Published online Dec 27, 2024. doi: 10.4240/wjgs.v16.i12.3862
Revised: September 19, 2024
Accepted: October 18, 2024
Published online: December 27, 2024
Processing time: 203 Days and 1.4 Hours
Mucosal adenocarcinoma of the descending duodenum is a very rare gastroin
A 61-year-old woman who was hospitalized with recurrent abdominal pain for more than 20 days. The patient developed epigastric pain with no obvious cause more than 20 days prior, mainly left epigastric pain and middle epigastric pain, and presented persistent dull pain without nausea or vomiting, fever or chills. The patient was treated at a local hospital, gastroscopy revealed a new lesion in the circum-intestinal cavity in the descending part of the duodenum, and pathological biopsy revealed mucous adenocarcinoma in the descending part of the duode
Mucosal adenocarcinoma of the descending duodenum has a high misdiagnosis rate and missed diagnosis rate, clinical manifestations lack specificity, and pathological diagnosis is the main basis for diagnosis.
Core Tip: The pathological diagnosis and clinical features of a rare case of descending duodenal mucosa adenocarcinoma were analyzed. Through detailed pathological examination, we confirmed the histological type of the tumor, combined with the patient’s clinical manifestations, imaging findings and treatment response, and comprehensively analyzed the pathogenesis, progression and prognosis of the case. The research focuses on revealing the diagnostic difficulties and treatment challenges of such rare tumors, aiming to provide references for clinicians and improve the level of diagnosis and treatment of similar cases.
- Citation: Zhang JY, Wu LS, Yan J, Jiang Q, Li XQ. Pathological diagnosis and clinical feature analysis of descending duodenal mucosal adenocarcinoma: A case report. World J Gastrointest Surg 2024; 16(12): 3862-3869
- URL: https://www.wjgnet.com/1948-9366/full/v16/i12/3862.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i12.3862
Mucosal adenocarcinoma of the descending duodenum is a rare malignant tumor of the digestive system, and its incidence is low; therefore, it is often neglected in clinical and pathological studies[1-3]. At present, the pathological features, clinical manifestations and treatment strategies are not completely clear. The diagnosis of this rare patient is often challenging because of its lack of clinical specificity, and this patient can easily be misdiagnosed or missed[4]. Given the relatively limited number of reports of this case, it is particularly important to study the pathological features and clinical manifestations of this rare tumor[5-7].
Through detailed pathological analysis and clinical evaluation of a patient with descending duodenal mucosal adenocarcinoma, this study comprehensively elucidated the characteristics of the disease and defined its diagnosis and treatment strategy. We will focus on the pathological features of the disease, including histological morphology, immunohistochemical expression and molecular biological features, to provide a more reliable basis for its diagnosis[8-10]. At the same time, we will conduct a comprehensive analysis of the clinical manifestations of the patients, including symptoms, signs, imaging and laboratory examination results, to explore the clinical characteristics and diagnostic difficulties of the disease[11]. Through the in-depth study of this case, we hope to provide clinicians with a more comprehensive and accurate diagnostic basis and a more effective treatment strategy. It is highly important to improve the diagnosis and treatment of rare diseases and improve the prognosis of patients[12]. Through in-depth study of this rare disease, we can also better understand its pathogenesis and tumor biological characteristics and provide new ideas and directions for future disease treatment and research. Through detailed analysis of the pathological features and clinical manifestations of descending duodenal mucosal adenocarcinoma, this study comprehensively elucidated the characteristics of this disease, clarified its diagnosis and treatment strategies, and provided a more accurate diagnostic basis and treatment plan for clinical treatment to improve the prognosis and quality of life of patients.
There was recurrent abdominal pain for more than 20 days.
The patient developed epigastric pain with no obvious cause more than 20 days ago, mainly in the left epigastric and middle epigastric pain, presenting persistent dull pain, no nausea, no fever, chills, no yellow all over the body, dark urine color, black stool and other discomfort. The patient was treated in a local hospital, and gastroscopic biopsy revealed mucous adenocarcinoma of the descending part of the duodenum. Currently, the patient is seeking further treatment at our hospital. The outpatient department plans to admit “malignant tumor of the duodenum” for surgical treatment.
The patient had a history of hypertension, regular oral antihypertensive medication treatment, and well-controlled blood pressure.
Nothing special.
There was upper abdominal tenderness; no rebound pain or muscle tension; no obvious mass in the abdomen; no liver, spleen or subcostal region; Murphy’s sign (-); and no hepatic buckle pain (-).
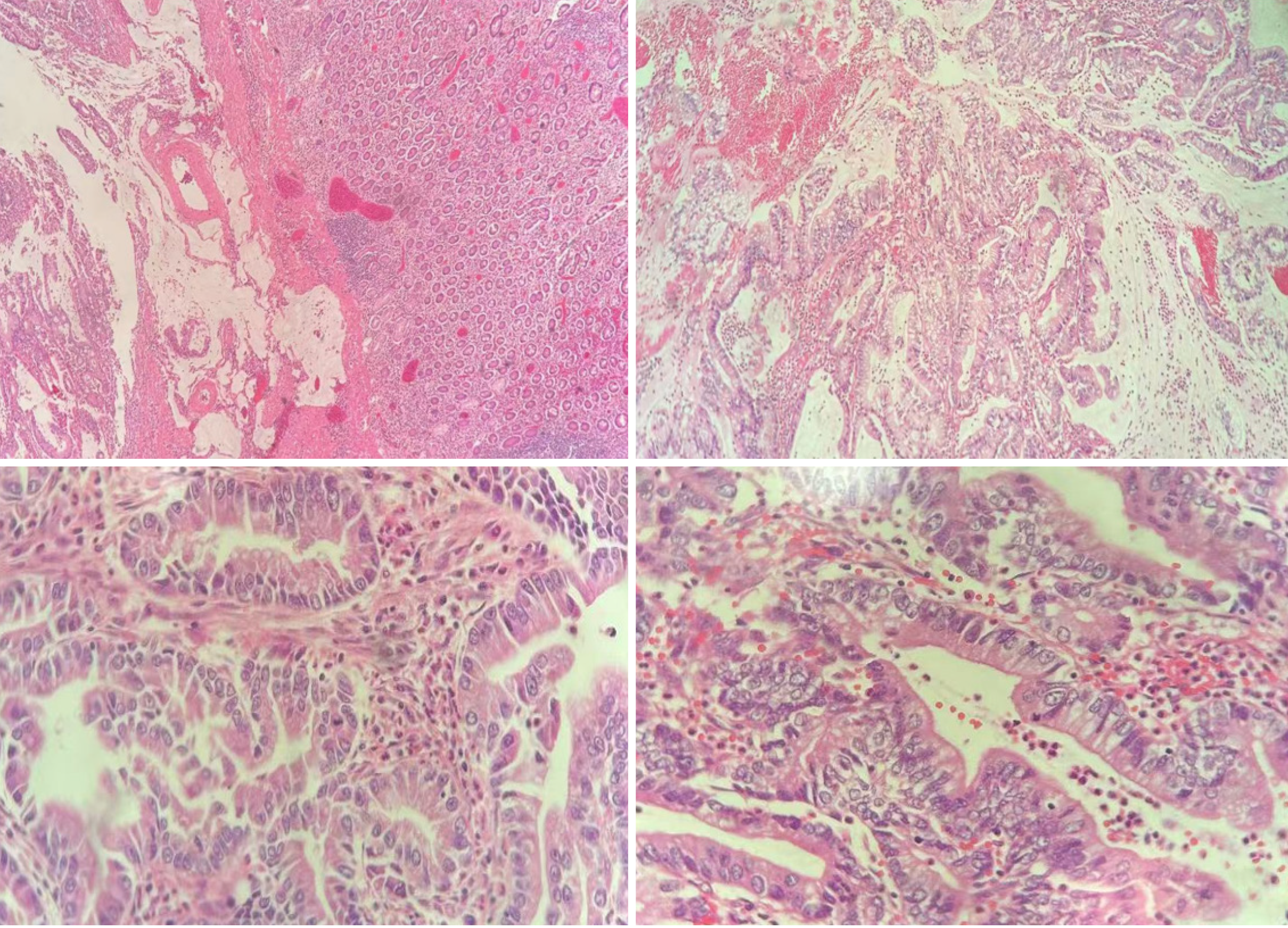
Histology revealed that the tumor cells exhibited a glandular tubular structure, abnormal enlargement of the nucleus, and nuclear division. Hematoxylin and eosin staining revealed deep staining of cell nuclei and uneven superficial staining of the cytoplasm. Immunohistochemical staining revealed that CK20 and CDX2 were positively expressed in tumor tissues, while CK7, CK19, carcinoembryonic antigen (CEA), carbohydrate antigen (CA) 19-9 and other markers were weakly or negatively expressed. In addition, the Ki-67 index was high, indicating that the tumor had strong proliferative activity. Combining the pathological features and immunohistochemical results, we concluded that the patient was diagnosed with adenocarcinoma of the descending duodenum mucosa. These features help to further understand the biological characteristics of this rare tumor and provide important guidance for its clinical diagnosis and treatment (Figure 1).
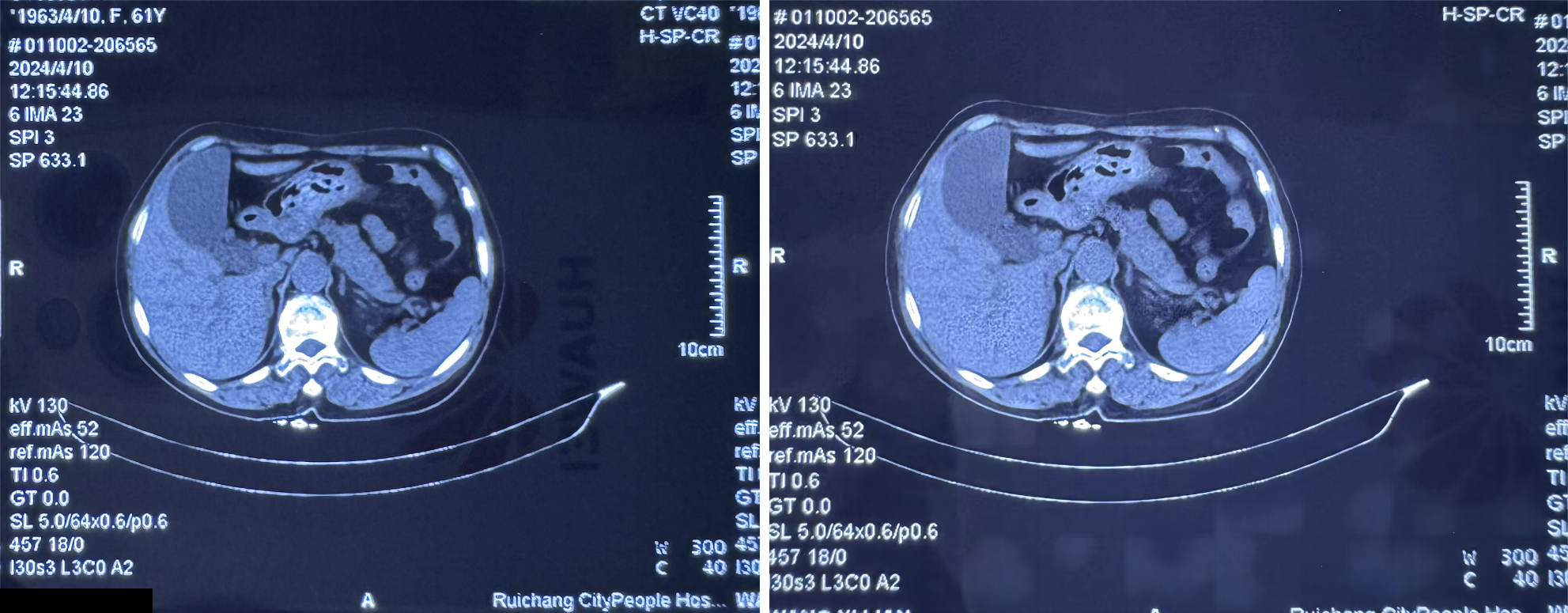
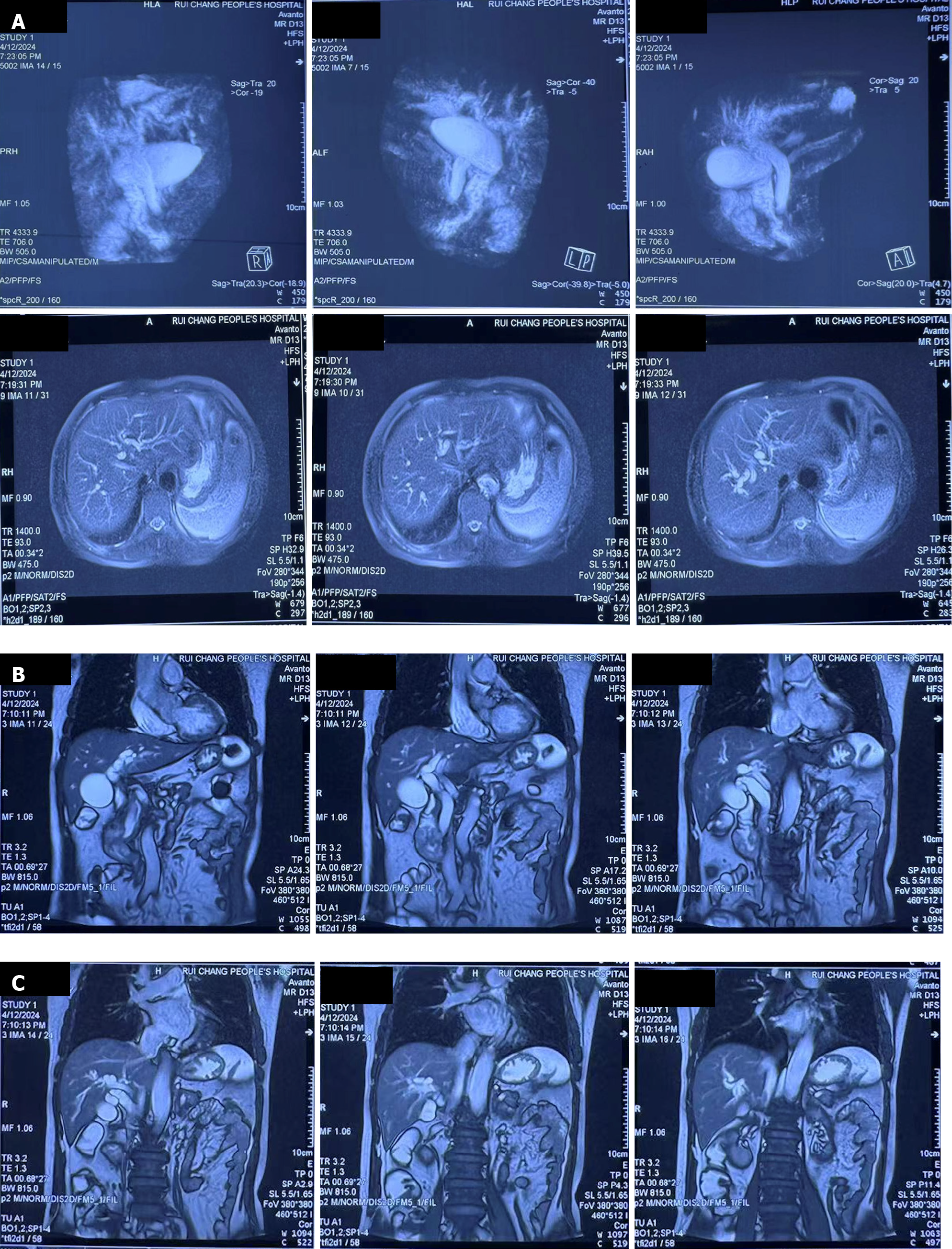
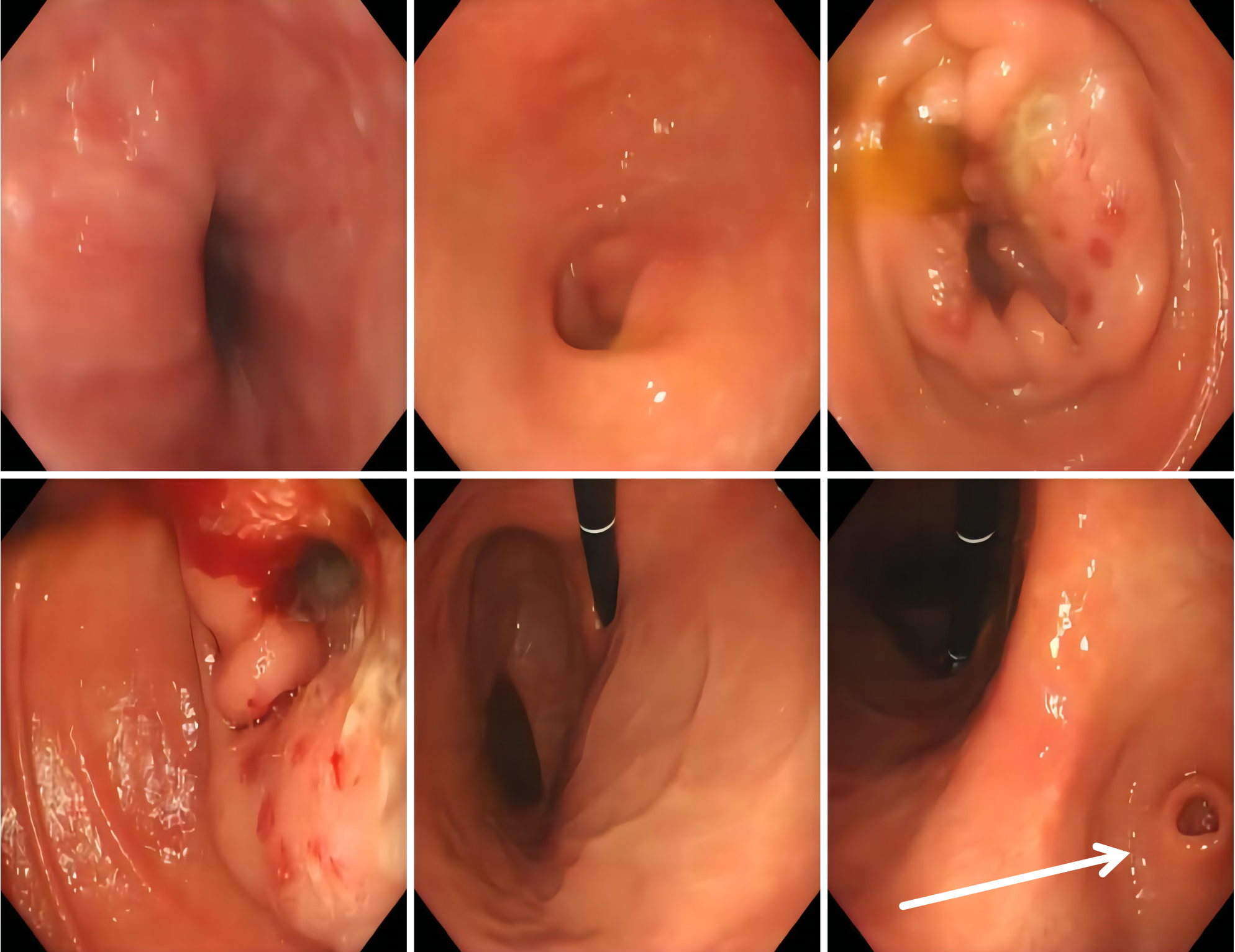
Abdominal computed tomography examination revealed that the intestinal wall was slightly thickened at the junction of the descending and horizontal parts of the duodenum, and the surrounding fat space was slightly blurred (Figure 2). Abdominal magnetic resonance imaging revealed that the intestinal wall of the descending duodenum was significantly thickened and that the signal was abnormal and tended to indicate neoplastic lesions; additionally, medical examination revealed secondary intrahepatic and external bile duct dilatation, hyperdilatation of the gallbladder, and slight dilatation of the pancreatic duct (Figure 3). Electronic proctoscopy revealed that new organisms were growing in the descending part of the duodenum, and the biopsy elasticity was poor (Figure 4).
The pathological diagnosis was descending duodenal mucosal adenocarcinoma.
We recommend that patients continue to receive treatment after surgery and undergo regular follow-up observations.
The patient recovered after the operation, and no recurrence was found after 3 months.
Mucosal adenocarcinoma of the descending part of the duodenum is a rare malignant tumor of the digestive system, and its pathological features are somewhat heterogeneous compared with those of other digestive system tumors[13-15]. In this study, we observed that the histological morphology of the tumor showed a glandular tubular structure, increased nuclear atypia, and obvious mitotic features. These features are similar to those of other adenocarcinomas of the digestive system but also have their own characteristics[16]. We noted that the clinical manifestations of this patient lacked specificity, and this patient was easily misdiagnosed or missed. This is similar to the clinical manifestations of other intestinal tumors, including abdominal pain, indigestion, and weight loss. Therefore, clinicians should be vigilant in the face of such cases, combined with clinical manifestations, imaging examination, and timely pathological examination, to make a clear diagnosis[17-19].
In terms of diagnosis, we emphasized the importance of pathological diagnosis in this disease. Immunohistochemical staining revealed positive expression of CK20 and CDX2, while the expression of CK7, CK19, CEA, CA19-9 and other markers was weak or negative, which helped to rule out the possibility of other tumors and further confirmed the diagnosis of mucosal adenocarcinoma in the descending part of the duodenum[20-22]. Because this patient had a certain degree of invasion and metastasis, active treatment was needed. Surgical resection is the preferred treatment, but for advanced cases, chemoradiotherapy is also necessary[23]. In addition, we emphasize the importance of a comprehensive treatment strategy, including a combination of surgery, chemoradiotherapy, and targeted therapy, to improve treatment outcomes and patient survival[24].
In terms of clinical features, we observed a lack of specificity in the symptoms of this patient, including abdominal pain, indigestion, weight loss, etc., which are similar to those of other intestinal tumors and can easily lead to misdiagnosis or missed diagnosis. Epidemiologically, adenocarcinoma of the descending duodenum is a rare disease with a low incidence and has rarely become the focus of clinical and pathological studies[25-27]. Pathological analysis revealed that the tumor tissue of this patient presented a glandular tubular structure, increased nuclear atypia, and obvious mitosis, similar to other digestive system adenocarcinomas but also had its own characteristics. In terms of immunohistochemistry, positive CK20 and CDX2 expression was detected, while weak or negative CK7, CK19, CEA, and CA19-9 expression was detected, which helped to further clarify the diagnosis. Because this patient had a certain degree of invasion and metastasis, active treatment measures were taken[28]. Surgical resection is the preferred treatment, but for advanced cases, chemoradiotherapy is also necessary. The importance of comprehensive treatment strategies, including surgery, chemoradiotherapy and targeted therapy, has been highlighted to improve the therapeutic efficacy and survival rate of patients.
This study is highly important for further understanding the pathological features and clinical manifestations of rare adenocarcinomas of the descending duodenum mucosa. Through pathological analysis, clinical evaluation and discussion of treatment strategies, we provide clinicians with more accurate diagnosis and treatment options to improve patient prognosis and quality of life.
| 1. | Abbass R, Rigaux J, Al-Kawas FH. Nonampullary duodenal polyps: characteristics and endoscopic management. Gastrointest Endosc. 2010;71:754-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Matsumoto S, Yoshida Y. Selection of appropriate endoscopic therapies for duodenal tumors: an open-label study, single-center experience. World J Gastroenterol. 2014;20:8624-8630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Goldner B, Stabile BE. Duodenal adenocarcinoma: why the extreme rarity of duodenal bulb primary tumors? Am Surg. 2014;80:956-959. [PubMed] |
| 4. | Nakayama A, Kato M, Masunaga T, Kubosawa Y, Hayashi Y, Mizutani M, Kiguchi Y, Sasaki M, Takatori Y, Matsuura N, Mutaguchi M, Takabayashi K, Yahagi N. Differential diagnosis of superficial duodenal epithelial tumor and non-neoplastic lesion in duodenum by magnified endoscopic examination with image-enhanced endoscopy. J Gastroenterol. 2022;57:164-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Wu L, Zheng Y, Liu J, Luo R, Wu D, Xu P, Wu D, Li X. Comprehensive evaluation of the efficacy and safety of LPV/r drugs in the treatment of SARS and MERS to provide potential treatment options for COVID-19. Aging (Albany NY). 2021;13:10833-10852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 6. | Wu L, Zhong Y, Wu D, Xu P, Ruan X, Yan J, Liu J, Li X. Immunomodulatory Factor TIM3 of Cytolytic Active Genes Affected the Survival and Prognosis of Lung Adenocarcinoma Patients by Multi-Omics Analysis. Biomedicines. 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 62] [Reference Citation Analysis (0)] |
| 7. | Iwamuro M, Tanaka T, Okada H. Review of lymphoma in the duodenum: An update of diagnosis and management. World J Gastroenterol. 2023;29:1852-1862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 8. | Beger HG, Mayer B, Poch B. Duodenum-Preserving Pancreatic Head Resection for Benign and Premalignant Tumors-a Systematic Review and Meta-analysis of Surgery-Associated Morbidity. J Gastrointest Surg. 2023;27:2611-2627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Hayashi H, Miyamoto H, Nakagawa S, Matsuno K, Miyata T, Tsukamoto M, Mima K, Nitta H, Tanaka Y, Baba H. Distinct approaches (antecolic and retrocolic) according to tumor location in laparoscopic and endoscopic cooperative surgery for non-ampullary duodenum tumors. Surg Endosc. 2023;37:6718-6726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 10. | Wu L, Liu Q, Ruan X, Luan X, Zhong Y, Liu J, Yan J, Li X. Multiple Omics Analysis of the Role of RBM10 Gene Instability in Immune Regulation and Drug Sensitivity in Patients with Lung Adenocarcinoma (LUAD). Biomedicines. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 55] [Reference Citation Analysis (0)] |
| 11. | Zeng Y, Yao H, Jiang X, Tang X, Wang X. GLI1-altered Mesenchymal Tumor Involving the Duodenum: Case Report and Literature Review. Int J Surg Pathol. 2023;31:1538-1547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Wu L, Zheng Y, Ruan X, Wu D, Xu P, Liu J, Wu D, Li X. Long-chain noncoding ribonucleic acids affect the survival and prognosis of patients with esophageal adenocarcinoma through the autophagy pathway: construction of a prognostic model. Anticancer Drugs. 2022;33:e590-e603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 70] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 13. | Milione M, Parente P, Grillo F, Zamboni G, Mastracci L, Capella C, Fassan M, Vanoli A. Neuroendocrine neoplasms of the duodenum, ampullary region, jejunum and ileum. Pathologica. 2021;113:12-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Okano K, Oshima M, Suto H, Ando Y, Asano E, Kamada H, Kobara H, Masaki T, Suzuki Y. Ampullary carcinoma of the duodenum: current clinical issues and genomic overview. Surg Today. 2022;52:189-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Del Toro C, Cabrera-Aguirre A, Casillas J, Ivanovic A, Scortegagna E, Estanga I, Alessandrino F. Imaging spectrum of non-neoplastic and neoplastic conditions of the duodenum: a pictorial review. Abdom Radiol (NY). 2023;48:2237-2257. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Wu L, Zhong Y, Yu X, Wu D, Xu P, Lv L, Ruan X, Liu Q, Feng Y, Liu J, Li X. Selective poly adenylation predicts the efficacy of immunotherapy in patients with lung adenocarcinoma by multiple omics research. Anticancer Drugs. 2022;33:943-959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 66] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 17. | Osama MA, Dhawan S, Khetan M, Rawat KS. Inflammatory myofibroblastic tumor of colon and duodenum: Metachronous, metastatic or local recurrence? An unusual presentation. J Cancer Res Ther. 2023;19:S917-S920. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Beger HG, Mayer B, Poch B. Resection of the duodenum causes long-term endocrine and exocrine dysfunction after Whipple procedure for benign tumors - Results of a systematic review and meta-analysis. HPB (Oxford). 2020;22:809-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Wu L, Li H, Liu Y, Fan Z, Xu J, Li N, Qian X, Lin Z, Li X, Yan J. Research progress of 3D-bioprinted functional pancreas and in vitro tumor models. Int J Bioprinting. 2024;10:1256. [DOI] [Full Text] |
| 20. | Chaparro Mirete M, López-López V, Robles Campos R. Lymphoepithelioma-like carcinoma of the duodenum: a very infrequent tumor. Rev Esp Enferm Dig. 2020;112:239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Portale G, Mazzeo A, Zuin M, Spolverato Y, Cipollari C, Fiscon V. Fully Laparoscopic Pancreas-Preserving Resection of the Third and Fourth Portion of the Duodenum for Adenocarcinomas and Gastrointestinal Stromal Tumors: Technical Report on a Case Series. J Laparoendosc Adv Surg Tech A. 2022;32:466-470. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Wu L, Li X, Qian X, Wang S, Liu J, Yan J. Lipid Nanoparticle (LNP) Delivery Carrier-Assisted Targeted Controlled Release mRNA Vaccines in Tumor Immunity. Vaccines (Basel). 2024;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 59] [Reference Citation Analysis (0)] |
| 23. | Fukusada S, Shimura T, Iwasaki H, Okuda Y, Katano T, Nishigaki R, Ozeki T, Kitagawa M, Nishie H, Tanaka M, Ozeki K, Kubota E, Tanida S, Kataoka H. Relationship between Immunophenotype and Clinicopathological Findings for Superficial Nonampullary Duodenal Epithelial Tumor. Digestion. 2021;102:870-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Boggi U. Laparoscopic duodenum-preserving total pancreatic head resection for pancreatic tumors: the difficult balance among overtreatment, ideal treatment, and undertreatment. Langenbecks Arch Surg. 2022;407:3859-3861. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Chen Y, Zhang H, Zhou Q, Lu L, Lin J. Metastases to duodenum in cervical squamous cell carcinoma: A case report and review of the literature. Medicine (Baltimore). 2022;101:e28526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Wu L, Chen X, Zeng Q, Lai Z, Fan Z, Ruan X, Li X, Yan J. NR5A2 gene affects the overall survival of LUAD patients by regulating the activity of CSCs through SNP pathway by OCLR algorithm and immune score. Heliyon. 2024;10:e28282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 41] [Reference Citation Analysis (0)] |
| 27. | Köroğlu G, Görür GD, Doğan S, Bayrak BY, Demir H. Incidental Uptake of 68Ga-DOTATATE Gastrointestinal Stromal Tumor of Duodenum. Clin Nucl Med. 2022;47:e289-e290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Liu W, Wang J, Ma L, Zhuang A, Xu J, He J, Yang H, Fang Y, Lu W, Zhang Y, Tong H. Which style of duodenojejunostomy is better after resection of distal duodenum. BMC Surg. 2022;22:409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |