Published online Oct 27, 2011. doi: 10.4240/wjgs.v3.i10.156
Revised: September 21, 2011
Accepted: September 26, 2011
Published online: October 27, 2011
Degos’ disease, otherwise known as “malignant atrophic papulosis” is a rare vasculopathy with an unknown etiology characterized by typical cutaneous lesions. Involvement of the gastrointestinal (GI) tract is observed in approximately half of patients and small infarctions in the mucosa can cause perforation and resulting peritonitis, the leading cause of death. We present a fatal case of Degos’ disease with skin and GI involvement, manifesting as recurrent intestinal perforations and peritonitis, in a 15-year-old Iranian boy.
- Citation: Ahmadi M, Rafi SA, Faham Z, Azhough R, Rooy SB, Rahmani O. A fatal case of Degos’ disease which presented with recurrent intestinal perforation. World J Gastrointest Surg 2011; 3(10): 156-158
- URL: https://www.wjgnet.com/1948-9366/full/v3/i10/156.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i10.156
Degos’ disease, otherwise known as “malignant atrophic papulosis” is a rare vasculopathy with an unknown etiology characterized by typical cutaneous lesions. Its involvement of the gastrointestinal (GI) tract is usually associated with a poor prognosis[1]. It is a rare, progressive, small and medium size arterial occluding disease, leading to tissue infarction and involving the skin, GI tract and central nervous system, related to a thrombotic vasculopathy of unknown origin. Involvement of the latter two sites is often the cause of death[2,3]. Here, we present the case of Degos’ disease with skin and GI involvement, manifesting as recurrent intestinal perforation, in a 15-year-old Iranian boy.
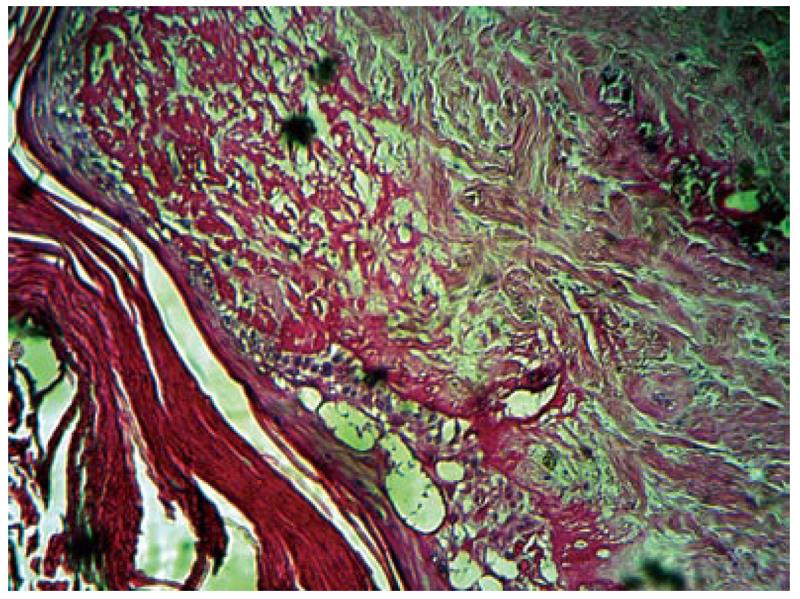
A 15-year-old Caucasian boy (Iranian) without any personal medical history, presented with more than 50 remittent eruptions of small papules with white centers surrounded by erythematous telangiectatic borders, 5-10 mm in diameter, nonpruritic and painless, which were widespread but located principally on the lower extremities and trunk that started 2 years ago without the complete disappearance of older ones. The soles, mucosae and face were not affected. After this period, he presented with acute abdominal signs, suggesting generalized peritonitis. Explorative laparotomy revealed two small bowel perforations in the ileum, 25 and 30 cm, proximal to the ileocecal valve. The perforated bowel segments were resected and an end-to-end anastomosis was performed, followed by irrigation and closure of abdominal wall. Broad spectrum antibiotics were started empirically. Microscopic examination showed acute severe serositis with intact mucosa and congestion and edema in all layers of the resected part. A second laparotomy was necessary on the 11th postoperative day because of acute abdominal signs due to new lenticular perforation which was detected 10cm proximal to the ileocecal valve which was resected and a double-barrel ileostomy was performed because of the abdominal cavity spillage. Despite 18 d of supportive care, the general condition of patient deteriorated. Abdominal CT scan showed multifocal fluid collections with a thickened wall, suggestive of multiple abscesses and prolonged peritonitis. On postoperative day 18, he underwent a third laparotomy because of two new perforations in the ascending colon and a right hemicolectomy was performed. In the three previous operations, we found a very abnormal texture of the intestine, probably due to an unknown underlying disease causing spontaneous perforations. Following an open discussion in an academic setting, the diagnosis of Degos’disease was proffered. So, we reviewed the literature and Degos’ disease was suggested as a probable diagnosis. To confirm this diagnosis, we took a biopsy from his chest skin lesion, which was reported as fat necrosis and hemorrhage in fatty lobules (panniculitis). Two weeks later, the histological examination of another skin biopsy from his leg lesion showed hyperkeratosis, atrophic epidermis, basal layer hydropic degeneration in the epidermis, on dermis collagen deposition and subendothelial sclerosis in the arterial wall in segmental foci is seen that caused ischemic infarct leading to atrophy of adnexal structures; which is compatible with Degos’ disease (Figure 1). We started Aspirin 325 mg and Dipyridamol 75 mg tablets daily based on recommendations in the literature but there were no considerable effects apart from mild improvement in his appetite. The complete blood count, serum biochemistry analysis, renal, hepatic and thyroid function tests were normal. The erythrocyte sedimentation rate, C-reactive protein, Wright and Coombs’ Wright tests were unremarkable. A brain CT scan was done because of a transient headache during his admission and this showed mild brain atrophy. Chest X-ray reported a mild right pleural effusion. After the third operation, his general condition continued to decline. He suffered an open abdomen, due to wound dehiscence and recurrent intestinal perforation, and severe malnutrition and died within 3 mo after admission.
Degos’ disease, also known as malignant atrophic papulosis (MAP), is a rare condition with reportedly stereotypical skin lesions on the trunk and proximal portion of the extremities, but the palms, soles and face tend to be spared, as in our case, consisting of largely asymptomatic, porcelain-white, atrophic papules, with surrounding erythema and telangiectasias. It has been alternatively regarded as an obliterating arteriolitis, necrotizing vasculitis, endovasculitis with secondary thrombosis, intravascular coagulation disorder or a disorder of fibrinolysis[4]. The exact nature of the disease remains controversial. Viral infection, autoimmune disease and coagulation defects have been proposed as underlying pathogenic mechanisms but none have been confirmed. Some believe that Degos’ disease is a thrombotic rather than an utoimmune disease. The disease is characterized by endothelial proliferation and swelling of small and medium-sized vessels. This progresses to luminal occlusion and eventual ischemia and infarction of the involved organ system. The internal organs most commonly involved in the order of decreasing frequency are the GI tract, CNS, thoracic organs and kidney. The eyes, cardiopulmonary system and hepatorenal system can also be involved in systemic MAP. Pulmonary features include pleuritis and bilateral effusion[5]. Intestinal perforation is the most severe complication and the bowel lesion may appear years after the cutaneous manifestation (similar to our case). Some published cases had a digestive manifestation before the onset of cutaneous involvement but the usual course is the opposite. The course of the disease may be as long as 20 years but once intestinal lesions have appeared, death usually occurs within a few months[6]. Although any portion of the intestinal system may be involved, the small bowel is predominantly affected[7]. In our case, we found two perforations in the ileum in the first and second operation and one in the ascending colon in the third operation. Generally when the CNS lesions are present, the intestinal lesions are absent or mild[8]. Our patient had no CNS findings, so based on our patient and literature review, we think that simultaneous severe involvement of the CNS and GI tract is very rare. Medical treatment for MAP, whether cutaneous or systemic, remains to be defined. Antiplatelet drugs (Aspirin, Dipyridamol) may have a role in the treatment of all variants of MAP, according to dramatic improvement in their general condition and disease symptoms shortly after treatment in some cases, suggesting that increased platelet aggregation may play a role in the pathogenesis of MAP[9]. Our patient was treated medically with Aspirin and Dipyridamol, improving his general condition mildly, confirming previous recommendations.
In conclusion, we reported a fatal case of Degos’ disease afflicting a 15-year-old Iranian boy. The onset of the disease was relatively earlier than those in previous reports but the disease progressed rapidly to systemic involvement, resulting in a poor prognosis. In our patient, the mild improvement in his general condition and disease symptoms shortly after treatment with antiplatelet drugs suggests that increased platelet aggregation may play a role in the pathogenesis of MAP but we think that it is ineffective or at most mildly effective after the presentation of GI involvement.
Peer reviewer: Yoshihiro Moriwaki, MD, PhD, Department of Critical Care and Emergency Center, Yokohama City University Medical Center, 4-57, Urafune-cho, Minami-ku, Yokohama 232-0024, Japan
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
| 1. | Kim DW, Kang SB, Lee KH, Choe GY, Park SY, Nicholay M. Degos' disease (malignant atrophic papulosis) as a fatal cause of acute abdomen: report of a case. Surg Today. 2008;38:866-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Atchabahian A, Laisné MJ, Riche F, Briard C, Nemeth J, Valleur P. Small bowel fistulae in Degos' disease: a case report and literature review. Am J Gastroenterol. 1996;91:2208-2211. [PubMed] |
| 3. | Torrelo A, Sevilla J, Mediero IG, Candelas D, Zambrano A. Malignant atrophic papulosis in an infant. Br J Dermatol. 2002;146:916-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | High WA, Aranda J, Patel SB, Cockerell CJ, Costner MI. Is Degos' disease a clinical and histological end point rather than a specific disease? J Am Acad Dermatol. 2004;50:895-899. [PubMed] |
| 5. | Fernández-Pérez ER, Grabscheid E, Scheinfeld NS. A case of systemic malignant atrophic papulosis (Köhlmeier-Degos' disease). J Natl Med Assoc. 2005;97:421-425. [PubMed] |
| 6. | Burg G, Vieluf D, Stolz W, Landthaler M, Braun-Falco O. [Malignant atrophic papulosis (Köhlmeier-Degos disease)]. Hautarzt. 1989;40:480-485. [PubMed] |
| 7. | Kocheril SV, Blaivas M, Appleton BE, McCune WJ, Ike RW. Degos' disease mimicking vasculitis. Arthritis Rheum. 2004;51:498-500. [PubMed] |
| 8. | Dastur DK, Singhal BS, Shroff HJ. CNS involvement in malignant atrophic papulosis (Kohlmeier-Degos disease): vasculopathy and coagulopathy. J Neurol Neurosurg Psychiatry. 1981;44:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Scheinfeld N. Malignant atrophic papulosis. Clin Exp Dermatol. 2007;32:483-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |