Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.100631
Revised: November 22, 2024
Accepted: December 17, 2024
Published online: February 27, 2025
Processing time: 153 Days and 19.3 Hours
Crohn's disease (CD) frequently leads to intestinal strictures, which pose sig
To investigate the safety and efficacy of stricturotomy under single-balloon enteroscopy in stricturing CD.
Patients diagnosed with stricturing CD at The First People's Hospital of Changzhou from June 2020 to April 2024 were enrolled and underwent en
Seventeen endoscopic strictures were created in 11 patients, achieving a 100% immediate success rate without any serious complications. During the follow-up period, stricture recurrence was observed in two patients, resulting in an endo
ES is a safe and effective treatment for CD-related strictures and warrants further clinical promotion and application.
Core Tip: This study evaluated the efficacy and safety of endoscopic stricturotomy (ES) for treating stricturing Crohn's disease in 11 patients. ES achieved a 100% immediate success rate with no significant complications. During follow-up, symptom relief was maintained for a median of 10 months, and the need for surgical intervention was reduced. ES was particularly effective for short-segment, solitary strictures and provided precise, minimally invasive treatment. These findings suggest ES is a viable alternative to surgery, which improves patient outcomes and delays recurrence or progression. Further research with larger sample sizes and multicenter studies is needed to validate these results.
- Citation: Cui L, Su M, Ding YB, Wang M, Sun KW. Preliminary study on the clinical value of endoscopic stricturotomy in the treatment of stricturing Crohn's disease. World J Gastrointest Surg 2025; 17(2): 100631
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/100631.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.100631
Crohn's disease (CD) is a chronic inflammatory granulomatous disease that affects the entire gastrointestinal tract. During its natural course, it often progresses into strictures. Intestinal strictures are very common in patients with CD; however, they are quite complex and difficult to cure. CD-related strictures are classified as inflammatory, fibrous, or mixed, with mixed strictures being the most common[1]. Currently, no medication has been proven to have a definite antifibrotic effect. Medications, including immunosuppressants and biologics, can improve inflammatory strictures. However, it is difficult to significantly improve fibrous and mixed strictures using medical treatments. Once bowel obstruction occurs, surgical intervention is typically required[2]. Surgical procedures carry high risks and are associated with numerous complications, including bleeding, infection, anastomotic leaks, short bowel syndrome, and postoperative restricture formation[3]. Endoscopic treatment is considered a bridge between medication therapy and surgical interventions. This approach includes endoscopic balloon dilation (EBD), endoscopic stricturotomy (ES), and stent placement. This study aimed to evaluate the efficacy and safety of ES under enteroscopic guidance for the treatment of stricturing CD.
This retrospective study included eleven patients diagnosed with stricturing CD and admitted between June 2020 and April 2024 in The First People's Hospital of Changzhou. All participants signed informed consent forms that outlined the potential risks and benefits of endoscopic treatment.
This study was approved by the Ethics Committee of The First People’s Hospital of Changzhou. Although this retrospective study collected and analyzed existing data, we ensured ethical principles were followed in the research process and protected the privacy and rights of the subjects.
Inclusion criteria: (1) Confirmed diagnosis; (2) Obstructive symptoms, including recurrent abdominal bloating, abdominal pain, and vomiting, occurring more than three times per year; and (3) Definite intestinal stenosis confirmed using abdominal imaging [computed tomography enterography (CTE), or magnetic resonance enterography (MRE)], with proximal dilatation or the inability of a single-balloon enteroscope to pass smoothly through the stenotic site.
Exclusion criteria: (1) Unconfirmed diagnosis; (2) Inflammatory strictures; (3) Malignant strictures; (4) Long-segment strictures (≥ 4 cm) or strictures with deep ulcers; (5) Missing follow-up data; and (6) Body mass index < 18.
Prior to the procedure, preoperative preparations were performed, including routine complete blood tests, coagulation function tests, liver and kidney function tests, electrocardiography, and CTE/MRE. Based on the results of the imaging examinations, the location, length, and number of strictures were evaluated to determine the method of endoscopic entry and treatment. Prior to the procedure, patients who underwent oral enteroscopy were fasted for 8-12 hours and abstained from water for 4-6 hours before the procedure, while patients who underwent transanal enteroscopy were administered a polyethylene glycol electrolyte solution for bowel preparation.
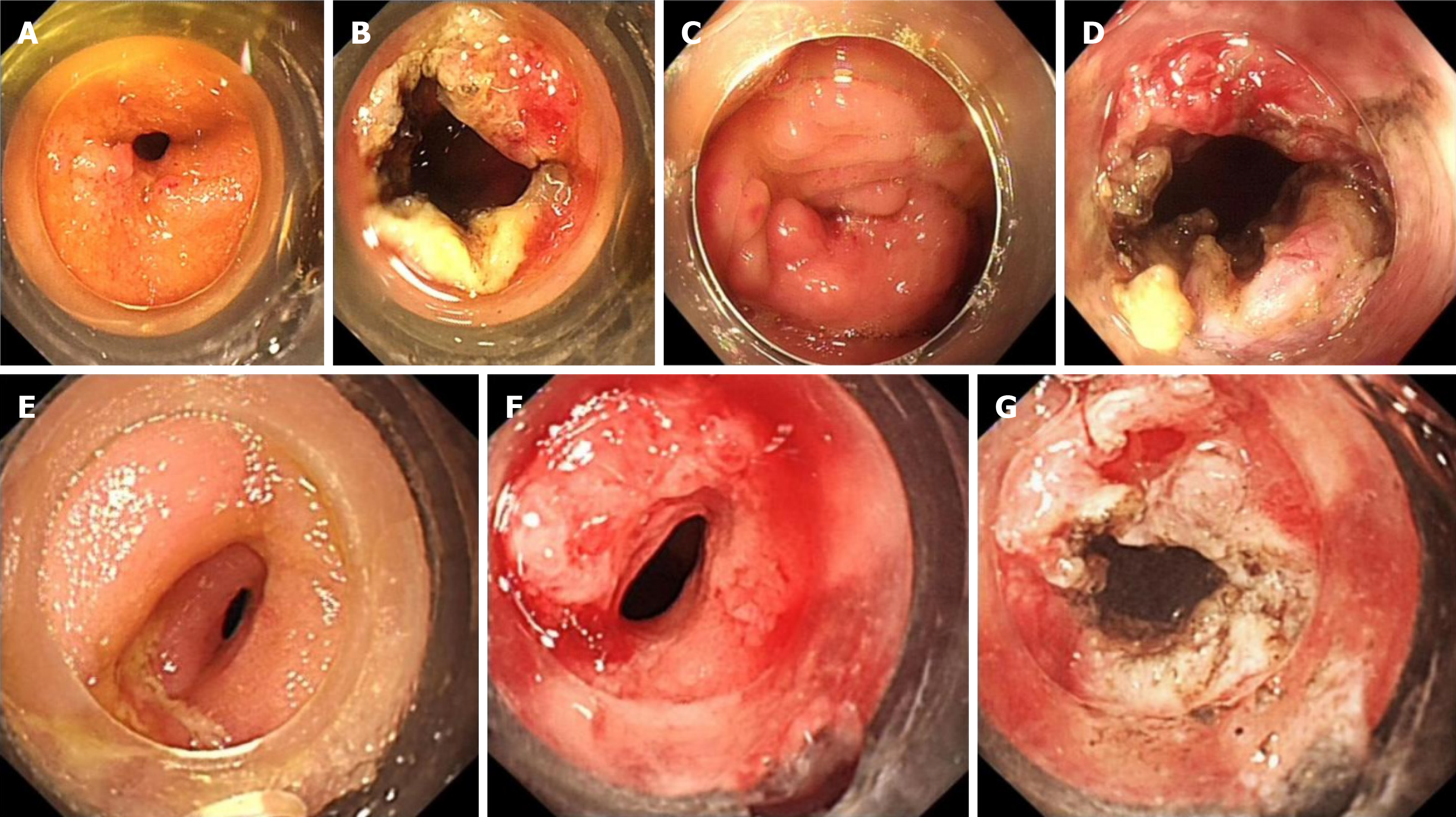
An oral or anal examination was selected according to the patient's specific condition, and both sides were examined where necessary. Oral enteroscopy requires endotracheal intubation anesthesia, while anal enteroscopy only requires intravenous anesthesia. The patients were placed in the left lateral decubitus position, and a single-balloon enteroscope (SIF-Q260, Olympus) was inserted orally or anally for comprehensive and meticulous observation of the small intestine. When a stricture lesion was identified, an IT knife (KD-611 L; Olympus) was inserted through the forceps channel, and radial incisions were made at the stricture site from shallow to deep under direct visualization. During the procedure, we took the following precautions: Avoided overinflation, controlled the depth of the incision, preserved as much of the muscle layer as possible, and examined the incision site for postoperative bleeding and perforation.
Other relevant information was obtained via telephone and outpatient follow-ups. Researchers were trained to understand the trial protocol, and they performed regular monitoring and review to ensure that the study process was compliant. Stricturotomy was performed by the same senior chief physician to reduce differences in outcomes.
Immediate success: Successful incision of the stricture lesion, allowing the enteroscope to pass smoothly through the stricture lesion to the distal or proximal intestinal segments.
Remission time: The time elapsed after the initial ES treatment without the need for further endoscopic or surgical treatment of the stricture.
Surgical treatment: The need for surgical intervention during the follow-up period after the initial ES treatment.
Re-endoscopic intervention: The need for repeat endoscopic treatment during the follow-up period after initial ES treatment, including balloon dilation and ES.
Complications: Perforation, massive bleeding, or infection occurring during or within 1 week after ES treatment.
Continuous variables are summarized as the mean ± SD or median with interquartile range. Categorical variables are expressed as percentages.
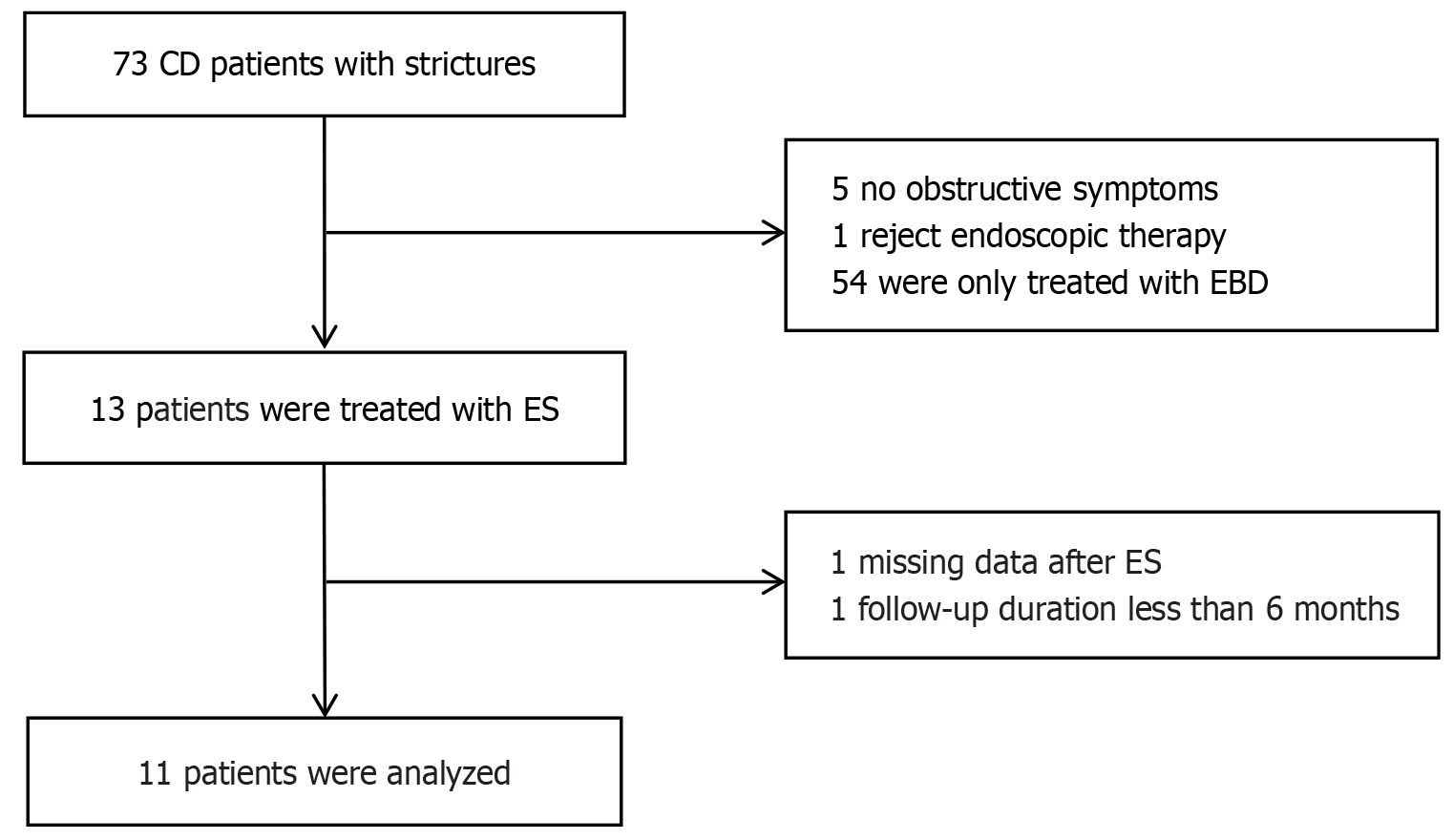
A total of 73 patients with stricturing CD were treated at our center between June 2020 and April 2024. After excluding patients with missing data and insufficient follow-up time, 11 eligible patients with CD who underwent ES were included, as shown in Figure 1. A total of 17 ES were performed in 11 patients. The average age was 40.1 ± 13.9 years, with six male and five female patients. Among them, three patients had previously undergone partial small bowel resection.
All patients were able to pass through the stenosis smoothly after treatment, with an immediate success rate of 100%. Among them, one patient underwent EBD and ES at the same site, and four patients underwent EBD and ES at different sites for a total of six times. During the follow-up period, two patients underwent partial small bowel resection in gastrointestinal surgery, and the rate of surgical treatment was 18.2%. Two patients had a recurrence of stenosis and required endoscopic treatment, and the rate of re-endoscopic intervention was 18.2%. The remission duration after the initial ES treatment was 10.1 ± 8.2 months, with a median remission time of 10 months. Another patient developed obstructive symptoms 18 months after ES that were relieved with conservative treatment and without surgical intervention. The detailed patient follow-up information is shown in Table 1. None of the patients treated with ES experienced immediate complications. Figure 2 show the BAE-based ES technique for stricture in patients with CD.
| Patient | Age (years) | History of small bowel surgery | Stricture incision site | Number of incisions | Two narrow distances (cm) | Stricture without angulation | Combined balloon dilatation | Re-intervention |
| 1 | 56 | No | Ileocecal valve | 1 | Yes | No | Partial small intestine resection was performed 6 months after surgery | |
| 2 | 51 | No | Ileum | 1 | Yes | Yes | No | |
| 3 | 37 | No | Ileocecal valve | 1 | No | No | No | |
| 4 | 28 | No | Ileocecal valve | 1 | Yes | No | Yes | |
| 29 | Ascending colon + ileocecal valve | 2 | 4 | Yes | Yes | Yes | ||
| 29 | Proximal ascending colon | 1 | Yes | Yes | Yes | |||
| 31 | Ileocecal valve | 1 | Yes | Yes | Yes | |||
| 5 | 60 | Yes | Ileum | 1 | Yes | Yes | No | |
| 6 | 30 | Yes | Ileocecal valve | 1 | Yes | No | No | |
| 7 | 33 | Yes | Duodenum | 1 | No | No | Yes | |
| 34 | Duodenum | 1 | No | Yes | No | |||
| 8 | 28 | No | Ileum | 1 | No | No | No | |
| 9 | 72 | No | Ileum | 2 | 6 | No | No | Partial small intestine resection was performed 1 month after surgery |
| 10 | 35 | No | Rectum | 1 | No | Yes | No | |
| 11 | 49 | No | Ileocecal valve | 1 | Yes | No | No |
CD typically begins with primary intestinal inflammation (B1 type) and gradually progresses to stricturing or penetrating types (B2 and B3 types). During prolonged intestinal inflammation, the excessive growth of fibrous tissue in the muscularis propria and mucosal layers leads to intestinal strictures. In patients with CD, strictures can be detected using CTE, MRE, or endoscopy. The most commonly affected sites of strictures are the terminal ileum, right colon, and surgical anastomosis. Although most patients with CD present with simple inflammation at onset, 5%-28% of individuals experience stricture complications at the time of initial diagnosis[4]. Intestinal strictures are the primary reason for hospitalization and surgery in patients with CD, with more than half of the patients experiencing intestinal stenosis or obstruction during disease progression[5]. Therefore, timely detection and treatment of strictures are crucial for patients with CD. Selecting appropriate treatment methods is the key to improving the quality of life and reducing the occurrence of complications.
Over the past decade, endoscopic interventions have led to significant advancements in the treatment of inflammatory bowel disease (IBD). Endoscopic therapy, an important means of improving intestinal strictures, has gradually gained international attention from physicians. EBD has been widely used to treat IBD-related strictures, and its effectiveness and safety have been validated. EBD is suitable for clinically significant obstructive patients, especially those with short benign strictures (length ≤ 5 cm) without sharp angulation or accompanying deep ulcers or fistulas, and it can effectively alleviate obstructive symptoms[6]. When performing balloon dilation, it is crucial to ensure that the maximum balloon diameter does not exceed 18 mm and that the inflation time is at least 1 minute to guarantee safe and effective treatment of strictures[3]. According to a meta-analysis by Bettenworth et al[7], the technical success rate of EBD in patients with small bowel strictures associated with CD was 94.9%, and 82.3% of patients experienced relief from obstructive symptoms. During a mean follow-up period of 20.5 months, 38.8% of the patients required repeat EBD treatment, and 27.4% of the patients eventually needed surgical intervention. Lee et al[8] demonstrated that EBD is safe and effective in treating benign strictures in patients with IBD. Over a follow-up period of up to 10 years, EBD continued to effectively alleviate symptoms of strictures in IBD patients, providing them with long-lasting benefits. In our gastrointestinal endoscopy center, we also investigated the efficacy of EBD in CD-associated intestinal stenosis. Our findings are similar to those of other studies. In this study, we combined EBD to perform stenosis dilation, and no serious complications were found intraoperatively. Our center has also conducted a study on the efficacy of EBD dilated stenosis, and the preliminary conclusions suggest EBD has good efficacy and safety for small intestine stenosis, which may require multiple endoscopic treatments. However, relevant data has yet to be published.
Currently, studies suggest that stent placement can be effective, but the occurrence of complications such as stent migration, fistula formation, or perforation is relatively high, which limits its widespread clinical application. However, with the continuous development of technology, the future prospects of this technique may be expanded by developing new types of stents that are resistant to migration, self-expanding, or biodegradable, potentially offering new avenues for advancement[9].
As a relatively new technique, stricturotomy has a relatively short history of implementation. Currently, endoscopic treatment studies on CD strictures focus primarily on balloon dilation, with few reports on stricturotomy. ES involves the use of an electrocautery knife to incise the mucosal layer and submucosal fibrosis along the longitudinal axis of the intestinal lumen, thereby enlarging the diameter of the stricture and achieving dilation[10]. Lan and Shen[11] confirmed in a controlled study that ES has higher immediate and clinical efficacy than EBD. Moreover, in terms of safety, ES carries a lower risk of perforation than does EBD, although the risk of immediate or delayed bleeding is higher with ES than with EBD. In this study, 11 patients underwent stricturotomy with a 100% immediate success rate and no bleeding, perfo
Additionally, in this study, one patient initially underwent balloon dilation at the stricture site, which failed to completely relieve the narrowing. Subsequently, a stricturotomy was performed, which successfully dilated the stricture, and the procedure proceeded smoothly. Another patient experienced obstructive symptoms 18 months postoperatively and was managed conservatively without surgical intervention. One patient underwent repeated endoscopic treatment for recurrent intestinal strictures. Despite multiple discussions with physicians recommending surgical intervention, the patient refused. However, the obstructive symptoms were relieved after ES and balloon dilation. ES is characterized by clear efficacy, minimal invasiveness, and safety. Although this may not completely prevent stricture recurrence, patients may require repeat endoscopic interventions. However, this delays the need for surgery and improves the quality of life of patients.
ES is performed under direct endoscopic visualization, allowing precise control over the location, direction, and depth of stricture incision, thereby effectively reducing the risk of injury to the intestinal tract and adjacent organs. Therefore, research suggests that ES is particularly suitable for treating rectal stenosis caused by perianal lesions in CD[12]. In this study, one patient with rectal stricture achieved satisfactory outcomes with ES performed under transanal enteroscopy. Additionally, in our department, one patient with CD underwent ES treatment under colonoscopy. During postoperative follow-up, there was no recurrence of strictures, and bowel habits improved.
This study suggests that ES treatment yields relatively good outcomes for short-segment solitary strictures located far from the ileocecal valve. Currently, ES is recommended for nonconcentric, nonhomogeneous strictures, particularly ulcerative and fusiform[10]. ES allows precise incisions tailored to these complex strictures, thereby maximizing treatment efficacy and enhancing procedural safety. EBD is recommended for the treatment of concentric valvular strictures. This is because valvular strictures typically have a more regular morphology, and balloons can uniformly dilate the narrowing site, achieving better treatment outcomes[13].
Because CD is characterized by segmental lesions, and strictures are often multi-segmental, the choice of treatment for strictures should be tailored to the specific location and characteristics of the lesions. In this study, physicians selected either ES or EBD for different strictures in the same patient, based on specific circumstances. This requires the operating physician to possess extensive professional knowledge and clinical experience. When choosing a treatment method, doctors need to comprehensively consider the patient’s specific condition, the location of the lesion, the degree of stricture, and other factors to develop a personalized treatment plan. In addition, patients should continue to receive standard medication therapy and postoperative follow-up care to control disease progression and prevent disease recurrence.
Our study had some limitations. First, this was a retrospective study, and heterogeneity in patient characteristics was inevitable. Second, it involved only a few cases, making it prone to statistical bias. Therefore, the sample size should be expanded, and multicenter long-term follow-up research should be considered to improve on these limitations. In future studies, it can be compared with EBD in the treatment of stenosis.
In patients with CD, ES can effectively alleviate symptoms caused by intestinal strictures, such as abdominal pain, bloating, and difficulty in defecation. Compared with surgical procedures, ES is less invasive, offers faster recovery, and reduces the risk of severe complications, such as bowel perforation and fistulas. ES is a reliable method for treating stricturing CD and is generally more acceptable to patients than surgical intervention. However, ES for treating stricturing CD is still in its early stages. Further large-scale clinical studies are required to confirm the long-term efficacy and potential risks of ES.
I would like to thank my colleagues, especially the nurses of the endoscopy team, Fu Xu and Jiao He, without whom the enteroscopy would not have been completed smoothly.
| 1. | Triantafillidis JK. Surgical treatment of inflammatory bowel disease: From the gastroenterologist's stand-point. World J Gastrointest Surg. 2024;16:1235-1254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Elford AT, Ardalan Z, Simkin P, Christensen B. Comprehensive review and update of stricturing Crohn's disease. Indian J Gastroenterol. 2024;43:64-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Meima-van Praag EM, Buskens CJ, Hompes R, Bemelman WA. Surgical management of Crohn's disease: a state of the art review. Int J Colorectal Dis. 2021;36:1133-1145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 4. | Chan WPW, Mourad F, Leong RW. Crohn's disease associated strictures. J Gastroenterol Hepatol. 2018;33:998-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 5. | Liu Z, Huang Z, Wang Y, Xiong S, Lin S, He J, Tan J, Liu C, Wu X, Nie J, Huang W, Zhang Y, Zhou L, Mao R. Intestinal strictures in Crohn's disease: An update from 2023. United European Gastroenterol J. 2024;12:802-813. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Ismail MS, Charabaty A. Management of Crohn's stricture: medical, endoscopic and surgical therapies. Frontline Gastroenterol. 2022;13:524-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 7. | Bettenworth D, Bokemeyer A, Kou L, Lopez R, Bena JF, El Ouali S, Mao R, Kurada S, Bhatt A, Beyna T, Halloran B, Reeson M, Hosomi S, Kishi M, Hirai F, Ohmiya N, Rieder F. Systematic review with meta-analysis: efficacy of balloon-assisted enteroscopy for dilation of small bowel Crohn's disease strictures. Aliment Pharmacol Ther. 2020;52:1104-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 8. | Lee HW, Park SJ, Jeon SR, Ye BD, Park JJ, Cheon JH, Kim TI, Kim WH; Korean Association for the Study of the Intestinal Diseases (KASID). Long-Term Outcomes of Endoscopic Balloon Dilation for Benign Strictures in Patients with Inflammatory Bowel Disease. Gut Liver. 2018;12:530-536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Sleiman J, El Ouali S, Qazi T, Cohen B, Steele SR, Baker ME, Rieder F. Prevention and Treatment of Stricturing Crohn's Disease - Perspectives and Challenges. Expert Rev Gastroenterol Hepatol. 2021;15:401-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 10. | Gu YB, Zhong J; Chinese IBD Endoscopic Club. Endoscopic management of stricturing Crohn's disease. J Dig Dis. 2020;21:351-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Lan N, Shen B. Endoscopic Stricturotomy Versus Balloon Dilation in the Treatment of Anastomotic Strictures in Crohn's Disease. Inflamm Bowel Dis. 2018;24:897-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Navaneethan U. Endoscopic Stricturotomy for Refractory Anal Strictures in Crohn's Disease. Inflamm Bowel Dis. 2020;26:e99-e100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Shen B, Kochhar G, Navaneethan U, Farraye FA, Schwartz DA, Iacucci M, Bernstein CN, Dryden G, Cross R, Bruining DH, Kobayashi T, Lukas M, Shergill A, Bortlik M, Lan N, Lukas M, Tang SJ, Kotze PG, Kiran RP, Dulai PS, El-Hachem S, Coelho-Prabhu N, Thakkar S, Mao R, Chen G, Zhang S, Suárez BG, Lama YG, Silverberg MS, Sandborn WJ. Practical guidelines on endoscopic treatment for Crohn's disease strictures: a consensus statement from the Global Interventional Inflammatory Bowel Disease Group. Lancet Gastroenterol Hepatol. 2020;5:393-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |