Peer-review started: November 24, 2023
First decision: December 7, 2023
Revised: December 15, 2023
Accepted: January 3, 2024
Article in press: January 3, 2024
Published online: January 26, 2024
Processing time: 55 Days and 15.1 Hours
The World Journal of Cardiology published an article written by Kuwahara et al that we take the pleasure to comment on. We focused our attention on venous conges
Core Tip: Fluid overload and venous congestion, including renal venous hypertension, play a major role in the pathogenesis of acute and chronic renal dysfunction occurring in heart disease. Physical assessment sensitivity alone to determine fluid status is scarce, limiting success in clinical decision-making. Ultrasonography and venous Doppler flow patterns evaluation is a valuable, non-invasive, bedside diagnostic tool for establishing fluid status, and guide its treatment.
- Citation: Di Maria A, Siligato R, Bondanelli M, Fabbian F. Venous Doppler flow patterns, venous congestion, heart disease and renal dysfunction: A complex liaison. World J Cardiol 2024; 16(1): 5-9
- URL: https://www.wjgnet.com/1949-8462/full/v16/i1/5.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i1.5
The paper written by Kuwahara et al[1] analyzed the relationship between portal vein pulsatility ratio (PVPR) and acute heart failure. The authors calculated the PVPR ratio in the right portal branch of 56 patients hospitalized with acute heart failure and 17 controls and found that reducing PVPR due to improving venous congestion was associated with better outcomes. PVPR was suggested to be a novel prognostic marker for hospitalized patients with acute heart failure.
Interestingly, the mean estimated glomerular filtration rate of the subjects investigated was between 39 and 47 mL/min/1.73 m2 in the three groups of patients with different PVPR values. The paper does not report whether the patients suffered only acute kidney injury or had an exacerbation of pre-existing chronic kidney disease. It is necessary to underline this problem because the vicious circle between heart and renal disease is a well-known clinical condition[2].
The relationship between heart and renal disease is defined as cardio-renal syndrome (CRS), a term describing the complex interactions between heart and kidney dysfunction. CRS is a challenging and evolving field, and more research is needed to understand better the pathophysiology, diagnosis, prevention, and treatment of this complex condition. CRS is classified into five subtypes, depending on the primary organ involved and the acute or chronic nature of the condition[3].
The epidemiology of CRS is not well established, as few prospective studies have assessed the prevalence, incidence, risk factors, and outcomes of different CRS subtypes. However, some estimates suggest that CRS is a common and severe complication of cardiovascular and renal diseases affecting people worldwide[4].
Aging, hypertension, diabetes, obesity, inflammation, oxidative stress, neurohormonal activation, and medications could contribute to the development of CRS. However, the cardiorenal connection is more complex than the hemodynamic model alone; it should be considered the effects of a network including the renin-angiotensin system, the nitric oxide, the reactive oxygen species, the inflammation, the anemia, and the sympathetic nervous system[5,6].
It could be argued that patients enrolled in the Kuwahara et al[1] study could be classified as acute or type 1 cardio-renal syndrome. In this clinical condition, acute worsening of heart function causes reduced kidney function. Acute renal dysfunction is diagnosed in 27%-40% of patients hospitalized for acute heart failure[7,8]; this clinical entity leads to higher morbidity and mortality, increasing the duration of admission[9]. Also, in internal medicine units, CRS type 1 is common, especially in elderly patients with stage 3-4 chronic kidney disease[10].
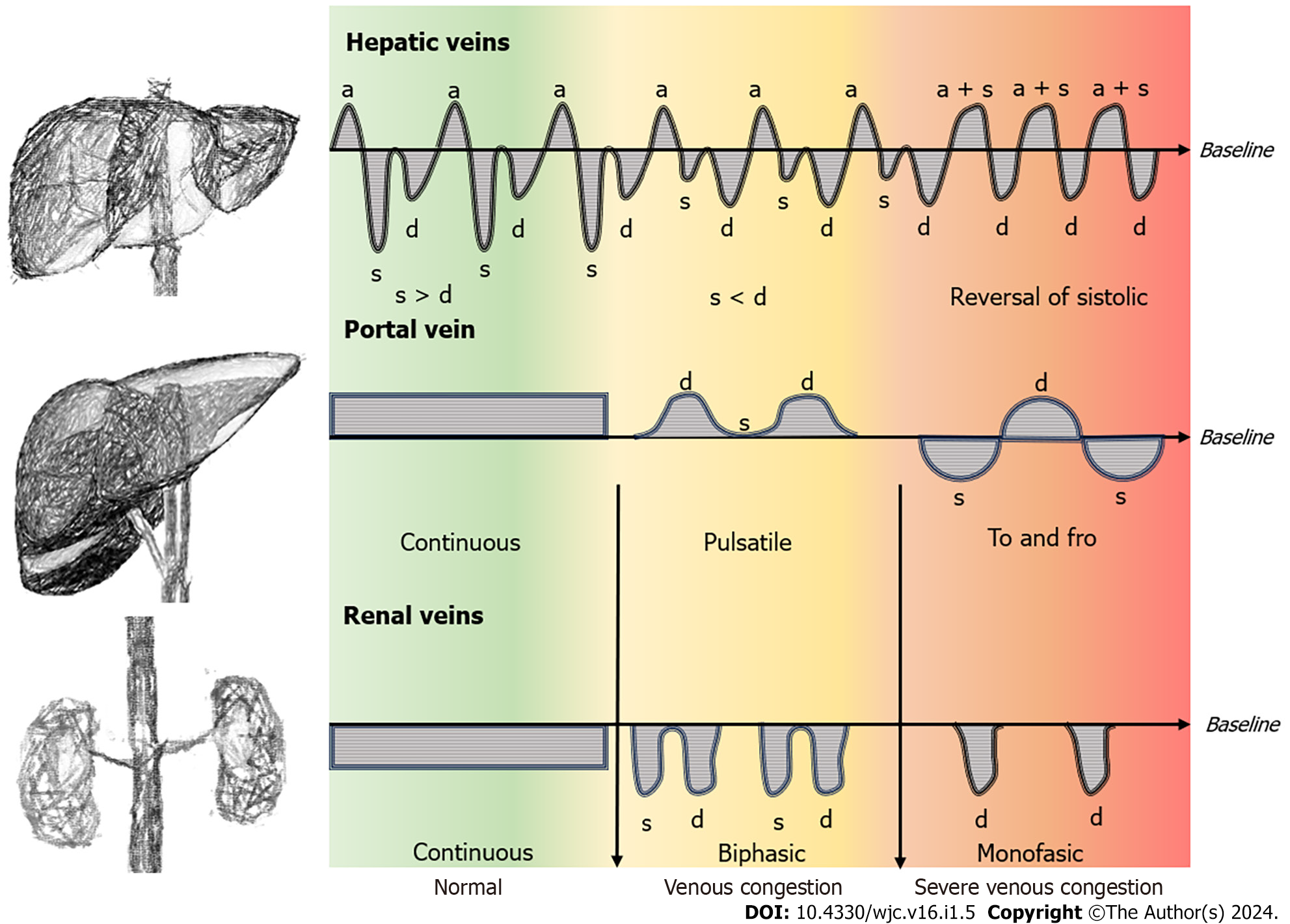
Using Doppler modalities during ultrasound investigations, the clinician could assess venous flow patterns relating the signal to the cardiac cycle. In the presence of hemodynamic changes within the systemic venous circulation leading to high venous pressure, venous Doppler profile abnormalities at multiple sites are detected (Figure 1). Clinically significant systemic venous congestion is diagnosed by abnormal Doppler flow patterns. Venous excess ultrasound (VExUS) score was studied in patients assessed with right heart catheterization, and proper atrial pressure was significantly associated with VExUS grade[11]. Organ congestion from venous hypertension could be involved in the development of organ injury in several clinical situations, such as critical diseases, congestive heart failure, and chronic kidney disease[12].
Fluid overload and venous congestion, including renal venous hypertension, are major determinants of acute and chronic renal dysfunction arising in heart disease[2]. Due to the limitations of traditional methods in evaluating venous congestion, detecting venous Doppler profile abnormalities (at multiple sites) related to elevated venous pressure is becoming very important in clinical assessment, mainly because it can be performed at the bedside[12].
In 2019, Husain-Syed et al[13] evaluated 205 subjects with suspected or pre-diagnosed pulmonary hypertension who underwent right heart catheterization. They also evaluated intrarenal venous patterns and concluded that the renal venous stasis index could predict the development of right heart failure.
In 2020, Spiegel et al[14] compared the morphology of hepatic veins, portal veins, and intra-renal veins waveform abnormalities VExUS for predicting major kidney events at 30 d in 114 adult patients admitted to an intensive care unit. They found that significant kidney events at 30 d were associated with abnormalities in hepatic and portal venous Doppler.
Severe venous congestion shown by flow abnormalities in Doppler patterns was associated with acute kidney injury (AKI) in 145 patients who underwent cardiac surgery. VExUS grade outperformed central venous pressure measure
Inferior vena cava and hepatic vein waveform, and portal vein pulsatility were investigated aiming at determining VExUS, in thirty CRS patients aged 59 years in order to evaluate the association between fluid overload and AKI. Authors found that improved renal function was related to improvement in VExUS grade[16].
Argaiz et al[17] suggested that in patients with acute left heart failure, the normalization of the size of the inferior vena cava, the restoration of its collapsibility, and the improvement of portal vein flow were related to the decrease in serum creatinine levels.
Hermansen et al[18] conducted a prospective, observational study to assess the connection between Doppler signals of renal perfusion and the development of AKI. Abnormal renal venous flow pattern on the first postoperative day and portal vein pulsatility fraction were associated with severe AKI development.
During 2023, at least four papers investigated the relationship between AKI and venous congestion. After cardiac surgery, abnormalities in intra-renal venous flow, portal vein pulsatility fraction, hepatic vein flow patterns, and central venous pressure were associated with the development of AKI[19]. In a prospective study evaluating subjects suffering from acute coronary syndrome, the increasing degree of VExUS was associated with AKI[20].
Patients admitted to intensive care units with a VExUS score greater than one were treated with diuretics more frequently than those with a VExUS score equal to or lower than 1. Moreover, subjects showing decreasing VExUS scores had more renal replacement therapy-free days in 28 d[21].
On the other hand, Andrei et al[22] could not detect any association between VExUS score and AKI and 28-d mortality.
Chronic kidney disease increases the risk of death during hospitalization in several clinical conditions, such as myocardial infarction[23], chronic obstructive pulmonary disease[24], stroke[25], and CRS[26]. Some of the strategies that may be beneficial in order to improve outcomes include optimizing fluid balance, reducing congestion, improving hemodynamics, preserving renal perfusion, preventing or treating acute kidney injury, and using cardioprotective and renoprotective drugs. Managing kidney failure and different clinical conditions, particularly those involving the heart, requires a multidisciplinary approach that addresses the underlying causes and the specific features of each subtype. Cardiologists and nephrologists should correctly manage the complex fluid problem due to its centrality in everyday clinical practice. Physical assessment sensitivity alone to determine fluid status is scarce, limiting success in clinical decision-making. Ultrasonography and venous Doppler flow pattern evaluation are valuable, non-invasive, bedside diagnostic tools for establishing fluid status and guiding the treatment of venous congestion[27].
We thank Claudia Righini and Donato Bragatto, Biblioteca Interaziendale di Scienze della Salute, Ferrara, Italy, for their valuable support.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu Y, China S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
| 1. | Kuwahara N, Honjo T, Sone N, Imanishi J, Nakayama K, Kamemura K, Iwahashi M, Ohta S, Kaihotsu K. Clinical impact of portal vein pulsatility on the prognosis of hospitalized patients with acute heart failure. World J Cardiol. 2023;15:599-608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (2)] |
| 2. | Deferrari G, Cipriani A, La Porta E. Renal dysfunction in cardiovascular diseases and its consequences. J Nephrol. 2021;34:137-153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 3. | Ronco C, McCullough P, Anker SD, Anand I, Aspromonte N, Bagshaw SM, Bellomo R, Berl T, Bobek I, Cruz DN, Daliento L, Davenport A, Haapio M, Hillege H, House AA, Katz N, Maisel A, Mankad S, Zanco P, Mebazaa A, Palazzuoli A, Ronco F, Shaw A, Sheinfeld G, Soni S, Vescovo G, Zamperetti N, Ponikowski P; Acute Dialysis Quality Initiative (ADQI) consensus group. Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. Eur Heart J. 2010;31:703-711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 592] [Cited by in RCA: 657] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 4. | Uduman J. Epidemiology of Cardiorenal Syndrome. Adv Chronic Kidney Dis. 2018;25:391-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Longhini C, Molino C, Fabbian F. Cardiorenal syndrome: still not a defined entity. Clin Exp Nephrol. 2010;14:12-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Gembillo G, Visconti L, Giusti MA, Siligato R, Gallo A, Santoro D, Mattina A. Cardiorenal Syndrome: New Pathways and Novel Biomarkers. Biomolecules. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 7. | Forman DE, Butler J, Wang Y, Abraham WT, O'Connor CM, Gottlieb SS, Loh E, Massie BM, Rich MW, Stevenson LW, Young JB, Krumholz HM. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 663] [Cited by in RCA: 664] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 8. | Gottlieb SS, Abraham W, Butler J, Forman DE, Loh E, Massie BM, O'connor CM, Rich MW, Stevenson LW, Young J, Krumholz HM. The prognostic importance of different definitions of worsening renal function in congestive heart failure. J Card Fail. 2002;8:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 403] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 9. | Ronco C, House AA, Haapio M. Cardiorenal syndrome: refining the definition of a complex symbiosis gone wrong. Intensive Care Med. 2008;34:957-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 128] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Fabbian F, Pala M, De Giorgi A, Scalone A, Molino C, Portaluppi F, Mikhailidis DP, Manfredini R. Clinical features of cardio-renal syndrome in a cohort of consecutive patients admitted to an internal medicine ward. Open Cardiovasc Med J. 2011;5:220-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Longino A, Martin K, Leyba K, Siegel G, Gill E, Douglas IS, Burke J. Correlation between the VExUS score and right atrial pressure: a pilot prospective observational study. Crit Care. 2023;27:205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 46] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 12. | Deschamps J, Denault A, Galarza L, Rola P, Ledoux-Hutchinson L, Huard K, Gebhard CE, Calderone A, Canty D, Beaubien-Souligny W. Venous Doppler to Assess Congestion: A Comprehensive Review of Current Evidence and Nomenclature. Ultrasound Med Biol. 2023;49:3-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Husain-Syed F, Birk HW, Ronco C, Schörmann T, Tello K, Richter MJ, Wilhelm J, Sommer N, Steyerberg E, Bauer P, Walmrath HD, Seeger W, McCullough PA, Gall H, Ghofrani HA. Doppler-Derived Renal Venous Stasis Index in the Prognosis of Right Heart Failure. J Am Heart Assoc. 2019;8:e013584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 14. | Spiegel R, Teeter W, Sullivan S, Tupchong K, Mohammed N, Sutherland M, Leibner E, Rola P, Galvagno SM Jr, Murthi SB. The use of venous Doppler to predict adverse kidney events in a general ICU cohort. Crit Care. 2020;24:615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 15. | Beaubien-Souligny W, Rola P, Haycock K, Bouchard J, Lamarche Y, Spiegel R, Denault AY. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 331] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 16. | Bhardwaj V, Vikneswaran G, Rola P, Raju S, Bhat RS, Jayakumar A, Alva A. Combination of Inferior Vena Cava Diameter, Hepatic Venous Flow, and Portal Vein Pulsatility Index: Venous Excess Ultrasound Score (VEXUS Score) in Predicting Acute Kidney Injury in Patients with Cardiorenal Syndrome: A Prospective Cohort Study. Indian J Crit Care Med. 2020;24:783-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 17. | Argaiz ER, Rola P, Gamba G. Dynamic Changes in Portal Vein Flow during Decongestion in Patients with Heart Failure and Cardio-Renal Syndrome: A POCUS Case Series. Cardiorenal Med. 2021;11:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Hermansen JL, Pettey G, Sørensen HT, Nel S, Tsabedze N, Hørlyck A, Chakane PM, Gammelager H, Juhl-Olsen P. Perioperative Doppler measurements of renal perfusion are associated with acute kidney injury in patients undergoing cardiac surgery. Sci Rep. 2021;11:19738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Li ZT, Huang DB, Zhao JF, Li H, Fu SQ, Wang W. Comparison of various surrogate markers for venous congestion in predicting acute kidney injury following cardiac surgery: A cohort study. J Crit Care. 2024;79:154441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 20. | Viana-Rojas JA, Argaiz E, Robles-Ledesma M, Arias-Mendoza A, Nájera-Rojas NA, Alonso-Bringas AP, De Los Ríos-Arce LF, Armenta-Rodriguez J, Gopar-Nieto R, Briseño-De la Cruz JL, González-Pacheco H, Sierra-Lara Martinez D, Gonzalez-Salido J, Lopez-Gil S, Araiza-Garaygordobil D. Venous excess ultrasound score and acute kidney injury in patients with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care. 2023;12:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 12.0] [Reference Citation Analysis (1)] |
| 21. | Rihl MF, Pellegrini JAS, Boniatti MM. VExUS Score in the Management of Patients With Acute Kidney Injury in the Intensive Care Unit: AKIVEX Study. J Ultrasound Med. 2023;42:2547-2556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (4)] |
| 22. | Andrei S, Bahr PA, Nguyen M, Bouhemad B, Guinot PG. Prevalence of systemic venous congestion assessed by Venous Excess Ultrasound Grading System (VExUS) and association with acute kidney injury in a general ICU cohort: a prospective multicentric study. Crit Care. 2023;27:224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 43] [Reference Citation Analysis (0)] |
| 23. | Fabbian F, Pala M, De Giorgi A, Manfredini F, Mallozzi Menegatti A, Salmi R, Portaluppi F, Gallerani M, Manfredini R. In-hospital mortality in patients with renal dysfunction admitted for myocardial infarction: the Emilia-Romagna region of Italy database of hospital admissions. Int Urol Nephrol. 2013;45:769-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Fabbian F, De Giorgi A, Manfredini F, Lamberti N, Forcellini S, Storari A, Gallerani M, Caramori G, Manfredini R. Impact of renal dysfunction on in-hospital mortality of patients with severe chronic obstructive pulmonary disease: a single-center Italian study. Int Urol Nephrol. 2016;48:1121-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Fabbian F, Gallerani M, Pala M, De Giorgi A, Salmi R, Dentali F, Ageno W, Manfredini R. Association between in-hospital mortality and renal dysfunction in 186,219 patients hospitalized for acute stroke in the Emilia-Romagna region of Italy. Angiology. 2014;65:906-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Fabbian F, De Giorgi A, Pala M, Mallozzi Menegatti A, Storari A, Mikhailidis DP, Manfredini R. Renal dysfunction and all-cause mortality in cardio-renal syndrome: calculation of glomerular filtration rate is crucial, independent of the equation. Int J Cardiol. 2013;170:e11-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Argaiz ER, Koratala A, Reisinger N. Comprehensive Assessment of Fluid Status by Point-of-Care Ultrasonography. Kidney360. 2021;2:1326-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |