Published online Apr 27, 2025. doi: 10.4240/wjgs.v17.i4.102442
Revised: February 11, 2025
Accepted: March 7, 2025
Published online: April 27, 2025
Processing time: 79 Days and 23.5 Hours
Surgery is the first choice of treatment for patients with colorectal cancer. Tra
To investigate the short-term efficacy of laparoscopic radical surgery and traditional laparotomy for the treatment of colorectal cancer, and the differences in the risk analysis of unplanned reoperation after operation.
As the research subjects, this study selected 100 patients with colorectal cancer who received surgical treatment at the Yulin First Hospital from January 2018 to January 2022. Among them, 50 patients who underwent laparoscopic radical resection were selected as the research group and 50 patients who underwent traditional laparotomy were selected as the control group. Data pertaining to clinical indexes, gastrointestinal hormones, nutrition indexes, the levels of inflammatory factors, quality of life, Visual Analog Scale score, and the postoperative complications of the two groups of patients before and after treatment were collected, and the therapeutic effects in the two groups were analyzed and compared.
Compared with the control group, perioperative bleeding, peristalsis recovery time, and hospital stays were significantly shorter in the research group. After surgery, the levels of gastrin (GAS) and motilin (MTL) were decreased in both groups, and the fluctuation range of GAS and MTL observed in the research group was significantly lower than that recorded in the control group. The he
Laparoscopy was effective for colorectal surgery by reducing the occurrence of complications and inflammatory stress reaction; moreover, the quality of life of patients was significantly improved, which warrants further promotion.
Core Tip: With the advancement of medical technology, laparoscopic colorectal cancer surgery began to be widely used in the clinic. A retrospective analysis of patients with colorectal cancer suggests that, compared with traditional open surgery, laparoscopic surgery has advantages, such as a smaller incision, lower intraoperative blood loss, shorter hospital stays, and faster recovery. Concomitantly, laparoscopic surgery is less stimulating to the digestive tract of patients, has a definite effect, can reduce the occurrence of complications, reduces the inflammatory stress response, and significantly improves the quality of life of patients, which is worthy of further promotion and application.
- Citation: Li WB, Li J, Yu W, Gao JH. Short-term efficacy of laparoscopic radical resection for colorectal cancer and risk of unplanned reoperation after surgery. World J Gastrointest Surg 2025; 17(4): 102442
- URL: https://www.wjgnet.com/1948-9366/full/v17/i4/102442.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i4.102442
Colorectal cancer is one of the most common malignant tumors of the digestive tract in clinical settings. Most of these patients are male and the fatality rate is high. The morbidity and mortality of colorectal cancer rank in third and fourth place among all malignant tumors, respectively, thus seriously threatening human life and health[1,2]. Epidemiological studies have shown that the gradual change in the lifestyle and diet structure of populations caused by social development has led to an increasing incidence of colorectal cancer[3,4]. The factors that induce colorectal cancer, such as low intake of dietary fiber, excessive intake of animal fat, genetic factors, and social factors, are complex and diverse[5,6]. The first choice of treatment for patients with colorectal cancer is surgery. Traditional laparotomy for colorectal cancer has many advantages, such as a clear and open field of vision, flexible and convenient operation, and complete tumor resection. However, because of its great damage to the patient’s body, the immune system is seriously damaged, resulting in adverse stress reactions, causing great difficulties to the postoperative rehabilitation of patients[7-9]. With the development of clinical treatment methods, laparoscopic minimally invasive technology has begun to be widely used for the surgical treatment of patients with celiac disease[10]. Compared with laparotomy, laparoscopic colorectal cancer surgery can avoid the application limitations of traditional laparotomy, can minimize stress injury to patients, and has short-term advantages, such as a small incision, rapid recovery, and short hospital stays. Because it further shortens the rehabilitation process of patients, it has been widely used in the clinic[11-14]. To explore the application value of laparoscopic surgery and laparotomy in patients with colorectal cancer, this study collected the clinical data of 100 patients with colorectal cancer who were admitted to our hospital and performed a statistical analysis to compare the clinical effects of laparoscopic radical resection with those of laparotomy.
The data of patients with colorectal cancer who were admitted to the Yulin First Hospital from January 2018 to January 2022 were collected. A total of 100 patients were included in the study: (1) 50 patients who had undergone laparoscopic radical resection were included in the research group; and (2) 50 patients who had received traditional laparotomy were included in the control group.
Inclusion criteria: (1) All patients were diagnosed with colorectal cancer by color Doppler ultrasound or computed tomography before operation and pathological examination after operation; (2) All patients met the relevant diagnostic criteria for colorectal cancer included in the “clinical diagnosis and treatment guidelines·tumor subvolume”; (3) No obvious invasion and distal metastasis were found before and during operation; and (4) All patients were in accordance with the relevant indications of operation and there were no contraindications for laparotomy in the open group and no contraindications in the laparoscopic group.
Exclusion criteria: (1) Patients with a history of tumor-related radiotherapy and chemotherapy; (2) Patients with inflammation, ascites, or severe adhesion in the abdominal cavity; (3) Patients with psychiatric disorders; and (4) Patients with severe underlying diseases, major organ failure, other malignant tumors, or coagulation disorders.
The basic data of the two groups are reported in Table 1. There was no significant difference in gender composition, average age, tumor site, tumor diameter, and tumor stage between the two groups (P > 0.05).
| Control group (n = 50) | Research group (n = 50) | P value | |
| Gender (male/female) | 27/23 | 30/20 | 0.5445 |
| Age | 57.36 ± 8.02 | 58.76 ± 7.23 | 0.8333 |
| Tumor site | 0.7205 | ||
| Rectum | 12 | 15 | |
| Sigmoid colon | 28 | 25 | |
| Ascending colon | 5 | 7 | |
| Descending colon | 5 | 3 | |
| Tumor diameter | 2.51 ± 0.48 | 2.42 ± 0.56 | 0.8429 |
| TNM stage | 0.8462 | ||
| Stage I | 18 | 17 | |
| Stage II | 26 | 25 | |
| Stage III | 6 | 8 |
Patients in the research group underwent laparoscopic radical surgery, whereas the patients in the control group underwent traditional laparotomy. The patients in both groups were placed on a liquid diet 24 hours before the operation and paid attention to maintaining a nutritional balance. The patients were treated with antibiotics and compound polyethylene glycol electrolyte powder at 24 hours before the operation, started fasting at 8 hours before the operation, were then placed on drinking fasting at 4 hours before the operation, and performed bladder emptying before the operation.
The specific surgical methods used to perform the laparoscopic radical surgery were as follows: The patients were placed in a low-level lithotomy position and were administered general anesthesia. A small incision of 2–4 cm was made in the left lower abdomen, to establish a CO2 artificial pneumoperitoneum (the pneumoperitoneum pressure was maintained at 12–14 mmHg). The five-hole surgical path was selected for laparoscopy implantation in the patient, the lesion site and lymph node metastasis were confirmed with the assistance of laparoscopy, the length of the auxiliary incision was controlled within 5–6 cm, the primary lesion was removed under laparoscopy, the regional lymph nodes were cleared, etc.; finally, all incisions were sutured after the operation.
The specific surgical methods used to perform the traditional laparotomy were as follows: The patients were placed in a supine position and were administered general anesthesia. An incision with a length of 10–15 cm was made in the abdomen. The lesion was explored routinely, the specific surgical plan was selected according to the location and size of the tumor, the lesion was effectively separated from the surrounding tissue, and the incision was closely sutured after the operation.
The patients in the two groups were treated with routine fasting, gastrointestinal decompression, prevention and anti-infection, nutritional support, etc.
The clinical indexes, gastrointestinal hormones, nutrition indexes, levels of inflammatory factors, quality of life, Visual Analog Scale (VAS) score, and postoperative complications were statistically analyzed in the two groups before and after the treatment.
The clinically related indicators included time of operation, perioperative bleeding, number of lymph nodes cleared, recovery time of intestinal peristalsis, first exhaust time, and length of hospital stay.
The gastrointestinal hormones included gastrin (GAS) and motilin (MTL), and the nutritional indicators included albumin (Alb) and hemoglobin (Hb).
The inflammatory factors included the tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and C-reactive protein (CRP). Fasting venous blood was collected (3 mL) before and 3 days after the operation. After routine centrifugation, the level of inflammatory factors in the serum was assessed using an automatic enzyme-labeled instrument (Thermo, United States) combined with an enzyme-linked immunosorbent assay kit (Huamei Bio, China).
The incidences of infection (including infection of the incisional wound, pulmonary infection, and urinary system infection), anastomotic fistula, uroschesis, ileus, and thrombus of the lower-extremity veins were statistically compared between the two groups.
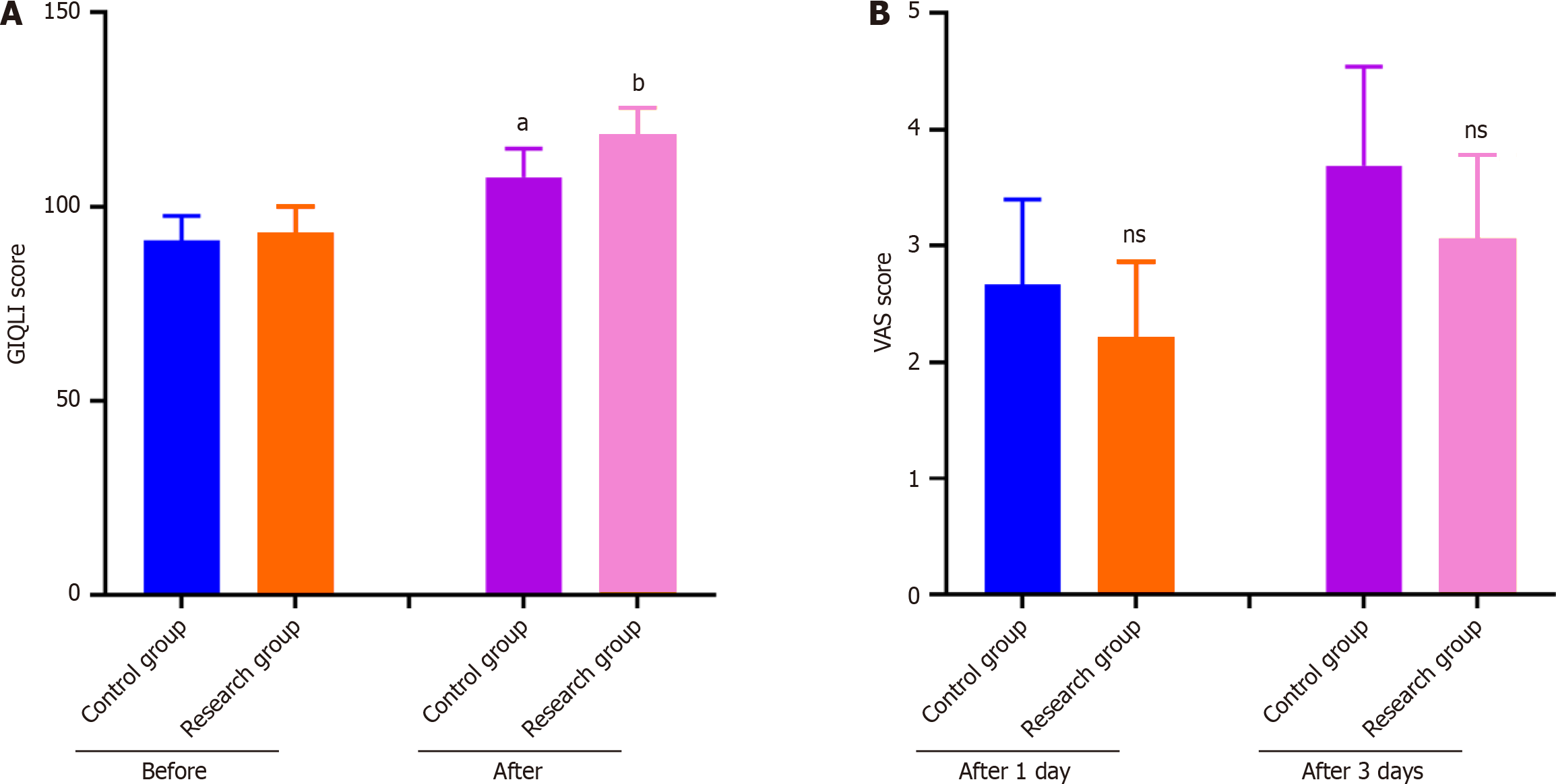
Before and after the operation, the quality of life of the two groups of patients was evaluated using the Gastrointestinal Quality of Life Index (GIQLI). The total score on the GIQLI is 144, and a higher score indicates a higher quality of life for patients. The VAS was used to evaluate the pain degree of the patients at 1 day and 3 days after the operation, with the score ranging from 0 to 10 and a higher indicating a greater pain severity.
The propensity score matching method was used to reduce the differences in the baseline data between the two groups. The matched covariates included gender, age, tumor site, tumor diameter, clinical TNM stage, preoperative GAS level, preoperative MTL level, preoperative Alb level, preoperative Hb level, preoperative inflammatory factor level, and preoperative GIQLI score.
In this study, Statistical Package for the Social Sciences 24.0 was used to perform the statistical analysis. The test of the normality of the measurement data was performed in advance. The data that met the normal distribution were expressed as the mean ± SD, and a t-test was used for inter-group comparisons; in turn, the data that did not meet the normal distribution were expressed as the median and quartile [M (P25, P75)], and the inter-group comparisons were carried out using the Shapiro–Wilks rank sum test. The χ2 test was used for the inter-group comparison of categorical variables, which were expressed as a percentage (%) or constituent ratio. Finally, the risk factors that exhibited statistical significance were analyzed using a multivariate binary logistic regression analysis.
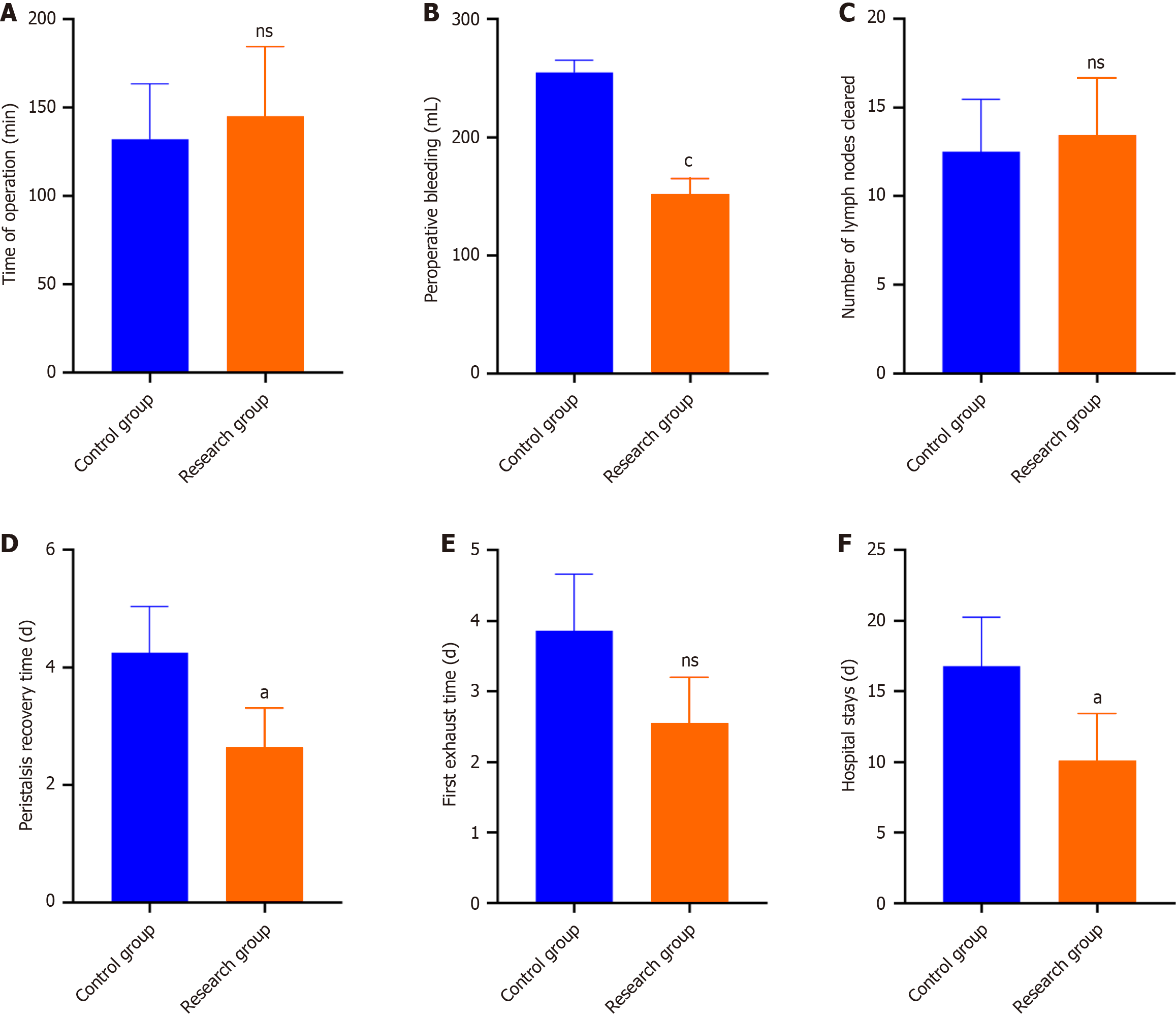
Compared with the control group, perioperative bleeding, the peristalsis recovery time, and hospital stays were significantly shorter in the research group (P < 0.05). In contrast, there was no significant difference in the time of operation, number of lymph nodes cleared, and first exhaust time between the two groups (P > 0.05) (Figure 1).
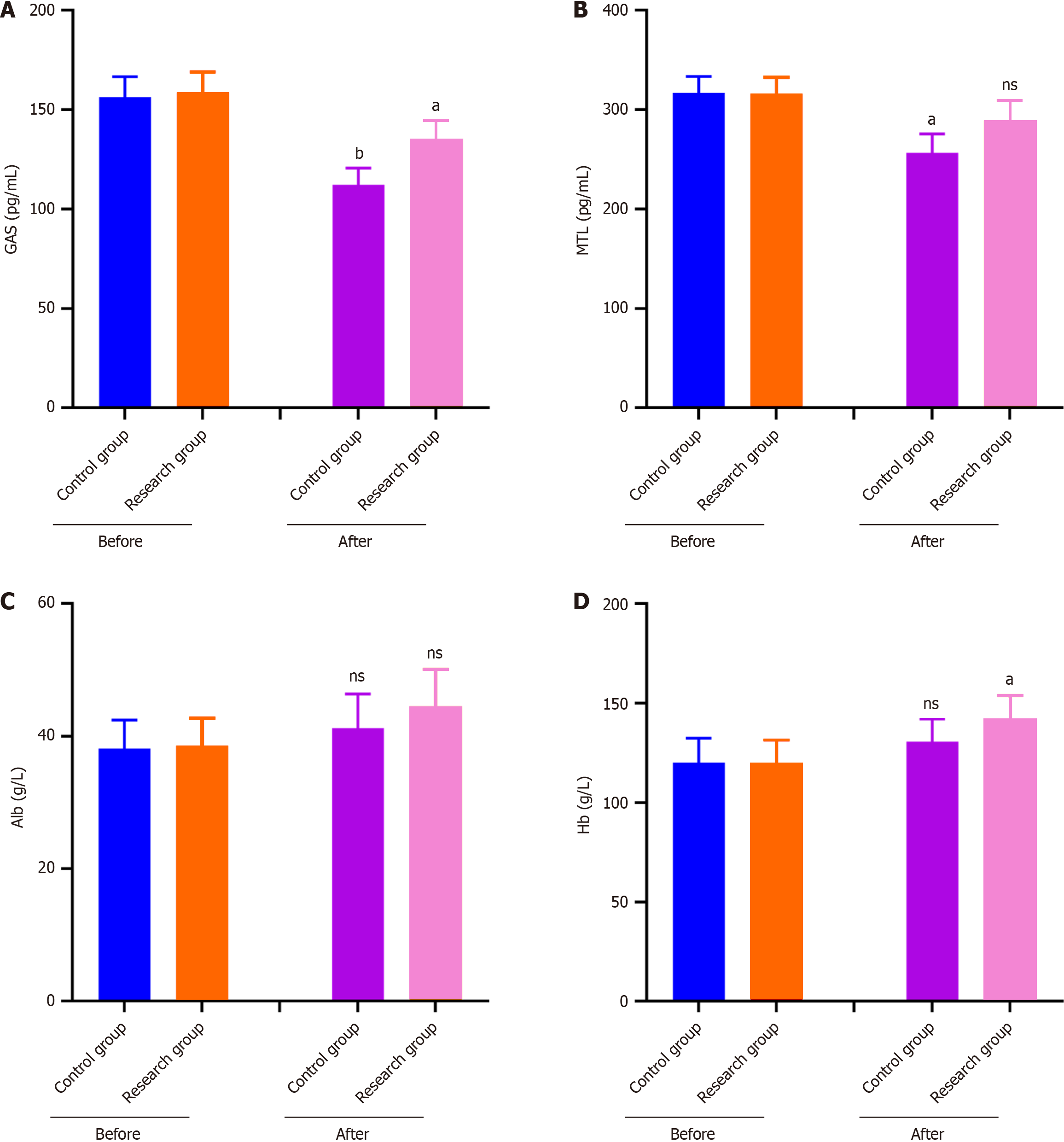
After the operation, the GAS and MTL levels were decreased in both groups, although the decrease in the GAS and MTL levels in the research group was smaller after the surgery (P < 0.05). The impact of laparoscopic radical surgery on the gastrointestinal tract was milder than that observed in the control group (Figure 2A and B). Conversely, the two treatment methods had no significant impact on the patients’ Alb levels (P > 0.05); in turn, the Hb levels of the patients in the research group were significantly increased after the surgery (P < 0.05), whereas there was no significant change in the control group (Figure 2C and D). The therapeutic effect of laparoscopic radical surgery was superior to that of the control group.
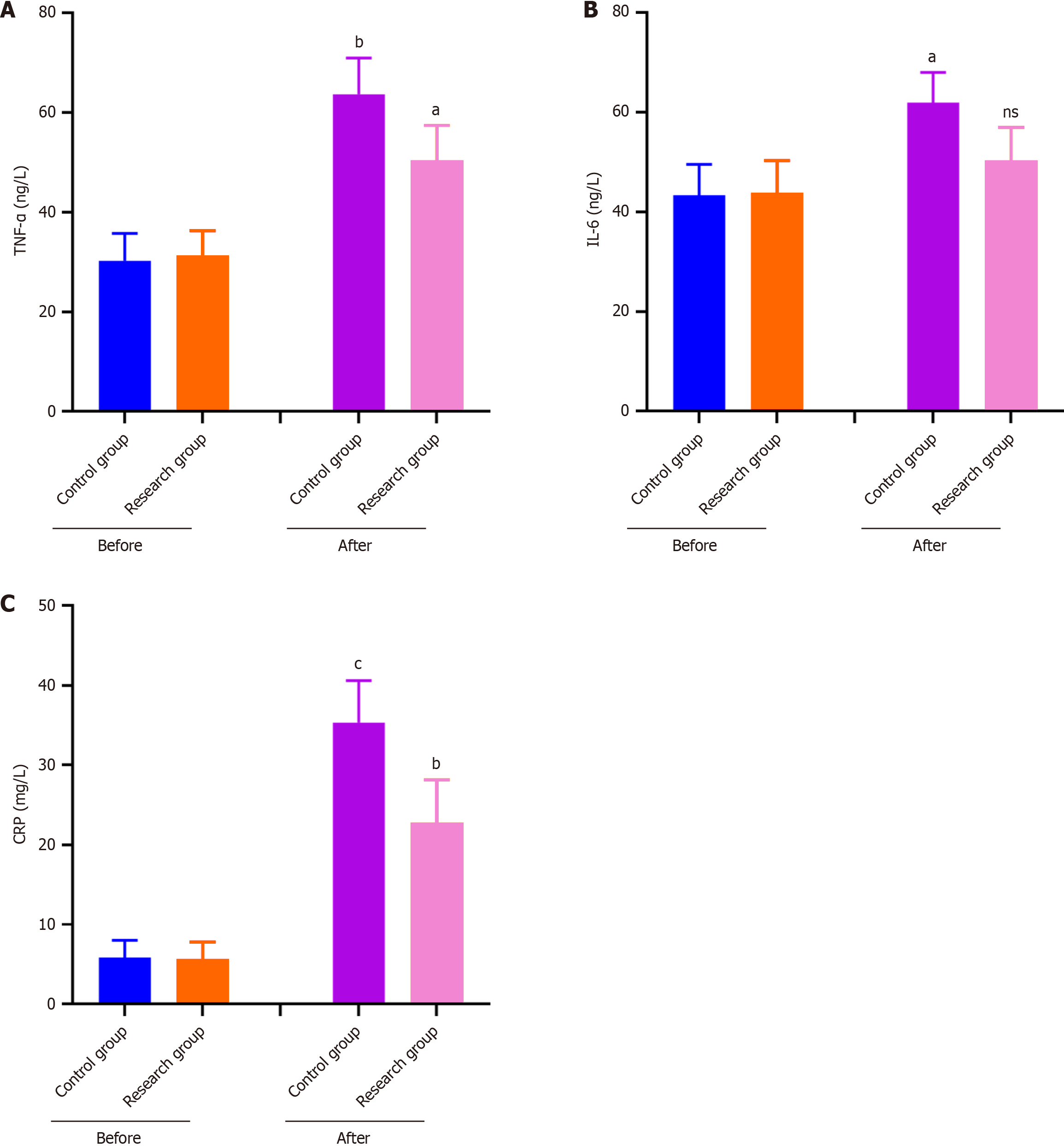
After the operation, the levels of inflammatory factors were significantly increased in both groups, although the levels of TNF-α, IL-6, and CRP were increased more significantly in the control group, with the differences between the two groups being statistically significant (P < 0.05) (Figure 3A–C).
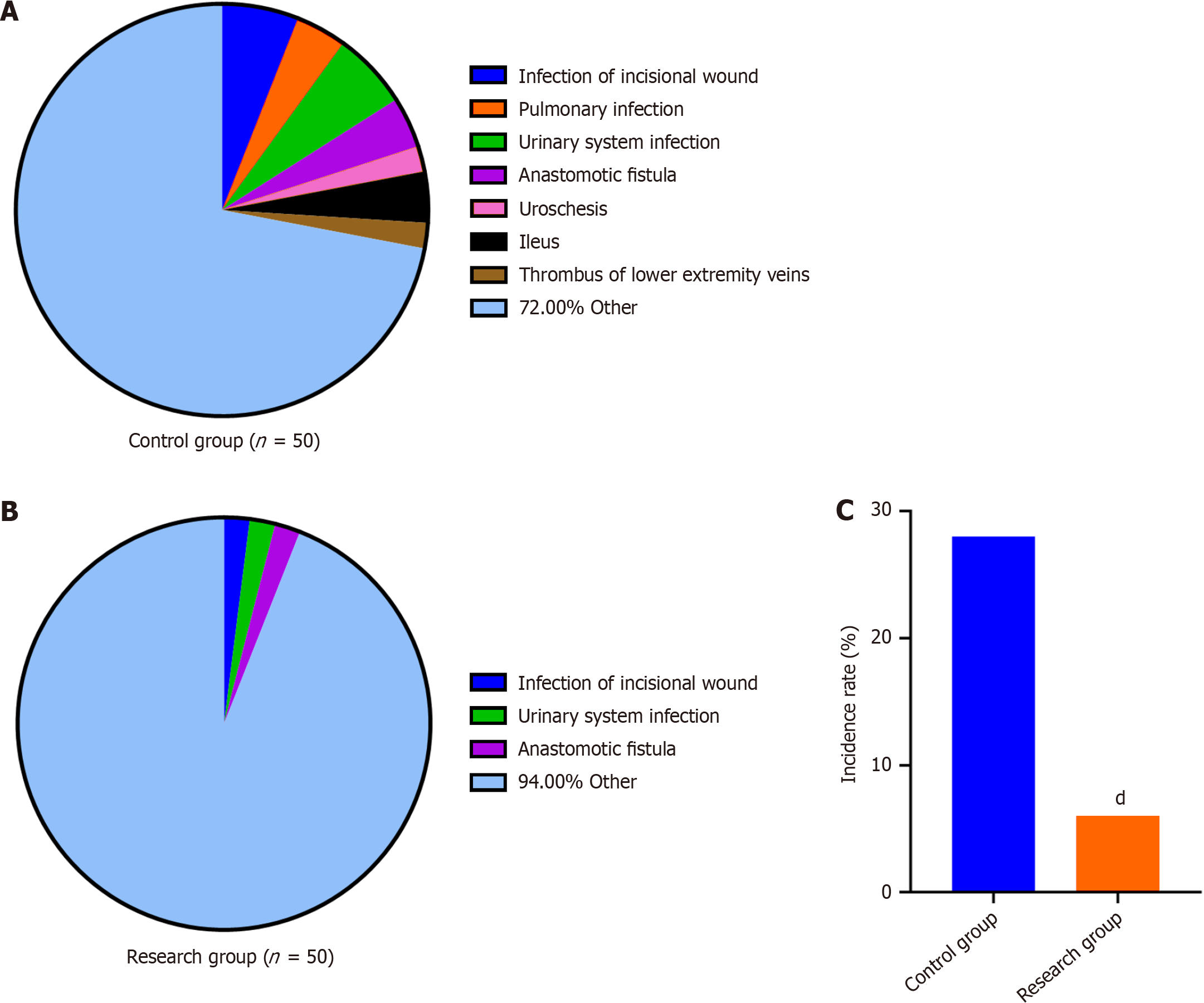
As shown in Figure 4A and B, several patients developed complications after the operation, such as wound infection, urinary system infection, and thrombus of the lower extremity veins. A total of 14 patients (28%) in the control group developed postoperative complications, and the total complication incidence was significantly higher than that detected in the research group (6%; P < 0.05) (Figure 4C).
The quality of life of the patients was greatly improved at 1 year after the operation, and the GIQLI score observed the research group was higher than that of the control group. The VAS score of the patients was slightly increased at 3 days after the surgery; however, the difference between the two groups was not significant (P > 0.05) (Figure 5).
Colorectal cancer occurs mostly in people aged 40–50 years and is mainly related to an irregular daily life and diet. The fatality rate of colorectal cancer is second only to that of lung cancer and liver cancer; thus, it brings great harm to the health of patients[15,16]. Currently, the gold-standard treatment for colorectal cancer is surgery, which mainly includes routine laparotomy and laparoscopic-assisted surgery; the latter is minimally invasive and highly recognized in clinical settings[17]. This study collected the clinical data of patients with colorectal cancer and analyzed the differences in short-term efficacy, long-term survival, and quality of life between laparoscopic radical surgery and traditional laparotomy. Compared with the control group, perioperative bleeding, the peristalsis recovery time, and the length of hospital stays were significantly shortened in the research group, which may be because the laparoscopic high-definition field of vision can clearly show the anatomical structure of the tumor foci, can ensure the effect of vascular root ligation and cutting, and will not produce operation traction on the intestinal tissue near the tumor, while ensuring the effect of lymph node clearance, reducing perioperative bleeding, and accelerating the recovery of intestinal function after operation[18,19]. Relevant clinical studies have also shown that compared with traditional laparotomy, laparoscopic radical surgery affords a shorter operation time, lower intraoperative blood loss, and shorter hospital stay[20]. This fully indicates that laparoscopic radical surgery can shorten the operation time, reduce the trauma to patients, and promote patient recovery after surgery.
Previous studies have pointed out that GSA and MTL are both gastrointestinal hormones and that their levels are closely related to gastrointestinal function in patients with abdominal surgery[21]. In this study, the postoperative GAS and MTL levels decreased to varying degrees in both groups, indicating that the stress response caused by the surgical treatment affected the secretion of digestive-tract hormones. However, the decrease in the GAS and MTL levels observed after surgery in the research group was more modest than that detected in the control group, whereas the Hb level in the research group was significantly higher than that in the control group. These results show that, compared with traditional laparotomy, laparoscopic surgery has a weaker effect on the secretion of GSA, MTL, and Hb. Therefore, laparoscopic surgery can help protect the gastrointestinal function of patients and is more beneficial to their postoperative recovery, because this procedure pulls the digestive tract of the patients to a lesser extent than does laparotomy; thus, it will not seriously affect the secretion of MTL and GAS. Moreover, it causes less stimulation to the nerves, blood vessels and intestines[22,23].
During the performance of abdominal surgery, and regardless of the surgical method that is selected, the organs and tissues in the abdominal cavity will be damaged to varying degrees, which may easily cause abnormal increases in the levels of inflammatory factors in the body, which, in severe cases, may lead to immune suppression[24]. TNF-α, CRP, and IL-6 are inflammation-related factors. Their levels can reflect the degree of the systemic inflammatory response in patients with colorectal cancer, and the effective control of the inflammatory response is key for the improvement of patient prognosis[25]. Here, the TNF-α, IL-6, and CRP levels in the research group were slightly increased after the operation, whereas the levels of inflammatory factors in the control group were increased more significantly. This indicates that laparoscopic surgery may minimize the damage to the patient’s immune system and the stress response to surgery[26]. Concomitantly, compared with traditional laparotomy, laparoscopic radical surgery had a lower incidence of postoperative complications and significantly improved the postoperative quality of life of the patients. It is suggested that laparoscopic radical surgery offers greater advantages regarding postoperative recovery and the reduction of the occurrence of adverse reactions.
In summary, compared with laparotomy, laparoscopic radical surgery for colorectal cancer can effectively reduce the risk of postoperative complications, reduce the inflammatory stress reaction of patients, and improve their quality of life after the operation, which is worthy of further application. However, this study was limited by its small sample size. Furthermore, this study only evaluated short-term prognostic indicators after surgery; therefore, the sample should be expanded through multiple channels to allow further long-term follow-up studies aimed at evaluating laparoscopic surgery regarding the long-term recovery of patients after surgery.
| 1. | Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1570] [Cited by in RCA: 3015] [Article Influence: 502.5] [Reference Citation Analysis (3)] |
| 2. | Baidoun F, Elshiwy K, Elkeraie Y, Merjaneh Z, Khoudari G, Sarmini MT, Gad M, Al-Husseini M, Saad A. Colorectal Cancer Epidemiology: Recent Trends and Impact on Outcomes. Curr Drug Targets. 2021;22:998-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 154] [Article Influence: 38.5] [Reference Citation Analysis (2)] |
| 3. | Patel SG, Karlitz JJ, Yen T, Lieu CH, Boland CR. The rising tide of early-onset colorectal cancer: a comprehensive review of epidemiology, clinical features, biology, risk factors, prevention, and early detection. Lancet Gastroenterol Hepatol. 2022;7:262-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 385] [Article Influence: 128.3] [Reference Citation Analysis (6)] |
| 4. | Zhou E, Rifkin S. Colorectal Cancer and Diet: Risk Versus Prevention, Is Diet an Intervention? Gastroenterol Clin North Am. 2021;50:101-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 5. | Kim J, Lee HK. Potential Role of the Gut Microbiome In Colorectal Cancer Progression. Front Immunol. 2021;12:807648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 111] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 6. | Siegel RL, Jakubowski CD, Fedewa SA, Davis A, Azad NS. Colorectal Cancer in the Young: Epidemiology, Prevention, Management. Am Soc Clin Oncol Educ Book. 2020;40:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 97] [Article Influence: 19.4] [Reference Citation Analysis (1)] |
| 7. | Devoto L, Celentano V, Cohen R, Khan J, Chand M. Colorectal cancer surgery in the very elderly patient: a systematic review of laparoscopic versus open colorectal resection. Int J Colorectal Dis. 2017;32:1237-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 8. | Gu J. [Resection margin of colorectal cancer surgery]. Zhonghua Wei Chang Wai Ke Za Zhi. 2022;25:36-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Hashida H, Mizuno R, Iwaki K, Kanbe H, Sumi T, Kawarabayashi T, Kondo M, Kobayashi H, Kaihara S. Laparoscopic Surgery for Colorectal Cancer in Super-Elderly Patients: A Single-Center Analysis. Surg Laparosc Endosc Percutan Tech. 2020;31:337-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Manning TG, Perera M, Christidis D, Kinnear N, McGrath S, O'Beirne R, Zotov P, Bolton D, Lawrentschuk N. Visual Occlusion During Minimally Invasive Surgery: A Contemporary Review of Methods to Reduce Laparoscopic and Robotic Lens Fogging and Other Sources of Optical Loss. J Endourol. 2017;31:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Sheng S, Zhao T, Wang X. Comparison of robot-assisted surgery, laparoscopic-assisted surgery, and open surgery for the treatment of colorectal cancer: A network meta-analysis. Medicine (Baltimore). 2018;97:e11817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Lai JH, Law WL. Laparoscopic surgery for colorectal cancer. Br Med Bull. 2012;104:61-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Martínez-Martínez AB, Arbonés-Mainar JM. Colorectal cancer: immune response in laparoscopic versus open colorectal surgery. Cir Cir. 2022;90:295-302. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Ustuner MA, Deniz A, Simsek A. Laparoscopic versus Open Surgery in Colorectal Cancer: Is Laparoscopy Safe Enough? J Coll Physicians Surg Pak. 2022;32:1170-1174. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Thanikachalam K, Khan G. Colorectal Cancer and Nutrition. Nutrients. 2019;11:164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 474] [Article Influence: 79.0] [Reference Citation Analysis (0)] |
| 16. | Li J, Ma X, Chakravarti D, Shalapour S, DePinho RA. Genetic and biological hallmarks of colorectal cancer. Genes Dev. 2021;35:787-820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 304] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 17. | Zeng WG, Zhou ZX. Mini-invasive surgery for colorectal cancer. Chin J Cancer. 2014;33:277-284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Bissolati M, Orsenigo E, Staudacher C. Minimally invasive approach to colorectal cancer: an evidence-based analysis. Updates Surg. 2016;68:37-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Drews G, Bohnsteen B, Knolle J, Gradhand E, Würl P. Laparoscopic surgery for colorectal cancer in an elderly population with high comorbidity: a single centre experience. Int J Colorectal Dis. 2022;37:1963-1973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Liu B, Yao C, Li H. Laparoscopic Radical Resection of Colorectal Cancer in the Treatment of Elderly Colorectal Cancer and Its Effect on Gastrointestinal Function. Front Surg. 2022;9:840461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Xi C, Wang X, Tian F. Effect of Shenqi millet porridge on gastrointestinal function decline. Int J Physiol Pathophysiol Pharmacol. 2023;15:50-55. [PubMed] |
| 22. | Sasaki M, Hirano Y, Yonezawa H, Shimamura S, Kataoka A, Fujii T, Okazaki N, Ishikawa S, Ishii T, Deguchi K, Sato H, Sakuramoto S, Okamoto K, Koyama I. Short-term results of robot-assisted colorectal cancer surgery using Senhance Digital Laparoscopy System. Asian J Endosc Surg. 2022;15:613-618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 23. | Zheng S, Zhao Z, Zheng H, Li J, Yang J, Zhao E. Safety analysis of natural orifice specimen extraction surgery for colorectal cancer. Medicine (Baltimore). 2022;101:e30087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 24. | Zhang B, Zheng L, Liang X, Liu L, Fu Y, Shi L. Short-term efficacy, safety and survival of laparoscopic radical resection for colorectal cancer patients with bowel obstruction. Med Eng Phys. 2022;107:103867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 25. | Florescu DN, Boldeanu MV, Șerban RE, Florescu LM, Serbanescu MS, Ionescu M, Streba L, Constantin C, Vere CC. Correlation of the Pro-Inflammatory Cytokines IL-1β, IL-6, and TNF-α, Inflammatory Markers, and Tumor Markers with the Diagnosis and Prognosis of Colorectal Cancer. Life (Basel). 2023;13:2261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 26. | Vacante M, Cristaldi E. Laparoscopic surgery for colorectal cancer: advantages and challenges. Updates Surg. 2016;68:421-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |