Published online Aug 27, 2014. doi: 10.4240/wjgs.v6.i8.160
Revised: May 18, 2014
Accepted: July 12, 2014
Published online: August 27, 2014
Processing time: 213 Days and 12.1 Hours
We describe an impressive and rare case of surgical emphysema after minimally invasive rectal surgery. This case reports on a patient who developed massive retroperitoneal, intraperitoneal and subcutaneous emphysema directly following a transanal endoscopic microsurgery (TEM) procedure for a rectal intramucosal carcinoma. Free intra-abdominal air after gastro-intestinal surgery can be a sign of a bowel perforation or anastomotic leakage. This is a serious complication often requiring immediate surgery. In our patient an abdominal computed tomography-scan with rectal contrast showed no signs of a rectal perforation. Therefore this emphysema was caused by the insufflation of CO2 gas in the rectum during the TEM-procedure. Conservative treatment resulted in an uneventful recovery. With the increasing usage of TEM for rectal lesions we expect this complication to occur more often. After ruling out a full thickness rectal wall perforation in patients with surgical emphysema following TEM, conservative treatment is the treatment of choice.
Core tip: Surgical emphysema after transanal endoscopic microsurgery (TEM) can be a sign of a rectal perforation. This report describes a patient with impressive retroperitoneal, intraperitoneal and subcutaneous emphysema directly following TEM without a full thickness rectal wall perforation. This is a rare complication after TEM in which conservative treatment resulted in an uneventful recovery.
- Citation: Simkens GA, Nienhuijs SW, Luyer MD, Hingh IH. Massive surgical emphysema following transanal endoscopic microsurgery. World J Gastrointest Surg 2014; 6(8): 160-163
- URL: https://www.wjgnet.com/1948-9366/full/v6/i8/160.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i8.160
Transanal endoscopic microsurgery (TEM) is a minimally invasive technique developed for the resection of rectal neoplasms. This technique was first described in the early 1980’s and was initially exclusively intended for benign adenomas[1]. By providing good stereoscopic views and allowing use of both hands, better exposure and more precise excision are achievable as compared to previously used techniques for local excision. With increasing experience, TEM is now considered safe and may also be offered for low-grade malignant rectal lesions without signs of lymphatic or systemic dissemination (T1-2, N0, M0)[2]. The major advantage of TEM is the significantly lower morbidity and mortality as compared to traditional treatment for malignant rectal lesions such as abdominoperineal resection and low anterior resection[2]. Furthermore, functional outcome is better since the sphincteric complex is preserved, the abdominal wall is spared and damage to autonomous pelvic nerves is absent. Postoperative complications are rare after TEM and include postoperative bleeding (1.7%-2.7%) and pelvic sepsis due to perforation (1%-2.7%). TEM associated mortality is low (0%-2%)[3]. In this case report, a rare and impressive complication after TEM is described being the occurrence of massive retroperitoneal, intraperitoneal and subcutaneous emphysema directly following a TEM-procedure.
A 60-year-old woman was referred to our hospital with changed bowel habits including frequent defecation and soiling. Her relevant medical history includes a uterus extirpation, alcohol abuse and smoking. On a colonoscopy several sessile polyps throughout the colon were discovered which could be removed endoscopically. Pathology reports showed that these were all tubulovillous adenomas without signs of malignancy. However, in the rectum also a large villous lesion measuring 5 cm in diameter was found, located approximately 8-10 cm from the anal verge. This lesion could not be removed endoscopically due to its size and appearance. Biopsies showed at least intramucosal carcinoma but additional computed tomography (CT)-scan of the abdomen, pelvic magnetic resonance imaging and rectal endo-echography did not show signs of invasive growth, pathologic lymph nodes or systemic metastases. The tumor was therefore staged as a cT1N0M0 rectal intramucosal carcinoma and the patient was referred for a TEM-procedure.
Prior to the surgical procedure antibiotic prophylaxis was given (Cefazolin 1000 mg and Metronidazole 1500 mg both once) and the tumor was visualised on the ventral side of the rectum using rectoscopy. The patient was placed in prone position, the extended TEM-tube (TEO 15 cm, Karl Storz, Germany) was inserted and a pneumorectum was applied by insufflation of CO2 at 6 L/min with a pressure limit of 12 mmHg using a Karl Storz insufflator. Using ultracision, the lesion was macroscopically radical removed. No rectal perforation into the peritoneal cavity was observed and the defect in the rectal wall was closed with a running suture. Duration of the procedure was 115 min. Pathological examination confirmed the diagnosis of a tubulovillous adenoma with the presence of intra-mucosal carcinoma and clear resection margins. Immediately after the procedure massive subcutaneous emphysema of the face, neck and body was noticed (Figure 1). Given the amount of emphysema in the face it was decided to keep the patient intubated and ventilated and transfer to the intensive care unit. Here, blood analysis revealed a slight leucocytosis (11.0 k/μL) and a C-reactive protein (CRP) level of < 6 mg/L. Chest X-ray showed subcutaneous emphysema of the thorax, signs of “free air” beneath the left diaphragm and a small pneumothorax of the right sinus (Figure 2). After a few hours emphysema in the face was dissolving and the patient was awake. She was then detubated and discharged from the intensive care unit. At this moment she did not experience any abdominal discomfort, systemic reaction or fever. Intravenous antibiotics (Metronidazole 500 mg, Cefuroxime 1500 mg, both 3 times daily for 3 d) were started empirically and the patient was kept hospitalized with solid diet until all subcutaneous air had resolved three days later.
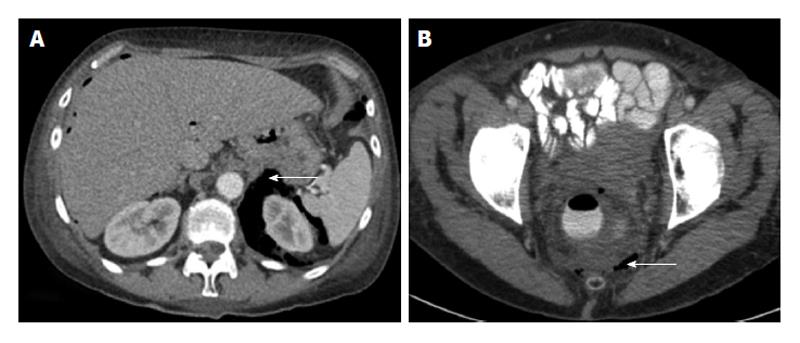
One day after discharge the patient visited the emergency ward with complaints of dyspnoea. Again, no abdominal discomfort or nausea were present, the patient had no fever and solid food was tolerated. However, blood analysis now showed an elevated CRP-level of 160 mg/L and based on the thoracic X-ray an increase in the amount of “free air” in the intra-abdominal space was suspected. Given the dyspnoea, “free abdominal air” and elevated inflammatory parameters a rectal perforation with leakage was suspected and an abdominal CT-scan with rectal contrast was performed. This revealed a large amount of air in the mesorectal fascia and especially in the retroperitoneal space and only a small amount of free air in the abdomen (Figure 3A). This retroperitoneal air had erroneously suggested the presence of free air in the abdomen. No signs of leakage from the rectal wound were found. In the lower thoracic field, pleural effusion and signs of a pneumonia were revealed (Figure 3B). This eventually explained for the dyspnoea and elevated inflammatory parameters. Conservative treatment with continuation of intravenous antibiotics was installed. In the following days, the dyspnoea disappeared and also, the retroperitoneal air disappeared on the thoracic X-ray. CRP and white blood count level normalised. On the tenth day she was discharged home in a good condition. Follow-up in our outpatient clinic did not show any abnormalities.
Free intraperitoneal air after gastro-intestinal surgery can be a sign of a bowel perforation or anastomotic leakage. These are serious and potentially life threatening complications often requiring immediate surgery and the formation of a (temporarily) diverting colostomy. Therefore, the possibility of a full-thickness defect of the rectal wall with communication to the peritoneal cavity should always be considered in patients with postoperative subcutaneous surgical emphysema and the suggestion of “free air” in the abdomen after a TEM-procedure. Close observation of body temperature, abdominal symptoms and blood infection parameters are helpful as well as an abdominal CT-scan with rectal contrast.
In the current case report subcutaneous emphysema and the suggestion of “free air” in the abdomen were suggestive of a persisting rectal wall perforation to the peritoneal cavity. However, no such defect in the rectal wall above the peritoneal fold was present and instead these features were most probably caused by insufflation of CO2 gas during the TEM-procedure. During this procedure, CO2 is insufflated under pressure into the rectum to create a pneumorectum. A full-thickness defect in the rectal wall is created on purpose during this procedure. Usually the mesorectal fat will seal the defect and prevent the CO2 from entering the body but in this case CO2“escaped” through the loose connective tissue into the retroperitoneal cavity and eventually subcutaneously. Subsequently, due to the elevated pressure in the retroperitoneal cavity and a decreased integrity of the retroperitoneal barrier CO2 gas was able to diffuse into the intraperitoneal cavity, as was also the case in our patient.
Surgical emphysema after a TEM-procedure has been previously described in 2 case reports describing 3 patients. Also in these patients no rectal perforation was present[4,5]. As in our case, conservative treatment in these cases resulted in an uneventful recovery. Thus, without clinical signs of a rectal perforation conservative treatment seems legitimate in patients with postoperative retroperitoneal and subcutaneous emphysema after a TEM-procedure.
In 2001 Kerr et al[6] described a case of a patient undergoing a TEM-procedure with intra-operative subcutaneous emphysema. Interestingly, this patient developed life-threatening hypercapnia in the early postoperative period. They hypothesize these complications were due to the insufflation of CO2 gas into the rectum. They conclude that a patient with arterial hypercapnia or surgical emphysema after TEM should be observed for a prolonged period in the recovery room with regular arterial carbon dioxide analysis.
Postoperative complications following TEM are rare and often mild, but life-threatening complications may occur. In this case-report an impressive but self-limiting complication occurred being massive subcutaneous and retroperitoneal emphysema. With the increasing usage of TEM for rectal lesions we expect this complication to occur more frequent. After ruling out a full-thickness perforation by an abdominal CT-scan with rectal contrast a conservative treatment may be followed.
Prolonged observation in the recovery room directly postoperative may be needed, especially in elderly patients to prevent or treat severe hypercapnia.
A 60-year-old woman with retroperitoneal, intraperitoneal and subcutaneous emphysema directly following a transanal endoscopic microsurgery (TEM)-procedure.
Subcutaneous emphysema of the head, neck and body without systemic or abdominal symptoms.
Rectal perforation or diffusion of gas during the procedure without a full thickness rectal wall defect.
White blood count: 11.0 k/μL; C-reactive protein-level: < 6 mg/L.
Abdominal computed tomography-scan with rectal contrast showed a large amount of air in the mesorectal fascia and especially in the retroperitoneal space and only a small amount of free air in the abdomen. No signs of leakage from the rectal wound were found.
cT1N0M0 rectal intramucosal carcinoma.
Conservative treatment with intravenous antibiotics.
Two reports previously described similar cases, with uneventful recovery after conservative treatment.
Free intra-abdominal air after TEM can occur without a full thickness rectal wall perforation and may be treated conservative.
Transanal endoscopic microsurgery is a minimally invasive technique developed for the resection of rectal neoplasms. This paper is very interesting case report of something observed not so rarely, even though not so evident.
P- Reviewer: Arezzo A, Agresta F, George V, Han X, Kita H S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
| 1. | Buess G, Hutterer F, Theiss J, Böbel M, Isselhard W, Pichlmaier H. [A system for a transanal endoscopic rectum operation]. Chirurg. 1984;55:677-680. [PubMed] |
| 2. | Léonard D, Remue C, Kartheuser A. The transanal endoscopic microsurgery procedure: standards and extended indications. Dig Dis. 2012;30 Suppl 2:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Bignell MB, Ramwell A, Evans JR, Dastur N, Simson JN. Complications of transanal endoscopic microsurgery (TEMS): a prospective audit. Colorectal Dis. 2010;12:e99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Cantos M, Bruna M, García-Coret MJ, Villalba FL, Roig JV. [Pneumomediastinum and subcutaneous emphysema like strange complications after transanal endoscopic microsurgery]. Rev Esp Enferm Dig. 2009;101:445-446. [PubMed] |
| 5. | Franken RJ, Moes DE, Acherman YI, Derksen EJ. Free Intra-Abdominal Air without Peritoneal Perforation after TEM: A Report of Two Cases. Case Rep Surg. 2012;2012:185429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Kerr K, Mills GH. Intra-operative and post-operative hypercapnia leading to delayed respiratory failure associated with transanal endoscopic microsurgery under general anaesthesia. Br J Anaesth. 2001;86:586-589. [PubMed] |