Published online Jul 26, 2022. doi: 10.4330/wjc.v14.i7.427
Peer-review started: April 7, 2022
First decision: May 12, 2022
Revised: May 13, 2022
Accepted: June 17, 2022
Article in press: June 17, 2022
Published online: July 26, 2022
Processing time: 103 Days and 21.1 Hours
As people living with human immunodeficiency virus (HIV) (PLWH) enjoy longer life expectancy with highly effective antiretroviral therapy, they are encountering challenging cardiovascular health risks.
To retrospectively examine the increasing burden of cardiovascular diseases in PLWH over the past decade.
All hospitalizations for heart failure (HF), ischemic heart disease (IHD), and cerebrovascular disease (CeVD) in PLWH were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD-10-CM codes in the National Inpatient Sample from 2008 to 2018. Outcomes included number of hospitalizations, in-hospital mortality, length of stay, and total hospital charge. Trend of the outcomes from 2008 to 2018 were analyzed using Cochran-Armitage trend test and simple linear regression.
The number of hospitalizations for HF in PLWH increased from 4212 in 2008 to 6700 in 2018 (Ptrend < 0.01). Similar increasing trend was seen with those for IHD and CeVD over the decade (Ptrend < 0.01). A decreasing trend of in-hospital mortality was observed in all hospitalizations of PLWH (Ptrend < 0.01) and CeVD in PLWH (Ptrend < 0.01), but not in those for HF (Ptrend = 0.67) and IHD (Ptrend = 0.13). The trend of length of stay was decreasing in all hospitalizations of PLWH (Ptrend < 0.01), but increasing in those for HF in PLWH (Ptrend < 0.01). An increasing trend of total hospital charge was observed in hospitalizations for HF, IHD, and CeVD (Ptrend < 0.01).
The burden of cardiovascular diseases has significantly increased in hospitalizations of PLWH from 2008 to 2018. Continued efforts are needed to address the additional cardiovascular risks in this vulnerable population.
Core Tip: People living with human immunodeficiency virus (HIV) are at risk of developing cardi
- Citation: Park DY, An S, Romero ME, Murthi M, Atluri R. National trend of heart failure and other cardiovascular diseases in people living with human immunodeficiency virus. World J Cardiol 2022; 14(7): 427-437
- URL: https://www.wjgnet.com/1949-8462/full/v14/i7/427.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i7.427
As of the year 2020, human immunodeficiency virus (HIV) affected 37.7 million people worldwide with 1.5 million new diagnoses and 680000 deaths due to illnesses associated with acquired immunodeficiency syndrome (AIDS)[1]. HIV infection used to be a debilitating disease leading to fatal infectious diseases, but with the advent of highly effective antiretroviral therapy, life expectancy for people living with HIV (PLWH) has increased by up to 10 years, approaching near-normal life expectancy especially in compliant patients[2,3]. As a result, the importance of cardiovascular diseases (CVDs) in PLWH is continually increasing, especially with new studies suggesting that inflammation and immune activation associated with HIV infection are contributing to additional cardiovascular risk[4].
Many previous studies have indicated that HIV infection is an independent risk factor for CVDs and cerebrovascular diseases (CeVDs), including heart failure (HF), myocardial infarction, and stroke[5-7]. However, studies on yearly dynamic changes brought about by CVDs in PLWH are lacking. Given the increasing burden of CVDs in PLWH, this study serves to elucidate the yearly trend of CVDs in PLWH by examining associated hospitalizations and in-hospital mortality from 2008 to 2018. Heart failure, along with ischemic heart disease (IHD) and CeVD, was used to represent the burden of CVDs in PLWH changing over the years[8].
All data used in this study are openly available in the public website of Healthcare Cost and Utilization Project (HCUP) at https://www.hcup-us.ahrq.gov/nisoverview.jsp. The National Inpatient Sample (NIS), a retrospective cohort study developed for the HCUP, is the largest publicly available inpatient database that covers more than 97% of the U.S. population stratified by hospital region and type of insurance[9]. The NIS consists of demographic and hospital characteristics at discharge, which are searchable using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and ICD-10-CM codes[10]. As the NIS is fully de-identified and public, ethics committee approval was not required in this study. The datasets used and analyzed during this study are available at https://www.hcup-us.ahrq.gov/databases.jsp[9].
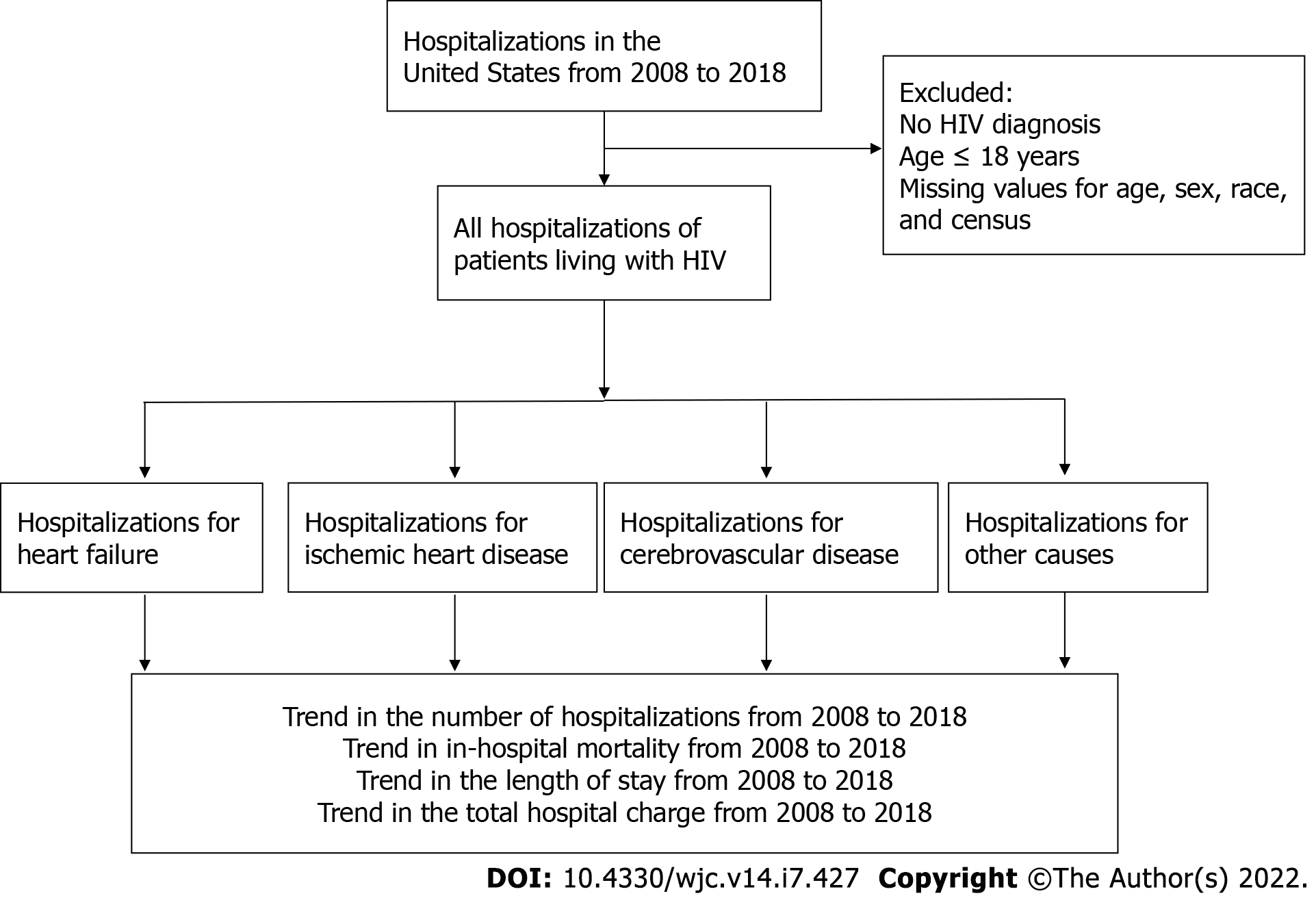
Total number of hospitalizations of PLWH was calculated as the sum of all hospitalizations with primary or secondary diagnosis of HIV: ICD-9-CM codes 042 and V08, or ICD-10-CM codes B20-24, R75, and Z21. Primary discharge diagnoses of CVDs were defined as follows: HF (ICD-9-CM codes 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428; ICD-10-CM codes I11.0, I13.0, I13.2, I09.81, I50), IHD (ICD-9-CM codes 410-411; ICD-10-CM codes I20-I25), and CeVD (ICD-9-CM codes 430-438; ICD-10-CM codes I60-I70). HF was chosen as the main CVD of interest as it comprised the largest proportion among the three. Other CVDs, including IHD and CeVD, were also included. The proportion of each CVD among all hospitalizations of PLWH was then calculated for each year. Only patients above 18 years were included, and hospitalizations with missing information on age, sex, and mortality status were excluded (Figure 1).
The primary outcome of this study was the in-hospital mortality of hospitalizations due to each of the selected CVDs in PLWH. Secondary outcomes included length of hospital stay and total hospital charges.
To calculate estimates that represent total nationwide numbers, survey analysis methods were used based on the weights of hospital-level discharge provided by the NIS. The baseline demographic and hospital characteristics including sex, age, race, comorbidities, Charlson comorbidity index, hospital region, hospital bed size, and location were summarized as percentages for categorical variables and as means with standardized error for continuous variables. The crude mortality rate was calculated by each year and linear trends were examined using the Cochran-Armitage trend test. The trends in continuous outcomes were tested based on simple linear regression. A P value of less than or equal to 0.05 was considered statistically significant. All analyses were conducted using SAS, version 9.4 (SAS Institute, Cary, NC).
From 2008 to 2018, 54987 hospitalizations of adults (> 18 years) with a primary diagnosis of heart failure and secondary diagnosis of HIV were examined. Hospitalization with a primary diagnosis of HF and secondary diagnosis of HIV steadily increased from 4212 in 2008 to 6,700 in 2018 (Ptrend < 0.001). The yearly demographics and comorbidities are shown in Table 1. About two-thirds of the population were male (65.5% in 2008 and 69.6% in 2018). In the year 2008, age less than 50 years was the largest group, but with progression of time, age group spanning from 50 to 59 years became the largest group. Majority of the population consisted of black race, which decreased over the years from 74.6% in 2008 to 71.5% in 2018 (Ptrend < 0.001). Comorbidities of hypertension, diabetes mellitus, chronic kidney disease, obesity, and chronic obstructive pulmonary disease all significantly increased from 2008 to 2018 (Ptrend < 0.001). Of note, hypertension and obesity markedly increased from 65.9% and 7.3% in 2008 to 91.2% and 17.1% in 2018, respectively. Such phenomenon was redemonstrated in the significantly increasing trend of Charlson comorbidity index over the years (Ptrend < 0.001). These findings are shown in Table 1.
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Ptrend | |
| n (sample) | 869 | 954 | 1021 | 910 | 825 | 868 | 928 | 979 | 1074 | 1248 | 1340 | < 0.001 |
| n (weighted) | 4212 | 4878 | 5225 | 4362 | 4125 | 4340 | 4640 | 4895 | 5370 | 6240 | 6700 | < 0.001 |
| Sex (%) | ||||||||||||
| Male | 65.5 | 67.1 | 68.5 | 64.8 | 69.0 | 68.4 | 65.7 | 67.4 | 68.0 | 67.2 | 69.6 | < 0.001 |
| Female | 34.5 | 32.9 | 31.5 | 35.2 | 31.0 | 31.6 | 34.3 | 32.6 | 32.0 | 32.8 | 30.4 | < 0.001 |
| Age (%) | ||||||||||||
| < 50 | 41.8 | 38.8 | 41.2 | 36.7 | 29.7 | 27.2 | 29.1 | 27.4 | 28.1 | 25.0 | 24.9 | < 0.001 |
| 50-59 | 35.2 | 38.5 | 36.2 | 41.3 | 41.1 | 42.5 | 42.0 | 39.6 | 37.9 | 37.3 | 35.1 | < 0.001 |
| 60-69 | 16.7 | 16.7 | 16.5 | 16.5 | 20.8 | 22.8 | 22.2 | 24.8 | 26.9 | 28.8 | 29.0 | < 0.001 |
| ≥ 70 | 6.3 | 6.0 | 6.1 | 5.5 | 8.4 | 7.5 | 6.7 | 8.2 | 7.1 | 8.9 | 10.0 | < 0.001 |
| Race (%) | ||||||||||||
| White | 11.8 | 12.0 | 12.8 | 13.6 | 16.9 | 15.5 | 18.1 | 16.9 | 17.3 | 17.6 | 15.9 | < 0.001 |
| Black | 74.6 | 74.5 | 76.2 | 76.4 | 71.7 | 72.1 | 70.2 | 73.8 | 71.5 | 69.2 | 71.5 | 0.002 |
| Hispanic | 10.9 | 8.9 | 8.3 | 6.2 | 6.6 | 7.9 | 8.5 | 5.6 | 7.7 | 8.8 | 9.5 | 0.203 |
| Asian | 0.6 | 0.1 | 0.3 | 0.3 | 0.5 | 0.5 | 0.2 | 0.3 | 0.7 | 1.1 | 0.7 | < 0.001 |
| AI/AN | 0.1 | 0.0 | 0.1 | 0.0 | 0.1 | 0.4 | 0.2 | 0.2 | 0.0 | 0.1 | 0.3 | < 0.001 |
| Other | 2.0 | 4.5 | 2.3 | 3.5 | 4.2 | 3.6 | 2.8 | 3.2 | 2.7 | 3.2 | 2.1 | < 0.001 |
| Comorbidities (%) | ||||||||||||
| Hypertension | 65.9 | 67.9 | 64.7 | 67.5 | 81.8 | 80.1 | 68.4 | 69.7 | 86.6 | 73.4 | 91.2 | < 0.001 |
| Diabetes mellitus | 33.4 | 33.2 | 31.3 | 32.5 | 34.4 | 35.1 | 37.8 | 37.4 | 38.0 | 37.9 | 36.7 | < 0.001 |
| CKD | 53.1 | 50.4 | 50.4 | 49.2 | 53.9 | 56.9 | 54.5 | 58.1 | 60.6 | 62.6 | 61.0 | < 0.001 |
| Obesity | 7.3 | 7.9 | 11.8 | 11.3 | 10.1 | 12.4 | 14.4 | 18.8 | 16.3 | 16.3 | 17.1 | < 0.001 |
| COPD | 31.2 | 32.7 | 33.0 | 38.1 | 43.8 | 47.1 | 39.4 | 42.2 | 41.4 | 42.6 | 43.4 | < 0.001 |
| Charlson comorbidity index | ||||||||||||
| Mean (SD) | NR | NR | 6.18 (0.10) | 6.17 (0.11) | 6.11 (0.12) | 6.28 (0.11) | 6.27 (0.11) | 5.37 (0.11) | 6.86 (0.10) | 7.19 (0.09) | 6.99 (0.09) | < 0.001 |
| Hospital characteristics | ||||||||||||
| Hospital region (%) | ||||||||||||
| Northwest | 25.4 | 35.3 | 35.9 | 30.9 | 32.1 | 31.8 | 28.0 | 274 | 24.8 | 25.8 | 26.3 | < 0.001 |
| Midwest | 11.5 | 11.1 | 13.1 | 11.4 | 11.6 | 9.7 | 13.6 | 11.7 | 10.4 | 9.3 | 11.6 | < 0.001 |
| South | 58.6 | 48.9 | 44.7 | 52.5 | 46.1 | 49.8 | 50.7 | 54.4 | 54.5 | 54.3 | 53.7 | < 0.001 |
| West | 4.5 | 4.7 | 6.4 | 5.2 | 10.2 | 8.8 | 7.7 | 6.4 | 10.3 | 10.7 | 8.4 | < 0.001 |
| Hospital bed size (%) | ||||||||||||
| Small | 8.1 | 9.5 | 9.6 | 6.0 | 11.5 | 10.3 | 16.8 | 13.3 | 14.4 | 17.0 | 17.8 | < 0.001 |
| Medium | 21.7 | 25.0 | 24.6 | 23.5 | 30.3 | 28.8 | 26.4 | 30.6 | 29.9 | 27.0 | 27.6 | < 0.001 |
| Large | 70.2 | 65.5 | 65.8 | 70.5 | 58.2 | 60.9 | 56.8 | 56.1 | 55.7 | 56.0 | 54.6 | < 0.001 |
| Urban location (%) | ||||||||||||
| Rural | 5.5 | 3.8 | 2.9 | 3.4 | 2.9 | 3.6 | 2.6 | 3.4 | 3.1 | 3.8 | 4.0 | < 0.001 |
| Urban nonteaching | 28.0 | 28.7 | 29.2 | 33.3 | 26.4 | 24.3 | 16.9 | 18.0 | 18.0 | 13.9 | 14.1 | < 0.001 |
| Urban teaching | 66.5 | 67.5 | 68.0 | 63.3 | 70.7 | 72.1 | 80.5 | 78.6 | 78.9 | 82.2 | 81.9 | < 0.001 |
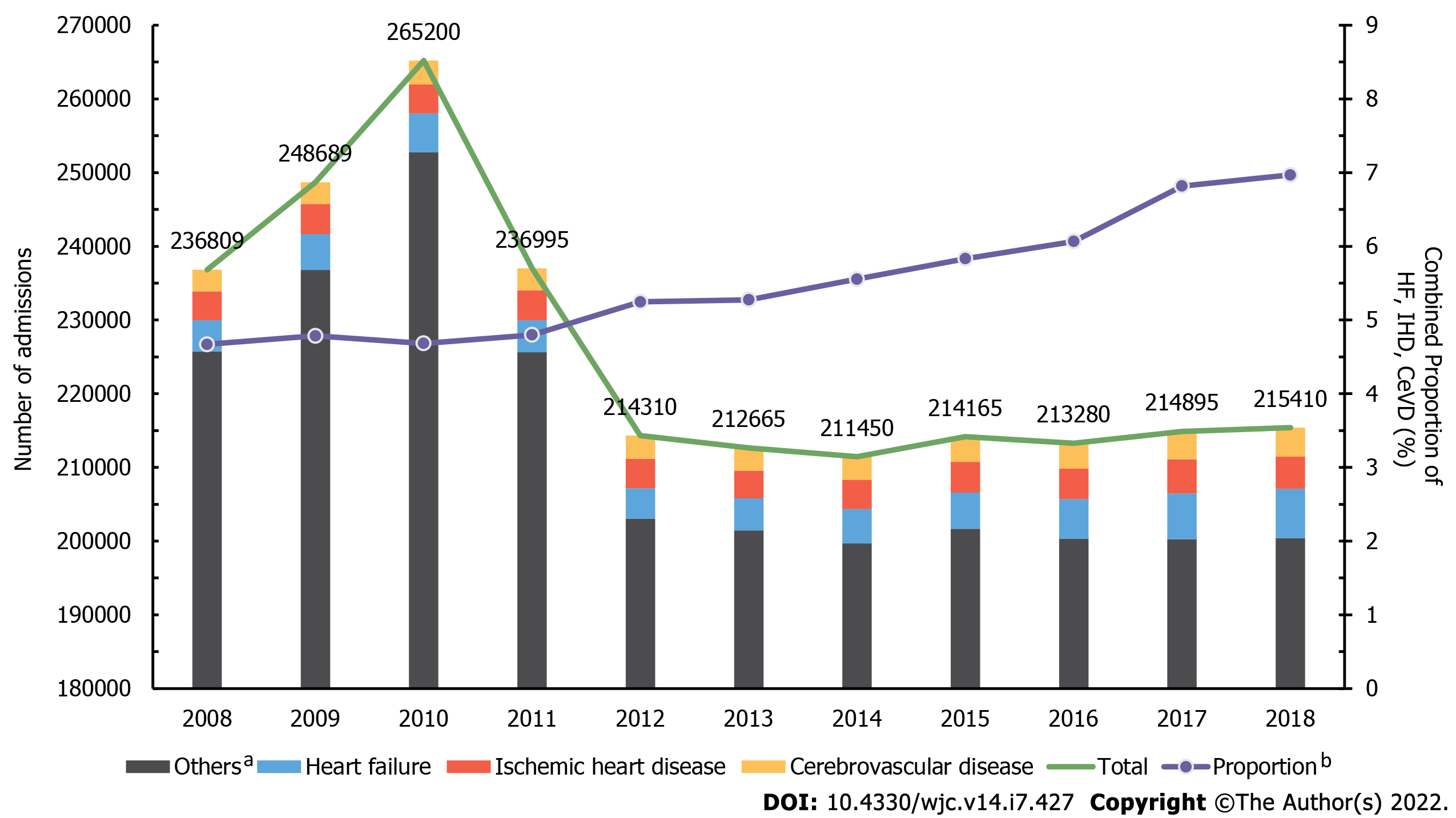
A total of 2,483,868 hospitalizations of PLWH with either primary or secondary diagnosis of HIV were reported from 2008 to 2018. Hospitalizations due to HF in PLWH increased from 4212 in 2008 to 6700 in 2018 (Ptrend < 0.001). IHD (3921 in 2008 and 4,350 in 2018) and CeVD (2927 in 2008 and 3960 in 2018) followed the same pattern (both Ptrend < 0.001). However, the overall hospitalizations of PLWH decreased from 236,809 in 2008 to 215,410 in 2018 (Ptrend < 0.001). At the same time, the proportion of HF, IHD, and CeVD over all hospitalizations of PLWH increased from 4.7% in 2008 to 7.0% in 2018 (all Ptrend < 0.001). These findings are illustrated in Figure 2.
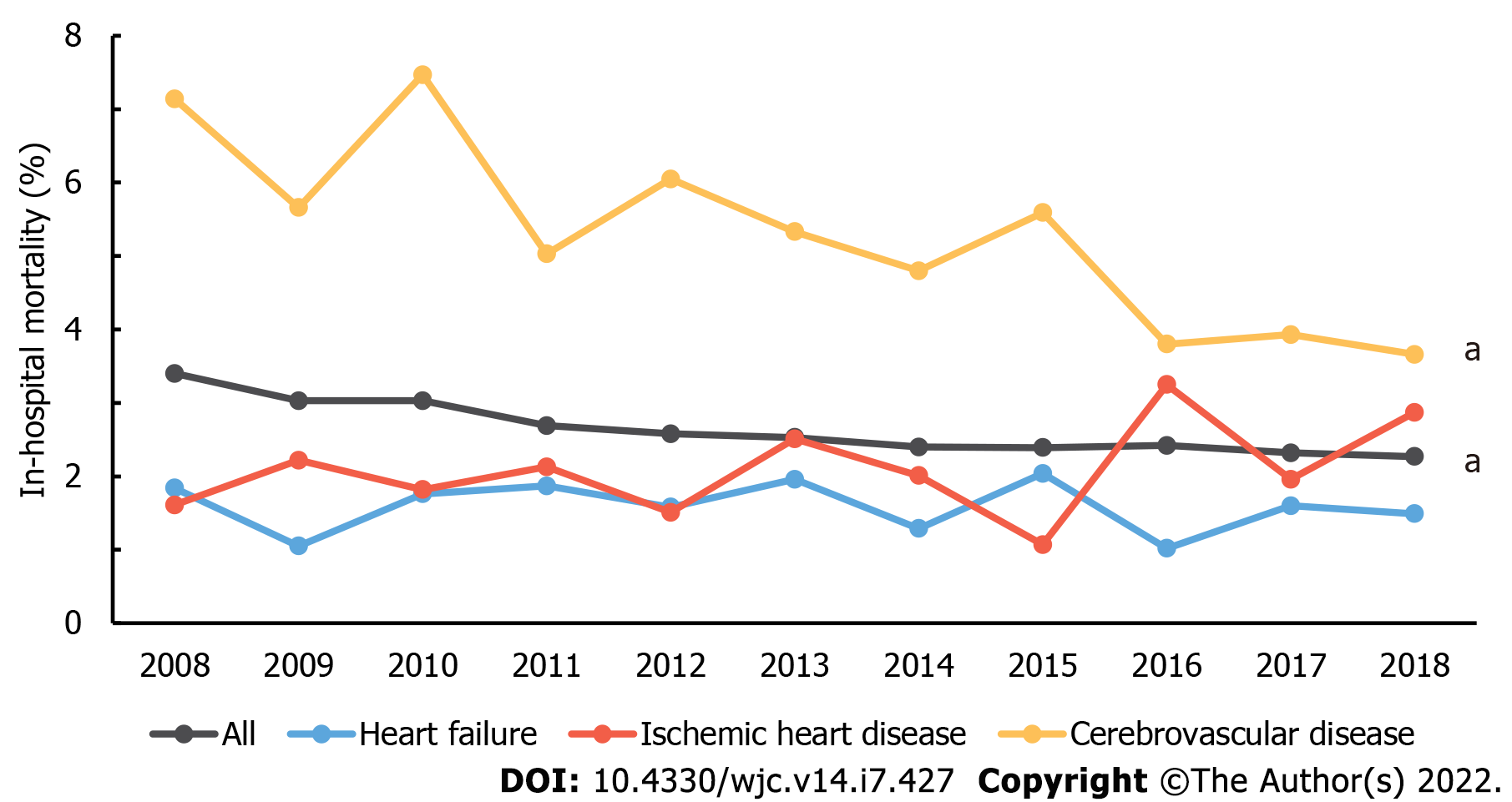
There was a statistically significant decline in the in-hospital mortality of all hospitalizations of PLWH (Ptrend < 0.001) from 3.40% in 2008 to 2.28% in 2018. A similar decline was observed in the in-hospital mortality of CeVD in PLWH (Ptrend < 0.001) from 7.14% in 2008 to 3.67% in 2018. On the other hand, no significant difference was found in the trend of in-hospital mortality rate in hospitalizations due to HF or IHD in PLWH. In-hospital mortality rate was 1.84% in 2008 and 1.49% in 2018 for heart failure (Ptrend = 0.672), and 1.61% in 2008 and 2.87% in 2018 for IHD (Ptrend = 0.13). Figure 3 illustrates these findings.
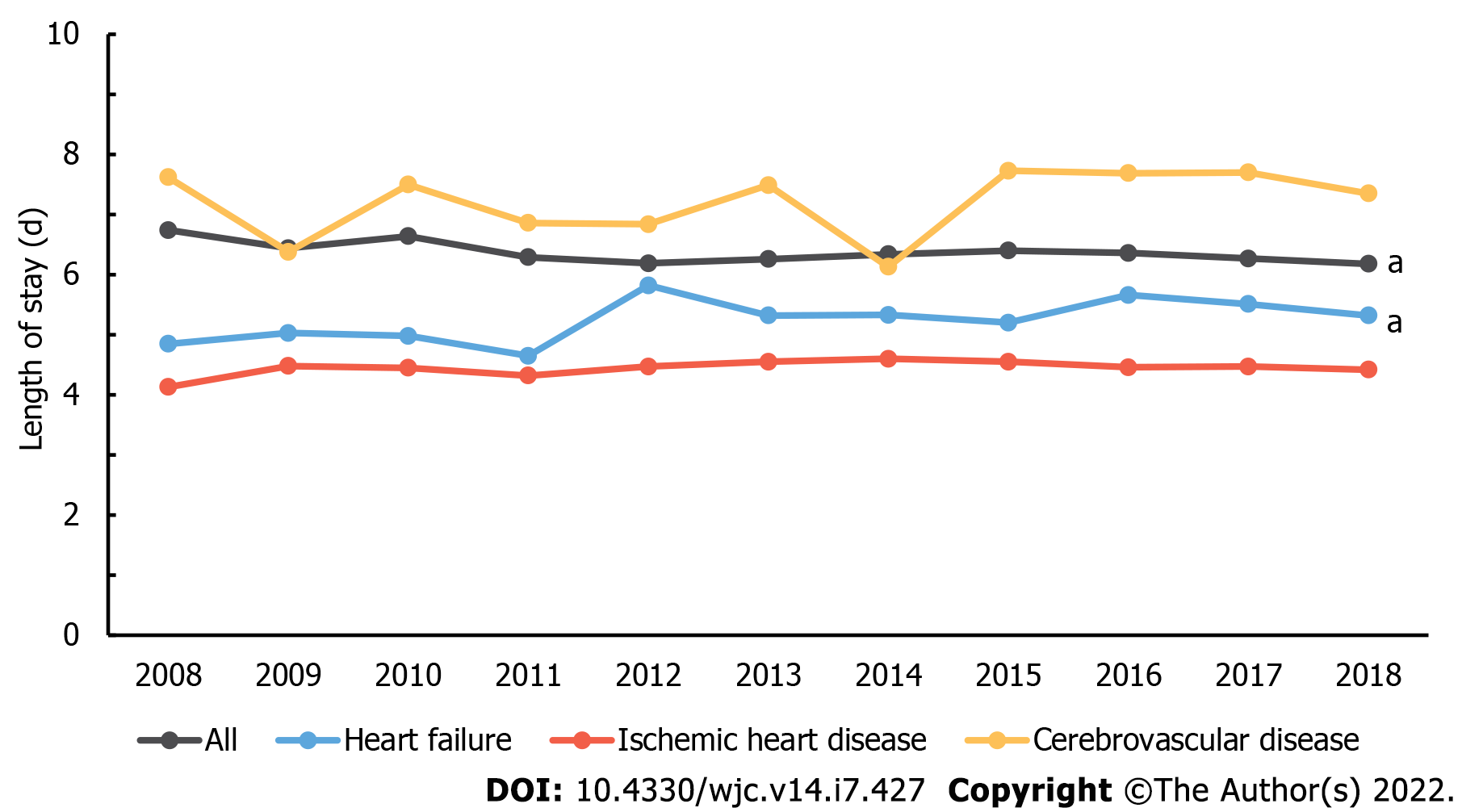
Average length of hospital stay in all hospitalizations of PLWH decreased from 6.74 days in 2008 to 6.18 days in 2018 (Ptrend < 0.001). However, that of HF in PLWH increased from 4.85 days in 2008 to 5.32 days in 2018 (Ptrend < 0.001). No significant trend was found with IHD (Ptrend = 0.294) and CeVD (Ptrend = 0.341). These trends are illustrated in Figure 4.
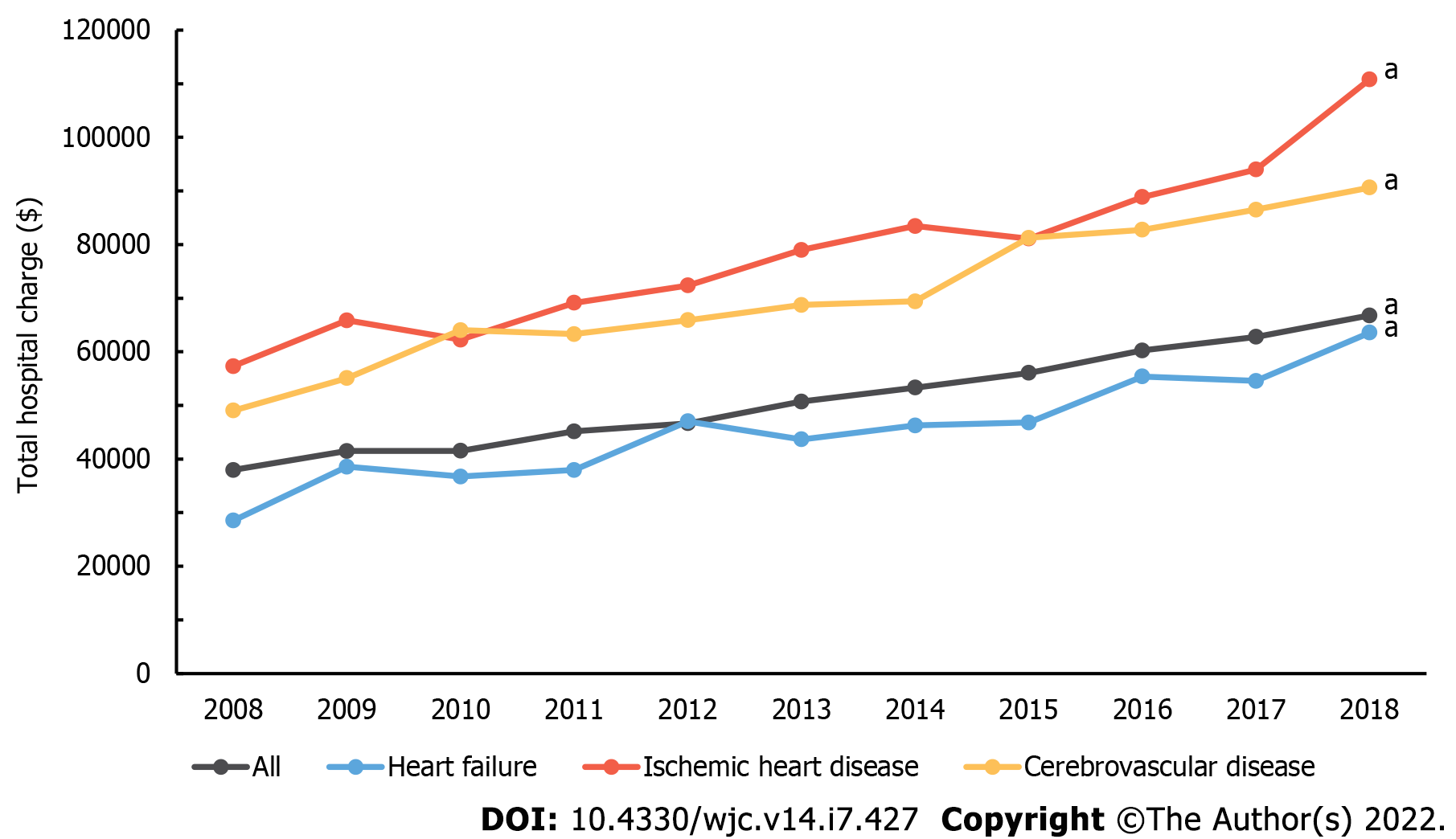
Statistically significant increase in average total hospital charge was observed in all hospitalizations of PLWH from 2008 to 2018. Similar trend was seen in hospitalizations for HF, IHD, and CeVD in PLWH (Figure 5). In absolute terms, IHD showed the greatest increase by $53500 from $57324 in 2008 to $110824. In relative terms, HF increased by 123% from $28503 in 2008 to $63566 in 2018. The order of total hospital charge was IHD, CeVD, and HF from highest to lowest.
PLWH have increased risks of CVDs, including myocardial infarction, HF, sudden cardiac death, peripheral artery disease, and CeVD[11,12]. The mechanism of this increased risk has been explained by a combination of factors in HIV tropism in cardiac myocytes and effects related to the immunologic response triggered by HIV[13,14]. In addition, traditional cardiovascular risk factors, such as dyslipidemia, diabetes, smoking, and HTN are more prevalent in PLWH[15]. Genetic factors and the association of antiretroviral and metabolic abnormalities may also be playing a role in increasing cardiovascular risks in PLWH[16,17,18]. On the other hand, immune activation and chronic inflammation mediated by HIV contribute to the progression of CVD. Ongoing viral replication and release of inflammatory markers, such as hsCRP, IL-6, and D-Dimer, trigger subclinical atherosclerosis and increase CV events[4]. HIV-associated atherosclerosis is known to have its own features, such as non-calcified plaques, given this chronic inflammation[11,19]. Even with HIV suppression with antiretroviral therapy, chronic inflammation persists, putting PLWH at risk of more cardiovascular events[4].
According to the trends described in the present study, hospitalizations due to HF, IHD, and CeVD in PLWH increased while overall hospitalizations of PLWH decreased. This is likely related to the impact of highly effective antiretroviral therapy, which allowed PLWH to have near-normal life expectancy and resulted in a rise in morbidity and mortality associated with age-related causes[20,21]. The dramatic changes brought about by antiretroviral therapy is shown by how the annual mortality of PLWH exceeded 20% prior to 1996 but declined to less than 2% only after a decade later[22]. With improvement in life expectancy, reduction of infectious burden, and changes in lifestyle, the prevalence of CVD is also expected to increase[23]. Increase in the prevalence of comorbidities among PLWH was also noted in the present study (Table 1).
Interestingly, a precipitous reduction in hospitalizations of PLWH from 2010 to 2012 was observed. This may be due to the National HIV/AIDS Strategy implemented in 2010, intensifying HIV prevention efforts, facilitating access to care for PLWH, and creating a coordinated national response to the HIV epidemic[24,25]. The President’s Emergency Plan for AIDS Relief in the U.S., whereby the government supported high active antiretroviral therapy (HAART) for more than 3.9 million people and provided care for nearly 13 million people, was also expanded in the year 2011[26]. With these national efforts to combat HIV, hospitalizations of PLWH have been subdued since 2012 and has been remaining relatively stable.
The trend analysis from this present study coincides with those seen in previous studies. According to a population-based cohort study from 1999 to 2018, diagnosis and mortality rate of HIV infection underwent annual decrease of 5% and 8%, respectively[27]. Earlier diagnosis, lower probability of AIDS-associated infections, and antiretroviral therapy factored into this decline[27]. The decline of in-hospital mortality of CeVD in PLWH seen in this study may be due to the reduced severity of stroke among PLHW explained by the effectiveness of HAART and better tools for stroke diagnosis and treatment[28]. This study did not show significant changes in the in-hospital mortality of HF and IHD in PLWH despite other epidemiological studies showing a decrease in the general population[29,30]. From such finding, one can hypothesize that additional cardiovascular risk factors are present in PLWH, which are not being sufficiently addressed.
The decrease in average length of hospital stay in PLWH over time has also been reported by a retrospective study of more than 700,000 admissions in three hospitals in New York City[31]. Rowell-Cunsolo et al[31] reported decreases in length of stay from 2006 to 2014, but noted that the length of stay was greater in PLWH than the general population. Other studies have also produced comparable results, including Berry et al[32] who reported decline in hospitalizations due to AIDS-defining illnesses from 6.7 to 2.7 per 100 person-years from 2001 to 2008 and Heslin et al[33] who reported 10% decrease in length stay from 2006 to 2013[32,33].
To the best of authors’ knowledge, the present study was the first to use the largest inpatient database in the U.S. to examine the trend in the number of hospitalizations, stratified to cardiovascular causes, in people living with HIV. In addition, trends in the in-hospital mortality, length of hospital stay, and total hospital charge were also uniquely examined. By analyzing the yearly trend of CVDs in PLWH, the objective of this study is to increase the awareness of burden of CVD in this more vulnerable population. Hospitalizations due to CVD has increased in PLWH, highlighting the importance of evaluating and managing cardiovascular risks factors imparted by HIV. Meanwhile, more research investigating the underlying mechanisms that link HIV and CVD must continue to provide potential solutions to this problem of additional risk. Mechanisms whereby antiretrovirals may contribute to this risk should also be studied. With better understanding of the association between HIV infection and CVD, tailored approaches may be warranted in managing cardiovascular risk factors in PLWH.
This study contains several limitations. Administrative data was used for clinical outcomes by using NIS in analyzing yearly trends for CVDs in PLWH. NIS data can have varying degrees of accuracy since cardiovascular events can be coded differently, leading to underestimation of event rates and misclassification[34]. As this study relied on NIS data, there was no control in either exposure or outcome. Not all cardiovascular diseases were included in the analysis. Age-standardized in-hospital mortality could not be calculated due to the skewed distribution of mortalities in different age groups. Prospective cohort studies should be implemented to better examine the burden of CVD in PLWH.
The present study used a national representative sample of U.S. hospital admissions from 2008 to 2018 to reach the following conclusions. First, hospitalizations due to HF, IHD, and CeVD in PLWH increased while total hospitalizations of PLWH decreased. Second, hospitalizations due to HF in PLWH steadily increased over 11 years along with the concomitant increase in the prevalence of comorbidities. Third, declining trends in the in-hospital mortality rate of overall hospitalizations in PLWH and those due to CeVD in PLWH were observed, whereas no change in trend was present with HF and IHD. Fourth, while the length of hospital stay in all hospitalizations of PLWH decreased, that due to HF increased. Finally, the healthcare costs increased for all admissions for all HF, IHD, and CeVD in PLWH. The results from this study demonstrate the increasing burden of CVD in PLWH as demonstrated by increasing hospitalizations, lack of improvement in in-hospital mortality, and increased length of hospital stay in those with HF.
Recent studies have reported a strong association between human immunodeficiency virus (HIV) infection and cardiovascular diseases. However, studies examining the trend of cardiovascular diseases in people living with HIV on a national level have been lacking.
The trends of cardiovascular diseases in people living with HIV have not been sufficiently examined using nationally representative database.
To demonstrate that the burden of cardiovascular disease in people living with HIV has been increasing in the recent decade, emphasizing the need for continual efforts to address the excess cardiovascular risks in this vulnerable population.
We retrospectively examined the National Inpatient Sample from 2008 to 2018 to analyze the trends in the hospitalizations for various cardiovascular diseases in people living with HIV. In addition, we looked at the trends of in-hospital mortality, length of hospital stay, and total hospital charge. Cochran-Armitage test and simple linear regression were used to examine the trends of categorical and continuous variables, respectively.
Hospitalizations for heart failure, ischemic heart disease, and cerebrovascular disease in people living with HIV showed an increasing trend, while the total number of hospitalizations in people with living HIV showed a decreasing trend from 2008 to 2018. The trend of in-hospital mortality and length of stay were variable in contrast to total hospital charge, which demonstrated a substantially increasing trend over the decade.
Nationally representative data showed that the burden of cardiovascular diseases in people living with HIV has been significantly.
Further studies and preventative measures are needed to mitigate the additional cardiovascular burden in people living with HIV.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (
P-Reviewer: Mohan S, India; Wierzbicka A, Poland S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | UNAIDS Report on the Global AIDS Epidemic. [cited 20 April 2022]. Available from: https://www.unaids.org/. |
| 2. | Antiretroviral Therapy Cohort Collaboration. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4:e349-e356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 555] [Cited by in RCA: 762] [Article Influence: 95.3] [Reference Citation Analysis (0)] |
| 3. | Rodger AJ, Lodwick R, Schechter M, Deeks S, Amin J, Gilson R, Paredes R, Bakowska E, Engsig FN, Phillips A; INSIGHT SMART, ESPRIT Study Groups. Mortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general population. AIDS. 2013;27:973-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 290] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 4. | Triant VA. Cardiovascular disease and HIV infection. Curr HIV/AIDS Rep. 2013;10:199-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 150] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 5. | Chow FC, Regan S, Feske S, Meigs JB, Grinspoon SK, Triant VA. Comparison of ischemic stroke incidence in HIV-infected and non-HIV-infected patients in a US health care system. J Acquir Immune Defic Syndr. 2012;60:351-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 276] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 6. | Freiberg MS, Chang CC, Kuller LH, Skanderson M, Lowy E, Kraemer KL, Butt AA, Bidwell Goetz M, Leaf D, Oursler KA, Rimland D, Rodriguez Barradas M, Brown S, Gibert C, McGinnis K, Crothers K, Sico J, Crane H, Warner A, Gottlieb S, Gottdiener J, Tracy RP, Budoff M, Watson C, Armah KA, Doebler D, Bryant K, Justice AC. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 886] [Cited by in RCA: 1041] [Article Influence: 86.8] [Reference Citation Analysis (0)] |
| 7. | Remick J, Georgiopoulou V, Marti C, Ofotokun I, Kalogeropoulos A, Lewis W, Butler J. Heart failure in patients with human immunodeficiency virus infection: epidemiology, pathophysiology, treatment, and future research. Circulation. 2014;129:1781-1789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 8. | Olvera Lopez E, Ballard BD, Jan A. Cardiovascular Disease. 2021 Aug 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. [PubMed] |
| 9. | Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality. [cited 20 April 2022]. Available from: www.hcup-us.ahrq.gov/db/nation/nis/nisarchive.jsp. |
| 10. | Mohan S, Thirumalai C and Rababah A. Classification of Heart Disease Using Cluster Based DT Learning. Journal of Computer Science. 2020;16:50-55. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Hsue PY, Waters DD. Time to Recognize HIV Infection as a Major Cardiovascular Risk Factor. Circulation. 2018;138:1113-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 93] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 12. | Delabays B, Cavassini M, Damas J, Beuret H, Calmy A, Hasse B, Bucher HC, Frischknecht M, Müller O, Méan M, Vollenweider P, Marques-Vidal P, Vaucher J. Cardiovascular risk assessment in people living with HIV compared to the general population. Eur J Prev Cardiol. 2022;29:689-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Prendergast BD. HIV and cardiovascular medicine. Heart. 2003;89:793-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | McGettrick P, Mallon PWG. Biomarkers to predict cardiovascular disease in people living with HIV. Curr Opin Infect Dis. 2022;35:15-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | So-Armah K, Freiberg MS. HIV and Cardiovascular Disease: Update on Clinical Events, Special Populations, and Novel Biomarkers. Curr HIV/AIDS Rep. 2018;15:233-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Blanco F, San Román J, Vispo E, López M, Salto A, Abad V, Soriano V. Management of metabolic complications and cardiovascular risk in HIV-infected patients. AIDS Rev. 2010;12:231-241. [PubMed] |
| 17. | Carr A, Samaras K, Burton S, Law M, Freund J, Chisholm DJ, Cooper DA. A syndrome of peripheral lipodystrophy, hyperlipidaemia and insulin resistance in patients receiving HIV protease inhibitors. AIDS. 1998;12:F51-F58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1793] [Cited by in RCA: 1691] [Article Influence: 62.6] [Reference Citation Analysis (0)] |
| 18. | Mohan S, Thirumalai C and Srivastava G. Effective Heart Disease Prediction Using Hybrid Machine Learning Techniques. IEEE Access. 2019;7:81542-81554. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1218] [Cited by in RCA: 223] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 19. | Poznyak AV, Bezsonov EE, Borisov EE, Grechko AV, Kartuesov AG, Orekhov AN. Atherosclerosis in HIV Patients: What Do We Know so Far? Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Alonso A, Barnes AE, Guest JL, Shah A, Shao IY, Marconi V. HIV Infection and Incidence of Cardiovascular Diseases: An Analysis of a Large Healthcare Database. J Am Heart Assoc. 2019;8:e012241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 137] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 21. | An S, Ahn C, Moon S, Sim EJ, Park SK. Individualized Biological Age as a Predictor of Disease: Korean Genome and Epidemiology Study (KoGES) Cohort. J Pers Med. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | May MT, Sterne JA, Costagliola D, Sabin CA, Phillips AN, Justice AC, Dabis F, Gill J, Lundgren J, Hogg RS, de Wolf F, Fätkenheuer G, Staszewski S, d'Arminio Monforte A, Egger M; Antiretroviral Therapy (ART) Cohort Collaboration. HIV treatment response and prognosis in Europe and North America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet. 2006;368:451-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 179] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 23. | Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. Can J Cardiol. 2010;26 Suppl C:8C-13C. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 154] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 24. | 30 Years of AIDS. Honoring the Past, Looking Toward the Future [web site], 2011. [cited 20 April 2022]. Available from: https://hab.hrsa.gov/livinghistory/2011. |
| 25. | Prior National HIV/AIDS Strategies (2010-2021). [cited 20 April 2022]. Available from: https://www.hiv.gov/federal-response/national-hiv-aids-strategy/national-hiv-aids-strategies-2010-2021. |
| 26. | FACT SHEET: The Beginning of the End of AIDS. [cited 20 April 2022]. Available from: https://obamawhitehouse.archives.gov/the-press-office/2011/12/01/fact-sheet-beginning-end-aids. |
| 27. | Fontela C, Aguinaga A, Moreno-Iribas C, Repáraz J, Rivero M, Gracia M, Floristán Y, Fresán U, Miguel RS, Ezpeleta C, Castilla J. Trends and causes of mortality in a population-based cohort of HIV-infected adults in Spain: comparison with the general population. Sci Rep. 2020;10:8922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 28. | Lin HL, Muo CH, Lin CY, Chen HJ, Chen PC. Incidence of stroke in patients with HIV infection: A population-based study in Taiwan. PLoS One. 2019;14:e0217147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Bytyçi I, Bajraktari G. Mortality in heart failure patients. Anatol J Cardiol. 2015;15:63-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 30. | Nowbar AN, Gitto M, Howard JP, Francis DP, Al-Lamee R. Mortality From Ischemic Heart Disease. Circ Cardiovasc Qual Outcomes. 2019;12:e005375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 254] [Cited by in RCA: 495] [Article Influence: 82.5] [Reference Citation Analysis (0)] |
| 31. | Rowell-Cunsolo TL, Liu J, Shen Y, Britton A, Larson E. The impact of HIV diagnosis on length of hospital stay in New York City, NY, USA. AIDS Care. 2018;30:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Berry SA, Fleishman JA, Moore RD, Gebo KA; HIV Research Network. Trends in reasons for hospitalization in a multisite United States cohort of persons living with HIV, 2001-2008. J Acquir Immune Defic Syndr. 2012;59:368-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 98] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 33. | Heslin KC, Elixhauser A. HIV Hospital Stays in the United States, 2006–2013: Statistical Brief #206. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US), 2006. [PubMed] |
| 34. | Psaty BM, Delaney JA, Arnold AM, Curtis LH, Fitzpatrick AL, Heckbert SR, McKnight B, Ives D, Gottdiener JS, Kuller LH, Longstreth WT Jr. Study of Cardiovascular Health Outcomes in the Era of Claims Data: The Cardiovascular Health Study. Circulation. 2016;133:156-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |