD34+ selected autologous bone marrow progenitor cells in patients with chronic ischemic cardiomyopathy: cell isolation, adherence to the infarcted area, and body distribution. Stem Cells. 2006;24:2279-2283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 76] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 101. | Hofmann M, Wollert KC, Meyer GP, Menke A, Arseniev L, Hertenstein B, Ganser A, Knapp WH, Drexler H. Monitoring of bone marrow cell homing into the infarcted human myocardium. Circulation. 2005;111:2198-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 729] [Cited by in RCA: 671] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 102. | Huang XP, Sun Z, Miyagi Y, McDonald Kinkaid H, Zhang L, Weisel RD, Li RK. Differentiation of allogeneic mesenchymal stem cells induces immunogenicity and limits their long-term benefits for myocardial repair. Circulation. 2010;122:2419-2429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 283] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 103. | Forrester JS, Price MJ, Makkar RR. Stem cell repair of infarcted myocardium: an overview for clinicians. Circulation. 2003;108:1139-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 104. | Wang JS, Shum-Tim D, Chedrawy E, Chiu RC. The coronary delivery of marrow stromal cells for myocardial regeneration: pathophysiologic and therapeutic implications. J Thorac Cardiovasc Surg. 2001;122:699-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 156] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 105. | Carlson S, Trial J, Soeller C, Entman ML. Cardiac mesenchymal stem cells contribute to scar formation after myocardial infarction. Cardiovasc Res. 2011;91:99-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 106. | Barbash IM, Chouraqui P, Baron J, Feinberg MS, Etzion S, Tessone A, Miller L, Guetta E, Zipori D, Kedes LH. Systemic delivery of bone marrow-derived mesenchymal stem cells to the infarcted myocardium: feasibility, cell migration, and body distribution. Circulation. 2003;108:863-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 916] [Cited by in RCA: 898] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 107. | Fischer UM, Harting MT, Jimenez F, Monzon-Posadas WO, Xue H, Savitz SI, Laine GA, Cox CS. Pulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effect. Stem Cells Dev. 2009;18:683-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 794] [Cited by in RCA: 925] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 108. | Hou D, Youssef EA, Brinton TJ, Zhang P, Rogers P, Price ET, Yeung AC, Johnstone BH, Yock PG, March KL. Radiolabeled cell distribution after intramyocardial, intracoronary, and interstitial retrograde coronary venous delivery: implications for current clinical trials. Circulation. 2005;112:I150-I156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 325] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 109. | Grajek S, Popiel M, Gil L, Breborowicz P, Lesiak M, Czepczynski R, Sawinski K, Straburzynska-Migaj E, Arazkiewicz A, Czyz A. Influence of bone marrow stem cells on left ventricular perfusion and ejection fraction in patients with acute myocardial infarction of anterior wall: randomized clinical trial. Eur Heart J. 2010;31:691-702. [DOI] [Full Text] |
| 110. | Hirsch A, Nijveldt R, van der Vleuten PA, Tijssen JG, van der Giessen WJ, Tio RA, Waltenberger J, ten Berg JM, Doevendans PA, Aengevaeren WR. Intracoronary infusion of mononuclear cells from bone marrow or peripheral blood compared with standard therapy in patients after acute myocardial infarction treated by primary percutaneous coronary intervention: results of the randomized controlled HEBE trial. Eur Heart J. 2011;32:1736-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 111. | Traverse JH, Henry TD, Ellis SG, Pepine CJ, Willerson JT, Zhao DX, Forder JR, Byrne BJ, Hatzopoulos AK, Penn MS. Effect of intracoronary delivery of autologous bone marrow mononuclear cells 2 to 3 weeks following acute myocardial infarction on left ventricular function: the LateTIME randomized trial. JAMA. 2011;306:2110-2119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 310] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 112. | Makkar RR, Smith RR, Cheng K, Malliaras K, Thomson LE, Berman D, Czer LS, Marbán L, Mendizabal A, Johnston PV. Intracoronary cardiosphere-derived cells for heart regeneration after myocardial infarction (CADUCEUS): a prospective, randomised phase 1 trial. Lancet. 2012;379:895-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1099] [Cited by in RCA: 1058] [Article Influence: 81.4] [Reference Citation Analysis (1)] |
| 113. | Turan RG, Bozdag-T I, Turan CH, Ortak J, Akin I, Kische S, Schneider H, Rauchhaus M, Rehders TC, Kleinfeldt T. Enhanced mobilization of the bone marrow-derived circulating progenitor cells by intracoronary freshly isolated bone marrow cells transplantation in patients with acute myocardial infarction. J Cell Mol Med. 2012;16:852-864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 114. | Bartunek J, Behfar A, Dolatabadi D, Vanderheyden M, Ostojic M, Dens J, El Nakadi B, Banovic M, Beleslin B, Vrolix M. Cardiopoietic stem cell therapy in heart failure: the C-CURE (Cardiopoietic stem Cell therapy in heart failURE) multicenter randomized trial with lineage-specified biologics. J Am Coll Cardiol. 2013;61:2329-2338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 374] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 115. | Regenerative Medicine Annual Report: March 2012- March 2013. 13. Available from: http://alliancerm.org/sites/default/files/ARM_Annual_Report_2013 _Website.pdf. |
| 116. | US National Institutes of Health Clinical Trials. 13. Available from: http://www.clinicaltrials.gov/. |