Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.103431
Revised: January 11, 2025
Accepted: January 21, 2025
Published online: March 27, 2025
Processing time: 94 Days and 20.3 Hours
This letter responds to Wang et al's recent publication on endoscopic biliary stenting for malignant obstructive jaundice (MOJ) by offering constructive feedback and suggestions for future research. We commend the authors for their comprehensive study design and execution, which included a clear delineation of study groups and a robust set of outcome measures. We suggest that future studies incorporate additional biomarkers, such as serum levels of liver enzymes and bilirubin, to provide a more nuanced understanding of liver function changes post-intervention. The study's focus on short-term survival rates is appreciated, but we recommend exploring longer-term follow-up periods to capture the full spectrum of survival outcomes. Additionally, the inclusion of quality of life assessments using validated instruments could offer a more holistic view of patient outcomes. From a critical care perspective, we advocate for the integration of advanced imaging techniques to better characterize biliary anatomy and potentially predict treatment response or complications. We believe that incor
Core Tip: The core tip of the manuscript is to evaluate the efficacy of endoscopic biliary stenting for malignant obstructive jaundice and compare it with the standard palliative approach, percutaneous transhepatic biliary drainage. The study suggests incorporating additional biomarkers for a nuanced understanding of liver function changes and emphasizes the importance of long-term follow-up to assess survival outcomes and the durability of palliative effects. It also highlights the need for quality of life assessments and advanced imaging techniques to predict treatment response and complications, contributing to a more holistic view of patient outcomes.
- Citation: Xie Y, Xie H, Wang RL. Enhancing palliative care in malignant obstructive jaundice: A critical care perspective on endoscopic biliary stenting. World J Gastrointest Surg 2025; 17(3): 103431
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/103431.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.103431
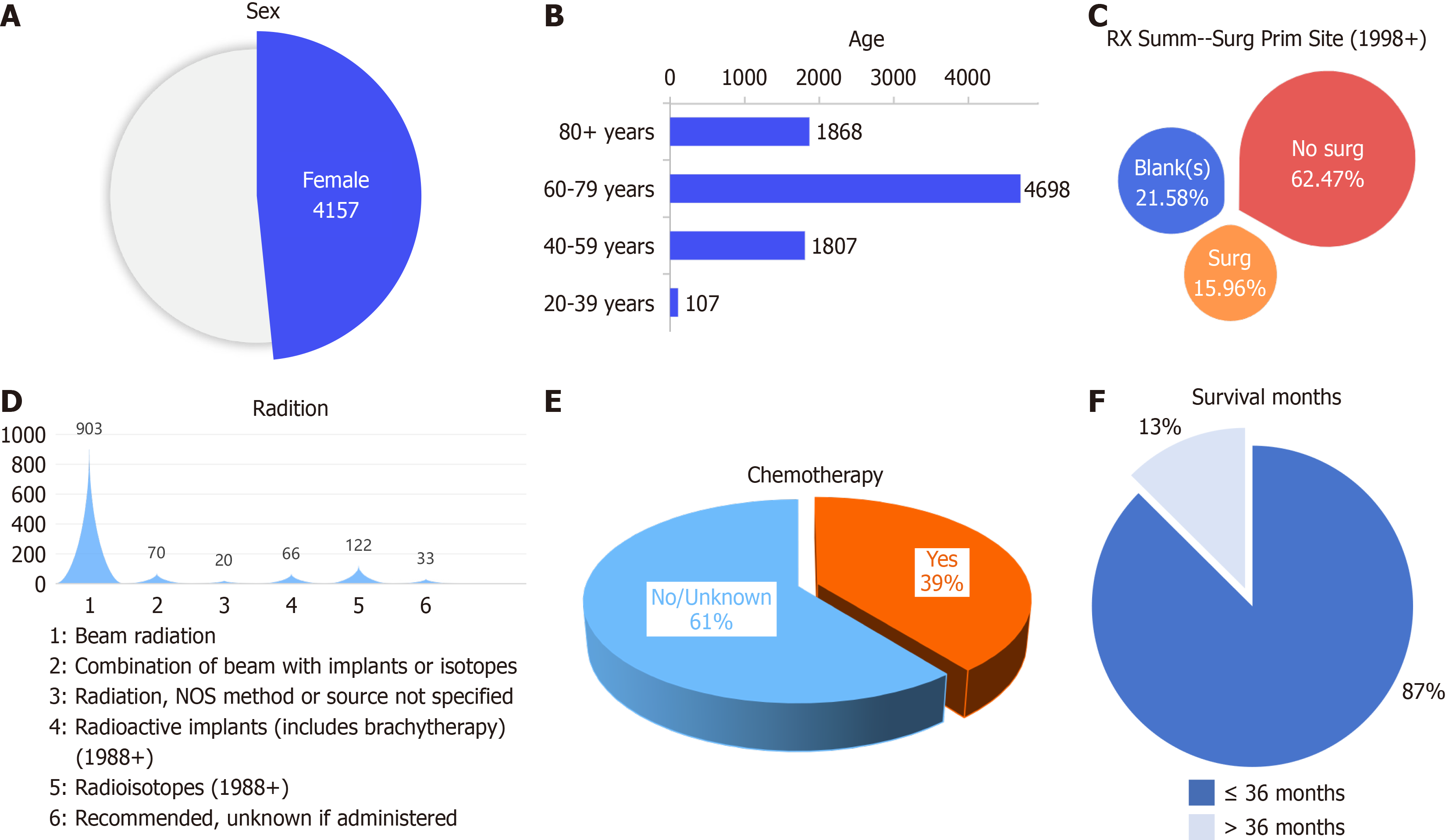
We recently read an interesting article titled "Clinical evaluation of endoscopic biliary stenting in treatment of malignant obstructive jaundice" by Wang et al[1], published in the World Journal of Gastrointestinal Surgery. This retrospective study provides valuable insights into the efficacy of endoscopic biliary stenting for treating malignant obstructive jaundice (MOJ) and offers a comparative analysis with percutaneous transhepatic biliary drainage (PTBD), a standard palliative approach. The most common causes of MOJ are pancreatic cancer and cholangiocarcinoma (primary cholangiocarcinoma or bile duct cell carcinoma). Let us take cholangiocarcinoma as an example. In the Surveillance, Epidemiology, and End Results (SEER) database, of 8584 cases of cholangiocarcinoma, 48.4% (n = 4157) were in women (Figure 1A), 54.7% (n = 4698) were in individuals aged 60-79 years (Figure 1B), 62.5% (n = 5362) were treated nonsurgically (Figure 1C), 15.9% (n = 1370) were treated surgically, 14.1% (n = 1214) were treated with radiotherapy (Figure 1D), of which beam radiation was the main treatment (n = 903), and 39% (n = 3374) were treated with chemotherapy (Figure 1E). Unfortunately, PTBD data were not recorded. We thank the authors for their thorough investigation and appreciate the potential implications for clinical practice in the management of MOJ. However, we would like to offer some constructive feedback and suggestions for future research on this topic.
First, the study was well designed and appropriately executed, with a clear delineation of the study groups and a comprehensive set of outcome measures. The use of liver function indices to assess the impact of interventions is a robust methodological choice. However, we suggest that future studies might benefit from incorporating additional biomarkers, such as serum levels of liver enzymes and bilirubin, to provide a more nuanced understanding of post-intervention changes in liver function[2].
Second, while the study provides a comparison of 3-year survival rates, a lack of statistical significance between the groups is noted. Our study revealed that 13% of cholangiocarcinoma patients in the SEER database survived for more than three years (Figure 1F). Future studies should include longer-term follow-up periods to capture the full spectrum of survival outcomes and to better understand the durability of the palliative effects of endoscopic biliary stenting.
Third, the study's focus on complications and adverse events is crucial, given the palliative nature of the treatment. However, the inclusion of quality of life assessments, using validated instruments such as the EQ-5D or the Liverpool-Pediatric Quality of Life, could offer a more holistic view of patient outcomes and the impact of the treatment on daily functioning and well-being. From a critical care perspective, Endoscopic biliary stenting effectively alleviates cholangial injury and obstruction in the palliative treatment of MOJ, reducing the incidence of acute suppurative obstructive cholangitis and thereby lowering the risk of infections and complications in the intensive care unit. By relieving biliary obstruction and mitigating or eliminating jaundice, this procedure improves patients' overall condition, decreasing the likelihood of common critical care issues such as electrolyte and acid-base imbalances caused by biliary obstruction, and providing a more stable physiological state. Postoperative care for endoscopic biliary stenting is crucial in the intensive care setting, with medical staff needing to closely monitor patients' vital signs and drainage status, promptly addressing potential complications like stent blockage or displacement to ensure patient safety and treatment efficacy. We also suggest that future research should consider the integration of advanced imaging techniques, such as cross-sectional imaging or cholangiography[3], to better characterize the biliary anatomy and potentially predict the response to treatment or the risk of complications.
There are several areas that could benefit from further expansion or clarification: (1) Discussion on other treatment modalities: The review could benefit from a brief mention of alternative palliative treatments for MOJ, such as newer stent technologies or intrahepatic biliary drainage. This would provide a broader view of the available therapeutic options and their potential advantages over endoscopic biliary stenting; (2) Statistical analysis: It would be helpful to include a more detailed critique of the statistical methods used in the original study, particularly in regard to survival analysis. Discussing specific statistical tests or models, such as Kaplan-Meier survival curves or Cox regression, would further enrich the review; and (3) Personalized treatment approaches: A mention of how patient-specific factors (e.g., cancer stage, comorbidities, age) could influence the choice of palliative treatment might add depth to the review. Personalization is a growing focus in medicine, and this aspect could be particularly relevant in the context of managing MOJ.
In conclusion, the study by Wang et al[1] contributes significantly to the body of knowledge on palliative care options for MOJ. We believe that the incorporation of our suggestions could further enhance the understanding of the role of endoscopic biliary stenting in the management of MOJ and its impact on patient outcomes. We look forward to witnessing how this research evolves and how it might influence clinical guidelines and practice.
| 1. | Wang W, Zhang C, Li B, Yuan G, Zeng Z. Clinical evaluation of endoscopic biliary stenting in treatment of malignant obstructive jaundice. World J Gastrointest Surg. 2025;17:97596. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 2. | An J, Dong Y, Li Y, Han X, Sha J, Zou Z, Niu H. Retrospective analysis of T-lymphocyte subsets and cytokines in malignant obstructive jaundice before and after external and internal biliary drainage. J Int Med Res. 2021;49:300060520970741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Cai Y, Fan Z, Yang G, Zhao D, Shan L, Lin S, Zhang W, Liu R. Analysis of the efficacy of Percutaneous Transhepatic Cholangiography Drainage (PTCD) and Endoscopic Retrograde Cholangiopancreatography (ERCP) in the treatment of Malignant Obstructive Jaundice (MOJ) in palliative drainage and preoperative biliary drainage: a single-center retrospective study. BMC Surg. 2024;24:307. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |