Published online Sep 26, 2012. doi: 10.4330/wjc.v4.i9.275
Revised: August 21, 2012
Accepted: August 28, 2012
Published online: September 26, 2012
Hypertension is a major risk factor for cardiovascular disease, resulting in increased incidence of cerebrovascular events, ischaemic heart disease, heart failure, and renal impairment. Thus, it is one of the most important preventable causes of premature morbidity and mortality. Despite current knowledge on the management of hypertension and the availability of several effective antihypertensive medications, uncontrolled hypertension remains a common and challenging clinical problem. Resistant hypertension is a complex condition with multiple contributing factors and overlapping comorbidities. Although there is limited hard evidence regarding resistant hypertension, our understanding of this condition has improved recently. This article will present an overview of resistant hypertension and highlight recent publications about this topic.
- Citation: Paiva L, Cachulo MC, Providencia R, Barra S, Dinis P, Leitao-Marques A. Overview of resistant hypertension: A glimpse of the cardiologist’s current standpoint. World J Cardiol 2012; 4(9): 275-283
- URL: https://www.wjgnet.com/1949-8462/full/v4/i9/275.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i9.275
Resistant hypertension is defined as high blood pressure (BP) in spite of appropriate lifestyle interventions and administration of three different antihypertensive drugs at optimal dose amounts, which should include a diuretic agent[1,2]. The goal systolic BP is usually defined as < 140 mmHg and < 90 mmHg for diastolic BP; however, current views on cardiovascular risk suggest lower targets for high-risk patients (e.g., those with diabetes mellitus, renal dysfunction). By this definition, subjects who achieve adequate BP control with optimal doses of 4 or more antihypertensive medications are considered to have resistant hypertension. This group of patients controlled with ≥ 4 drugs accounts for 30% of the resistant hypertension cases[3], and should be considered as a separate category in future studies (as they seem to represent a more benign phenotype), to better characterize the most severe forms of truly resistant hypertension. Although arbitrary, the above definition focuses on a subset of hypertensive patients with a higher cardiovascular risk and potentially reversible causes of hypertension that should be thoroughly pursued. Prognosis among patients with resistant hypertension compared with those who are non-resistant, though expectedly worse, is not well established in the literature[4,5]. Resistant hypertension pathophysiology needs a greater understanding, as does its incidence and prognosis. Whether the worse cardiovascular outcome is related to a resistant-to-treatment phenotype or linked to BP control also needs to be better understood. Knowing the patterns of medication class use, the importance of medication adherence, and the efficacy of certain therapy interventions (change in medication class, increase in drug dose, novel antihypertensive treatments) in a population with resistant hypertension would help to guide future interventions and improve management of these challenging patients.
The prevalence of resistant hypertension, though not uncommon, is not well established and has been defined as a priority area in future studies[2]. There is no specifically designed research concerning resistant hypertension, and our knowledge mainly derives from cross-sectional analyses and some recent clinical trials. However, failure to apply a uniform definition of resistant hypertension, very selective populations, restricted treatment regimens, and the inability to exclude pseudoresistant hypertension has limited the interpretation of results. The 2003 to 2008 National Health and Nutrition Examination Survey included > 15 000 unselected adults in the United States, and found resistant hypertension criteria to be met in 8.9% of all individuals with hypertension, and in 12.8% of the hypertensive drug-treated population[5]. Another large survey in Spanish hypertensive patients found similar results, with 12.2% incidence of resistant hypertension in treated patients[6]. The work by Daugherty et al[5] has found that 16% of the patients were taking ≥ 3 medications, once they had excluded poor adherence to treatment regimens. Furthermore, this study has shown that 1 in 50 cases in whom antihypertensive treatment is started will develop resistant hypertension within 1.5 years[4]. Nonetheless, in a progressively older population, with an increasing incidence of comorbidities related to resistant hypertension such as diabetes, obesity and renal impairment, the prevalence of resistant-to-treatment hypertension is much more likely to increase.
A poor BP measurement technique can often be misleading. The most common errors are an inappropriate cuff size, incorrect patient and arm positions, and inadequate premeasurement at rest. Moreover, marked arterial stiffness which does not compress with pressure should be seen as a potential cause of pseudohypertension, especially in the elderly or in those with other treatment symptoms.
Non-adherence to lifestyle interventions and/or antihypertensive therapy is a major cause of uncontrolled hypertension. About half of the patients who were prescribed an antihypertensive drug had stopped taking it within one year[7]. Factors that influence adherence include patient demographics, side effects of medications, convenience of drug dosing, cost and number of medications, as well as patients’ knowledge, beliefs and attitudes about hypertension. A study on resistant hypertension highlighted the importance of patients’ compliance by reporting a BP reduction to normotensive values in about 30% of the participants, attributable merely to patient self-perception of being monitored and without any changes in medication regimen[8]. Nonetheless, physician failure to comply with guidelines and actively pursue adequate BP in their patients is, also, a significant contributor to the lack of BP control. The latter may be illustrated in a recent clinical study which has found that resistant hypertension patients were taking less than 50% of the recommended maximal daily doses of their antihypertensive medications at follow-up[9]. Moreover, patients already on 3 or more antihypertensive medications are at an increased risk for poor treatment adherence and clinical inertia (because of the potential adverse effects of multiple drug combinations or physician scepticism about the benefit of intensifying therapy).
Most patients have higher BP levels when measured by the physician than when assessed out of the office. This “white-coat” effect is often more pronounced in patients with severe hypertension. Moreover, 20%-30% of patients with apparent resistant hypertension referred for ambulatory BP monitoring in fact have normal BP readings[10]. It is of note that patients with white-coat hypertension have less severe target organ damage and cardiovascular risk compared to those with persistent elevated BP readings in ambulatory monitoring.
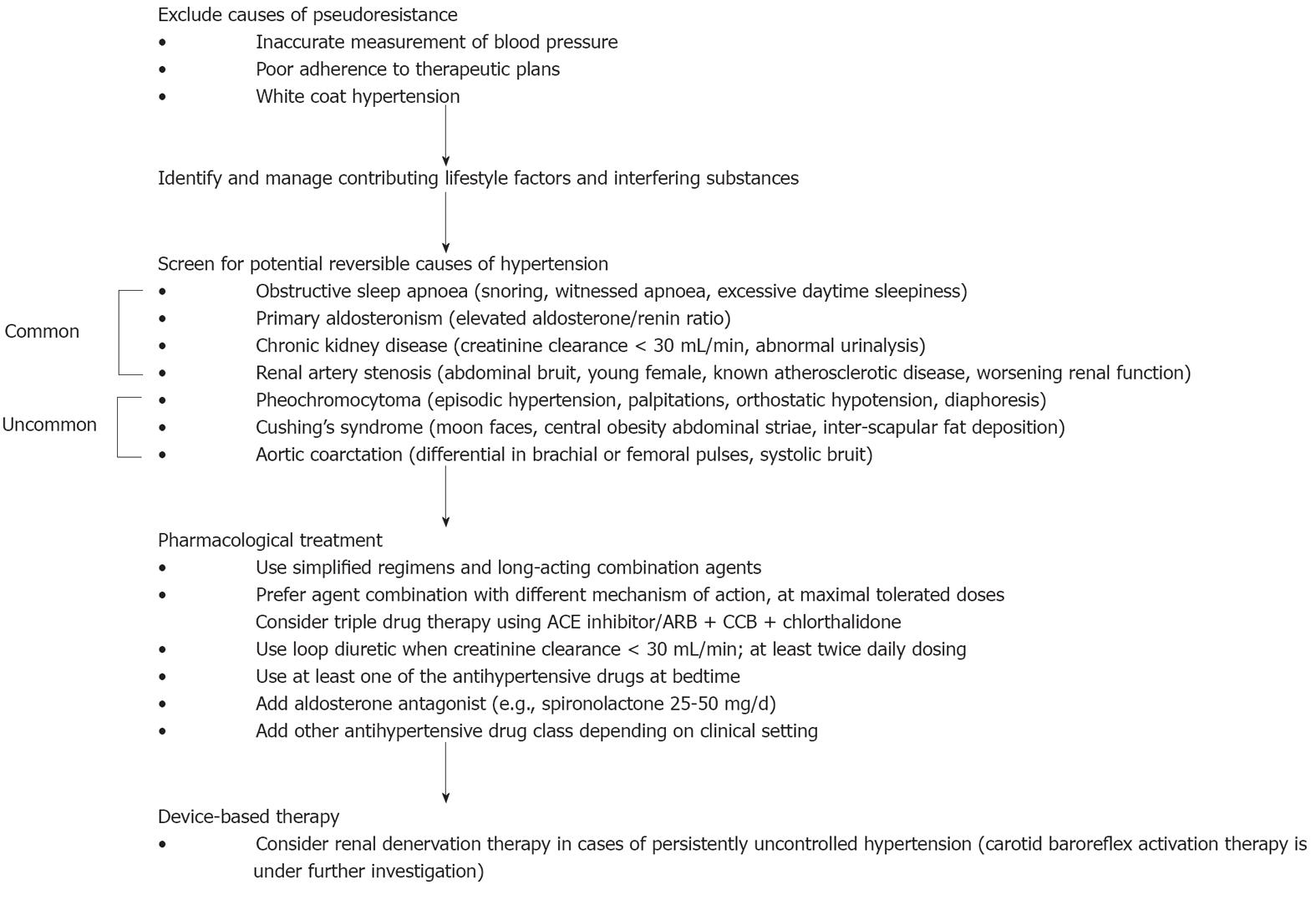
Resistant hypertension should not be confused with uncontrolled hypertension, which includes pseudoresistance, inadequate therapeutic regimen, as well as true resistant-to-treatment hypertension. Thus, resistant hypertension is a diagnosis of exclusion that should be carefully established using a stepwise patient evaluation, according to the American Heart Association state of the art manuscript on resistant hypertension[2].
In the presence of uncontrolled hypertension, the patient’s evaluation should begin with a correct BP measurement to avoid false high readings, and then confirmed by out-of-office BP monitoring to exclude white-coat hypertension. Patient compliance assessment is of utmost importance. The next step, after pseudoresistance exclusion, is the identification and possibly reversing of contributing lifestyle factors. Obesity is a common feature in resistant hypertension patients and is related to poor antihypertensive treatment response. It has been reported that each 10% increase in weight is associated with a 6.5 mmHg increase in systolic BP[11]. Dietary salt intake can blunt the effects of the majority of antihypertensive drugs, especially in salt-sensitive patients such as the elderly and black race patients, and in renal impairment. Several pharmacological agents can significantly interfere with BP and/or antihypertensive effect of medications; hence interfering substances should be promptly discontinued or minimized. The recognition of other common contributing factors such as non-steroidal anti-inflammatory drug use, oral contraceptive hormones or progressive renal impairment is needed in order to achieve BP control in resistant-to-treatment patients.
Resistant hypertension is complex in nature and almost always multifactorial in aetiology. Although uncommon, the potential reversible causes of hypertension should always be carefully ruled out by medical history, physical examination, biochemical evaluation, and/or non-invasive imaging (Figure 1). Sleep apnoea is among the commonest secondary causes of hypertension. Its association with hypertension is due to the sustained increase in sympathetic nervous system activity, and its prevalence is approximately 85% of the true resistant-to-treatment patients[12]. However, continuous positive airway pressure has only shown a modest antihypertensive benefit[13,14]. Primary aldosteronism seems to be a much more common secondary cause of hypertension than previously recognized, with a reported prevalence of approximately 20% in resistant hypertension[15]. Recognition that most patients do not have low serum potassium levels, and a more effective screening using aldosterone and renin levels, has led to an improved detection of this condition. Renal parenchymal disease and renal artery stenosis are other common causes of secondary hypertension that should be assessed in both analytical and imaging modalities. Less common causes including aortic coarctation, Cushing syndrome, and pheochromocytoma are rarely seen (< 1%)[4].
The management of resistant hypertension is arduous and involves extensive testing, which should include the following: biochemical evaluation, including serum sodium, potassium, glucose, and creatinine (creatinine clearance); plasma aldosterone and renin; urinalysis; and 24-h urine collection to estimate dietary sodium, potassium, and aldosterone excretion. Testing for urinary or plasma metanephrines/catecholamines is indicated only when pheochromocytoma is suspected. Non-invasive imaging is mandatory when there is a suspicion of renal artery stenosis, adrenal adenoma/tumour, parenchymal renal disease or aortic coarctation.
High BP is a heritable trait influenced by several biological pathways and responsive to environmental stimuli. The determination of the genetic variants involved in hypertension would provide new insight into BP regulation, and there are several lines of evidence which point towards an important genetic contribution. Furthermore, it is reasonable to expect an even greater genetic role in severe phenotypes, as true resistant hypertension. To date, few variants associated with interindividual BP variation have been consistently identified[16,17], and our understanding of the genetic determinants of hypertension is in its early phase. Nonetheless, efforts in the dissection of BP genetics would create new targets for therapeutic approaches, and future use of individually tailored treatment will improve drug efficacy and reduce its toxicity.
If a specific secondary cause of hypertension is suspected or if the BP is persistently high despite six months of more intensive treatment, patient referral to a hypertension specialist is advised[2]. Recommendations on the treatment of secondary causes of hypertension are beyond the scope of this review.
This includes reversal of lifestyle factors contributing to treatment resistance, and discontinuation or minimisation of interfering substances. There is usually a beneficial result with lower salt diet (< 100 mEq of sodium/24 h), ingestion of low fat and high fibre diet, weight loss in obese or overweight patients, moderation of alcohol intake to no more than two drinks per day for most men and one drink for women or lighter-weight persons, advising smoking cessation, and regular physical activity. Do not offer calcium, magnesium or potassium supplements as a method for reducing BP[17].
Drug treatment of resistant hypertension involves, by definition, combinations of three or more drugs.
Diuretic therapy: Inappropriate volume expansion contributes to resistant hypertension, even among patients already on thiazide diuretics. In order to increase efficiency it may be necessary to add a diuretic, increase the usual dose or change to different diuretic class. In those without significant renal impairment, the long acting thiazide diuretic chlorthalidone is preferred over hydrochlorothiazide for the treatment of resistant hypertension[18]. It has a more potent antihypertensive effect, longer half-life and has been shown to achieve better BP control, in comparison with hydrochlorothiazide. Among patients with an estimated glomerular filtration < 30 mL/min per m2, thiazide diuretics become less effective and loop diuretics should be used instead, such as furosemide, which needs at least twice daily dosing due to its short half-life. In the presence of refractory volume retention, medical intervention should focus on reducing dietary sodium intake and increasing the diuretic treatment intensity.
Aldosterone antagonists: The prevalence of primary aldosteronism in resistant hypertension patients seems to be much more common than previously acknowledged, and recent studies using aldosterone antagonists, such as spironolactone, eplerenone, and amiloride, reported significant antihypertensive benefits when added to a multiple drug regimen in patients with difficult-to-treat hypertension[19]. The antihypertensive effect of spironolactone was evaluated in randomized trials and has proven efficacy, although results were more modest than initial expectations. Compared to a placebo, spironolactone 25 mg significantly decreased mean daytime and nighttime ambulatory systolic BPs by 5.4 and 8.6 mmHg, respectively, with no significant change in diastolic pressure[20]. However, as suggested by the authors, it is possible that higher doses of spironolactone could have had a greater impact on BP levels. Regarding which add-on therapy to use in resistant hypertension, a recent study designed to compare spironolactone vs dual blockade of the renin-angiotensin-aldosterone system (RAS) has found that spironolactone has greater antihypertensive effect than dual blockade of the RAS in resistant hypertension[21].
Choice of regimen: Regimens should be simplified and long-acting combination agents should be preferred, to improve efficacy and adherence to treatment. Non-invasive hemodynamic studies assessing cardiac output, vascular resistance and intravascular volume may be considered to guide a pharmacological approach. While several studies have reported additive antihypertensive benefit by combining two different classes of drugs, few studies have systematically evaluated the combination of three or more medications in the treatment of resistant hypertension[2]. Considering no specific indication for a class of drugs, a reasonable approach would be to sequentially combine agents with different mechanisms of action to improve efficacy and drug tolerance. The use of same-class combinations such as dihydropyridine and non-dihydropyridine calcium channel blockers (CCB), combinations of diuretic, an angiotensin-converting enzyme inhibitor (ACEi) or an angiotensin receptor blocker (ARB) are not advocated over different classes of antihypertensive agents. The latter combination therapy, with a recognizably larger biologic effect, was evaluated in The Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial[22], and despite the reported small reduction in systolic BP in the combination-therapy group as compared with the ramipril group, no significant benefit was seen among patients receiving the two-drug therapy. However, combination therapy adverse effects were significantly increased (hypotension, syncope, renal dysfunction and hyperkalaemia). The authors concluded that no additional advantage and possibly some harm could occur from this drug combination. Although the lack of an additional benefit from a substantial lowering of BP is puzzling, similar results were found in the VALIANT study[23], in which the combination of a full dose of captopril plus valsartan did not significantly reduce the occurrence of the primary outcome but there was an increase in treatment-related adverse effects. Nonetheless, these findings contrast with a previous clinical trial done in a heart failure population, CHARM[24], in which candesartan added to existing therapy with any ACEi was superior to placebo in reducing deaths or hospitalization for heart failure.
Evidence-based recommendations in primary hypertension consider an ACEi or ARB plus a CCB and a diuretic as the most rational triple drug treatment. Among patients who still have their BP uncontrolled with the triple drug regimen at maximum recommended and tolerable doses, spironolactone 25-50 mg/d should be added to the treatment. Further increases in spironolactone doses are not recommended in the absence of documented primary aldosteronism. Adverse effects of aldosterone antagonists are uncommonly seen with eplerenone use.
In primary hypertension, with no compelling indication for a beta-blocker (e.g., ischaemic heart disease or heart failure), patients should not receive a beta-blocker as the first-line of treatment. Several studies have reported that beta-blockers are not as effective as other antihypertensive drug classes in the prevention of cardiovascular events of uncomplicated hypertension, and the combination with thiazide diuretics increases the risk of developing diabetes mellitus[1]. Nonetheless, beta-blockers are a reliable therapeutic option for uncontrolled hypertension and complicated hypertension, especially those with vasodilating properties, such as carvedilol and nebivolol. Furthermore, the association between beta and alpha-blockers may potentiate their antihypertensive effect[25].
The work by Hermida et al[26] in resistant hypertension underlined the importance of ensuring at least one of the antihypertensive drugs is taken at bedtime, in comparison with subjects receiving all drugs on awakening. This chronotherapeutic approach resulted in a significant 60% increase in BP control, and a 32% improvement in nighttime BP and in the prevalence of a non-dipper pattern, and should be implemented in resistant-to-treatment patients.
Other available agents can be added sequentially in the presence of persistent uncontrolled BP, such as centrally acting agents (clonidine, rilmenidine), or direct vasodilators (minoxidil, hydralazine). The two former pharmacological agents are potent vasodilators which should be reserved for cases of hypertension refractory to the above-mentioned medications because of frequent adverse effects.
A work by Hanselin et al[27] retrospectively studied antihypertensive use in > 140 000 patients with resistant hypertension. With regard to antihypertensive class use, 96.2% of the resistant hypertension patients were on ACE inhibitors and/or ARBs, 93.2% were taking diuretics, 83.6% a CCB, and 80.0% were on beta-blockers. Only 3.0% of patients were taking chlorthalidone and 5.9% aldosterone antagonists. Moreover, a total of 15.6% of patients were instead treated with ACE inhibitors plus ARB, which is not a first-line drug association. The authors concluded that although guideline-recommended first-line agents were used frequently, effective medications such as chlorthalidone and aldosterone antagonists were still underused.
A recent study evaluated the patterns of hypertension treatment, medication adherence, and treatment intensification (either increase in medication class or dose) in a resistant hypertension population[9]. The authors found that only 55% of the patients achieved BP control one year after resistant hypertension identification. In the first year of follow up the majority of patients were adherent to their antihypertensive medications (median medication adherence rates were nearly 85%); however, the use of many antihypertensive medication classes declined over 1 year, and one of the largest drops was seen in diuretic use. The latter underlines the difficulty to maintain adherence in patients with multiple antihypertensive regimens. One of the most important findings of this study was the evaluation of the role of therapy intensification in resistant hypertension patients. Over 1 year of follow-up, the intensification of the treatment regimen occurred in only 21.6% of visits with an elevated BP documented (10% had a class addition and 32% had a dose increase), which is much less than the expected intensification of the antihypertensive treatment for this high-risk group. However, the treatment intensification, but not treatment adherence, associated with improved BP control supports the importance of therapy optimization in resistant hypertension management.
Currently, BP remains uncontrolled in many cases despite the availability of multiple antihypertensive drugs and the patient’s adherence to treatment. The absence of novel antihypertensive drugs targeting new pathways has led to new treatment strategies using different combinations of available drugs, particularly those targeting sodium balance and RAS, which are the major recognizable factors affecting BP control. Some of these new strategies combine different diuretic drugs that act on different nephron segments[28] and others combine different RAS blockers[29], both approaches theoretically minimise counter-regulatory mechanisms that often limit the antihypertensive effect of the medical regimens. A recent work by Bobrie et al[30] compared the efficacy and safety of two stepped-care strategies of sequential nephron blockage (SNB) vs sequential RAS blockage (SRASB) added to a triple standardized therapy regimen (including an ARB, CCB and thiazide) in patients with resistant hypertension. The SNB strategy consisted of the sequential addition of low doses of one to three other diuretics acting at different nephron segments (spironolactone, furosemide and amiloride), rather than the standard approach of increasing the dose of a single diuretic or changing the class of the diuretic. The rationale of this novel approach is to minimise the effects of intrarenal counterregulatory mechanisms that are triggered by the use of diuretics acting at a single site. The SRASB strategy consisted of reinforcing RAS blockage by adding an ACEi and beta-blocker, in order to neutralise RAS counterregulatory mechanisms. In this study, the SNB was more effective than SRASB. The incidence of adverse events was similar in both groups and both treatment strategies were well tolerated. The authors concluded that progressive sodium depletion by the SNB strategy is effective to reduce BP in resistant hypertension patients. Moreover, antinatriuretic counterregulatory mechanisms seem to contribute more to uncontrolled hypertension pathophysiology than counterregulation inside the RAS. The choice of other diuretic classes instead of thiazide-type drugs, such as chlorthalidone, or bumetanide in place of furosemide, their doses and optimal sequence of administration needs further study and definition.
Renal denervation: The role of afferent and efferent sympathetic nerves in essential hypertension has been long recognised and recently reappraised. Efferent sympathetic outflow produces renal vasoconstriction, decreases renal blood flow, and increases renin release as well as sodium uptake, and afferent signals increase central sympathetic activity and contribute to neurogenic hypertension. A catheter-based radiofrequency ablation has been developed to selectively disrupt the renal nerves, and its efficacy and safety are supported by the Symplicity HTN-2 trial[31] comprising resistant hypertension subjects who had a baseline systolic pressure ≥ 160 mmHg (≥ 150 mmHg in diabetes type 2 patients). After 6 mo, office BP in the renal denervation group reduced by 32/12 mmHg from baseline, and home BP had a less pronounced reduction of 11/7 mmHg. The comparatively large discrepancy between the effects on clinic and ambulatory BP is noteworthy, and has been reported similarly by other study groups[32,33]. The antihypertensive effect seems to be sustained over 2 years. Moreover, the renal denervation registered a very favourable safety profile and was of minor complexity. Although procedure effects on cardiovascular outcomes are not well established, subsequent reports suggested important benefits in coexisting metabolic syndrome and sleep apnoea. Witkowski et al[32] concluded that renal denervation improves indices of insulin action and glucose metabolism (plasma glucose concentration 2 h after glucose administration: 7.0 mmol/L vs 6.4 mmol/L; hemoglobin A1C: 6.1% vs 5.6%) as well as sleep apnea (apnea-hypopnea index: 16.3 events/h vs 4.5 events/h) at 6-mo follow up. A study by Brandt et al[34] has investigated the effect of catheter-based renal sympathetic denervation on left ventricular hypertrophy and systolic and diastolic function, parameters related to chronic activation of the sympathetic nervous system and to increased mortality, in patients with resistant hypertension. This study found a significant reduction in left ventricular mass, left ventricular filling pressures and left atrium dimensions, and a significant increase in ejection fraction. The prognostic importance of these results is not yet clear, and it is not possible to distinguish what proportion of these changes were caused by BP reduction or were related to the sympathetic denervation per se. Nevertheless, the long-term improvement in left ventricular dimension and function may have significant morbidity and mortality impact, in addition to BP-lowering effect. Furthermore, the Symplicity HF trial, designed to address the efficacy of renal denervation in heart failure patients, will further define the usefulness of this technique in other clinical settings besides resistant hypertension.
Although catheter-based renal denervation opens new interesting therapeutic perspectives, there are several limitations in the studies supporting this novel procedure that were recently reviewed by Steichen et al[35]. In the Symplicity HTN-1 trial[36] there was no control group with which to make comparisons regarding BP and glomerular filtration rate responses over time. The number of patients included in the pivotal studies[31,36] was small (205 patients), and only a few have reached the 24-mo follow-up time point. This limited follow-up appears not to be appropriate to exclude delayed adverse effects that may derive from the percutaneous technique. The study design was weak and may have exposed the investigators to several biases. It is of note that secondary hypertension and white-coat hypertension were not properly excluded. The BP reductions should be carefully interpreted, as no intervention was proposed in the control group. It would be preferable to optimize the pharmacological approach in a standardized fashion in the two groups before randomisation and to carry out a factitious intervention (sham) in the control group, to clearly establish the real added value of the denervation procedure compared to the optimal medical therapy. In addition, office-based measurements of BP were the main method used to evaluate procedure efficacy, which is not the preferable approach, particularly in an open study (placebo effect). The benefit for the BP control was much more modest in the ambulatory BP group than in the clinic reading group. Only a relatively small number of the randomized patients had 24-h BP monitoring before and 6 mo after denervation, and the average reduction in systolic BP was only 11 mmHg, much less impressive than the 32 mmHg reported in the office-based BP measurements. The difference compared to the control group was only 8 mmHg, similar to the effect expected with the addition of a new antihypertensive drug class. The experience from surgical renal denervation showed that the reduction in BP could be maintained over time[37]; however, long-term BP reduction after percutaneous renal denervation is uncertain. In the latter, denervation is less complete and sympathetic reinnervation may possibly be seen, a phenomenon well documented after renal transplantation. Moreover, the maintenance of the BP reduction was only reported in a small group of patients followed over 24 mo (18 patients)[36]. A prolonged follow-up of these patients with noninvasive imaging would be essential to evaluate long-term possible lesions induced by the denervation ablation. Finally, there are no available results on morbidity or mortality. Despite the above considerations, the European Society of Cardiology Council for Cardiology Practice[38] considers catheter-based renal denervation useful, particularly in the treatment of patients with hypertension coexisting with sleep apnea and metabolic syndrome.
Carotid baroreflex activation: Another device-based therapy for resistant hypertension is carotid baroreflex activation, consisting of an implanted pulse generator and electrodes around carotid sinuses. The Rheos Baroreflex Hypertension Therapy System enhances afferent nerve outflow from the baroreceptors to the cardiovascular control centres of the brain, reducing sympathetic outflow and, subsequently, BP. The Device-Based Therapy in Hypertension Trial was a non-randomised study which documented carotid baroreflex activation effect on office and ambulatory BP of patients with resistant hypertension[39]. The office BP reduced by an average of 21/12 mmHg and heart rate decreased by 8 beats/min from baseline, and the antihypertensive effect was sustained through the 24-mo follow up. However, in home BP monitoring the systolic BP was reduced nonsignificantly by 6 mmHg (P = 0.10), but with a significant decrease in diastolic BP (4 mmHg, P = 0.04), and in heart rate (5 beats/min, P < 0.001). Conversely, the subsequent randomised controlled trial reported less convincing results, due to failure to meet endpoints for acute responders and procedural safety[40]. Moreover, the implantation’s complexity and invasiveness are a noteworthy limitation. Nonetheless, the development and investigation of baroreflex activation therapy continues, and future clinical trials will further define its therapeutic benefit.
Table 1 summarizes the most relevant therapeutic approaches in resistant hypertension discussed in the manuscript.
| Usefulness | Limitations | |
| Medical treatment | ||
| Aldosterone antagonists | High prevalence of primary aldosteronism Higher efficacy than dual RAS blockade | 70% of resistant-to-treatment hypertension cases are not controlled with ≥ 4 antihypertensive drugs |
| Aldosterone antagonists cause frequent adverse effects, particularly in kidney disease | ||
| Sequential nephron/RAS blockade1 | Act on sodium balance and RAS (major blood pressure determinants) Sequential nephron blockade superior to RAS blockade | Sequential blockade benefits need further validation Sequential nephron blockade regimen complexity Potential higher incidence of adverse effects/poor tolerance Needs regular medical evaluation |
| Device–based therapy | ||
| Catheter-based renal denervation | Novel therapeutic target for resistant to drug treatment patients Promising effects on glycemic control, sleep apnea and heart structure/function Potential benefits in heart failure patients | Needs further validation of study results Needs complete evaluation of delayed procedure complications Not available to all uncontrolled blood pressure patients Procedure success variability related to operator/patient factors |
| Carotid baroreflex activation | Novel therapeutic target for resistant to drug treatment patients | Needs further validation of study results Implantation's complexity and invasiveness |
Hypertension is one of the most important preventable causes of premature morbidity and mortality, and despite the availability of effective antihypertensive drugs, it remains uncontrolled in too many patients. The causes of uncontrolled hypertension and the distinction between pseudoresistance and true resistant hypertension should be carefully pursued using a systematic approach to the patient. Understanding the pathophysiology of uncontrolled BP will help direct future efforts to improve the outcome in this high-risk population. The management of resistant hypertension should be standardised and follow the current treatment guidelines, including device-based therapy in specific cases, which has shown encouraging results in BP, metabolic control, and heart dimensions and function. In the absence of novel antihypertensive drugs targeting new pathways, an active pursuit of treatment intensification and the use of different combinations of antihypertensive drugs, particularly those targeting renal antinatriuretic counterregulatory mechanisms, may be an effective approach to manage truly resistant hypertension patients.
Peer reviewers: Bin Jiang, Professor, Department of Neuro-epidemiology, Beijing Neurosurgical Institute, Capital Medical University, 6 Tiantan Xili, Yongnei Street, Chongwen District, Beijing 100050, China; Gergely Feher, MD, PhD, Department of Neurology, Medical School, University of Pecs, 2 Ret str., Pecs, H-7623 Baranya, Hungary
S- Editor Cheng JX L- Editor Logan S E- Editor Li JY
| 1. | Mansia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S. 2007 ESH-ESC Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Press. 2007;16:135-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 879] [Cited by in RCA: 917] [Article Influence: 50.9] [Reference Citation Analysis (0)] |
| 2. | Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510-e526. [PubMed] |
| 3. | Persell SD. Prevalence of resistant hypertension in the United States, 2003-2008. Hypertension. 2011;57:1076-1080. [PubMed] |
| 4. | Pisoni R, Ahmed MI, Calhoun DA. Characterization and treatment of resistant hypertension. Curr Cardiol Rep. 2009;11:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, O'Connor PJ, Selby JV, Ho PM. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125:1635-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 135] [Reference Citation Analysis (0)] |
| 6. | de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, Oliveras A, Ruilope LM. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898-902. [PubMed] |
| 7. | Vrijens B, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008;336:1114-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 613] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 8. | Burnier M, Schneider MP, Chioléro A, Stubi CL, Brunner HR. Electronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisions. J Hypertens. 2001;19:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 179] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Daugherty SL, Powers JD, Magid DJ, Masoudi FA, Margolis KL, O'Connor PJ, Schmittdiel JA, Ho PM. The association between medication adherence and treatment intensification with blood pressure control in resistant hypertension. Hypertension. 2012;60:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 78] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Brown MA, Buddle ML, Martin A. Is resistant hypertension really resistant? Am J Hypertens. 2001;14:1263-1269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 121] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Lloyd-Jones DM, Evans JC, Larson MG, O'Donnell CJ, Roccella EJ, Levy D. Differential control of systolic and diastolic blood pressure : factors associated with lack of blood pressure control in the community. Hypertension. 2000;36:594-599. [PubMed] |
| 12. | Pratt-Ubunama MN, Nishizaka MK, Boedefeld RL, Cofield SS, Harding SM, Calhoun DA. Plasma aldosterone is related to severity of obstructive sleep apnea in subjects with resistant hypertension. Chest. 2007;131:453-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 228] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 13. | Barbé F, Mayoralas LR, Duran J, Masa JF, Maimó A, Montserrat JM, Monasterio C, Bosch M, Ladaria A, Rubio M. Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness. a randomized, controlled trial. Ann Intern Med. 2001;134:1015-1023. [PubMed] |
| 14. | Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, Mullins R, Jenkinson C, Stradling JR, Davies RJ. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet. 2002;359:204-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 627] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 15. | Calhoun DA, Nishizaka MK, Zaman MA, Thakkar RB, Weissmann P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension. 2002;40:892-896. [PubMed] |
| 16. | Kupper N, Willemsen G, Riese H, Posthuma D, Boomsma DI, de Geus EJ. Heritability of daytime ambulatory blood pressure in an extended twin design. Hypertension. 2005;45:80-85. [PubMed] |
| 17. | McManus RJ, Caulfield M, Williams B. NICE hypertension guideline 2011: evidence based evolution. BMJ. 2012;344:e181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Ernst ME, Carter BL, Goerdt CJ, Steffensmeier JJ, Phillips BB, Zimmerman MB, Bergus GR. Comparative antihypertensive effects of hydrochlorothiazide and chlorthalidone on ambulatory and office blood pressure. Hypertension. 2006;47:352-358. [PubMed] |
| 19. | Nishizaka MK, Zaman MA, Calhoun DA. Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens. 2003;16:925-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 347] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 20. | Václavík J, Sedlák R, Plachy M, Navrátil K, Plásek J, Jarkovsky J, Václavík T, Husár R, Kociánová E, Táborsky M. Addition of spironolactone in patients with resistant arterial hypertension (ASPIRANT): a randomized, double-blind, placebo-controlled trial. Hypertension. 2011;57:1069-1075. [PubMed] |
| 21. | Alvarez-Alvarez B, Abad-Cardiel M, Fernandez-Cruz A, Martell-Claros N. Management of resistant arterial hypertension: role of spironolactone versus double blockade of the renin-angiotensin-aldosterone system. J Hypertens. 2010;28:2329-2335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, Dagenais G, Sleight P, Anderson C. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547-1559. [PubMed] |
| 23. | Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667-1675. [PubMed] |
| 24. | McMurray JJ, Ostergren J, Swedberg K, Granger CB, Held P, Michelson EL, Olofsson B, Yusuf S, Pfeffer MA. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet. 2003;362:767-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1422] [Cited by in RCA: 1253] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 25. | Townsend RR, DiPette DJ, Goodman R, Blumfield D, Cronin R, Gradman A, Katz LA, McCarthy EP, Sopko G. Combined alpha/beta-blockade versus beta 1-selective blockade in essential hypertension in black and white patients. Clin Pharmacol Ther. 1990;48:665-675. [PubMed] |
| 26. | Hermida RC, Ayala DE, Calvo C, López JE, Mojón A, Fontao MJ, Soler R, Fernández JR. Effects of time of day of treatment on ambulatory blood pressure pattern of patients with resistant hypertension. Hypertension. 2005;46:1053-1059. [PubMed] |
| 27. | Hanselin MR, Saseen JJ, Allen RR, Marrs JC, Nair KV. Description of antihypertensive use in patients with resistant hypertension prescribed four or more agents. Hypertension. 2011;58:1008-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Knauf H, Mutschler E. Sequential nephron blockade breaks resistance to diuretics in edematous states. J Cardiovasc Pharmacol. 1997;29:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Azizi M, Ménard J. Combined blockade of the renin-angiotensin system with angiotensin-converting enzyme inhibitors and angiotensin II type 1 receptor antagonists. Circulation. 2004;109:2492-2499. [PubMed] |
| 30. | Bobrie G, Frank M, Azizi M, Peyrard S, Boutouyrie P, Chatellier G, Laurent S, Menard J, Plouin PF. Sequential nephron blockade versus sequential renin-angiotensin system blockade in resistant hypertension: a prospective, randomized, open blinded endpoint study. J Hypertens. 2012;30:1656-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 31. | Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet. 2010;376:1903-1909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1656] [Cited by in RCA: 1614] [Article Influence: 107.6] [Reference Citation Analysis (0)] |
| 32. | Witkowski A, Prejbisz A, Florczak E, Kądziela J, Śliwiński P, Bieleń P, Michałowska I, Kabat M, Warchoł E, Januszewicz M. Effects of renal sympathetic denervation on blood pressure, sleep apnea course, and glycemic control in patients with resistant hypertension and sleep apnea. Hypertension. 2011;58:559-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 337] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 33. | Egan BM. Renal sympathetic denervation: a novel intervention for resistant hypertension, insulin resistance, and sleep apnea. Hypertension. 2011;58:542-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 45] [Reference Citation Analysis (0)] |
| 34. | Brandt MC, Mahfoud F, Reda S, Schirmer SH, Erdmann E, Böhm M, Hoppe UC. Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol. 2012;59:901-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 381] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 35. | Steichen O, Sapoval M, Frank M, Bobrie G, Plouin PF, Azizi M. [Renal-nerve ablation in patients with resistant hypertension: caution is still needed]. Presse Med. 2012;41:349-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of blood pressure reduction out to 24 months. Hypertension. 2011;57:911-917. [PubMed] |
| 37. | Page IH, Heuer GJ. A surgical treatment of essential hypertension. J Clin Invest. 1935;14:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Wojakowski W, Tendera M, Jadczyk T, Januszewicz A, Witkowski A. Catheter-based renal denervation. E-journal of the ESC Council for Cardiology Practice. 2012;10:No. 22 Available from: http://www.escardio.org/communities/councils/ccp/e-journal/volume10/Pages/catheter-based-renal-denervation-tendera-m-wojakowksy-w.aspx. |
| 39. | Scheffers IJ, Kroon AA, Schmidli J, Jordan J, Tordoir JJ, Mohaupt MG, Luft FC, Haller H, Menne J, Engeli S. Novel baroreflex activation therapy in resistant hypertension: results of a European multi-center feasibility study. J Am Coll Cardiol. 2010;56:1254-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 249] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 40. | Bisognano JD, Bakris G, Nadim MK, Sanchez L, Kroon AA, Schafer J, de Leeuw PW, Sica DA. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011;58:765-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 429] [Article Influence: 30.6] [Reference Citation Analysis (0)] |