Published online Aug 27, 2024. doi: 10.4240/wjgs.v16.i8.2538
Revised: June 27, 2024
Accepted: June 28, 2024
Published online: August 27, 2024
Processing time: 126 Days and 12.1 Hours
Acute appendicitis is one of the most common emergency abdominal disease, and recent studies have evaluated conservative treatment using antibiotics for uncomplicated appendicitis. Although the efficacy of conservative treatment for uncomplicated appendicitis is known, its efficacy for complicated appendicitis remains unknown, so are risk factors for the conservative treatment of appendi
To investigate the indication of conservative treatment by antibiotics for uncomplicated and complicated acute appendicitis
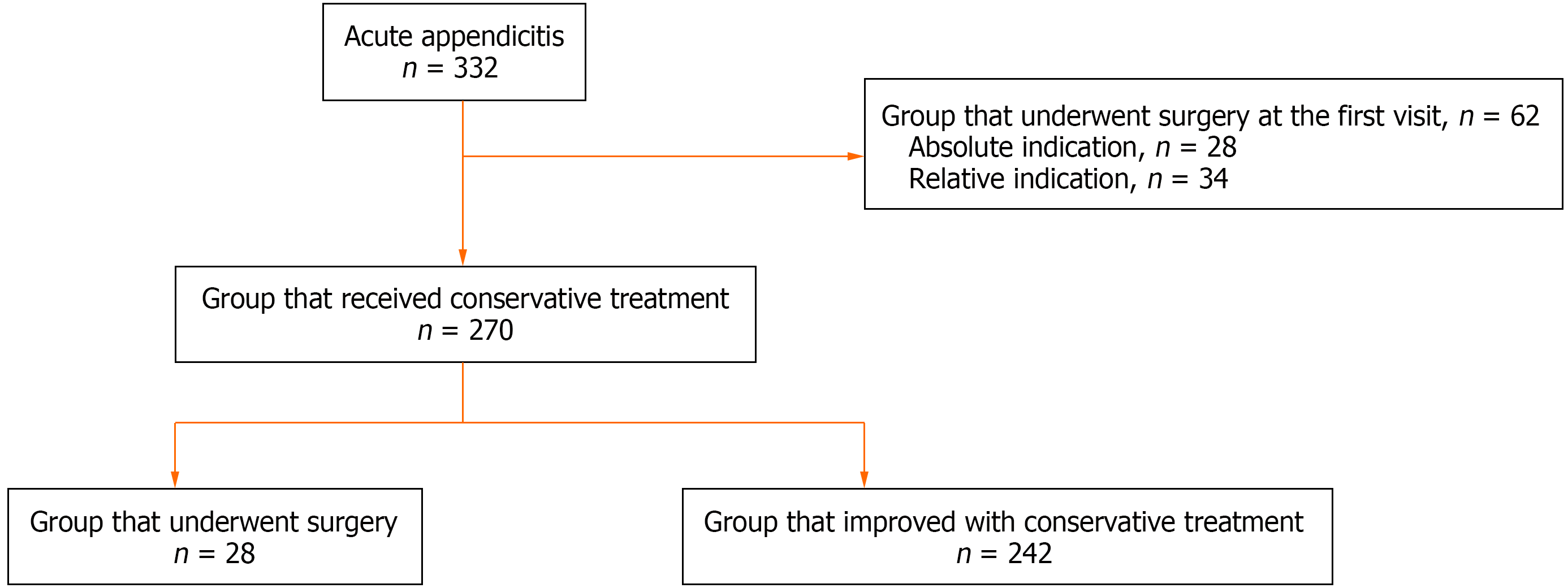
We investigated 270 patients who received conservative treatment for acute appendicitis at the Nishitokyo Central General Hospital, between April 2011 and February 2022. Twenty-eight (10.3%) patients were resistant to conservative treatment and underwent surgery. We retrospectively investigated the outcomes of conservative treatment for appendicitis and the risk factors for resistance to conservative treatment using the receiver operating characteristic curves and Cox hazard model.
Two hundred and forty-two (89.7%) patients improved with conservative treatment. The significant and independent predictors of resistance to conservative treatment were body temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid visible on computed tomography (CT). The rate of resistance to conservative treatment was 66.7% (6/9) for patients with the above three factors, 22.9% (8/35) for patients with two factors (appendicolith and body temperature ≥ 37.3 °C), 16.7% (2/12) for patients with two factors (Douglas sinus fluid and appendicolith) and 11.1% (1/9) for patients with two factors (Douglas sinus fluid and body temperature ≥ 37.3 °C).
A temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid on CT might be clinical risk factors of resistance to conservative treatment for acute appendicitis.
Core Tip: This is a retrospective study to investigate the outcomes of conservative treatment for uncomplicated and complicated acute appendicitis. The success rate of conservative treatment of acute appendicitis was 89.7%. The significant and independent predictors of resistance to conservative treatment were body temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid. The rate of resistance to conservative treatment was 66.7% for patients with the above three factors, therefore, surgical treatment should be recommended at the first visit. Body temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid might be clinical risk factors for resistance to conservative treatment for acute appendicitis.
- Citation: Hosokawa Y, Moritani M, Makuuchi Y, Nagakawa Y. Indication of conservative treatment by antibiotics for uncomplicated and complicated acute appendicitis. World J Gastrointest Surg 2024; 16(8): 2538-2545
- URL: https://www.wjgnet.com/1948-9366/full/v16/i8/2538.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i8.2538
Acute appendicitis is one of the most common emergency abdominal diseases, and appendectomy has long been the standard treatment. However, recent studies have evaluated conservative treatment using antibiotics for uncomplicated appendicitis[1-9]. In addition, international guidelines suggest that conservative treatment is effective and an alternative to surgery for uncomplicated appendicitis[10-13].
Coronavirus disease 2019 (COVID-19) was first reported in China in 2019 and has since spread worldwide. COVID-19 potentially increases surgical morbidity and mortality, therefore, emergency surgery is not recommended for COVID-19 patients[14,15]. Furthermore, surgery under general anesthesia increases the risk of COVID-19 infection for medical staff because of viral transmission via aerosolization. Therefore, the use of antibiotics alone for acute appendicitis has become more prevalent and paramount. However, International guidelines recommend conservative treatment for uncomplicated appendicitis but not for complicated appendicitis[10-12]. Although, complicated appendicitis is generally associated with perforation, abscess, appendicolith, etc.[8,10-12], there are no reports or guidelines with a clear definition of the difference between uncomplicated and complicated appendicitis. Therefore, at present, the kind of treatment to be selected for each case is not known, especially in complicated appendicitis.
In our institution, conservative treatment has long been the first choice for most appendicitis cases, except for perforation. Therefore, this novel study investigated the outcomes of conservative treatment for uncom
We collected the data of 332 patients who were hospitalized at Nishitokyo Central General Hospital, because of acute appendicitis between April 2011 and February 2022. We retrospectively investigated the outcomes of conservative treatment for appendicitis and the risk factors for resistance to conservative treatment.
Nishitokyo Central General Hospital has its own Institutional Review Board (IRB). This study was approved for use in the hospital database for research by the IRB (Approval No. 2018-004).
To diagnose acute appendicitis, computed tomography (CT) and laboratory tests were performed on all patients at the first visit. A diagnosis of acute appendicitis was made by comprehensive physical examination, increased inflammatory reaction [white blood cell (WBC), C-reactive protein (CRP)], and the presence of an enlarged appendix on CT. Patients who were strongly suspected of having a neoplasm through a CT scan at the first visit were excluded from this study. Patients with rebound pain in the entire abdomen (diffuse peritonitis), vital signs indicating shock, and perforation of the appendix (extraluminal air present) on CT were not suitable for conservative treatment. However, they were absolute indications for surgery. Furthermore, patients who wanted to undergo surgery were also not suitable for conservative treatment and hence, were a relative indication for surgery. Regardless of the level of inflammation, we performed the conservative treatment with antibiotics in all patients. All patients were hospitalized and managed by fasting, cooling the site of abdominal pain, and administering antibiotics. We basically administered intravenous flomoxef sodium. On the other hand, we administered meropenem hydrate for cases with severe abdominal pain, CRP ≥ 10, abscess, or appendix size ≥ 15mm. Laboratory and abdominal examinations were performed daily. When we judged that the condition had not improved due to persistent fever, no improvement in abdominal pain and in WBC and CRP, a CT scan was done to determine whether surgery was indicated.
All statistical analyses were performed using the chi-square test, Mann-Whitney U-test and SPSS for Windows (SPSS, Tokyo, Japan). Receiver operating characteristic (ROC) curves were used to determine the cutoff points for data concentrations that indicated resistance to conservative treatment. Significant factors were identified using univariate analysis and further examined using multivariate analysis. A multivariate regression analysis was performed using the Cox hazard model. A P value of less than 0.05 indicated a statistically significant difference between the two groups.
A total of 332 patients were diagnosed with appendicitis. Out of this, 28 patients had an absolute indication for surgery, and 34 patients had a relative indication for surgery. Therefore, 270 patients received conservative treatment for acute appendicitis. Twenty-eight (10.3%) patients were resistant to conservative treatment and underwent surgery (Figure 1). We compared the age and laboratory tests such as WBC count, CRP level, time taken to hospital, body temperature and size of the appendix on CT between the group that underwent surgery and the group that improved with conservative treatment (Table 1). Only body temperature was significantly higher in the surgery group, and there were no significant differences in WBC count, CRP level, and appendix size on CT.
| Surgery group, n = 28 | Conservative group, n = 242 | P value | |
| Age | 41.9 ± 19.8 | 44.8 ± 20.7 | 0.495 |
| Time to visit hospital (hour) | 38.6 ± 70.0 | 37.6 ± 66.1 | 0.453 |
| Body temperature (°C) | 37.8 ± 1.0 | 37.2 ± 0.8 | < 0.001 |
| WBC count (/μL) | 13440.4 ± 4130.1 | 12489.8 ± 3986.3 | 0.325 |
| CRP (mg/dL) | 5.9 ± 7.3 | 4.2 ± 5.3 | 0.311 |
| Size of appendix (mm) | 14.0 ± 3.7 | 12.3 ± 4.1 | 0.014 |
A ROC curve was constructed to determine the cut-off points for resistance to conservative treatment by the time taken to visit the hospital, body temperature, WBC count, CRP level and appendix size on CT. The optimal cut off points were defined as points plotted close to the point from the upper left corner of the ROC curve. The optimal cut-off points were 22 hours for the time to visit the hospital, 37.3 °C for body temperature, 15160 count/μL for WBC, 4.6 mg/dL for CRP and 12 mm for appendix (Table 2).
| Cutoff value | Area under the curve | FPF | TPF | |
| Time to visit hospital (hour) | 22 | 0.5432 | 0.434 | 0.571 |
| Body temperature (°C) | 37.3 | 0.6923 | 0.368 | 0.679 |
| WBC count (/μL) | 15160 | 0.5568 | 0.236 | 0.429 |
| CRP (mg/dL) | 4.6 | 0.5584 | 0.351 | 0.500 |
| Size of appendix (mm) | 12 | 0.6409 | 0.533 | 0.786 |
To determine the predictors of resistance to conservative treatment, we examined 16 items: Age, sex, past history of appendicitis, the existence of rebound pain, time to visit the hospital, body temperature, WBC count, CRP, size of the appendix, stranding of the adjacent fat and periappendiceal fluid and air in the appendix. Additionally, abscess and appendicolith and Douglas sinus fluid on CT, and type of antibiotics were assessed (Table 3). Univariate analysis showed that the following 10 factors were associated with resistance to conservative treatment: Body temperature ≥ 37.3 °C (P = 0.001), WBC count ≥ 15160/μL (P = 0.027), appendix size ≥ 12 mm (P = 0.011), stranding of the adjacent fat (P = 0.020), the air in the appendix (P = 0.014), abscess (P = 0.048), appendicolith (P < 0.001), Douglas sinus fluid (P = 0.003), and broad-spectrum antibiotics (P = 0.009). Multivariate analysis showed that, body temperature ≥ 37.3 °C (P = 0.028), appendicolith (P = 0.008) and Douglas sinus fluid (P = 0.016) were significant and independent predictors of resistance to conservative treatment.
| | Surgery group, n = 28 | Conservative group, n = 242 | Univariate analysis, P value | Multivariate analysis, P value | Hazard ration |
| Age | |||||
| < 75 | 26 (10.7) | 216 (89.3) | 0.554 | ||
| ≥ 75 | 2 (7.1) | 26 (92.9) | |||
| Sex | |||||
| Female | 12 (11.1) | 96 (88.9) | 0.744 | ||
| Male | 16 (9.9) | 146 (90.1) | |||
| Past history of appendicitis | |||||
| (-) | 25 (11.6) | 190 (88.4) | 0.180 | ||
| (+) | 3 (5.5) | 52 (94.5) | |||
| Rebound pain | |||||
| (-) | 9 (7.8) | 106 (92.2) | 0.238 | ||
| (+) | 19 (12.3) | 136 (87.7) | |||
| Time to visit hospital (hour) | |||||
| < 22 | 12 (8.1) | 137 (81.9) | 0.166 | ||
| ≥ 22 | 16 (13.2) | 105 (86.8) | |||
| Body temperature (°C) | |||||
| < 37.3 | 9 (5.6) | 153 (94.4) | 0.001 | 0.028 | 2.945 |
| ≥ 37.3 | 19 (17.6) | 89 (82.4) | |||
| WBC count (/μL) | |||||
| < 15160 | 16 (8.0) | 185 (92.0) | 0.027 | 0.138 | |
| ≥ 15160 | 12 (17.4) | 57 (82.6) | |||
| CRP (mg/dL) | |||||
| < 4.6 | 14 (8.2) | 157 (91.8) | 0.122 | ||
| ≥ 4.6 | 14 (14.1) | 85 (85.9) | |||
| Size of appendix (mm) | |||||
| < 12 | 6 (5.0) | 113 (95.0) | 0.011 | 0.600 | |
| ≥ 12 | 22 (14.6) | 129 (85.4) | |||
| Stranding of the adjacent fat | |||||
| (-) | 1 (1.3) | 79 (98.7) | 0.001 | 0.162 | |
| (+) | 27 (16.6) | 163 (83.4) | |||
| Periappendiceal fluid | |||||
| (-) | 19 (8.4) | 206 (91.6) | 0.020 | 0.892 | |
| (+) | 9 (20.0) | 36 (80.0) | |||
| Air in appendix | |||||
| (-) | 22 (8.9) | 224 (81.1) | 0.014 | 0.164 | |
| (+) | 6 (25.0) | 18 (75.0) | |||
| Abscess | |||||
| (-) | 24 (9.4) | 230 (80.6) | 0.048 | 0.083 | |
| (+) | 4 (25.0) | 12 (75.0) | |||
| Appendicolith | |||||
| (-) | 9 (5.1) | 167 (94.9) | < 0.001 | 0.008 | 3.746 |
| (+) | 19 (20.2) | 75 (79.8) | |||
| Douglas sinus fluid | |||||
| (-) | 17 (7.7) | 203 (92.3) | 0.003 | 0.016 | 3.580 |
| (+) | 11 (22.0) | 39 (78.0) | |||
| Antibiotics | |||||
| Second-generation cephems | 14 (7.3) | 178 (92.7) | 0.009 | 0.260 | |
| Broad-spectrum | 14 (17.9) | 64 (82.1) |
Of the patients with three factors (body temperature ≥ 37.3 °C, existences of appendicolith and Douglas sinus fluid), six (66.7%) were resistant to conservative treatment. Among the patients with two factors, one patient (11.1%) with Douglas sinus fluid and body temperature ≥ 37.3 °C, two (16.7%) with Douglas sinus fluid and appendicolith, and eight (22.9%) with appendicolith and body temperature ≥ 37.3 °C were resistant to conservative treatment (Table 4).
| Number of risk factors | Total number | Surgery |
| 0 factor | 92 | 2 (2.2) |
| 1 factor | ||
| Body temperature ≥ 37.3 °C | 55 | 4 (7.3) |
| Douglas sinus fluid | 20 | 2 (10.0) |
| Appendicolith | 38 | 3 (7.9) |
| 2 factors | ||
| Douglas sinus fluid + body temperature ≥ 37.3 °C | 9 | 1 (11.1) |
| Douglas sinus fluid + appendicolith | 12 | 2 (16.7) |
| Appendicolith + body temperature ≥ 37.3 °C | 35 | 8 (22.9) |
| 3 factors | 9 | 6 (66.7) |
The purpose of this study was to determine whether patients with acute appendicitis were resistant to conservative treatment using data from their first visit to the hospital. In this study, the success rate of the conservative treatment was 89.7%. However, 28 (10.3%) patients were resistant to conservative treatment and underwent surgery. The significant and independent predictors of resistance to conservative treatment were body temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid on CT. Generally, guidelines[10-12] defined complicated appendicitis as perforation, appendicolith, or abscess. Furthermore, these cases were excluded from the indications for conservative treatment for acute appendicitis in randomized control studies. At our institution, conservative treatment is administered for acute appendicitis, regardless of the data on inflammation, except for perforated cases. Therefore, we performed this study to identify factors associated with resistance for conservative treatment for acute appendicitis, including complicated appendicitis.
Although appendicolith and abscess are generally defined as risk factors for complicated appendicitis, in this study, appendicolith was indicated as a risk factor, and abscess was not indicated. On the other hand, although not defined, fever and Douglas sinus fluid were also indicated as factors associated with resistance to conservative treatment. Fever was not identified as a risk factor in some guidelines[8,10-12], however, it was indicated as an appendicitis severity score in some reports[15-17]. Recently, some studies reported percutaneous drainage of abscesses, followed by interval appendectomy[18,19]. We believe that abscess drainage is an effective procedure. However, there were no patients in whom abscess drainage was performed in this study owing to facility problems. In this study, 16 patients were diagnosed with abscesses, of whom four underwent surgery and 12 improved with conservative treatment. The median size of abscess in the 16 patients was 25 (5-45) mm, with the median size in the 4 and 12 patients being 25 (19-32) mm and 21 (5-45) mm, respectively, with no significant difference in size. In addition, we re-examined the CT scans of 16 patients with abscess; there were no cases in which abscess drainage was considered safe. We believe that abscess drainage is an effective procedure as part of conservative treatment for large abscesses that can be safely drained. However, even when the abscess cannot be drained, we believe that the condition can be improved with conservative treatment without abscess drainage.
Few studies have discussed the relationship between imaging findings and complicated acute appendicitis[17]. Similarly, in this study, we focused on following CT imaging such as the size of the appendix, stranding of the adjacent fat, periappendiceal fluid, air in appendix, abscess, appendicolith, and Douglas sinus fluid. Among these findings, only Douglas sinus fluid was indicated as a risk factor, except for appendicolith. Fujiwara et al[17] reported the imaging findings of stranding of the adjacent fat and periappendiceal fluid also indicated as a risk factor of complicated appendicitis[17]. However, this report defined complicated appendicitis as pathological appendicitis with gangrene, which might be different from clinically complicated appendicitis being resistant to conservative treatment as we think. Intraoperative findings included infected ascites in a few patients who underwent surgery and serous ascites in others. Douglas sines fluid was a risk factor even when these patients were included, and might represent the spread of inflammation.
The average length of hospital stay for conservative treatment was 10 days, which was longer than that in some reports. This attributed to the inclusion of all cases in which conservative treatment was indicated at the request of the patient despite the high inflammation level, and CT-detected appendicolith and abscess. These patients may require a relatively long time to improve. In addition, this was probably because all patients were managed by fasting until the data indicating inflammation improved. Moreover, they were hospitalized for several days after starting the diet. However, for patients who desire to avoid surgery, this length of hospital stay is considered acceptable if surgery can be avoided. Another problem is the long hospitalization period of 16 days for patients who underwent surgery. This is probably because 6 of 28 patients who underwent surgery underwent ileocecal resection.
There was also a risk that a neoplasm would be present in the patient with complicated appendicitis. Some reports have indicated that approximately 10% of neoplasms were found in interval appendectomy for complicated appendicitis[20,21]. In this study, 28 patients who were resistant to conservative treatment and underwent surgery had no neoplasms. However, we strongly recommended colonoscopy and CT after one month for all patients with findings such as appendicoliths and abscesses that improved with conservative treatment. There were no neoplasms among the patients who underwent CT and colonoscopy. However, it is uncertain whether this follow-up method is sufficient to rule out neoplasms.
This study has a limitation. There were no clear surgical criteria for patients whose conditions worsened after conservative treatment. The decision to perform surgery was left to the surgeons at the time. However, as the chief of our surgical team during this study did not change, we do not believe that the decision for surgery has changed significantly.
This study was a retrospective study conducted at a single institution. In the future, it may be desirable to conduct prospective studies for the patients with the above three or two factors; however, conducting such a study would be challenging. Therefore, we believe that it is necessary to present these results to patients with the above three or two risk factors and allow them to choose a treatment method. Furthermore, whether the results improve perioperative factors such as hospital stay and surgical complications should be examined.
In this study, the success rate of conservative treatment of acute appendicitis was 89.7%. The significant and independent predictors of resistance to conservative treatment were body temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid on CT. The rate of resistance to conservative treatment was 66.7% for patients with the above three factors, therefore, surgical treatment should be recommended at the first visit. Body temperature ≥ 37.3 °C, appendicolith and Douglas sinus fluid on CT might be clinical risk factors for resistance to conservative treatment for acute appendicitis.
| 1. | Livingston E, Vons C. Treating Appendicitis Without Surgery. JAMA. 2015;313:2327-2328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Podda M, Cillara N, Di Saverio S, Lai A, Feroci F, Luridiana G, Agresta F, Vettoretto N; ACOI (Italian Society of Hospital Surgeons) Study Group on Acute Appendicitis. Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15:303-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 3. | Poon SHT, Lee JWY, Ng KM, Chiu GWY, Wong BYK, Foo CC, Law WL. The current management of acute uncomplicated appendicitis: should there be a change in paradigm? A systematic review of the literatures and analysis of treatment performance. World J Emerg Surg. 2017;12:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Harnoss JC, Zelienka I, Probst P, Grummich K, Müller-Lantzsch C, Harnoss JM, Ulrich A, Büchler MW, Diener MK. Antibiotics Versus Surgical Therapy for Uncomplicated Appendicitis: Systematic Review and Meta-analysis of Controlled Trials (PROSPERO 2015: CRD42015016882). Ann Surg. 2017;265:889-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 135] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Prechal D, Damirov F, Grilli M, Ronellenfitsch U. Antibiotic therapy for acute uncomplicated appendicitis: a systematic review and meta-analysis. Int J Colorectal Dis. 2019;34:963-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 6. | Rollins KE, Varadhan KK, Neal KR, Lobo DN. Antibiotics Versus Appendicectomy for the Treatment of Uncomplicated Acute Appendicitis: An Updated Meta-Analysis of Randomised Controlled Trials. World J Surg. 2016;40:2305-2318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 7. | Yang Z, Sun F, Ai S, Wang J, Guan W, Liu S. Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 2019;19:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | CODA Collaborative, Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE, Drake FT, Fischkoff K, Johnson J, Patton JH, Evans H, Cuschieri J, Sabbatini AK, Faine BA, Skeete DA, Liang MK, Sohn V, McGrane K, Kutcher ME, Chung B, Carter DW, Ayoung-Chee P, Chiang W, Rushing A, Steinberg S, Foster CS, Schaetzel SM, Price TP, Mandell KA, Ferrigno L, Salzberg M, DeUgarte DA, Kaji AH, Moran GJ, Saltzman D, Alam HB, Park PK, Kao LS, Thompson CM, Self WH, Yu JT, Wiebusch A, Winchell RJ, Clark S, Krishnadasan A, Fannon E, Lavallee DC, Comstock BA, Bizzell B, Heagerty PJ, Kessler LG, Talan DA. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N Engl J Med. 2020;383:1907-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 331] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 9. | Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Mecklin JP, Sand J, Virtanen J, Jartti A, Grönroos JM. Five-Year Follow-up of Antibiotic Therapy for Uncomplicated Acute Appendicitis in the APPAC Randomized Clinical Trial. JAMA. 2018;320:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 315] [Article Influence: 45.0] [Reference Citation Analysis (2)] |
| 10. | Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De' Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De' Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 596] [Article Influence: 119.2] [Reference Citation Analysis (109)] |
| 11. | Flum DR. Clinical practice. Acute appendicitis--appendectomy or the "antibiotics first" strategy. N Engl J Med. 2015;372:1937-1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 126] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 12. | Schuster KM, Holena DN, Salim A, Savage S, Crandall M. American Association for the Surgery of Trauma emergency general surgery guideline summaries 2018: acute appendicitis, acute cholecystitis, acute diverticulitis, acute pancreatitis, and small bowel obstruction. Trauma Surg Acute Care Open. 2019;4:e000281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Flemming S, Hankir M, Ernestus RI, Seyfried F, Germer CT, Meybohm P, Wurmb T, Vogel U, Wiegering A. Surgery in times of COVID-19-recommendations for hospital and patient management. Langenbecks Arch Surg. 2020;405:359-364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 14. | English W, Habib Bedwani N, Smith C, Doganay E, Marsden M, Muse S, Mak WK, Chana M, Eves J, Shatkar V. Suspected appendicitis and COVID-19, a change in investigation and management-a multicentre cohort study. Langenbecks Arch Surg. 2021;406:357-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015;102:979-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 133] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 16. | Avanesov M, Wiese NJ, Karul M, Guerreiro H, Keller S, Busch P, Jacobsen F, Adam G, Yamamura J. Diagnostic prediction of complicated appendicitis by combined clinical and radiological appendicitis severity index (APSI). Eur Radiol. 2018;28:3601-3610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Fujiwara K, Abe A, Masatsugu T, Hirano T, Hiraka K, Sada M. Usefulness of several factors and clinical scoring models in preoperative diagnosis of complicated appendicitis. PLoS One. 2021;16:e0255253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 18. | Takeda K, Yamada T, Uehara K, Matsuda A, Shinji S, Yokoyama Y, Takahashi G, Iwai T, Kuriyama S, Miyasaka T, Kanaka S, Yoshida H. The benefits of interval appendectomy and risk factors for nonoperative management failure in the therapeutic strategy for complicated appendicitis. Surg Today. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 19. | Peltrini R, Schiavo C, Pilone V. Three reasons to consider interval appendectomy for the management of complicated appendicitis. Updates Surg. 2024;76:1121-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 20. | Hayes D, Reiter S, Hagen E, Lucas G, Chu I, Muñiz T, Martinez R. Is interval appendectomy really needed? A closer look at neoplasm rates in adult patients undergoing interval appendectomy after complicated appendicitis. Surg Endosc. 2021;35:3855-3860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Peltrini R, Cantoni V, Green R, Lionetti R, D'Ambra M, Bartolini C, De Luca M, Bracale U, Cuocolo A, Corcione F. Risk of appendiceal neoplasm after interval appendectomy for complicated appendicitis: A systematic review and meta-analysis. Surgeon. 2021;19:e549-e558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |