Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.503
Peer-review started: November 27, 2023
First decision: December 29, 2023
Revised: January 6, 2024
Accepted: February 5, 2024
Article in press: February 5, 2024
Published online: February 27, 2024
Processing time: 90 Days and 12.1 Hours
Although en bloc dissection of hepatic hilum lymph nodes has many advantages in radical tumor treatment, the feasibility and safety of this approach for laparoscopic pancreaticoduodenectomy (LPD) require further clinical evaluation and investigation.
To explore the application value of the "five steps four quadrants" modularized en bloc dissection technique for accessing hepatic hilum lymph nodes in LPD patients.
A total of 52 patients who underwent LPD via the "five steps four quadrants" modularized en bloc dissection technique for hepatic hilum lymph nodes from April 2021 to July 2023 in our department were analyzed retrospectively. The patients' body mass index (BMI), preoperative laboratory indices, intraoperative variables and postoperative complications were recorded. The relationships between preoperative data and intraoperative lymph node dissection time and blood loss were also analyzed.
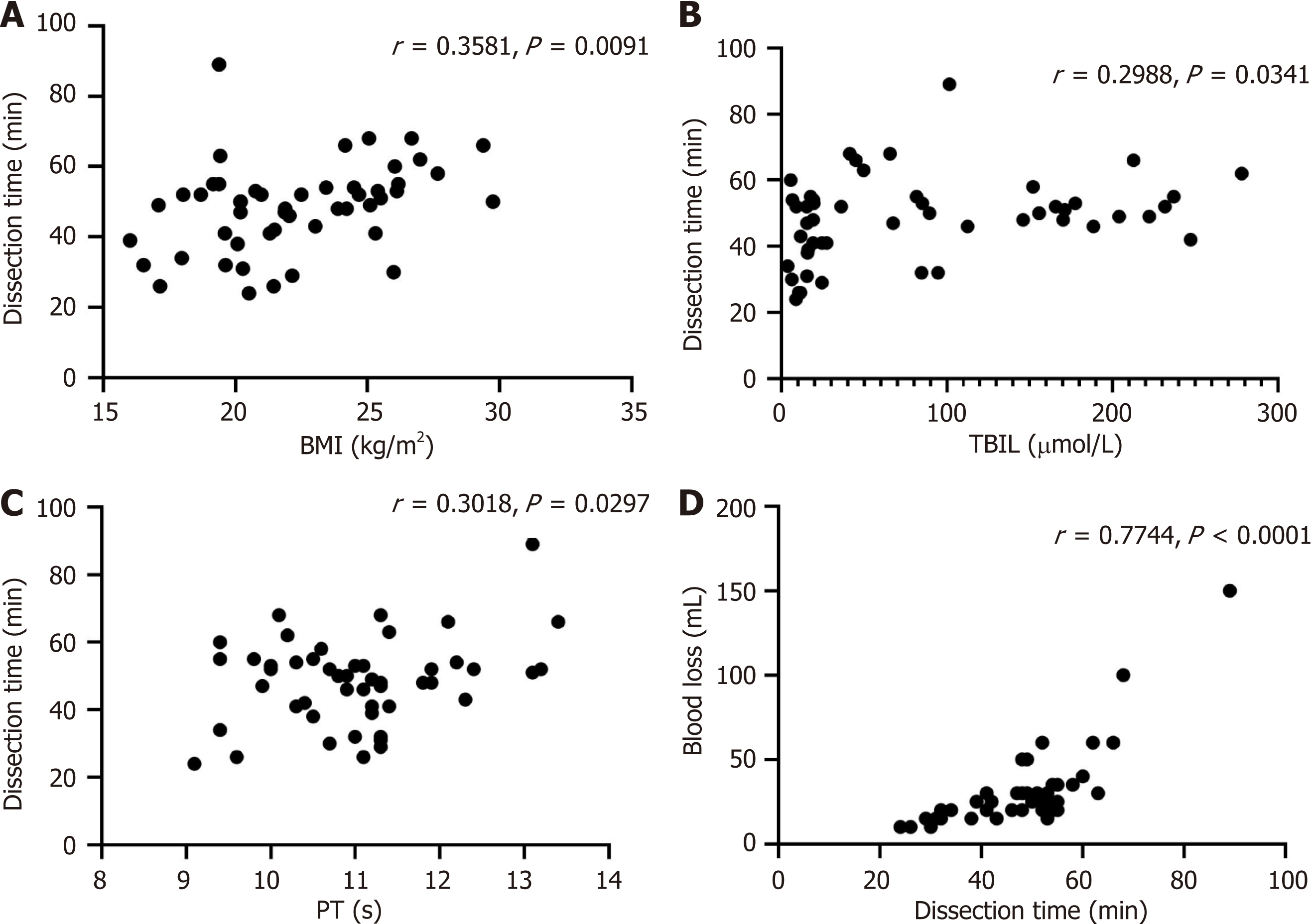
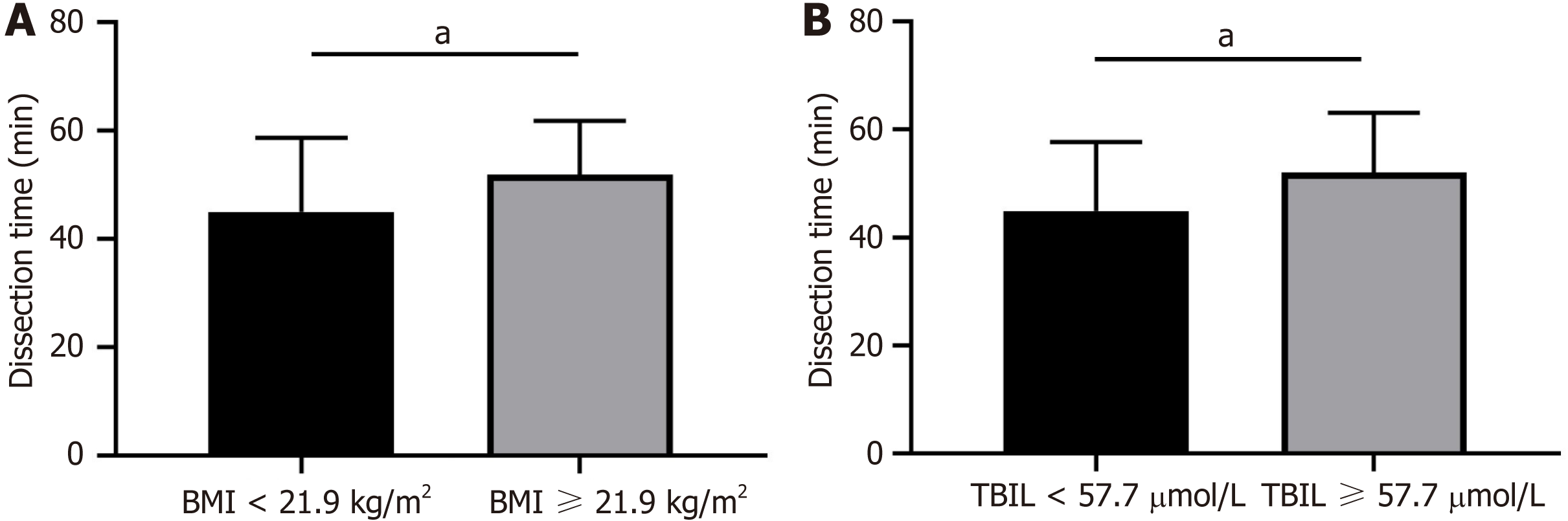
Among the 52 patients, 36 were males and 16 were females, and the average age was 62.2 ± 11.0 years. There were 26 patients with pancreatic head cancer, 16 patients with periampullary cancer, and 10 patients with distal bile duct cancer. The BMI was 22.3 ± 3.3 kg/m², and the median total bilirubin (TBIL) concentration was 57.7 (16.0-155.7) µmol/L. All patients successfully underwent the "five steps four quadrants" modularized en bloc dissection technique without lymph node clearance-related complications such as postoperative bleeding or lymphatic leakage. Correlation analysis revealed significant associations between preoperative BMI (r = 0.3581, P = 0.0091), TBIL level (r = 0.2988, P = 0.0341), prothrombin time (r = 0.3018, P = 0.0297) and lymph node dissection time. Moreover, dissection time was significantly correlated with intraoperative blood loss (r = 0.7744, P < 0.0001). Further stratified analysis demonstrated that patients with a preoperative BMI ≥ 21.9 kg/m² and a TIBL concentration ≥ 57.7 μmol/L had significantly longer lymph node dissection times (both P < 0.05).
The "five steps four quadrants" modularized en bloc dissection technique for accessing the hepatic hilum lymph node is safe and feasible for LPD. This technique is expected to improve the efficiency of hepatic hilum lymph node dissection and shorten the learning curve; thus, it is worthy of further clinical promotion and application.
Core Tip: Although en bloc dissection of hepatic hilum lymph nodes has many advantages, the feasibility and safety of this approach for laparoscopic pancreaticoduodenectomy (LPD) requires further clinical investigation. We showed that the emerging technique of "five steps four quadrants" modularized en bloc dissection of hepatic hilum lymph nodes is safe and feasible for LPD. In this technique, a preoperative elevated body mass index, total bilirubin concentration, and prothrombin time increase the difficulty of lymph node dissection. This approach is expected to improve the efficiency of hepatic hilum lymph node dissection and shorten the learning curve; thus, this technique is worthy of further clinical promotion and application.
- Citation: Hu XS, Wang Y, Pan HT, Zhu C, Chen SL, Liu HC, Pang Q, Jin H. "Five steps four quadrants" modularized en bloc dissection technique for accessing hepatic hilum lymph nodes in laparoscopic pancreaticoduodenectomy. World J Gastrointest Surg 2024; 16(2): 503-510
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/503.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.503
In recent years, with the advancements in surgical techniques and the renewal of treatment concepts, en bloc resection has been widely regarded as a radical treatment for several malignant tumors, such as cholangiocarcinoma, periampullary carcinoma and pancreatic head cancer[1-3]. En bloc resection usually includes resection of the tumor and dissection of the regional lymph node and surrounding tissues. En bloc dissection of the hepatic hilum lymph node refers to the dissection of the lymph node and neuroconnective tissues along the vascular axis [usually the common hepatic artery (CHA) and portal vein (PV)] during radical surgery and the en bloc removal of the lymph node and surrounding connective tissues around the vessel[4]. Compared with traditional selective dissection, this technique can thoroughly remove potential lymph nodes and micrometastases and increase the R0 resection rate[5,6]. Although en bloc dissection of hepatic hilum lymph nodes has many advantages in radical tumor treatment, the feasibility and safety of this approach for laparoscopic pancreaticoduodenectomy (LPD) require further clinical evaluation and investigation. In recent years, based on long-term clinical practice, our center has summarized the "five steps four quadrants" approach for modular hepatic hilum lymph node dissection, which has been successfully applied during LPD surgery and initially shown satisfactory clinical efficacy. In this study, we summarize the relevant data as follows.
The clinical and surgical data of patients who underwent LPD in our department between April 2021 and July 2023 were retrospectively analyzed. The inclusion criteria were as follows: (1) ≥ 18 years of age; (2) diagnosed with periampullary carcinoma, distal bile duct carcinoma, or pancreatic head carcinoma preoperatively, and LPD was performed with the technique of "five steps four quadrants" modular hepatic hilum lymph node dissection; (3) Eastern Cooperative Oncology Group score 0-2; (4) without other malignancies; and (5) without a history of supreme abdominal surgery.
This study was performed in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Second People's Hospital of Anhui Province (approval number: 2022-011). Written informed consent was obtained from the patients preoperatively.
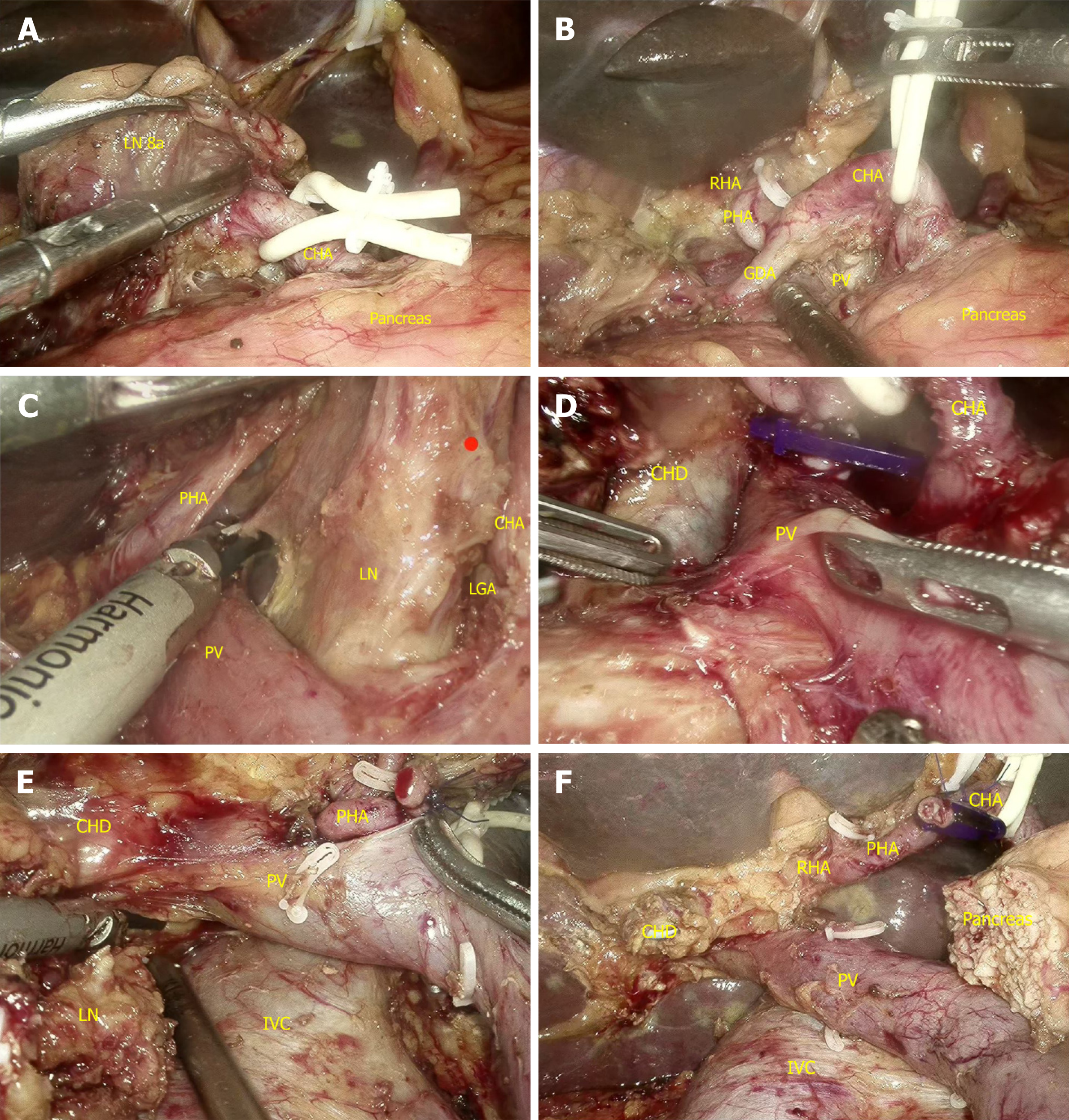
Kocher incision separation was performed routinely, and the jejunum was severed after the resectability of the tumor was determined (it should be noted that the inferior vena cava should be fully separated from the rear of the hepatic portal during Kocher incision separation to facilitate dissection of the hepatic hilum region after the operation). Furthermore, the stomach was severed, the hepatic hilum region was exposed, and the "five steps four quadrants" modularized en bloc dissection technique (Figure 1) was implemented as follows:
Step 1: The No. 8a lymph node was separated from the upper margin of the pancreas, after which the CHA was exposed and suspended, after which the inferior PV was exposed. Subsequently, the hepatic hilum region was bounded by the hepatic artery (HA)/PV axis and divided into four zones: upper, lower, left and right zones (Figure 1A).
Step 2: As shown in Figure 1B, Dissection of the upper zone of the HA/PV axis. The upper zone was separated toward the hepatic hilum along the 12-point position of the HA and PV surfaces, and the No. 12a and 8p lymph nodes and surrounding tissues were pushed to the left and right zones but were not severed by using the combination of blunt and sharp dissection. Then, the full course of the HA/PV axis was exposed, and the left and right hepatic arteries were also exposed [the right gastric artery (RGA) or gastroduodenal artery (GDA) could be automatically lapped and severed provided that the operation was significantly affected].
Step 3: As shown in Figure 1C, Dissection of the left zone of the HA/PV axis. First, the lower left zone was separated toward the abdominal trunk along the HA/PV axis. The No. 9 lymph node and surrounding tissues were dissected, above which the No. 7 lymph node and surrounding tissues were further dissected through the left gastric artery. Then, the upper left and left zones of the HA/PV axis were dissected successively in a counterclockwise direction until the left edge of the PV was completely exposed. The dissected tissues in the left zone were pushed behind the PV. The surgeon should focus on the anatomical variation, injury and bleeding of the left gastric vein (LGV). The LGV should be disconnected if it empties into the PV.
Step 4: As shown in Figure 1D, Dissection of the right zone of the HA/PV axis. The GDA was severed after it was determined that there was no variation in the right hepatic artery (RHA). The No. 12b lymph node and surrounding tissues in the right zone of the HA/PV axis were pushed to the middle and distal bile duct using the combination of blunt and sharp dissection until the right margin of the PV was completely exposed. Then, the RGA was severed, and the gallbladder was removed. The hepatic duct was separated for subsequent dissection from the upper margin of the confluence with the gallbladder duct.
Step 5: As shown in Figure 1E, Dissection of the lower zone of the HA/PV axis. The pancreatic neck and uncinate process were successively severed, and the PV was subsequently separated from the No. 12p lymph node and surrounding tissues behind the PV. Subsequently, from the right rear side, the above dissected tissues in the left zone and the dissected tissues in the rear zone of the HA/PV axis were pulled out below the PV. The posterosuperior tissues in the right zone were separated from the hepatic hilum and finally attached to the common hepatic duct. The surrounding tissues of the inferior common hepatic duct were severed, the common hepatic duct was severed, and en bloc dissection of the hepatic hilum region was completed (Figure 1F).
Sex, age, body mass index (BMI), preoperative total bilirubin (TBIL), albumin (ALB), prothrombin time (PT), platelet count (PLT), carbohydrate antigen 19-9 (CA19-9), carcinoembryonic antigen (CEA), carbohydrate antigen 125 (CA125) and other laboratory indices were collected. Intraoperative lymph node dissection time, blood loss, postoperative blood loss, lymphatic leakage and other related complications were also analyzed. The correlations between preoperative data and intraoperative dissection time and blood loss were also analyzed.
SPSS 25.0 statistical software was used to process and analyze the data. Continuous variables are expressed as the mean ± SD or median (interquartile range) and were compared by using the t test or Wilcoxon test. Categorical data are expressed as frequencies and were compared by using the χ2 test or Fisher's exact probability method. Pearson correlation analysis was performed to assess the correlation between two variables. P < 0.05 was considered to indicate statistical significance.
A total of 52 patients were included, all of whom underwent LPD via the technique of "five steps four quadrants" modular hepatic hilum lymph node dissection. All the operations were performed by the same team. Among them, 36 were males and 16 were females. The mean age of the patients was 62.2 ± 11.0 years, the mean BMI was 22.3 ± 3.3 kg/m2, and the median TIBL concentration was 57.7 (16.0-155.7) µmol/L. Twenty-six lesions were located in the pancreatic head, 16 were in the periampulla, and 10 were in the distal bile duct. The median lymph node dissection time, dissection number, and intraoperative blood loss were 50 (41-54) min, 6 (6-7), and 25.0 (20.0-33.8) mL, respectively. The baseline information of the patients is shown in Table 1.
| Variables | Value |
| Gender: Male/female | 36/16 |
| Age (yr) | 62.2 ± 11.0 |
| BMI (kg/m2) | 22.3 ± 3.3 |
| Tumor site: Pancreatic head/periampulla/distal biliary duct | 26/16/10 |
| TBIL (µmol/L) | 57.7 (16.0-155.7) |
| Preoperative biliary drainage: Yes/no | 6/46 |
| ALB (g/L) | 37.2 (34.7-39.2) |
| PT (s) | 11.1 (10.3-11.4) |
| PLT (109/L) | 209 (163.5-261.8) |
| CA19-9 (U/mL) | 59.9 (13.3-391.6) |
| CEA (ng/mL) | 2.0 (1.1-3.8) |
| CA125 (U/mL) | 9.8 (6.1-15.8) |
| Lymph node dissection time (min) | 50 (41-54) |
| Number of lymph node dissection | 6 (6-7) |
| Number of positive lymph node: 0/1/2/3 | 40/8/3/1 |
| Intraoperative blood loss (mL) | 25.0 (20.0-33.8) |
The correlation analysis showed that preoperative BMI (r = 0.3581, P = 0.0091), TIBL level (r = 0.2988, P = 0.0341) and PT (r = 0.3018, P = 0.0297) were significantly associated with intraoperative lymph node dissection time (Figure 2). In addition, the lymph node dissection time was significantly correlated with intraoperative blood loss (Figure 2D; r = 0.7744, P < 0.0001).
Further stratification according to BMI showed that patients with a preoperative BMI ≥ 21.9 kg/m2 had significantly longer lymph node dissection times than did those with a BMI < 21.9 kg/m2 (Figure 3A; 51.92 ± 9.94 vs 45.00 ± 13.73 min, t = 2.082, P = 0.042). Stratified analysis according to TBIL showed that patients with preoperative TBIL ≥ 57.5 μmol/L had significantly longer lymph node dissection times than did those with TBIL < 57.5 μmol/L (Figure 3B; 52.04 ± 11.03 vs 44.88 ± 12.81 min, t = 2.158, P = 0.036).
None of the patients had postoperative complications caused by lymph node dissection, such as postoperative blood transfusion or long-term catheter catheterization caused by hemorrhage and lymphatic leakage.
In recent years, with the continuous improvement of minimally invasive technology and the widespread popularization of minimally invasive approaches, LPD has been promoted and applied in an increasing number of centers. However, it remains difficult to grasp surgical quality control[7-9]. An increasing number of scholars are concerned about how to streamline and modularize the complex process of LPD to achieve homogeneity of curative effects. Hilar lymph node dissection is a key procedure in the surgical process of LPD[10,11]. Traditionally, according to the anatomical distribution, we locally locate and remove lymph node tissues in batches. However, due to the diverse distributions of lymph nodes in the hepatic hilum, there may be anatomical variation and incomplete dissection of lymph node tissues during surgery, which can affect the treatment efficacy of surgery[12].
En bloc resection of hepatic hilum lymph nodes is a relatively new technique that has been used in radical surgery for periampullary carcinoma, cholangiocarcinoma, and pancreatic head carcinoma in recent years. In this technique, en bloc dissection is used to remove lymph node tissues from the hepatic hilum region as a whole to ensure thoroughness of the lymph node dissection. Studies have shown that, compared with traditional methods, en bloc dissection of regional lymph nodes improves the number, integrity and efficiency of lymph node dissection and thus increases the radical resection rate[6,13]. However, en bloc hepatic hilum lymph node dissection also increases the difficulty and risk of surgery and has high surgical requirements.
On the basis of long-term clinical practice, we used the "five steps four quadrants" technique for en bloc resection of the hepatic hilar region. This technique started with the isolation of the No. 8a lymph node[14]. Then, according to the boundary of the HA/PV axis, the hepatic hilum region was divided into four zones: upper, lower, left and right. The four zones were dissected separately, and the en bloc was removed. The technique follows the concept of "simplification of complex problems and modularization of simple problems", thus allowing the dissection of hepatic hilum lymph node tissues more smoothly and thoroughly. Compared with traditional methods, the "five steps four quadrants" technique can be used to dissect lymph node tissues more completely. In addition, this technique avoids residual lymph nodes, increases the number of dissected lymph nodes, and thus improves the effectiveness of radical resection. Moreover, the concept of this technology is simple and easy to master. This technology is expected to shorten the learning curve and has potential value for popularization and application.
The results of the present study showed that, via the use of "five steps four quadrants", the median number of dissected lymph nodes was six, which meets the standards required by experts and guidelines[15-18]. Moreover, this technique significantly improved lymph node dissection and allowed more thorough dissection of lymph node tissues in the hepatic hilum region. However, the postoperative pathological results suggested that the proportion of patients with positive lymph nodes was relatively low (23.1%, 12/52). However, long-term, multicenter studies with larger sample sizes are needed to explore whether these methods could improve patient prognosis. Furthermore, the median lymph node dissection and intraoperative blood loss were 50 min and 25 mL, respectively, indicating that proficiency in this technique can improve surgical efficiency and control intraoperative risk. Our study further showed that higher BMI, TBIL and PT may increase the difficulty of lymph node dissection. Therefore, to improve surgical confidence, beginners can select appropriate cases according to the three indicators. Due to the complete removal and thorough dissection of lymph nodes, none of the patients in this study experienced postoperative complications such as blood transfusion or long-term catheter implantation, which further confirmed the safety of this technique.
Although this study showed that the application of the "five steps four quadrants" technique in LPD patients is safe and effective, there are still some limitations. First, this was a single-center study with a relatively small sample size, which may have led to selection bias and statistical bias. Second, the effect of this technique on postoperative survival and recurrence could not be assessed due to the short follow-up time. Third, as surgical videos of previous patients without the implementation of the ''five steps four quadrants'' modularized en bloc dissection technique were missing, the control group was absent from this study. Therefore, multicenter, large-sample randomized controlled studies are needed to further verify the superiority of this technique. In addition, as a new surgical technique, "five steps four quadrants" still need to be further perfected and optimized. In clinical practice, this technique may be affected by complex anatomic variations, tumor invasion, preoperative biliary drainage, and other factors. In this study, there were 3 patients with relatively significant intraoperative blood loss. Further analysis of surgical video data showed that all of them had accidental tears of PV variant branches. Therefore, this technology requires that surgeons and assistants have a wealth of surgical experience. A more accurate preoperative evaluation is also necessary. The operating specifications and training system of this technology should be further improved in the future to ensure the stability and replicability of the technical path.
In general, the "five steps four quadrants" modularized en bloc dissection technique for hepatic hilum lymph nodes is safe and feasible for LPD. This method is expected to improve the efficiency of hepatic hilum lymph node dissection and shorten the learning curve and thus is worthy of further clinical promotion and application.
Although the en-bloc dissection of hepatic hilum lymph node shows many advantages in the radical treatment of several malignant tumors such as cholangiocarcinoma, periampullary carcinoma and pancreatic head cancer, the feasibility and safety of which for laparoscopic pancreaticoduodenectomy (LPD) require further clinical evaluation and investigation.
The motivation behind this article is to provide the emerging and valuable technique of the "five steps four quadrants" modularized en-bloc dissection in the field of hepatic hilum lymph node dissection of LPD.
The objective of this study is to explore the application value of the "five steps four quadrants" modularized en-bloc dissection technique for accessing hepatic hilum lymph nodes in LPD patients.
A total of 52 patients who underwent LPD with the technique of "five steps four quadrants" modularized en-bloc dissection technique of hepatic hilum lymph node from April 2021 to July 2023 in our department were analyzed retro
There were 26 cases of pancreatic head cancer, 16 cases of periampullary cancer, and 10 cases of distal bile duct cancer. All patients successfully underwent the "five steps four quadrants" modularized en-bloc dissection technique without lymph node clearance-related complications such as postoperative bleeding or lymphatic leakage. Correlation analysis revealed significant associations between preoperative body mass index (BMI, r = 0.3581, P = 0.0091), total bilirubin (TBIL, r = 0.2988, P = 0.0341), prothrombin time (r = 0.3018, P = 0.0297) and lymph node dissection time. Moreover, dissection time was significantly correlated with intraoperative blood loss (r = 0.7744, P < 0.0001). Further stratified analysis demonstrated that patients with preoperative BMI ≥ 21.9 kg/m² and TBIL ≥ 57.7 μmol/L had significantly longer lymph node dissection time (both P < 0.05).
In general, the "five steps four quadrants" modularized en bloc dissection technique for hepatic hilum lymph nodes is safe and feasible for LPD.
This method is expected to improve the efficiency of hepatic hilum lymph node dissection and shorten the learning curve and thus is worthy of further clinical promotion and application.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stepanyan SA, Armenia S-Editor: Yan JP L-Editor: A P-Editor: ZhangYL
| 1. | Bednarsch J, Czigany Z, Lurje I, Tacke F, Strnad P, Ulmer TF, Gaisa NT, Bruners P, Neumann UP, Lurje G. Left- versus right-sided hepatectomy with hilar en-bloc resection in perihilar cholangiocarcinoma. HPB (Oxford). 2020;22:437-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Tsiotos GG, Ballian N, Michelakos T, Milas F, Ziogou P, Papaioannou D, Salla C, Athanasiadis I, Razis E, Stavridi F, Psomas M. Portal-Mesenteric Vein Resection in Borderline Pancreatic Cancer; 33 Month-Survival in Patients with Good Performance Status. J Pancreat Cancer. 2019;5:43-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Nakamura T, Okada KI, Ohtsuka M, Higuchi R, Takahashi H, Nagai K, Unno M, Murakami Y, Oba A, Tomikawa M, Kato A, Horiguchi A, Nakamura M, Yagi S, Satoi S, Endo I, Amano R, Matsumoto I, Ito YM, Nagakawa T, Hirano S. Insights from managing clinical issues in distal pancreatectomy with en bloc coeliac axis resection: experiences from 626 patients. Br J Surg. 2023;110:1387-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 4. | Li J, Zhou MH, Ma WJ, Li FY, Deng YL. Extended lymphadenectomy in hilar cholangiocarcinoma: What it will bring? World J Gastroenterol. 2020;26:3318-3325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (36)] |
| 5. | Kang MJ, Kim SW. En bloc proximal peri-mesenteric clearance for pancreatic head cancer surgery. Ann Hepatobiliary Pancreat Surg. 2020;24:389-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Cheng J, Liu J, Dou CW, Xie ZC, Fan BF, Jin LM, Liang L, Zhang CW. Standardized lymph node dissection for gallbladder cancer under laparoscopy: en-bloc resection technique. Langenbecks Arch Surg. 2023;408:183. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Wang M, Peng B, Liu J, Yin X, Tan Z, Liu R, Hong D, Zhao W, Wu H, Chen R, Li D, Huang H, Miao Y, Liu Y, Liang T, Wang W, Cai Y, Xing Z, Cheng W, Zhong X, Zhao Z, Zhang J, Yang Z, Li G, Shao Y, Lin G, Jiang K, Wu P, Jia B, Ma T, Jiang C, Peng S, Qin R. Practice Patterns and Perioperative Outcomes of Laparoscopic Pancreaticoduodenectomy in China: A Retrospective Multicenter Analysis of 1029 Patients. Ann Surg. 2021;273:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 110] [Article Influence: 27.5] [Reference Citation Analysis (1)] |
| 8. | Wu Y, Peng B, Liu J, Yin X, Tan Z, Liu R, Hong D, Zhao W, Wu H, Chen R, Li D, Huang H, Miao Y, Liu Y, Liang T, Wang W, Yuan J, Li S, Zhang H, Wang M, Qin R; Minimally Invasive Treatment Group in the Pancreatic DiseaseBranch of China’s International Exchange and Promotion Association for Medicine and Healthcare (MITG-P-CPAM). Textbook outcome as a composite outcome measure in laparoscopic pancreaticoduodenectomy: a multicenter retrospective cohort study. Int J Surg. 2023;109:374-382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Qin R, Kendrick ML, Wolfgang CL, Edil BH, Palanivelu C, Parks RW, Yang Y, He J, Zhang T, Mou Y, Yu X, Peng B, Senthilnathan P, Han HS, Lee JH, Unno M, Damink SWMO, Bansal VK, Chow P, Cheung TT, Choi N, Tien YW, Wang C, Fok M, Cai X, Zou S, Peng S, Zhao Y. International expert consensus on laparoscopic pancreaticoduodenectomy. Hepatobiliary Surg Nutr. 2020;9:464-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 10. | Wennerblom J, Saksena P, Jönsson C, Thune A. Lymph node 8a as a prognostic marker for poorer prognosis in pancreatic and periampullary carcinoma. Scand J Gastroenterol. 2018;53:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Shen Z, Wu X, Huang F, Chen G, Liu Y, Yu Z, Zhu C, Tan Z, Zhong X. Management of the Uncinate Process in No-Touch Laparoscopic Pancreaticoduodenectomy. J Vis Exp. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Mantel HT, Wiggers JK, Verheij J, Doff JJ, Sieders E, van Gulik TM, Gouw AS, Porte RJ. Lymph Node Micrometastases are Associated with Worse Survival in Patients with Otherwise Node-Negative Hilar Cholangiocarcinoma. Ann Surg Oncol. 2015;22 Suppl 3:S1107-S1115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Chun YS, Pawlik TM, Vauthey JN. 8th Edition of the AJCC Cancer Staging Manual: Pancreas and Hepatobiliary Cancers. Ann Surg Oncol. 2018;25:845-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 543] [Article Influence: 67.9] [Reference Citation Analysis (0)] |
| 14. | Tang R, Li A, Zhang X, Yu L, Yang S, Han D, Dong J, Lu Q. Suprapancreatic-approach fixed dissection of common hepatic artery for surgery. Zhongguo Shiyong Waike Zazhi. 2018;38:1414-1417. |
| 15. | Giuliante F, Ardito F, Guglielmi A, Aldrighetti L, Ferrero A, Calise F, Giulini SM, Jovine E, Breccia C, De Rose AM, Pinna AD, Nuzzo G. Association of Lymph Node Status With Survival in Patients After Liver Resection for Hilar Cholangiocarcinoma in an Italian Multicenter Analysis. JAMA Surg. 2016;151:916-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 16. | Mao K, Liu J, Sun J, Zhang J, Chen J, Pawlik TM, Jacobs LK, Xiao Z, Wang J. Patterns and prognostic value of lymph node dissection for resected perihilar cholangiocarcinoma. J Gastroenterol Hepatol. 2016;31:417-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Health Commission of The People's Republic of China N. National guidelines for diagnosis and treatment of pancreatic cancer 2022 in China (English version). Chin J Cancer Res. 2022;34:238-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 18. | Terasaki F, Sugiura T, Okamura Y, Ashida R, Ohgi K, Yamada M, Ohtsuka S, Uesaka K. Benefit of lymph node dissection for perihilar and distal cholangiocarcinoma according to lymph node stations. J Hepatobiliary Pancreat Sci. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |