Published online Nov 26, 2018. doi: 10.4330/wjc.v10.i11.222
Peer-review started: August 14, 2018
First decision: September 7, 2018
Revised: September 8, 2018
Accepted: November 2, 2018
Article in press: November 2, 2018
Published online: November 26, 2018
Processing time: 103 Days and 16.7 Hours
To establish whether frequency-domain optical coherence tomography (FD-OCT) is safe and effective in the evaluation and treatment of angiographically-intermediate coronary lesions (ICL)
Sixty-four patients with 2-dimensional quantitative coronary angiography (2D-QCA) demonstrating ICL were included. OCT imaging was performed. According to predetermined OCT criteria, patients were assigned to either of 2 groups: OCT-guided percutaneous coronary intervention (PCI) or OCT-guided optimal medical therapy (OMT). The primary efficacy endpoint was to demonstrate the superiority and higher accuracy of FD-OCT compared to 2D-QCA in evaluating stenosis severity in patients with ICL. The primary safety endpoint was the incidence of 30-d major adverse cardiac events (MACE). Secondary endpoints included MACE at 12 mo and other clinical events.
Analysis of the primary efficacy endpoint demonstrates that 2D-QCA overestimates the stenosis severity of ICL in both the OCT-guided PCI and OMT groups, proving FD-OCT to be superior to and more precise than 2D-QCA in treating this subset of lesions. The primary safety endpoint was fully met with the incidence of 30-d MACE being nil in both the OCT-guided PCI and OCT-guided OMT groups. Incidences of secondary endpoints were found to be low in both arms, the only exception being the relatively high incidence of recurrent episodes of angina which was, however, very similar in the 2 groups.
FD-OCT is safe and effective in the evaluation and treatment of ICL. Larger studies are needed to firmly establish the efficacy and safety of FD-OCT in treating ICL across all coronary artery disease population subgroups.
Core tip: The management of intermediate coronary lesions (ICL), defined as a diameter stenosis of 40% to 70%, remains a therapeutic dilemma. The 2-dimensional representation of the arterial lesion by angiography is limited in guiding therapy. Frequency-domain optical coherence tomography (FD-OCT) is an ultra-high resolution imaging technique that enables a detailed evaluation of the coronary lumen. Despite its undebatable superiority over angiography and other intravascular imaging techniques, the benefit of FD-OCT over its procedural risks in clinical practice is uncertain. The current study is the first to date to investigate whether FD-OCT is safe and effective in the evaluation of ICL, in guiding treatment, and optimizing procedural outcomes.
- Citation: Khurwolah MR, Meng HY, Wang YS, Wang LS, Kong XQ. Safety and efficacy of frequency-domain optical coherence tomography in evaluating and treating intermediate coronary lesions. World J Cardiol 2018; 10(11): 222-233
- URL: https://www.wjgnet.com/1949-8462/full/v10/i11/222.htm
- DOI: https://dx.doi.org/10.4330/wjc.v10.i11.222
An intermediate coronary lesion (ICL) on angiography is defined as a luminal narrowing with a diameter stenosis ≥ 40% but ≤ 70%. Cardiac catheterisation laboratory assessment of a coronary lesion with intermediate severity continues to be a challenge for cardiologists both from a diagnostic and therapeutic perspective. Selective coronary angiography (CAG) is accepted as the standard for determining the presence and extent of epicardial coronary artery disease (CAD), but has obvious limitations given that it provides only a two-dimensional projection of the three-dimensional geometry of the coronary artery lumen[1,2]. Although there is little controversy regarding the usefulness of CAG in separating patients with entirely normal coronary arteries from those with severe high-grade stenotic lesions, the potential of the coronary arteriogram in predicting the hemodynamic significance of lesions that appear angiographically moderate remains controversial[3]. For this subset of obstructions, a number of adjunctive, invasive techniques have been proposed to improve the diagnostic accuracy of the coronary angiogram. Fractional-flow-reserve (FFR) represents the gold standard to evaluate ICL. Three randomized trials (DEFER, FAME-I and FAME-II) established FFR as the gold standard for assessing the significance of non-left main coronary artery intermediate lesions[4]. Intracoronary FD-OCT, on the other hand, is a novel, advanced imaging technique that allows ultra-high resolution evaluation of the coronary artery lumen, 10-20 times higher than the resolution obtained by intravascular ultrasound (IVUS)[5]. The superior spatial resolution of OCT could thus very well translate into meaningful clinical benefits in patients with ICL. However, while the superiority of OCT in comparison to any other available intravascular imaging modality in terms of spatial resolution is unchallenged, there is uncertainty in its risk-benefit role in routine extensive clinical practice compared to IVUS or angiography alone[6,7]. In the setting of ICL, no interventional study has to date investigated whether FD-OCT, as an invasive intracoronary imaging technique, is safe and effective in the evaluation of ICL, in guiding their treatment, and in optimizing procedural outcomes. Furthermore, the efficacy and safety of OCT in evaluating and treating ICL in patients presenting with acute coronary syndromes (ACS) as opposed to stable angina (SA) alone is unknown. We therefore designed this study aiming to explore the safety and efficacy of FD-OCT in dealing with angiographically-borderline coronary artery lesions in the cardiac catheterisation laboratory.
This was a single center, prospective, interventional study to investigate the safety and efficacy of FD-OCT in the evaluation and treatment of patients with ICL. The study protocol was approved by the ethics committee of the First Affiliated Hospital of Nanjing Medical University (Ethics Approval ID: 2017-SR-328). The study conforms to the Declaration of Helsinki. Each patient gave written informed consent prior to the procedure.
From August 2016 to August 2017, diagnostic CAG was performed at the interventional cardiology center of the First Affiliated Hospital of Nanjing Medical University, Nanjing, China, on patients presenting with one of the following: SA, defined as chest discomfort and associated symptoms precipitated by some form of physical activity, with minimal or non-existent symptoms at rest or after administration of sublingual nitroglycerin, unstable angina (UA, defined as chest pain occurring at rest or minimal exertion and generally lasting more than 20 min, or severe and new-onset chest pain, or chest pain manifesting in a crescendo pattern, with no biochemical evidence of myocardial damage), non ST-elevation myocardial infarction [NSTEMI, biochemical evidence of myocardial damage with no ST-elevation on electrocardiography (ECG)], or ST-elevation myocardial infarction (STEMI, biochemical evidence of myocardial damage with ST-elevation on ECG). Most of these patients had initial non-invasive testing for CAD with either Exercise Stress Test or Coronary Computed Tomography Angiography.Patients of all ages in whom assessment by 2D-QCA demonstrated ICL (considered as lesions with an angiographic stenosis severity of ≥ 45% but < 75%), and who consented to undergo further assessment with OCT, were enrolled in the study to determine whether they would benefit from PCI or OMT. Sixty-four patients with angiographically-demonstrated ICL consented to proceed with imaging. Based on the OCT findings, the patients were assigned to one of 2 arms: OCT-Guided PCI or OCT-Guided OMT. Predetermined OCT criteria used to decide which patient to assign to which arm were as follows: patients with an ICL atherosclerotic plaque burden > 76%, or a minimum luminal area (MLA) < 2.6 mm2, or in whom unstable plaque factors existed (endocardial discontinuity, or a fibrous cap thickness < 65 µm, or a large lipid core > 180 degrees, or evidence of macrophage aggregation) were assigned to the PCI arm. On the other hand, patients with a plaque burden ≤ 76%, and with a MLA ≥ 2.6 mm2, and in whom OCT showed no features of plaque instability were assigned to the OMT group. The inclusion criteria for this study were only those participants in whom diagnostic CAG and 2D-QCA demonstrated ICL and who consented to undergo further evaluation with OCT imaging. Exclusion criteria were subjects presenting with cardiogenic shock, acute stroke, renal dysfunction, left main stem ICL, and acute or chronic total occlusion coronary lesions.
The primary efficacy endpoint of the study was to demonstrate that FD-OCT is superior to and more accurate than 2D-QCA alone in evaluating the degree of stenosis in patients with ICL. The primary safety endpoint was defined as the incidence of 30-d MACE composed of cardiac death, peri-procedural myocardial infarction (MI), acute stent thrombosis, emergency coronary artery bypass graft, significant vessel dissection or perforation, cerebrovascular accident and major vascular complications in both the OCT-guided PCI and OCT-guided OMT groups. Secondary end points were the incidence of MACE at 12 mo, plus recurrent episodes of angina, repeat hospitalisation, major bleeding events, minor bleeding episodes (defined as minimal amount of bleeding, for example bruising, bleeding gums and oozing from injection sites, not requiring intervention or treatment), stroke and heart failure. All outcomes were defined in keeping with the Academic Research Consortium recommendations[8].
2D-QCA measurements of the ICL were performed offline using an automated software. These were done on image sequences adequately filled with contrast and when the vessel was not foreshortened. Calibration was performed on the contrast filled segment of the guiding catheter.
OCT imaging was performed using a FD-OCT system (C7-XR OCT Intravascular Imaging System, St. Jude Medical, St. Paul, MN, United States). The radial approach was used in most patients (87%) for CAG and OCT imaging. Weight-adjusted, unfractionated heparin or bivalirudin was administered for anticoagulation. After placement of the guiding catheter (6 Fr) into the coronary ostium, a standard percutaneous transluminal coronary angioplasty guide wire was advanced into the coronary artery and the lesion was crossed. The C7 Dragonfly™ OCT catheter was then advanced over the wire. Once the catheter was positioned distal to the lesion, it was pulled backed manually at a speed of 15 mm/s. All images were acquired using a non-occlusive technique with manual injection of iso-osmolar iodixanol (Visipaque™ by GE Healthcare) contrast to clear the vessel of blood. OCT image analysis scrutinized serial cross-sectional images of the vessel at 1 mm intervals using the Light Lab Imaging offline software.
Coronary artery parameters measured by 2D-QCA and FD-OCT in the OCT-guided PCI and OCT-guided OMT groups were the following: Reference area (RA), Minimum Luminal Area (MLA) and % Area Stenosis (AS), from which appropriate statistical analysis was performed.
No statistical sample-size calculation was undertaken in this study as this was a pioneering experience of our center in terms of use of intracoronary OCT imaging to assess ICL leading to several patients not consenting to the OCT procedure, hence automatically reducing our sample size, and given the time restriction of the current study to 1 year duration which further limits the number of subjects that could be included in the study, statistical calculation of sample size to achieve a reasonable statistical power would have been futile. Furthermore, no recently published findings from studies with a similar clinical design could be found to enable statistical determination of what sample size of subjects per group is needed to answer the research question. An independent statistician performed the statistical analysis. Continuous variables were expressed as mean ± SD and categorical variables as percentage and counts. Calculations and statistical analyses were performed by using the SPSS 19.0 software (SPSS, Statistics, IBM, United States). The Chi-square or Fisher exact test or χ2 correction test for continuity performed on categorical variables. Continuous variables were tested using the Mann-Whitney U test, student’s t test and Wilcoxon rank-sum test. A P-value of < 0.05 was considered as statistically significant.
All patients were individually followed up for a total period of 12 mo to record the incidence of MACE, defined as the occurrence of any one or more of the following: death, recurrent MI, stent thrombosis or repeat revascularization of the target lesion. Other clinical events recorded during this 12-mo period were the incidences of recurrent episodes of angina, repeat hospitalisation, stroke, heart failure and bleeding events if any. All clinical events were recorded using a clinical report form and evaluated independently by a blinded clinical events committee.
A total of 64 patients were included in the study to proceed with OCT after diagnostic angiography and 2D-QCA demonstrated an angiographically-intermediate coronary lesion. Following OCT imaging and in accordance with the predetermined OCT criteria mentioned above, 38 patients (59.4%) were assigned to the PCI arm, and the other 26 patients (40.6%) to the OMT arm (Table 1). Our study population comprised 43 males (67.2%) and 21 females (32.8%), with an overall mean age of 63.17 ± 9.68 years. 39 patients (60.9%) suffered from hypertension, 10 patients (15.6%) from diabetes, and none reported any bleeding disorder. 53 patients (82.8%) presented with UA, 7 (10.9%) with stable angina (SA), while the NSTEMI and STEMI presentations comprised only 2 patients each (3.1%). The left anterior descending artery comprised most of the ICL (57.8%), followed by the right coronary artery (23.4%) and circumflex artery (18.8%). The mean post-procedural in-hospital stay was 3.0 ± 0.7 d. Discharge treatment was similar in both arms with 100% prescription of aspirin, and 100% and 96.1% prescription of P2Y12 inhibitors in the PCI and OMT groups respectively.
| Variable | Overall (n = 64) | OCT-guided PCI (n = 38) | OCT-guided OMT (n = 26) | P-value |
| Age (yr) | 63.17 ± 9.68 | 63.42 ± 9.88 | 62.81 ± 9.56 | 0.806 |
| Male (%) | 43 (67.2) | 25 (65.8) | 18 (69.2) | 0.773 |
| Diabetes mellitus (%) | 10 (15.6) | 7 (18.4) | 3 (11.5) | 0.693 |
| Hypertension (%) | 39 (60.9) | 22 (57.9) | 17 (65.4) | 0.546 |
| Discharge treatment | ||||
| Aspirin (%) | 64 (100) | 38 (100) | 26 (100) | 1 |
| P2Y12 inhibitor (%) | 59 (92.2) | 38 (100) | 25 (96.1) | 0.406 |
| Statin (%) | 64 (100) | 38 (100) | 26 (100) | 1 |
| Beta-blocker (%) | 29 (45.3) | 19 (50) | 10 (38.5) | 0.362 |
| ACE-I/ARB (%) | 33 (51.6) | 23 (60.5) | 10 (38.5) | 0.083 |
| CCB (%) | 24 (37.5) | 13 (34.2) | 11 (42.3) | 0.511 |
| Nitrates (%) | 36 (56.2) | 21 (55.3) | 15 (57.7) | 0.847 |
| Admission diagnosis | 0.068 | |||
| Stable angina (%) | 7 (10.9) | 4 (10.5) | 3 (11.5) | |
| Unstable angina (%) | 53 (82.8) | 34 (89.5) | 19 (73.1) | |
| NSTEMI (%) | 2 (3.1) | 0 (0) | 2 (7.7) | |
| STEMI (%) | 2 (3.1) | 0 (0) | 2 (7.7) | |
| ICL vessel | 0.671 | |||
| LAD (%) | 37 (57.8) | 21 (55.3) | 16 (61.5) | |
| LCX (%) | 12 (18.8) | 6 (15.8) | 6 (23.1) | |
| RCA (%) | 15 (23.4) | 10 (26.3) | 5 (19.2) |
Of the 38 patients in the PCI group, the vast majority of them (34, 89.5%) presented with UA, only 4 (10.5%) with SA, and none with NSTEMI or STEMI (Table 1). On the other hand, out of the 26 patients treated with OMT, most of them (19, 73.1%) were also admitted with UA, while the rest were divided between SA (3, 11.5%), NSTEMI (2, 7.7%) and STEMI (2, 7.7%). UA was therefore, by far the most common admission diagnosis in both the PCI and OMT groups. Furthermore, from the UA admission subgroup of 53 patients, 34 (64.1%) were treated with PCI while the rest (19, 35.9%) were treated with OMT, while in the SA subgroup of 7 patients, 4 (57.1%) were managed interventionally, and the rest (3, 42.9%) medically. On the other hand, the 4 (6.2%) patients presenting with NSTEMI and STEMI combined were all treated with OMT after OCT imaging was performed.
Pre-OCT 2D-QCA findings are summarized in Table 2. Retrospective analysis of parameters measured by 2D-QCA showed the following: The median RA as obtained from 2D-QCA was 7.97 (6.01-11.16) mm2 in the OMT arm compared to 7.91 (5.6-10.45) mm2 in the PCI arm (P = 0.538). Similarly, the median MLA measured by 2D-QCA was also comparatively larger in the OMT [2.40 (1.73-3.82) mm2] vs the PCI group [1.97 (1.37-2.80) mm2] (P = 0.029). The mean % AS was less severe (67.77% ± 6.44%) in the OMT as opposed to 74.02% ± 6.43% in the PCI arm (P = 0.001).
| Variable | OCT-guided PCI (n = 38) | OCT-guided OMT (n = 26) | P-value |
| Reference area, mm2 | 7.91 (5.61-10.45) | 7.97 (6.01-11.16) | 0.538 |
| Minimum luminal area, mm2 | 1.97 (1.37-2.80) | 2.40 (1.73-3.82) | 0.029 |
| Area stenosis % | 74.02 ± 6.43 | 67.77 ± 6.44 | 0.001 |
These findings are summarized in Table 3. All lesions were suitable for OCT imaging analysis, which revealed a higher mean stenosis severity (mean % AS) of the ICL in the PCI group (72.22% ± 7.39%) compared to the OMT group (61.87% ± 7.51%) (P < 0.001). The median MLA measured by OCT was also smaller in the PCI [2.44 (1.93-3.15) mm2] compared to the OMT arm [3.43 (2.61-4.72) mm2] (P = 0.001), while there was no significant difference between the median RA obtained in the PCI vs the OMT arm (P = 0.507). Furthermore, the ICL in all the patients comprising the PCI group demonstrated either features of plaque instability, or a plaque burden exceeding 76%.
| Variable | OCT-guided PCI (n = 38) | OCT-guided OMT (n = 26) | P-value |
| Reference area mm2 | 9.00 (7.56-11.21) | 9.32 (7.73-12.14) | 0.507 |
| Minimum luminal area mm2 | 2.44 (1.93-3.15) | 3.43 (2.61-4.72) | 0.001 |
| Area stenosis % | 72.22 ± 7.39 | 61.87 ± 7.51 | < 0.001 |
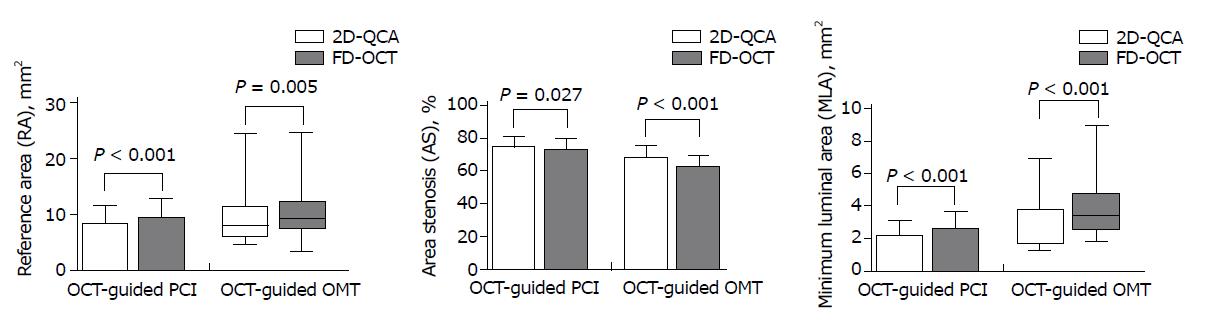
OCT was successfully performed and well-tolerated in all of the intervened patients. The primary efficacy endpoint was met by comparing the mean RA, MLA and AS values obtained by 2D-QCA analysis with similar parameter values from OCT imaging (Table 4). Our results clearly demonstrate that 2D-QCA overestimates the stenosis severity of the ICL both in the OCT-guided PCI and OMT groups. In the PCI group, the mean AS was 72.22% ± 7.39% as assessed by OCT, compared to 74.02% ± 6.44% by 2D-QCA (P = 0.027). In the same group, the mean MLA was found to be 2.58 ± 1.04 mm2 by OCT as opposed to 2.14 ± 1.00 mm2 by 2D-QCA analysis (P < 0.001). Similarly, the mean RA was 9.39 ± 3.28 mm2 by OCT compared to 8.16 ± 3.24 mm2 by 2D-QCA evaluation (P < 0.001). In the OMT group, similar results were obtained in that 2D-QCA assessment demonstrated a comparatively smaller mean RA (P = 0.005) and mean MLA (P < 0.001), thereby leading to an overestimation of the mean % AS by 2D-QCA in comparison with FD-OCT (67.77% ± 7.31% vs 61.87% ± 7.51%), (P < 0.001). The results of the efficacy assessment of OCT compared to 2D-QCA in evaluating the stenosis severity of ICL were therefore statistically significant as illustrated by the box plot diagrams in Figure 1.
| Group | 2D-QCA | FD-OCT | P-value |
| Reference area, mm2 | |||
| OCT-guided PCI | 8.16 ± 3.24 | 9.39 ± 3.28 | < 0.001 |
| OCT-guided OMT | 7.97 (6.01-11.16) | 9.32 (7.73-12.14) | 0.005 |
| Minimum luminal area mm2 | |||
| OCT-guided PCI | 2.14 ± 1.00 | 2.58 ± 1.04 | < 0.001 |
| OCT-guided OMT | 2.40 (1.73-3.82) | 3.43 (2.61- 4.72) | < 0.001 |
| Area stenosis % | |||
| OCT-guided PCI | 74.02 ± 6.44 | 72.22 ± 7.39 | 0.027 |
| OCT-guided OMT | 67.77 ± 7.31 | 61.87 ± 7.51 | < 0.001 |
No procedural complications were observed, including the no-reflow phenomenon, acute vessel occlusions, coronary vasospasm, angiographically-detectable dissections, thrombi formation or embolic phenomena. Transient chest discomfort during the procedure was rare, with no significant ECG changes. Furthermore, none of the patients in the 2 groups developed acute kidney injury following the procedure. There were also no serious in-hospital post-procedural adverse events noted. The primary safety end-point (incidence of MACE at 30 d post-procedure) was fully met in both groups, with none of the 64 patients experiencing any of the following: Cardiac death, post-procedure MI, acute stent thrombosis, significant vessel perforation or dissection, emergent revascularization, major vascular complications or cerebrovascular accidents. However, given the relatively small sample size of this study, the above results pertaining to the 30-d MACE primary safety end-point should be interpreted with caution in the current context of this study.
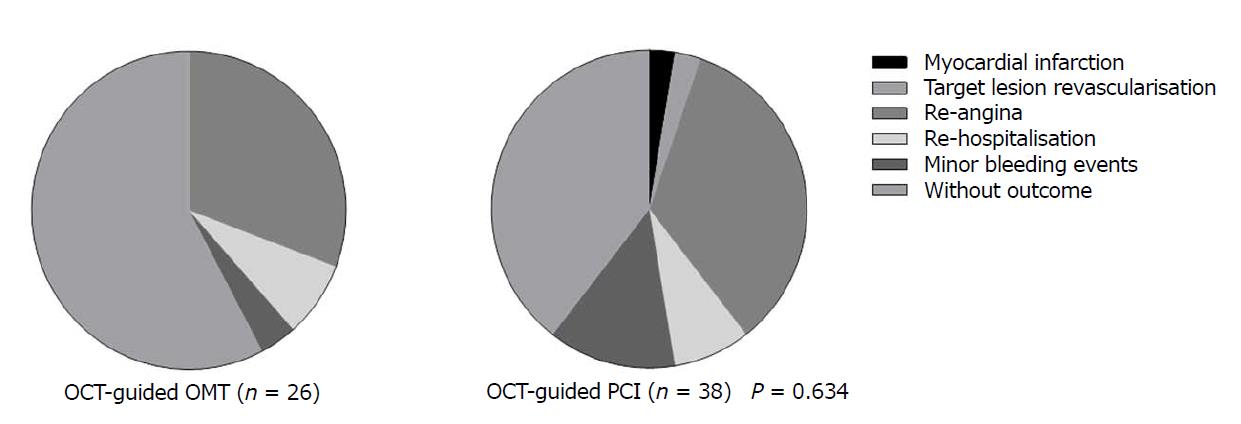
Follow-up was undertaken in person so as to achieve optimal subjective evaluation, after each of the 64 patients was telephonically informed of his/her follow-up date. None of the patients were lost to follow up. At 12 mo, no death, thrombosis, heart failure, cerebrovascular accidents and major bleeding events was observed in either group. Only 1 recurrent MI (2.6%) was noted in the OCT-guided PCI group that had no relation with the target vessel (Table 5), while none was recorded in the OCT-guided OMT group. With regards to the rates of target lesion revascularization, no significant difference (2.6% vs 0%) was noted between the 2 groups. Repeat episodes of angina was the only most frequent event observed, with 13 (34.2%) patients in the PCI arm reporting recurrent chest pain, compared to 8 (30.1%) patients in the OMT arm. The incidences of the remaining 2 secondary endpoints (repeat hospitalization and minor bleeding events) were also low and similar in both groups, making the overall comparison of safety clinical outcomes between the OCT-Guided PCI and OCT-Guided OMT groups not statistically significant (P = 0.634) (Figure 2).
| Variable | OCT-guided PCI (n = 38) | OCT-guided OMT (n = 26) | P-value, overall = 0.634 |
| Myocardial infarction | 1 (2.6) | 0 | 1 |
| Target lesion revascularisation | 1 (2.6) | 0 | 1 |
| Re-angina | 13 (34.2) | 8 (30.8) | 0.603 |
| Re-hospitalisation | 3 (7.9) | 2 (7.7) | 0.920 |
| Minor bleeding events | 5 (13.2) | 1 (3.8) | 0.427 |
The present study is the first to date to explore the safety and efficacy of FD-OCT in evaluating and guiding the treatment of patients with ICL. Several studies have analyzed the role of OCT in guiding PCI and evaluating post-PCI results. However, none has thus far investigated the efficacy and safety of OCT in the evaluation and optimal treatment of angiographically-borderline coronary artery lesions.
The statistically significant results demonstrated by our study as reported in Table 4 and Figure 1 prove that FD-OCT is superior to and more accurate than 2D-QCA in evaluating stenosis severity in ICL owing to its superior spatial resolution, thus meeting our primary efficacy end-point. FD-OCT provides a more accurate evaluation of stenosis severity in ICL, and hence positively influences physician decision-making regarding whether to proceed with PCI or to treat the lesion medically. In addition, other parameters such as % plaque burden and unstable plaque morphology can be clearly delineated and measured by FD-OCT, crucial in influencing physician decision-making in the setting of ICL. From our results of % mean AS by OCT in Table 3 (72.22% ± 7.39% in the PCI and 61.87 ± 7.51 in the OMT group), we may conclude that it is beneficial to proceed with OMT as opposed to PCI in any ICL with an average % AS of less than 62% on FD-OCT imaging, provided that plaque stability is not compromised and the plaque burden is ≤ 76%. These results also lead us to conclude that lesions with an average % AS greater than 72%, or demonstrating unstable plaque morphology features, or a plaque burden exceeding 76% are likely to benefit more from PCI than OMT. For ICL with a % AS between 62% and 72%, the decision whether to proceed with OMT or PCI should be taken on an individual basis, taking into account whether unstable plaque factors exist and the % of atherosclerotic plaque burden. To the best of our knowledge, the only study that compared 2D-QCA directly with OCT in the assessment of coronary artery lesion dimensions was conducted by Mazhar et al[9]. It showed there is a good correlation between QCA and OCT for measurement of proximal and distal reference diameters of a lesion, but the MLD was underestimated by QCA. The latter findings are in keeping with the results of our study. However, the aim of this study did not set its focus on the ICL subset of narrowings, but instead considered a whole range of coronary stenoses from moderate to severe.
The results of our study also demonstrate that the primary safety end-point (incidence of 30-d MACE) was fully met, with none of the 64 subjects experiencing any serious post-procedural adverse events such as cardiac death, post-procedure MI, acute stent thrombosis, significant vessel perforation or dissection, emergent revascularization, major vascular complications or cerebrovascular accidents. Therefore, major complications following intracoronary OCT study of ICL are highly unlikely, which can be minimized using a careful procedural scheme. Furthermore, no patients developed acute kidney injury during their in-hospital stay despite the additional amount of contrast media used during the FD-OCT procedure. However, these results evaluating safety end-points of the current study should be interpreted with appropriate caution, given the relatively small sample size. In addition, other safety end-points such as duration of the procedure, fluoroscopy time, amount of contrast media used, and radiation dose delivered were not formally evaluated by our study.
Evaluation of the secondary end-points showed that at 12 mo, up to one-third of patients in each group experienced recurrent episodes of chest pain, the most frequent event of the secondary end-points (Table 5). Whether repeat episodes of angina has any relation to the intervened or non-intervened ICL is a difficult question to answer, and therefore cannot be used on its own as a measure to evaluate success or failure of the FD-OCT procedure. Factors such as the patient’s subjective interpretation of angina, progression of disease, de novo coronary lesions, poor compliance to anti-platelet therapy are factors that could account for recurrence of angina episodes in these patients. However, with the exception of the relatively high incidence of repeat episodes of angina in both the OCT-guided PCI and OCT-guided OMT groups, incidence of the other secondary end-points such as MACE at 12 mo and other adverse clinical events during that time period were nil or similarly very low (Figure 2), leading to the comparison of safety clinical outcomes between the 2 groups being statistically not significant. This proves that FD-OCT is a safe technique as it did not itself contribute to a worse clinical outcome whether the patient was treated with PCI or OMT following intracoronary OCT imaging.
Further deductions can be made from the results of our study. 53 of the 64 patients (82.8%) presented with UA, only 7 (10.9%) patients presented with SA, while NSTEMI and STEMI presentations accounted for 2 patients each (6.2% combined) (Table 1). From these findings, it can be inferred that patients with ICL have a high likelihood of presenting with symptoms of UA and are at increased risk of acute coronary events. OCT thus presents as a crucial investigative tool to decide whether to treat the ICL in these patients interventionally or conservatively, depending on the OCT findings of % AS, plaque instability and % plaque burden. Out of the 53 patients who presented with UA, there was a significant difference between the percentage of subjects treated with PCI (64.1%) compared to OMT (35.9%), showing that OCT is determinant in guiding optimal therapy of the ICL found in this subset of ACS patients. With regards to the SA subgroup of 7 patients, 4 (57.1%) were treated with PCI, while the remaining 3 (42.9%) were managed medically; however, the number of patients comprising this subgroup was too small to draw any definitive conclusions.
On the other hand, only 4 (6.2%) patients in our study presented with either a STEMI or NSTEMI, all of whom were treated with OMT post-OCT. In this minority of patients, no indications were found to proceed with PCI based on the predetermined OCT criteria or, the pathological hallmark in these patients comprised the entity of myocardial infarction with non-obstructive coronary arteries (MINOCA)[10]. The small number of patients comprising this subgroup limits our ability to conclude whether OCT is safe and effective in the setting of an acute myocardial infarction (AMI). However, it does importantly demonstrate that patients with AMI not always require PCI, but can be managed conservatively should OCT demonstrate no features of plaque instability or no significant stenosis. These deductions can potentially be linked to the findings of the recently published landmark ORBITA trial[11]. The latter indicated that among SA patients with anatomically and functionally significant coronary stenoses (≥ 70% severity), PCI did not result in greater improvements in exercise times or anginal frequency compared with a placebo procedure, though it did resolve ischemia more effectively as ascertained by follow-up stress echocardiography, these findings requiring however to be validated in a larger randomized controlled trial. Even though the ORBITA trial did not involve the use of OCT as an imaging tool to evaluate the degree of stenosis on the coronary lesions and its aim was, in fact, to evaluate the efficacy of PCI compared with a placebo procedure for angina relief among patients with SA, it did however show that SA patients with severe coronary stenoses are not automatically candidates for PCI, as many of them can have an equally good outcome with OMT. In this setting, OCT can be of utmost value in guiding the interventionist to decide as to which of these patients will benefit more from PCI than OMT and vice-versa, based on accurate OCT assessment of stenosis severity, and other crucial parameters such as plaque instability and % of atherosclerotic plaque burden obtained from the OCT study.
Whether OCT is effective and safe in evaluating and treating ICL in patients presenting with an AMI, in whom emergency CAG shows no obstructive lesions, but instead borderline or even minimal coronary stenosis in accordance with the MINOCA entity, is an important issue. In the setting of an unstable patient with an AMI undergoing emergency CAG, the efficacy and safety of FD-OCT with regards to the optimal outcome for the patient is debatable. FD-OCT can be time-consuming in less experienced hands, requires additional instrumentation and increased doses of contrast agent and anticoagulants. On the other hand, it does provide vital information on plaque stability or instability of the ICL suspected to be the infarct-related lesion, crucial in aiding decision whether to proceed with PCI or OMT in the AMI setting. In their study on the OCT evaluation of intermediate coronary lesions in patients with NSTEMI, Bogale et al[12] showed that OCT imaging confirmed the lack of severe anatomical stenosis in most patients but also identified coronary lesions with unstable features. On the other hand, Takahashi et al[13] showed in their case report on an OCT-based diagnosis in a patient with STEMI and non-obstructive coronary arteries that OCT may provide a clue to identifying the underlying pathophysiological process especially in patients with MINOCA caused by coronary disorders. Another case report by Shah and Ing on the role of OCT in managing patients with STEMI demonstrated that OCT offers significantly improved resolution over IVUS, and hence should be used for assessment of the infarct-related lesion, especially in cases where the underlying pathophysiology is not clearly evident. The authors however pointed out that performing such an investigation requires additional vessel instrumentation and increased contrast use[14]. Both of these case reports and the clinical study by Bogale et al[12] did not shed any light though on how safe and effective OCT is in dealing with the ICL subset of lesions in a patient presenting with an AMI.
The only 3 efficacy clinical studies conducted so far on the OCT evaluation and treatment of patients with angiographically-borderline coronary lesions mostly focused on comparing OCT with FFR, but none investigated how effective OCT is as a stand-alone technique in dealing with ICL in the cardiac catheterization laboratory[15-17]. Furthermore, the OPUS-CLASS, CLI-OPCI and ILUMIEN I studies clearly show the advantages conferred by OCT in providing reliable quantitative measurements of coronary artery dimensions, improving clinical outcomes of patients undergoing PCI, and positively influencing both physician decision-making and procedural strategy pre and post-PCI respectively[18-20], while the ILUMIEN II, OPINION and CLI-OPCI II studies all investigated the efficacy of OCT in assessing stent deployment and expansion[21-23]. Despite highlighting the clinical and interventional benefits of OCT, none of these trials however explored the efficacy of this ultra-high resolution intracoronary imaging procedure in the ICL subset of stenosis alone.
On the other hand, whether the theoretical advantages of OCT also translate into safety benefits has been evaluated by only a limited number of clinical trials to date. A pioneering experience by Imola et al[24] on the safety of FD-OCT to guide decision making in PCI, showed OCT guidance to be safe. Furthermore, a multicenter study by Yoon et al[25] demonstrated that FD-OCT provides fast and reliable resolution images of the coronary artery, and the pullback can be safely performed over long segments of the artery without serious adverse events. The only 2 published randomised trials to have compared OCT-guided PCI with angiography-guided PCI (ILUMIEN III and DOCTORS) both showed that OCT-guided PCI was safe and did not increase peri-procedural complications[26,27]. Three other studies successfully demonstrated the safety and also the efficacy of intravascular OCT for coronary artery evaluation in the clinical setting, none of which however focused on the ICL subset of coronary narrowings[28-30]. So despite demonstrating intracoronary OCT to be a safe procedure, the question as to whether the above studies would have reached similar conclusions in dealing with ICL alone cannot be answered. Therefore, in our opinion, the present study is of significant value as it is the first one ever to investigate both the efficacy and safety of FD-OCT in evaluating and guiding the optimal treatment of patients with angiographically-borderline coronary artery lesions.
The present study has certain noteworthy limitations. First, it was a single-center study conducted over a 1 year period with a relatively sample size which was nevertheless reasonable considering the time duration of the study and the selection criteria of the patient population being studied. Because of the small sample size, the study lacked statistical power to determine whether the more accurate mean % AS measurement obtained by FD-OCT contrasted significantly with that obtained by 2D-QCA, even though a statistically significant difference was actually observed. In addition, as explained in the methodology section, no statistical sample-size calculation was undertaken in this study. Second, this was a non-randomized study as the subjects were assigned to either arm based on specific predetermined OCT criteria. Confounding and bias resulting from non-randomization could potentially affect the results of the study. In view of the favorable experience of this study, we intend to conduct a multi-center clinical trial which is registered in ClinicalTrials.gov (NCT03229993), with a larger sample size and a longer clinical study and follow-up time duration.
Our study clearly demonstrates that in evaluating and treating patients with angiographically-intermediate coronary lesions, OCT is a safe and effective ultra-high resolution imaging technique. It is superior to and more accurate than visual diagnostic CAG and 2D-QCA, hence allowing better evaluation and treatment of the ICL subset of coronary narrowings. In experienced hands, major procedural complications are rare, as are short to medium-term MACE. The data from our study warrant a large-scale randomized controlled trial to establish if OCT is equally safe and effective in the evaluation and treatment of ICL in patients presenting with the whole spectrum of ACS and SA, and whether proceeding with OCT imaging in these subjects does actually improve clinical outcomes in comparison with decisions based on angiographic guidance alone.
Conventional angiography and other adjunct coronary imaging techniques such as fractional flow reserve and intravascular ultrasound have in the past been used to evaluate the anatomical and physiological significance of coronary lesions considered to fall in the intermediate category (40%-70%). However, to this date, no study has been conducted to assess the safety and efficacy of frequency-domain optical coherence tomography (FD-OCT) in the evaluation and treatment of angiographically-intermediate coronary lesions (ICL). Our interventional team wanted to explore if FD-OCT could assist us in our daily practice to better evaluate and treat this subset of coronary lesions, compared to when angiographic-guidance alone is used to guide decision making in this clinical setting.
The current study addresses a very important topic in interventional cardiology, as it focuses specifically on the management of ICL. Cases of coronary lesions considered to be borderline are frequently under- or over-treated, hence providing a reliable tool for the accurate assessment of these lesions is of great importance to their appropriate management. Coronary angiography has several known limitations, including a lack of correlation between the percentage of stenosis and the lesion’s physiologic importance, and considerable inter-observer variability in classifying the lesion’s severity. On the other hand, percutaneous coronary intervention (PCI) has inherent risks even in the most experienced hands. The possibility of procedural complications with PCI such as coronary dissection, no reflow phenomenon, in-stent restenosis, and stent thrombosis requires accurate stratification of patients with intermediate coronary lesions to appropriate therapy. The present study explores the use of FD-OCT as an ultra-high resolution intracoronary imaging tool with regards to its safety and efficacy to accurately assess and manage intermediate coronary lesions interventionally or medically, and will spark interest for further research in this specific setting to reinforce the concept being explores.
Our aim in designing this study was to demonstrate that FD-OCT is a safe and effective procedure to be performed when faced with intermediate coronary artery lesions during coronary angiography in the cardiac catheterization laboratory. As this is the first study to investigate the safety and efficacy of OCT in the setting of ICL, it will pave the way for further studies (multi-center, larger sample size, longer follow-up times) to be conducted to confirm our findings, and reinforce our conclusions and recommendations. In particular, these studies are expected to have higher statistical power, with a larger sample size and a more equal representation of patients from the different coronary artery disease (CAD) population subgroups. This paper will provide investigators from across the world a platform to improve on the study design, methodology in conducting studies with similar objectives, taking into account the difficulties we encountered in this study, and the related limitations that ensued.
With the aim in mind of elucidating whether FD-OCT was safe and effective in treating ICL, we decided to conduct the study by including patients found to have borderline lesions on angiography in our cardiac catheterization laboratory, and who consented to the OCT procedure. Patients who presented with cardiogenic shock, acute stroke, renal dysfunction, left main stem ICL, and acute or chronic total occlusion coronary lesions were excluded from the study. Patients were assigned to either of the 2 arms of the study based on specific predetermined OCT criteria. Focusing importantly on the specific aim of our study, we clearly defined our primary efficacy endpoint (demonstration of the superiority and higher accuracy of FD-OCT compared to 2D-QCA in evaluating stenosis severity in patients with ICL), primary safety endpoint [incidence of 30-d major adverse cardiac events (MACE)] and secondary endpoints (MACE at 12 mo and other clinical events), and obtained the necessary 2D-QCA and FD-OCT measurements, as well as the follow-up statistical results on MACE and other clinical outcomes. These results generated enabled an in-depth discussion and appropriate conclusions to be made. We hope that the methodology and study design used in our study will be useful in assisting investigators to design further studies with similar objectives.
The primary efficacy endpoint of our study was fully met, with statistically significant results clearly demonstrating that 2D-QCA overestimates the stenosis severity of the ICL in both the OCT-guided PCI and OMT groups. Our primary safety endpoint was also fully met, with none of the patients in the study experiencing any MACE at 30 d post-procedure. Incidences of secondary endpoints were also found to be low in both arms, the only exception being the relatively high incidence of recurrent episodes of angina which was, however, very similar in the 2 groups. Analysis of the above results gives a clear insight into the superiority of FD-OCT compared to 2D-QCA in evaluating stenosis severity of ICL, and lays a foundation on which further studies to further reinforce this finding and implement its application in clinical practice in managing patients with angiographically-borderline lesions, owing to the efficacy of the FD-OCT in this setting. The findings of the present study also highlighted the safety of this intracoronary-imaging technique in the same setting. However, these results should be interpreted with appropriate caution, given the relatively small sample size of the study, which resulted in the study lacking statistical power. In addition, patients across the different CAD population subgroups are not equally represented in this study, especially patients presenting with an AMI. Further studies are required to address these limitations from our present study, so that the safety and efficacy of FD-OCT can be extrapolated to the management of ICL in patients presenting with different categories of CAD.
To this date, the efficacy and safety of FD-OCT when specifically faced with an ICL in the cardiac catheterization laboratory irrespective of the clinical presentation of the patient, was unknown. The present study provides significant insight into the topic and successfully meets the objectives laid out by its investigators. It shows that in evaluating and treating an ICL, performing FD-OCT following coronary angiography adds significant value to the assessment and management of that lesion, and is found to be a safe and effective procedure in this setting. However, further studies are required with larger sample size and higher statistical power to determine whether this statement can be applicable to patients with ICL across the different CAD population subgroups, and if OCT is equally safe and effective in treating ICL in patients presenting with an AMI, compared to those presenting with UA or SA. It is expected that this pioneering study sparks further interest amongst researchers in the field of CAD and amongst interventional cardiologists in practice to design and conduct large, multicenter clinical trials in order to obtain more reliable data that can be used to implement guidelines and positively change clinical practice, as well as provide direction for future research in this field and in the clinical setting of ICL.
This study shows that 2D-QCA leads to an overestimation of lesion severity in comparison to FD-OCT, which is a prerequisite for overtreatment. On the other hand, the results show that OCT-guided decision making seems to be safe. The population with intermediate coronary lesions is largely underrepresented across different randomized trials. Therefore, despite its relatively small sample size, this prospective single center interventional study adds a lot of important data to the topic and provides a good platform for future larger multicenter clinical trials to be conducted to further reinforce the utility of FD-OCT in evaluating and treating ICL with regards to its safety and efficacy in this specific clinical setting.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and Cardiovascular Systems
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Karatza AA, Traykov V, Vidal-Perez RC S- Editor: Wang XJ L- Editor: A E- Editor: Wu YXJ
| 1. | Bezerra HG, Costa MA, Guagliumi G, Rollins AM, Simon DI. Intracoronary optical coherence tomography: a comprehensive review clinical and research applications. JACC Cardiovasc Interv. 2009;2:1035-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 488] [Cited by in RCA: 467] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 2. | Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, Camici PG, Cerqueira MD, Chow BJW, Di Carli MF. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62:1639-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 430] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 3. | Fearon WF. Assessing intermediate coronary lesions: more than meets the eye. Circulation. 2013;128:2551-2553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Mintz GS. Clinical utility of intravascular imaging and physiology in coronary artery disease. J Am Coll Cardiol. 2014;64:207-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 101] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 5. | Bezerra HG. Intravascular OCT in PCI. American College of Cardiology 2013. Available from: https://www.acc.org/latest-in-cardiology/articles/2016/06/13/10/01/intravascular-oct-in-pci. |
| 6. | Lotfi A, Jeremias A, Fearon WF, Feldman MD, Mehran R, Messenger JC, Grines CL, Dean LS, Kern MJ, Klein LW; Society of Cardiovascular Angiography and Interventions. Expert consensus statement on the use of fractional flow reserve, intravascular ultrasound, and optical coherence tomography: a consensus statement of the Society of Cardiovascular Angiography and Interventions. Catheter Cardiovasc Interv. 2014;83:509-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 7. | Bezerra HG, Attizzani GF, Sirbu V, Musumeci G, Lortkipanidze N, Fujino Y, Wang W, Nakamura S, Erglis A, Guagliumi G. Optical coherence tomography versus intravascular ultrasound to evaluate coronary artery disease and percutaneous coronary intervention. JACC Cardiovasc Interv. 2013;6:228-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 114] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, Steg PG, Morel MA, Mauri L, Vranckx P. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115:2344-2351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4265] [Cited by in RCA: 4694] [Article Influence: 260.8] [Reference Citation Analysis (0)] |
| 9. | Mazhar J, Shaw E, Allahwala UK, Figtree GA, Bhindi R. Comparison of two dimensional quantitative coronary angiography (2D-QCA) with optical coherence tomography (OCT) in the assessment of coronary artery lesion dimensions. Int J Cardiol Heart Vasc. 2015;7:14-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Pasupathy S, Tavella R, Beltrame JF. Myocardial Infarction With Nonobstructive Coronary Arteries (MINOCA): The Past, Present, and Future Management. Circulation. 2017;135:1490-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 11. | Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, Davies J, Keeble T, Mielewczik M, Kaprielian R, Malik IS. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018;391:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 576] [Cited by in RCA: 718] [Article Influence: 102.6] [Reference Citation Analysis (0)] |
| 12. | Bogale N, Lempereur M, Sheikh I, Wood D, Saw J, Fung A. Optical coherence tomography (OCT) evaluation of intermediate coronary lesions in patients with NSTEMI. Cardiovasc Revasc Med. 2016;17:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Takahashi T, Okayama H, Matsuda K, Yamamoto T, Hosokawa S, Kosaki T, Kawamura G, Shigematsu T, Kinoshita M, Kawada Y. Optical coherence tomography-based diagnosis in a patient with ST-elevation myocardial infarction and no obstructive coronary arteries. Int J Cardiol. 2016;223:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Shah A, Ing DJ. Role of optical coherence tomography in managing patients with ST elevation myocardial infarction. Cardiovasc Revasc Med. 2017;18:136-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Burzotta F, Nerla R, Hill J, Paraggio L, Leone AM, Byrne J, Porto I, Niccoli G, Aurigemma C, Trani C. Correlation between frequency-domain optical coherence tomography and fractional flow reserve in angiographically-intermediate coronary lesions. Int J Cardiol. 2018;253:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Pawlowski T, Prati F, Kulawik T, Ficarra E, Bil J, Gil R. Optical coherence tomography criteria for defining functional severity of intermediate lesions: a comparative study with FFR. Int J Cardiovasc Imaging. 2013;29:1685-1691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Stefano GT, Bezerra HG, Attizzani G, Chamié D, Mehanna E, Yamamoto H, Costa MA. Utilization of frequency domain optical coherence tomography and fractional flow reserve to assess intermediate coronary artery stenoses: conciliating anatomic and physiologic information. Int J Cardiovasc Imaging. 2011;27:299-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Kubo T, Akasaka T, Shite J, Suzuki T, Uemura S, Yu B, Kozuma K, Kitabata H, Shinke T, Habara M. OCT compared with IVUS in a coronary lesion assessment: the OPUS-CLASS study. JACC Cardiovasc Imaging. 2013;6:1095-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 225] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 19. | Prati F, Di Vito L, Biondi-Zoccai G, Occhipinti M, La Manna A, Tamburino C, Burzotta F, Trani C, Porto I, Ramazzotti V. Angiography alone versus angiography plus optical coherence tomography to guide decision-making during percutaneous coronary intervention: the Centro per la Lotta contro l’Infarto-Optimisation of Percutaneous Coronary Intervention (CLI-OPCI) study. EuroIntervention. 2012;8:823-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 272] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 20. | Wijns W, Shite J, Jones MR, Lee SW, Price MJ, Fabbiocchi F, Barbato E, Akasaka T, Bezerra H, Holmes D. Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study. Eur Heart J. 2015;36:3346-3355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 194] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 21. | Maehara A, Ben-Yehuda O, Ali Z, Wijns W, Bezerra HG, Shite J, Généreux P, Nichols M, Jenkins P, Witzenbichler B. Comparison of Stent Expansion Guided by Optical Coherence Tomography Versus Intravascular Ultrasound: The ILUMIEN II Study (Observational Study of Optical Coherence Tomography [OCT] in Patients Undergoing Fractional Flow Reserve [FFR] and Percutaneous Coronary Intervention). JACC Cardiovasc Interv. 2015;8:1704-1714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 132] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 22. | Otake H, Kubo T, Takahashi H, Shinke T, Okamura T, Hibi K, Nakazawa G, Morino Y, Shite J, Fusazaki T. Optical Frequency Domain Imaging Versus Intravascular Ultrasound in Percutaneous Coronary Intervention (OPINION Trial): Results From the OPINION Imaging Study. JACC Cardiovasc Imaging. 2018;11:111-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 23. | Prati F, Romagnoli E, Burzotta F, Limbruno U, Gatto L, La Manna A, Versaci F, Marco V, Di Vito L, Imola F. Clinical Impact of OCT Findings During PCI: The CLI-OPCI II Study. JACC Cardiovasc Imaging. 2015;8:1297-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 266] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 24. | Imola F, Mallus MT, Ramazzotti V, Manzoli A, Pappalardo A, Di Giorgio A, Albertucci M, Prati F. Safety and feasibility of frequency domain optical coherence tomography to guide decision making in percutaneous coronary intervention. EuroIntervention. 2010;6:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Yoon JH, Di Vito L, Moses JW, Fearon WF, Yeung AC, Zhang S, Bezerra HG, Costa MA, Jang IK. Feasibility and safety of the second-generation, frequency domain optical coherence tomography (FD-OCT): a multicenter study. J Invasive Cardiol. 2012;24:206-209. [PubMed] |
| 26. | Ali ZA, Maehara A, Généreux P, Shlofmitz RA, Fabbiocchi F, Nazif TM, Guagliumi G, Meraj PM, Alfonso F, Samady H. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet. 2016;388:2618-2628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 488] [Article Influence: 54.2] [Reference Citation Analysis (0)] |
| 27. | Meneveau N, Souteyrand G, Motreff P, Caussin C, Amabile N, Ohlmann P, Morel O, Lefrançois Y, Descotes-Genon V, Silvain J. Optical Coherence Tomography to Optimize Results of Percutaneous Coronary Intervention in Patients with Non-ST-Elevation Acute Coronary Syndrome: Results of the Multicenter, Randomized DOCTORS Study (Does Optical Coherence Tomography Optimize Results of Stenting). Circulation. 2016;134:906-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 250] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 28. | Prati F, Cera M, Ramazzotti V, Imola F, Giudice R, Albertucci M. Safety and feasibility of a new non-occlusive technique for facilitated intracoronary optical coherence tomography (OCT) acquisition in various clinical and anatomical scenarios. EuroIntervention. 2007;3:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Yamaguchi T, Terashima M, Akasaka T, Hayashi T, Mizuno K, Muramatsu T, Nakamura M, Nakamura S, Saito S, Takano M. Safety and feasibility of an intravascular optical coherence tomography image wire system in the clinical setting. Am J Cardiol. 2008;101:562-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 114] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 30. | Lehtinen T, Nammas W, Airaksinen JK, Karjalainen PP. Feasibility and safety of frequency-domain optical coherence tomography for coronary artery evaluation: a single-center study. Int J Cardiovasc Imaging. 2013;29:997-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |