Published online Jul 27, 2024. doi: 10.4240/wjgs.v16.i7.2221
Revised: June 3, 2024
Accepted: June 18, 2024
Published online: July 27, 2024
Processing time: 83 Days and 8.4 Hours
Peripherally inserted central catheters (PICCs) are commonly used in hospitalized patients with liver cancer for the administration of chemotherapy, nutrition, and other medications. However, PICC-related thrombosis is a serious complication that can lead to morbidity and mortality in this patient population. Several risk factors have been identified for the development of PICC-related thrombosis, including cancer type, stage, comorbidities, and catheter characteristics. Under
To analyze the influencing factors of PICC-related thrombosis in hospitalized patients with liver cancer, construct a predictive model, and validate it.
Clinical data of hospitalized patients with liver cancer admitted from January 2020 to December 2023 were collected. Thirty-five cases of PICC-related thrombosis in hospitalized patients with liver cancer were collected, and 220 patients who underwent PICC placement during the same period but did not develop PICC-related thrombosis were randomly selected as controls. A total of 255 samples were collected and used as the training set, and 77 cases were collected as the validation set in a 7:3 ratio. General patient information, case data, catheterization data, coagulation indicators, and Autar Thrombosis Risk Assessment Scale scores were analyzed. Univariate and multivariate unconditional logistic regression analyses were performed on relevant factors, and the value of combined indicators in predicting PICC-related thrombosis in hospitalized patients with liver cancer was evaluated using receiver operating characteristic (ROC) curve analysis.
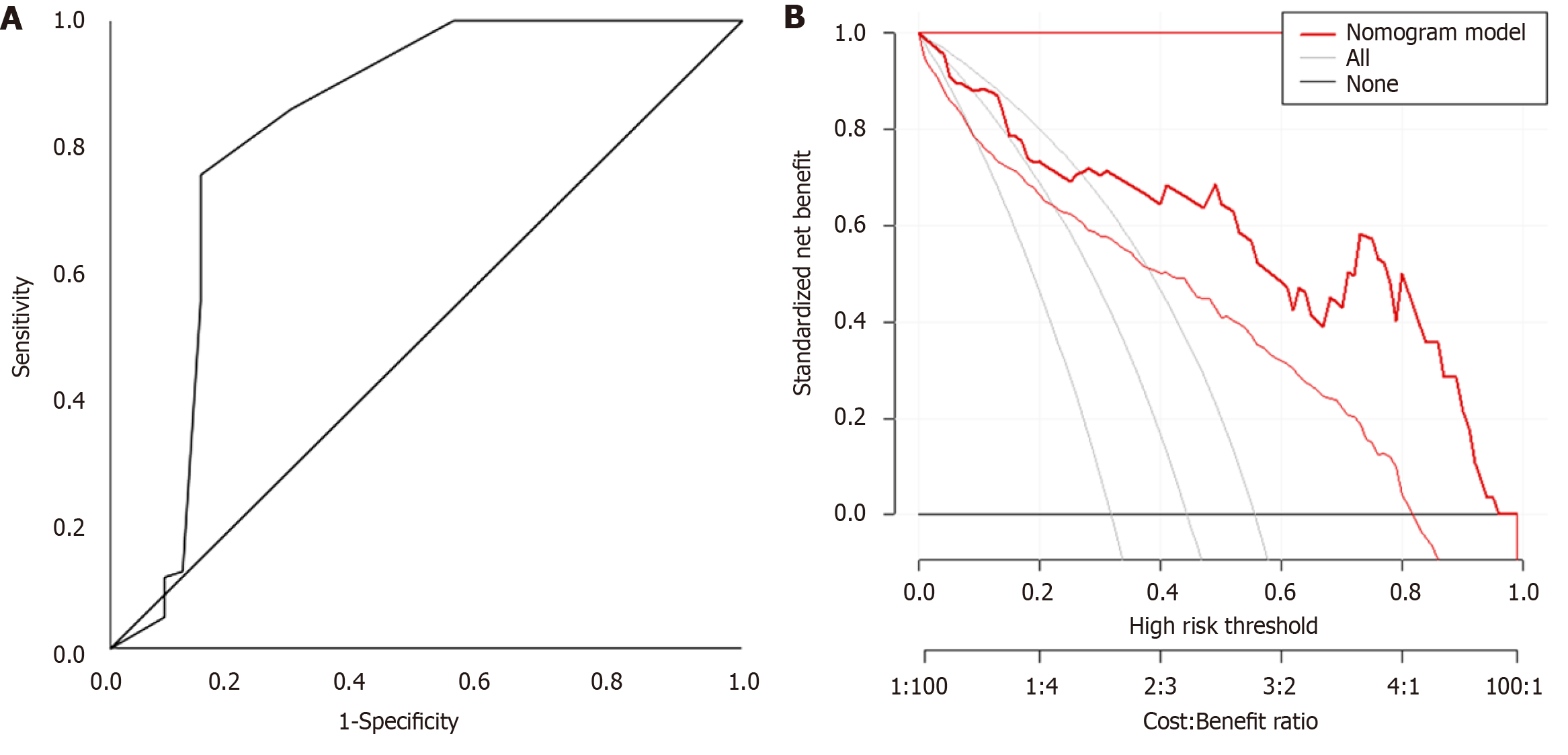
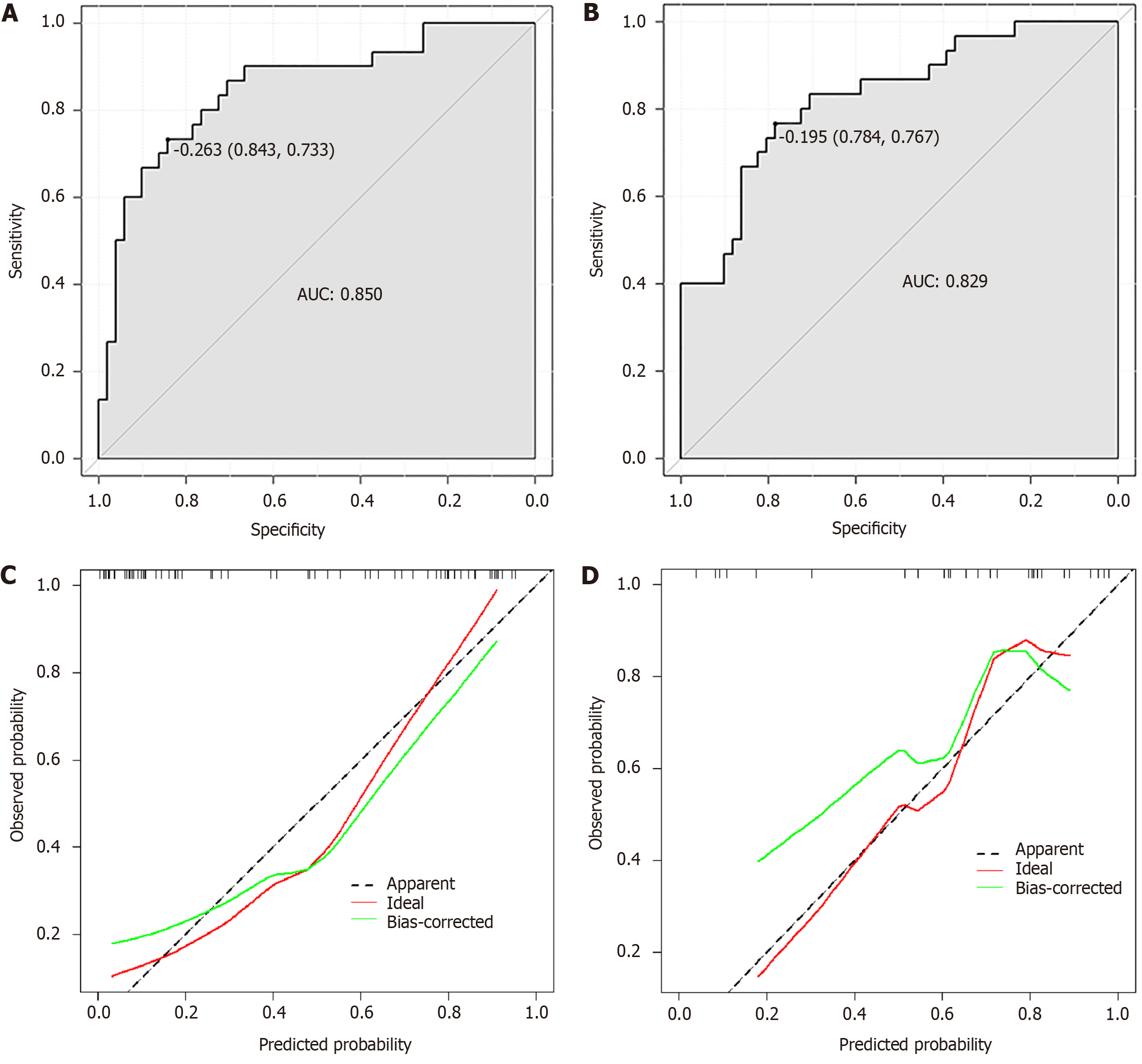
Univariate analysis showed statistically significant differences (P < 0.05) in age, sex, Karnofsky performance status score (KPS), bedridden time, activities of daily living impairment, parenteral nutrition, catheter duration, distant metastasis, and bone marrow suppression between the thrombosis group and the non-thrombosis group. Other aspects had no statistically significant differences (P > 0.05). Multivariate regression analysis showed that age ≥ 60 years, KPS score ≤ 50 points, parenteral nutrition, stage III to IV, distant metastasis, bone marrow suppression, and activities of daily living impairment were independent risk factors for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). Catheter duration of 1-6 months and catheter duration > 6 months were protective factors for PICC-related thrombosis (P < 0.05). The predictive model for PICC-related thrombosis was obtained as follows: P predictive probability = [exp (Logit P)]/[1 + exp (Logit P)], where Logit P = age × 1.907 + KPS score × 2.045 + parenteral nutrition × 9.467 + catheter duration × 0.506 + tumor-node-metastasis (TNM) staging × 2.844 + distant metastasis × 2.065 + bone marrow suppression × 2.082 + activities of daily living impairment × 13.926. ROC curve analysis showed an area under the curve (AUC) of 0.827 (95%CI: 0.724-0.929, P < 0.001), with a corresponding optimal cut-off value of 0.612, sensitivity of 0.755, and specificity of 0.857. Calibration curve analysis showed good consistency between the predicted occurrence of PICC-related thrombosis and actual occurrence (P > 0.05). ROC analysis showed AUCs of 0.888 and 0.729 for the training and validation sets, respectively.
Age, KPS score, parenteral nutrition, TNM staging, distant metastasis, bone marrow suppression, and activities of daily living impairment are independent risk factors for PICC-related thrombosis in hospitalized patients with liver cancer, while catheter duration is a protective factor for the disease. The predictive model has an AUC of 0.827, indicating high predictive accuracy and clinical value.
Core Tip: In this study, we comprehensively analyzed the influencing factors of peripherally inserted central catheters-related thrombosis in hospitalized patients with liver cancer. We constructed a predictive model to accurately predict the risk of thrombosis and validated its performance. Age, Karnofsky performance score, parenteral nutrition, tumor-node-metastasis staging, distant metastasis, bone marrow suppression, and activities of daily living impairment were identified as independent risk factors, while catheter duration was a protective factor. The predictive model demonstrated high accuracy, with an area under the curve of 0.827, indicating its potential clinical value in enhancing the quality of care for peripherally inserted central catheters patients with liver cancer.
- Citation: Chen XF, Wu HJ, Li T, Liu JB, Zhou WJ, Guo Q. Establishment and validation of a predictive model for peripherally inserted central catheter-related thrombosis in patients with liver cancer. World J Gastrointest Surg 2024; 16(7): 2221-2231
- URL: https://www.wjgnet.com/1948-9366/full/v16/i7/2221.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i7.2221
According to global cancer statistics[1], as of 2020, approximately 906000 new cases of liver cancer were reported worldwide, resulting in 830000 deaths. Characterized by its propensity for metastasis and high invasiveness, liver cancer poses significant challenges in selecting treatment strategies[2]. Given the necessity for long-term treatment in liver cancer patients, venous catheterization often emerges as the preferred clinical approach to facilitate continuous drug infusion and chemotherapy. Peripherally inserted central catheter (PICC) is commonly employed for venous catheterization and involves the insertion of a catheter into the superior vena cava through a small incision in the elbow vein[3]. Catheter-related thrombosis, wherein thrombi form in the vicinity of the catheter, can lead to severe complications, such as pulmonary embolism and superior vena cava obstruction[4]. Previous studies indicated[5] that the incidence of PICC-related thrombosis ranges from 0.47% to 50.00%, with the majority being asymptomatic covert types, while only 2% to 26% of patients exhibit evident clinical symptoms. Consequently, accurately assessing the risk of PICC-related thrombosis in hospitalized patients with liver cancer holds particular significance.
Although some studies have delved into PICC-related thrombosis in liver cancer patients, an effective predictive model for the occurrence of this condition is currently lacking. Hence, this study endeavors to analyze the influencing factors of PICC-related thrombosis in hospitalized patients with liver cancer and to formulate a precise and dependable predictive model to assist clinicians in proactively identifying high-risk patients and implementing effective preventive measures in clinical practice.
We conducted a retrospective analysis of clinical data of liver cancer patients who received treatment at Chengdu Shangjinnanfu Hospital, West China Hospital of Sichuan University from January 2020 to December 2023.
The inclusion criteria encompassed patients hospitalized with liver cancer confirmed by pathology or imaging[2]; aged 18 years and above; undergoing PICC insertion for chemotherapy during hospitalization; and capable of furnishing complete clinical data. Exclusion criteria included pregnant and lactating women; patients with hematological diseases (such as hemophilia, thrombocytopenic purpura) or undergoing anticoagulant therapy; patients with a history of thrombosis; patients with an expected hospital stay less than 3 days; and patients unable to provide comprehensive clinical data or declining participation in the study. This study was approved by the Ethics Committee of West China Hospital of Sichuan University (No. 2023-1712), and the Ethics Committee agreed to waive informed consent.
Statistical analysis requirements stipulate that the sample size for variables in the risk factor study should be at least 5 to 10 times the number of variables. Approximately 22 predictive variables were identified based on literature review on factors influencing controlled randomized trial. These variables included age, sex, education level, hypertension, smoking, Karnofsky performance status (KPS) score, bedridden time, body mass index (BMI), impairment in activities of daily living, parenteral nutrition, vascular placement, arm, lumen, thrombosis history, PICC placement history, D-dimer, catheter duration, catheter-related complications, catheter diameter, tumor-node-metastasis (TNM) staging, distant metastasis, and bone marrow suppression. The sample size (n) ranged from approximately 110 to 220 cases. Thirty-five cases of PICC-related thrombosis in hospitalized patients with liver cancer were amassed, and 220 patients who underwent PICC placement during the same period but did not develop PICC-related thrombosis were randomly selected as controls. A total of 255 samples were amassed, with 255 cases utilized as the training set and 77 cases collected anew as the validation set in a 7:3 ratio.
Study tools: General patient information included sex, age, education level. PICC catheter information included placement history, placement arm, placement vein diameter, catheter duration, other related complications of PICC catheter. Patient disease-related data included number of comorbidities (e.g., hypertension), thrombosis history, smoking history, BMI, daily bedridden time (within the past week), hematological examination indicators (D-dimer). The Autar Thrombosis Risk Assessment Scale included seven modules such as age, physique, activity level. Each module was assigned a score of 0 to 7 based on specific risk factors. The cumulative score was used to assess the risk of thrombosis: Low (7–10 points), moderate (11–14 points), or high (≥ 15 points)[6]. PICC catheter-related thrombosis occurrence was evaluated by recording the B-ultrasound diagnosis results[7].
Data collection: Data were collected by the researchers themselves at Chengdu Shangjinnanfu Hospital, West China Hospital of Sichuan University PICC Outpatient Clinic. The process included filling out forms for general patient information, basic information of PICC placement, reviewing patient disease-related data, and using the Autar thrombosis assessment scale to assess thrombosis risk. Ultrasound Doppler equipment was used to conduct vascular ultrasound examinations on patients. During the examination, patients were exposed from the waist up and laid flat on the examination bed. The limb on the side of the catheter placement was externally rotated by 90° to fully expose the vein of the limb. The thrombosis diagnostic criteria included the following[8]: Dilation of the vein lumen, visible thrombus echo within the vein lumen, inability of the vessel to deform or be compressed when pressure is applied with the probe, and blood flow signal filling defect or bypass or absence.
SPSS 27.0 software was used for analysis. In the statistical analyses, normality was tested for continuous variables using the Shapiro-Wilk test. Quantitative data were expressed as (mean ± SD) and bilateral independent sample t test analysis. Categorical data were expressed as [n (%)] and compared using χ2 tests. The receiver operating characteristic (ROC) curve was used to calculate the optimal cut-off value, sensitivity, and specificity. An area under the curve (AUC) > 0.9 indicates high predictive value, an AUC of 0.7-0.9 indicates moderate predictive value, and an AUC of 0.5-0.7 indicates low predictive value. A significance level of P < 0.05 was considered statistically significant. Variables with P < 0.05 were included in the binary logistic regression model to determine the independent risk factors for PICC-related thrombosis in hospitalized patients with liver cancer.
Among the 255 cases, 35 cases had PICC catheter-related thrombosis, with an incidence rate of 13.73%. Twenty-seven cases (77.14%) were asymptomatic thrombosis, and 8 cases (22.86%) were symptomatic thrombosis. Among the eight patients with symptomatic thrombosis, specific symptoms included pain, swelling, and numbness in the fingers, with 2 cases of pain, 5 cases of swelling, and 1 case of finger numbness.
Univariate analysis showed statistically significant differences (P < 0.05) in age, sex, KPS score, bedridden time, activities of daily living impairment, parenteral nutrition, catheter duration, distant metastasis, and bone marrow suppression between the thrombosis group and the non-thrombosis group. Statistically significant differences were not observed in other aspects (P > 0.05; Table 1).
| Variable | n | Thrombus (n = 35) | Non-thrombosis (n = 220) | Statistical value | P value |
| Age (years) | χ2 = 4.270 | 0.039 | |||
| < 60 | 150 | 15 (42.86) | 135 (61.36) | ||
| ≥ 60 | 105 | 20 (57.14) | 85 (38.64) | ||
| Sex | χ2 = 4.785 | 0.029 | |||
| Male | 159 | 16 (45.71) | 143 (65.00) | ||
| Female | 96 | 19 (54.29) | 77 (35.00) | ||
| Educational level | χ2 = 3.062 | 0.080 | |||
| Primary and below | 104 | 19 (54.29) | 85 (38.64) | ||
| Junior high school and above | 151 | 16 (45.71) | 135 (61.36) | ||
| Hypertension | χ2 = 0.632 | 0.426 | |||
| No | 154 | 19 (54.29) | 135 (61.36) | ||
| Yes | 101 | 16 (45.71) | 85 (38.64) | ||
| Smoking | χ2 = 0.520 | 0.471 | |||
| No | 146 | 22 (62.86) | 124 (56.36) | ||
| Yes | 109 | 13 (37.14) | 96 (43.64) | ||
| KPS score (points) | χ2 = 5.022 | 0.025 | |||
| ≤ 50 | 186 | 31 (88.57) | 155 (70.45) | ||
| > 50 | 69 | 4 (11.43) | 65 (29.55) | ||
| Time in bed (hour/day) | χ2 = 4.935 | 0.026 | |||
| ≤ 12 | 146 | 14 (40.00) | 132 (60.00) | ||
| > 12 | 109 | 21 (60.00) | 88 (40.00) | ||
| BMI (kg/m2) | χ2 = 0.352 | 0.553 | |||
| < 30 | 99 | 12 (34.29) | 87 (39.55) | ||
| ≥ 30 | 156 | 23 (65.71) | 133 (60.45) | ||
| Disability of self-care ability | χ2 = 10.737 | 0.001 | |||
| No | 220 | 24 (68.57) | 196 (89.09) | ||
| Yes | 35 | 11 (31.43) | 24 (10.91) | ||
| Parenteral nutrition | χ2 = 6.068 | 0.014 | |||
| No | 245 | 31 (88.57) | 214 (97.27) | ||
| Yes | 10 | 4 (11.43) | 6 (2.73) | ||
| Vascularization | χ2 = 6.149 | 0.105 | |||
| Venae magnalis | 173 | 20 (57.14) | 153 (69.55) | ||
| Brachial vein | 54 | 7 (20.00) | 47 (21.36) | ||
| Cephalic vein | 16 | 5 (14.29) | 11 (5.00) | ||
| Median vein | 12 | 3 (8.57) | 9 (4.09) | ||
| Arm | χ2 = 0.832 | 0.362 | |||
| Left arm | 142 | 17 (48.57) | 125 (56.82) | ||
| Right arm | 113 | 18 (51.43) | 95 (43.18) | ||
| Lumen | χ2 = 0.811 | 0.368 | |||
| Single lumen | 250 | 35 (100.00) | 215 (97.73) | ||
| Bicavate | 5 | 0 | 5 (2.27) | ||
| History of thrombosis | χ2 = 0.483 | 0.487 | |||
| No | 252 | 35 (100.00) | 217 (98.64) | ||
| Yes | 3 | 0 | 3 (1.36) | ||
| PICC catheterization history | χ2 = 3.029 | 0.082 | |||
| No | 246 | 32 (91.43) | 214 (97.27) | ||
| Yes | 9 | 3 (8.57) | 6 (2.73) | ||
| D-D (mg/L) | χ2 = 0.206 | 0.650 | |||
| < 30 | 111 | 14 (40.00) | 97 (44.09) | ||
| ≥ 30 | 144 | 21 (60.00) | 123 (55.91) | ||
| Tube time (month) | χ2 = 6.582 | 0.037 | |||
| < 1 | 147 | 14 (40.00) | 133 (60.45) | ||
| 1-6 | 96 | 20 (57.14) | 76 (34.55) | ||
| > 6 | 12 | 1 (2.86) | 11 (5.00) | ||
| Catheter-related complications | χ2 = 0.209 | 0.648 | |||
| No | 133 | 17 (48.57) | 116 (52.73) | ||
| Yes | 122 | 18 (51.43) | 104 (47.27) | ||
| Catheter diameter | χ2 = 0.647 | 0.421 | |||
| 4F | 251 | 35 (100.00) | 216 (98.18) | ||
| 5F | 4 | 0 | 4 (1.82) | ||
| TNM | |||||
| I-II | 133 | 11 (31.43) | 122 (55.45) | χ2 = 6.985 | 0.008 |
| III-IV | 122 | 24 (68.57) | 98 (44.55) | ||
| Distant metastasis | χ2 = 10.587 | 0.001 | |||
| No | 194 | 19 (54.29) | 175 (79.55) | ||
| Yes | 61 | 16 (45.71) | 45 (20.45) | ||
| Myelosuppression | χ2 = 10.610 | 0.001 | |||
| No | 210 | 22 (62.86) | 188 (85.45) | ||
| Yes | 45 | 13 (37.14) | 32 (14.55) |
Table 2 shows specific variable assignment details. Multivariate regression analysis showed that age ≥ 60 years, KPS score ≤ 50 points, parenteral nutrition, stage III to IV, distant metastasis, bone marrow suppression, and activities of daily living impairment were independent risk factors for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). Catheter duration was a protective factor for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05; Table 3).
| Variable | Content | Assign |
| Y | Whether blood clots | No thrombus = 0, thrombus = 1 |
| X1 | Age | < 60 = 0, ≥ 60 = 1 |
| X2 | Sex | Male = 0, female = 1 |
| X3 | KPS score | > 50 = 0, ≤ 50 = 1 |
| X4 | Time in bed | ≤ 12 hours/day = 0, > 12 hours/day = 1 |
| X5 | Parenteral nutrition | No = 0, yes = 1 |
| X6 | Tube time | < 1 = 0, 1-6 = 1, > 6 = 2 |
| X7 | TNM staging | I-II = 0, III-IV = 1 |
| X8 | Distant metastasis | No = 0, yes = 1 |
| X9 | Myelosuppression | No = 0, yes = 1 |
| X10 | Disability of self-care ability | No = 0, yes = 1 |
| Factor | B | SE | Wald χ2 | P value | OR | 95%CI |
| Constant | 11.176 | 1.675 | 44.321 | < 0.001 | 0.000 | - |
| Age ≥ 60 years | 0.644 | 0.308 | 4.342 | 0.036 | 1.907 | 1.038-3.491 |
| KPS score ≤ 50 points | 2.261 | 2.263 | 4.338 | 0.038 | 2.045 | 1.276-3.899 |
| Parenteral nutrition | 2.249 | 0.791 | 8.092 | 0.005 | 9.467 | 2.011-43.596 |
| Duration of the tube is from 1 to 6 months | -0.681 | 0.321 | 4.556 | 0.032 | 0.506 | 0.271-0.955 |
| Tube time > 6 months | -1.682 | 0.778 | 4.681 | 0.030 | 0.185 | 0.042-0.856 |
| Phase III to IV | 2.025 | 2.021 | 4.349 | 0.032 | 2.844 | 1.865-3.621 |
| Distant metastasis | 0.726 | 0.308 | 5.556 | 0.018 | 2.065 | 1.131-3.778 |
| Myelosuppression | 0.735 | 0.318 | 5.298 | 0.022 | 2.082 | 1.114-3.892 |
| Disability of self-care ability | 2.633 | 1.086 | 5.899 | 0.016 | 13.926 | 1.661-116.254 |
Significant data from the baseline were included in the binary logistic regression analysis to obtain predictive model for PICC-related thrombosis in hospitalized patients with liver cancer: P predictive probability = [exp (Logit P)]/[1 + exp (Logit P)], where Logit P = age × 1.907 + KPS score × 2.045 + parenteral nutrition × 9.467 + catheter duration × 0.506 + TNM staging × 2.844 + distant metastasis × 2.065 + bone marrow suppression × 2.082 + activities of daily living impairment × 13.926. The relationship between the P predictive probability obtained from patients and thrombosis was used to construct the ROC curve, with an AUC of 0.827 (95%CI: 0.724–0.929, P < 0.001), corresponding to the optimal cut-off value of 0.612, sensitivity of 0.755, and specificity of 0.857 (Figure 1A). Calibration curve analysis showed good consistency between the predicted occurrence of PICC-related thrombosis and actual occurrence in the validation set (P > 0.05; Figure 1B). ROC analysis results showed AUCs of 0.888 and 0.729 for the training and validation sets, respectively (Table 4, Figure 2).
| Index | AUC | Sensitivity (%) | Specificity (%) | 95%CI | P value |
| Training set | 0.888 | 90.76 | 87.77 | 0.851-0.965 | < 0.001 |
| Validation set | 0.729 | 87.89 | 85.45 | 0.822-0.942 | < 0.001 |
Among 255 cases, 35 had PICC catheter-related thrombosis, with an incidence rate of 13.73%. These findings are consistent with previous relevant reports[9]. This study found that symptomatic thrombosis in patients mainly presented as pain, swelling, and numbness in the fingers, with 2 cases of pain, 5 cases of swelling, and 1 case of finger numbness. In clinical practice, patient complaints should be highly regarded, especially for those who only present with symptoms of venous inflammation. Local treatment alone should not be applied, and the existence of thrombotic risk should not be overlooked. Instead, the cause should be promptly investigated, and a diagnosis should be made based on relevant examinations to ensure the safe use of catheters.
This study found that age ≥ 60 years is an independent risk factor for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). As age increases, endothelial cells release more procoagulant factors, so blood is more prone to coagulation; a hypercoagulable state is one of the risk factors for thrombosis formation. Shi et al[10] also showed that age > 60 years is a major risk factor for thrombosis formation in Chinese PICC chemotherapy patients. Therefore, the occurrence of thrombosis should be given attention in elderly patients after PICC catheter insertion. Patients should be taught to identify abnormal conditions in the limb with the catheter, seek medical attention promptly if abnormalities occur, be encouraged to drink water to reduce blood viscosity, and perform appropriate active and passive limb exercises daily to promote blood circulation and reduce the risk of thrombosis.
The KPS score is an important indicator used to assess the effectiveness of tumor treatment and the functional status of patients[11]. A higher score indicates better physical condition and functional ability. This study found that a KPS score ≤ 50 points is an independent risk factor for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). Patients with a KPS score below 50 have poorer physical condition and are more prone to muscle atrophy, metabolic abnormalities, and blood circulation disorders, leading to slower blood flow, endothelial cell damage, and increased platelet activity, making thrombosis more likely to occur[12]. Moreover, patients with low KPS scores may require prolonged use of PICC, thereby increasing the risk of thrombosis. Therefore, effective preventive and treatment measures should be taken to reduce the incidence of thrombosis in patients with KPS score ≤ 50 points.
This study found that parenteral nutrition is an independent risk factor for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). Parenteral nutrition is often used for tumor patients who cannot eat or have insufficient food intake and for those who experience adverse reactions such as vomiting, diarrhea, leading to malnutrition. These patients often have hypovolemia, and the infusion of high-concentration nutrients will further increase blood viscosity[13]. Increased blood viscosity slows blood flow and increases the risk of thrombosis formation. Therefore, close monitoring of patients' blood viscosity and thrombosis risk is required during parenteral nutrition therapy for tumor patients. Corresponding measures, such as appropriately diluting parenteral nutrition solution and implementing thrombosis prevention measures (such as anticoagulation therapy), should be implemented to reduce the risk of thrombosis-related events[14].
Stage III-IV liver cancer represents the advanced stage of liver cancer development and is associated with severe conditions and poor physical status; patients in this stage are susceptible to various factors, including the risk of thrombosis formation[15]. This study found that stage III-IV liver cancer is an independent risk factor for PICC-related thrombosis in hospitalized patients with liver cancer. Patients with stage III-IV liver cancer often have impaired liver function, poor blood circulation, abnormal platelet and coagulation factor levels, and liver cancer itself, which may affect the function of endothelial cells and increase the risk of thrombosis formation[16]. Additionally, patients with stage III-IV liver cancer typically require longer periods of PICC insertion, prolonging endothelial cell damage and thrombosis formation, which is also a significant contributing factor to thrombosis occurrence[17]. Therefore, enhanced thrombosis risk assessment and prevention measures, including anticoagulant therapy and regular PICC catheter replacement, are necessary for patients with stage III-IV liver cancer undergoing PICC treatment. Moreover, active disease control and improvement of patient physical status during liver cancer treatment are essential to reduce the risk of PICC-related thrombosis.
Distant metastasis is an independent risk factor for PICC-related thrombosis in hospitalized patients with liver cancer
Bone marrow suppression is an independent risk factor for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). This condition refers to a decrease or inhibition of hematopoietic stem cell function in the bone marrow, leading to dysfunctions in the blood and immune systems[20]. In patients with liver cancer, bone marrow suppression may be caused by factors such as liver function failure and tumor infiltration into the bone marrow[21]. Bone marrow suppression leads to a decrease in platelet count and impaired coagulation function in patients with liver cancer, thereby increasing the risk of thrombosis formation[22].
Impaired activities of daily living are independent risk factors (P < 0.05). In patients with liver cancer, impaired activities of daily living may result from disease progression, liver function failure, adverse reactions to treatment, and other factors. Impaired activities of daily living may lead to prolonged bed rest and reduced mobility, thereby increasing the risk of blood stasis and thrombosis formation[23]. The characteristics of the PICC catheter itself may also increase the risk of thrombosis in patients with impaired activities of daily living. For example, the use of PICC catheters may limit the patient’s range of motion, slow blood circulation, and further increase the risk of thrombosis formation. Therefore, when treating hospitalized patients with liver cancer who have impaired activities of daily living with PICC catheters, necessary rehabilitation care and support should be provided as much as possible to promote patient mobility and reduce the risk of blood stasis and thrombosis formation.
The duration of catheterization is a protective factor for PICC-related thrombosis in hospitalized patients with liver cancer (P < 0.05). The occurrence of PICC-related thrombosis is mostly concentrated in the early stages of catheterization. After catheterization, patients undergo chemotherapy, during which a large number of tumor cells die, releasing a large amount of active substances, leading to the hypercoagulable state of the blood. Additionally, catheterization causes varying degrees of endothelial damage, which promotes platelet aggregation. Moreover, patients in the early stages of catheterization may reduce the activity of the cathetered limb due to lack of knowledge and fear of adverse effects on the catheter, thereby increasing the risk of thrombosis occurrence[24,25]. Therefore, after catheterization, patient education should be strengthened, appropriate levels and frequencies of activity should be advised to alleviate psychological pressure and reduce risk factors for thrombosis formation.
Based on the relationship between the predicted probability (P) obtained from patients and thrombosis, an ROC curve was constructed, with an AUC of 0.827 (95%CI: 0.724–0.929, P < 0.001), corresponding to an optimal cut-off value of 0.612, sensitivity of 0.755, and specificity of 0.857. Hence, the predictive model has high accuracy and reliability in identifying PICC-related thrombosis in hospitalized patients with liver cancer.
In summary, age, KPS score, parenteral nutrition, TNM stage, distant metastasis, bone marrow suppression, and impaired activities of daily living are independent risk factors for PICC-related thrombosis in hospitalized patients with liver cancer, while the duration of catheterization is a protective factor. Moreover, the predictive model has an AUC of 0.827, indicating high predictive accuracy and clinical value. Most thromboses in patients are asymptomatic, so patients should undergo regular vascular ultrasound examinations during catheterization, especially for patients with high-risk factors. Patient complaints should be given attention, and patient education should be strengthened. However, this study was only a cross-sectional survey; hence, further large-scale prospective studies are needed to clarify risk factors for prevention and early identification of PICC-related thrombosis.
| 1. | Singal AG, Sanduzzi-Zamparelli M, Nahon P, Ronot M, Hoshida Y, Rich N, Reig M, Vilgrain V, Marrero J, Llovet JM, Parikh ND, Villanueva A. International Liver Cancer Association (ILCA) white paper on hepatocellular carcinoma risk stratification and surveillance. J Hepatol. 2023;79:226-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 46] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 2. | Modest DP, Karthaus M, Kasper S, Moosmann N, Keitel V, Kiani A, Uhlig J, Jacobasch L, Fischer V Weikersthal L, Fuchs M, Kaiser F, Lerchenmüller C, Sent D, Junghanß C, Held S, Lorenzen S, Kaczirek K, Jung A, Stintzing S, Heinemann V. FOLFOX plus panitumumab or FOLFOX alone as additive therapy following R0/1 resection of RAS wild-type colorectal cancer liver metastases - The PARLIM trial (AIO KRK 0314). Eur J Cancer. 2022;173:297-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 3. | Huang Q, Chen L, Aiqun J, Shi F, Feng D. Effectiveness of the Hospital-Community-Family Nursing Model in Breast Cancer Patients Discharged with PICC Lines. J Community Health Nurs. 2023;40:255-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Itkin M, Mondshein JI, Stavropoulos SW, Shlansky-Goldberg RD, Soulen MC, Trerotola SO. Peripherally inserted central catheter thrombosis--reverse tapered versus nontapered catheters: a randomized controlled study. J Vasc Interv Radiol. 2014;25:85-91.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Fallouh N, McGuirk HM, Flanders SA, Chopra V. Peripherally Inserted Central Catheter-associated Deep Vein Thrombosis: A Narrative Review. Am J Med. 2015;128:722-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 6. | Autar R. Nursing assessment of clients at risk of deep vein thrombosis (DVT): the Autar DVT scale. J Adv Nurs. 1996;23:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Shi YQ, Liu L, Li N, Luo GX, Li HS. [Research advances on venous thromboembolism in burn patients]. Zhonghua Shao Shang Yu Chuang Mian Xiu Fu Za Zhi. 2023;39:264-268. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Xu B, Geng CZ, Lu ZQ. Safety guidelines for vascular pathways in tumor therapy. Beijing: China Union Medical College Press, 2015: 135. |
| 9. | Mariggiò E, Iori AP, Micozzi A, Chistolini A, Latagliata R, Berneschi P, Giampaoletti M, La Rocca U, Bruzzese A, Barberi W, Foà R, Morano SG. Peripherally inserted central catheters in allogeneic hematopoietic stem cell transplant recipients. Support Care Cancer. 2020;28:4193-4199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Shi Y, Wen L, Zhou Y, Tao S. Thrombotic risk factors in patients undergoing chemotherapy via peripherally inserted central catheter. J Int Med Res. 2014;42:863-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Tsien CI, Pugh SL, Dicker AP, Raizer JJ, Matuszak MM, Lallana EC, Huang J, Algan O, Deb N, Portelance L, Villano JL, Hamm JT, Oh KS, Ali AN, Kim MM, Lindhorst SM, Mehta MP. NRG Oncology/RTOG1205: A Randomized Phase II Trial of Concurrent Bevacizumab and Reirradiation Versus Bevacizumab Alone as Treatment for Recurrent Glioblastoma. J Clin Oncol. 2023;41:1285-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 108] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 12. | Ma S, Shen C, Li Q, Yang H, Hu Y, Wei X, Liang T. Clinical factors of PICC-RVT in cancer patients: a meta-analysis. Support Care Cancer. 2023;31:393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Koizumi Y, Hiraoka A, Michitaka K, Tazuya N, Ichiryu M, Nakahara H, Ochi H, Tanabe A, Hidaka S, Kodama A, Uehara T, Hasebe A, Miyamoto Y, Ninomiya T, Kumagi T, Abe M, Matsuura B, Horiike N, Hiasa Y, Onji M. Severe hypoglycemia associated with insulin-like growth factor II-producing liver metastasis from gastric carcinoma treated with overnight total parenteral nutrition via a central vein catheter reserve port. Clin J Gastroenterol. 2011;4:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Chakedis J, Schmidt CR. Surgical Treatment of Metastatic Colorectal Cancer. Surg Oncol Clin N Am. 2018;27:377-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Komatsu S, Kido M, Kuramitsu K, Tsugawa D, Gon H, Fukushima K, Urade T, Yanagimoto H, Toyama H, Fukumoto T. Impact of Hepatectomy for Advanced Hepatocellular Carcinoma with Major Portal Vein Tumor Thrombus. J Gastrointest Surg. 2022;26:822-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Yu J, Zhuang L, Liu P, Liu Z, Ling S, Deng Y, Li J, Yang B, Chen Z, Wang Z, Zang Y, Yang Y, Zheng S, Xu X. Long-term outcomes of deceased donor liver transplantation in hepatocellular carcinoma patients with portal vein tumor thrombus: A multicenter study. Eur J Surg Oncol. 2022;48:121-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Lv JY, Zhang NN, Du YW, Wu Y, Song TQ, Zhang YM, Qu Y, Liu YX, Gu J, Wang ZY, Qiu YB, Yang B, Tian DZ, Guo QJ, Zhang L, Sun JS, Xie Y, Wang ZL, Sun X, Jiang WT, Lu W. Comparison of Liver Transplantation and Liver Resection for Hepatocellular Carcinoma Patients with Portal Vein Tumor Thrombus Type I and Type II. Yonsei Med J. 2021;62:29-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | E Y, Sun S, Fan X, Lu C, Ji P, Huang Y, Sun J, Yang X, Yu C. Prediction of liver and lung metastases in patients with early-onset colorectal cancer by nomograms based on heterogeneous and homogenous risk factors. Cancer Med. 2023;12:20712-20726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Bing S, Smotherman C, Rodriguez RG, Skarupa DJ, Ra JH, Crandall ML. PICC versus midlines: Comparison of peripherally inserted central catheters and midline catheters with respect to incidence of thromboembolic and infectious complications. Am J Surg. 2022;223:983-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Sicart CSVA, Luz RPC, Rizzi SKLA, Nazário ACP, Facina G, Elias S. Effect of acupuncture in myelosuppression and quality of life in women with breast cancer undergoing chemotherapy: a randomized clinical study. Support Care Cancer. 2023;31:156. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Björn N, Jakobsen Falk I, Vergote I, Gréen H. ABCB1 Variation Affects Myelosuppression, Progression-free Survival and Overall Survival in Paclitaxel/Carboplatin-treated Ovarian Cancer Patients. Basic Clin Pharmacol Toxicol. 2018;123:277-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Hazarika M, Rock E, Williams G, Dagher R, Sridhara R, Booth B, Farrell A, Justice R, Pazdur R. Lenalidomide in combination with dexamethasone for the treatment of multiple myeloma after one prior therapy. Oncologist. 2008;13:1120-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Zhang X, Zhang D, Yu P, Li X. Effects of Continuous Care Combined with Evidence-Based Nursing on Mental Status and Quality of Life and Self-Care Ability in Patients with Liver from Breast Cancer: A Single-Center Randomized Controlled Study. Comput Math Methods Med. 2022;2022:3637792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 24. | Zhao XN, Wang YT. [An analysis of the factors affecting the treatment of peripheral inserted central catheter associated upper extremity deep vein thrombosis in elderly patients]. Zhongguo Ying Yong Sheng Li Xue Za Zhi. 2016;32:124-127. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Sousou T, Khorana AA. Cancer patients and awareness of venous thromboembolism. Cancer Invest. 2010;28:44-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |