Published online Dec 27, 2024. doi: 10.4240/wjgs.v16.i12.3643
Revised: September 3, 2024
Accepted: September 9, 2024
Published online: December 27, 2024
Processing time: 231 Days and 19.3 Hours
In this editorial we comment on the article published in the recent issue of the World Journal of Gastrointestinal Surgery. It investigates the potential mechanism of alcohol use disorder (AUD) following weight loss and its future prospects. We are particularly interested in this issue. According to existing research, the occurrence of AUD is closely linked to social factors, and the prevalence of AUD varies across different regions. However, there are limited studies on bariatric surgery and postoperative AUD in the Asian population, leaving ample room for further re
Core Tip: Patients with moderate-to-severe obesity can achieve durable weight loss and relief of related complications through surgery. However, the potential for various post-surgical complications cannot be overlooked. Postoperative follow-up, diet management and psychological counseling are critical to the treatment of obesity. Currently, there is a paucity of research on bariatric surgery within the Asian population, leaving ample room for further investigation in this area.
- Citation: Ma R, Jiang PQ, Liu SY, Yang DQ, Jiao Y. Obesity-Surgery is not the end. World J Gastrointest Surg 2024; 16(12): 3643-3646
- URL: https://www.wjgnet.com/1948-9366/full/v16/i12/3643.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i12.3643
Obesity is a prevalent global disease and a significant risk factor for a variety of conditions, including cardio-cere
The short-term complications of bariatric surgery primarily consist of anastomotic stenosis, fistula, bleeding, infection and so on. Long-term complications encompass malnutrition, weight regain, and psychological issues. The present primary research emphasis lies in examining the mechanisms and treatments for post-operative weight regain and psychological-related problems among patients. However, there is a limited amount of research on postoperative alcohol use disorder (AUD) in patients who undergo bariatric surgery.
AUD refers to a medical condition where individuals continue to consume alcohol despite experiencing adverse effects on their health, including physiological, psychological, behavioral, and social consequences[1] The Diagnostic and Statistical Manual of Mental Disorders and the International Classification of Diseases both provide detailed criteria for diagnosing AUD based on the presence of these adverse effects over the past year (Figure 1).
This study conducted a comprehensive study of the epidemiology, pathophysiology, and clinical outcomes of AUD and alcohol-related liver disease in individuals undergoing bariatric surgery. It summarizes the potential reasons for the increased risk of AUD among these patients and discusses opportunities to enhance postoperative care, emphasizing the importance of post-bariatric surgery management.
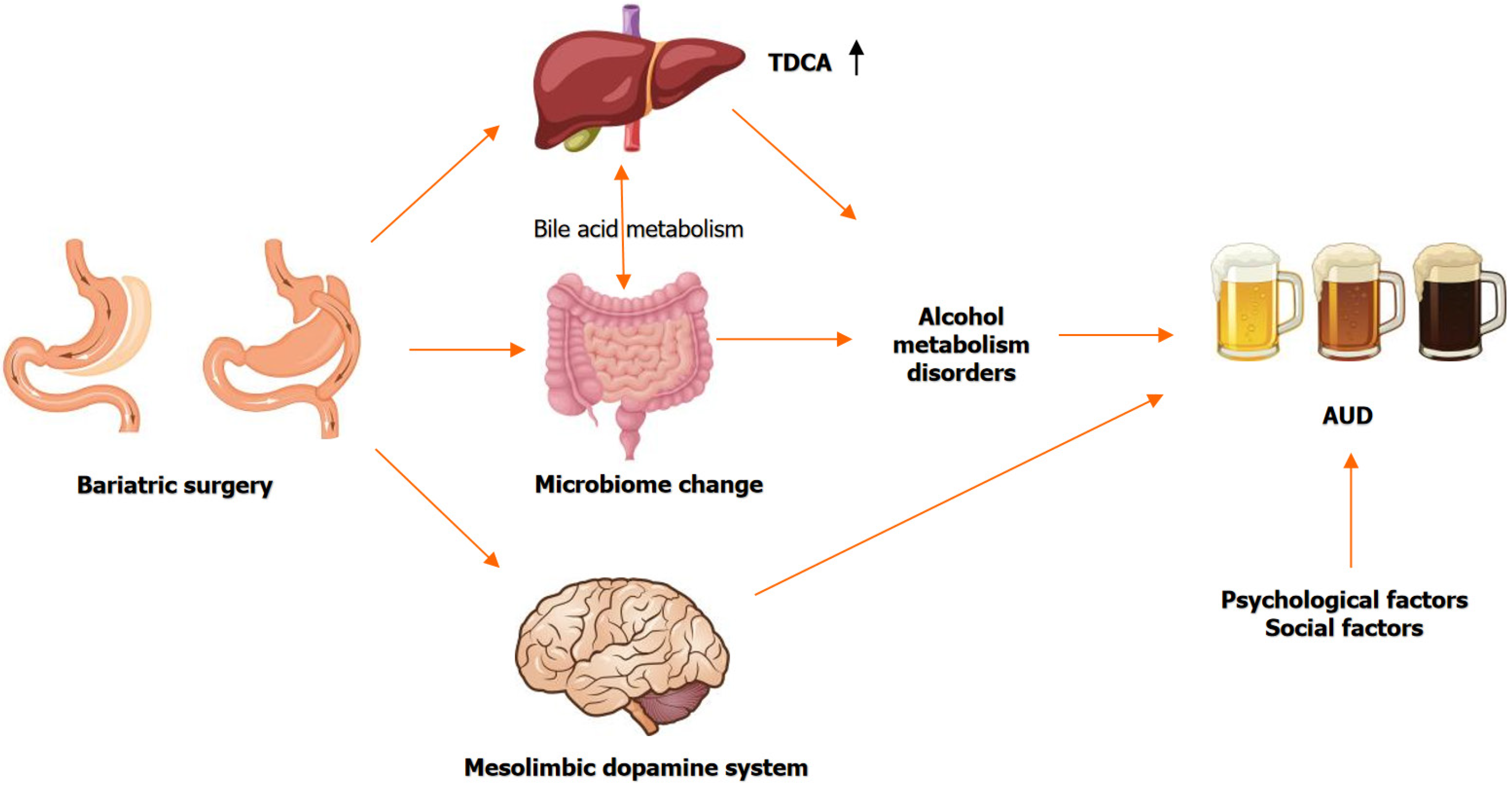
Bariatric surgery induces structural and functional changes in the body's original digestive system, which can impact the gut microbiome and hormonal regulation. These multifaceted changes encompass metabolic, psychological, and neurobiological aspects that may collectively contribute to an increased risk of developing AUD.
Bariatric surgery, such as SG, induces significant changes in the gut microbiome. These changes include alterations in bile acid metabolism, such as increased levels of taurodeoxycholic acid, which can improve glucose metabolism and potentially influence alcohol metabolism and preference[2]. The surgery also affects the composition of gut bacteria, such as an increase in Akkermansia, which is associated with reduced glucose-dependent insulinotropic polypeptide signaling. This alteration may indirectly affect alcohol metabolism and the risk of AUD by modifying metabolic pathways[3].
Bariatric surgery impacts hormonal regulation, including changes in ghrelin levels, which can affect the mesolimbic dopamine system, a key player in the brain's reward pathways. This alteration may increase the reinforcing value of alcohol, thereby elevating the risk of AUD[3]. The surgery also leads to changes in alcohol pharmacokinetics, particularly in procedures like RYGB and SG, which can result in higher blood alcohol concentrations and potentially increase the risk of developing AUD[4].
Psychological factors, such as depression and anxiety, are prevalent in patients undergoing bariatric surgery and can contribute to the development of AUD. The surgery may lead to a shift in coping mechanisms from food to alcohol, especially in individuals with pre-existing psychological vulnerabilities[4,5]. Despite these risks, some studies have not found a significant increase in AUD post-surgery, suggesting that individual variability and the type of surgical procedure may play a role in the risk of developing AUD[6].
Besides, research on AUD suggests that its development is influenced by multiple social factors, including alcohol availability, economic development level, and culture, in addition to individual factors such as age, smoking status and family history of alcohol consumption, the prevalence of AUD varies between men and women.
The main emphasis of this article's study is on the populations of Europe and America. There are significant differences in dietary and drinking habits between Asian populations and those in Europe and America. Based on a national survey regarding drug use, approximately 71.4% of Americans (ages 0-18) have started drinking alcohol and have difficulty quitting, and 10.2% of Americans (ages ≥ 12) have AUD. In Asia, by 2020, approximately 4.9 million (37.2%) people (ages ≥ 26 years) are alcohol users, of whom 7.5% (993000) have AUD. About 32.2 % (656000) of young adults (18-25 years) drank alcohol, of whom 9 % (184000) had AUD[7,8]. Currently, the reasons for the variations in the prevalence of AUD among different countries and their determinants remain unclear.
While bariatric surgery can improve metabolic health, it also poses a risk for AUD due to complex interactions between microbiome changes, hormonal shifts, and psychological factors. This underscores the importance of comprehensive pre- and post-operative monitoring and support to mitigate these risks. Further research is needed to fully understand these mechanisms and develop targeted interventions. Currently, the effectiveness of pharmacological treatment of AUD has been well established, but there are limited evaluations of the therapeutic effects of AUD-related pharmacological interventions in patients undergoing bariatric surgery. The research opportunities here are plentiful. It also reconfirms the need for a multidisciplinary approach to the treatment of obesity, as surgery or pharmacological interventions alone are not sufficient to address obesity and obesity-related diseases. Postoperative follow-up, diet management and psychological counseling are critical to the treatment of obesity.
| 1. | Alcohol's Effects on Health. Alcohol Use Disorder: A Comparison Between DSM-IV and DSM−5 on Alcohol abuse or Alcoholism. Available from: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-use-disorder-comparison-between-dsm. |
| 2. | Chen Y, Chaudhari SN, Harris DA, Roberts CF, Moscalu A, Mathur V, Zhao L, Tavakkoli A, Devlin AS, Sheu EG. A small intestinal bile acid modulates the gut microbiome to improve host metabolic phenotypes following bariatric surgery. Cell Host Microbe. 2024;32:1315-1330.e5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Reference Citation Analysis (0)] |
| 3. | Dong TS, Katzka W, Yang JC, Chang C, Arias-Jayo N, Lagishetty V, Balioukova A, Chen Y, Dutson E, Li Z, Mayer EA, Pisegna JR, Sanmiguel C, Jacobs JP. Microbial changes from bariatric surgery alters glucose-dependent insulinotropic polypeptide and prevents fatty liver disease. Gut Microbes. 2023;15:2167170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Paupério JM, Martins FS, Peixoto MJ, Mota M. Bariatric surgery as a risk factor for alcohol use disorder: a clinical case and literature review. Eur Psychiatr. 2023;66:S380-S381. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Gomes BB, Brandão HBDM, Pinheiro SI, Lima FR, Garcia HJ, Campos ACA, Silvestre VS, Aros MS, Francisco LD, Miura AVSAS. Post-Bariatric Transformations: The Relationship Between Bariatric Surgery and Alcoholism. Int J Health Sci. 2024;4:2-6. [DOI] [Full Text] |
| 6. | Oliveira KC, Santa-Cruz F, Souza Leão LM, Kreimer F, Ferraz ÁAB. Alcohol use disorder in patients after undergoing bariatric surgery. 2024 preprint. [DOI] [Full Text] |
| 7. | SAMHSA. The National Survey on Drug Use and Health: 2020. Available from: https://www.samhsa.gov/data/release/2020-national-survey-drug-use-and-health-nsduh-releases. |
| 8. | Belay GM, Lam KKW, Liu Q, Wu CST, Mak YW, Ho KY. Magnitude and determinants of alcohol use disorder among adult population in East Asian countries: A systematic review and meta-analysis. Front Public Health. 2023;11:1144012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |