Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3301
Revised: August 23, 2024
Accepted: September 3, 2024
Published online: October 27, 2024
Processing time: 178 Days and 3 Hours
Gallbladder perforation is a serious complication of acute cholecystitis. Such perforation is a rare but life-threatening situation that can lead to the formation and rupture of liver hematomas. Here, we report a case of a ruptured intrahepatic hematoma caused by intrahepatic gallbladder perforation, and we present a literature review.
A 70-year-old male was admitted to the hospital with a complaint of right upper quadrant abdominal pain, flustering and dizziness. The preoperative diagnosis was a ruptured malignant liver tumor, and the patient’s medical images and increased level of carbohydrate antigen-199 suggested that the gallbladder had been invaded. However, the tumor was proven to be a liver hematoma secondary to gallbladder perforation after surgery. The patient was discharged uneventfully on the fifteenth postoperative day.
Intrahepatic gallbladder perforation is difficult to diagnose preoperatively. Radiological examinations play a crucial role in the diagnosis but only for partial cases. Early diagnosis and appropriate surgery are key to managing this rare condition.
Core Tip: In this work, we present a rare clinical case in which a ruptured malignant liver tumor with invasion of the gallbladder was suspected but was proven to be a liver hematoma secondary to gallbladder perforation after surgery. Moreover, we conducted a literature review on intrahepatic gallbladder perforation. Here, the symptoms, examinations, diagnosis and treatments of intrahepatic gallbladder perforation are summarized. Additionally, we propose a new classification system for gallbladder perforation, which provides a valuable reference for the diagnosis and treatment of this condition.
- Citation: Huang HW, Wang H, Leng C, Mei B. Formation and rupture of liver hematomas caused by intrahepatic gallbladder perforation: A case report and review of literature. World J Gastrointest Surg 2024; 16(10): 3301-3311
- URL: https://www.wjgnet.com/1948-9366/full/v16/i10/3301.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i10.3301
Gallbladder perforation (GBP) is a rare but life-threatening complication of acute cholecystitis, occurring in 2%-11% of patients with cholecystitis[1,2]. GBP remains an important problem for surgeons because many cases fail to be diagnosed before surgery, and the mortality rate is as high as 12%-16%[3]. In 1934, Niemeier firstly classified GBP into three types: (1) Type I chronic perforation with fistula formation between the gallbladder and another viscus; (2) Type II subacute perforation where the perforated gallbladder is surrounded by an abscess that is walled off by adhesions from the general peritoneal cavity; and (3) Type III acute perforation into the free peritoneal cavity without protective adhesions[1]. Intrahepatic GBP is a rare type that has only been reported in a few studies. Cases of GBP leading to the formation and rupture of liver hematomas have seldom been reported.
Herein, we report a case of a ruptured liver hematoma caused by GBP. Moreover, we conducted a literature review about intrahepatic GBP to characterize the common clinical manifestations, diagnosis and treatments.
Right upper quadrant abdominal pain.
A 70-year-old man with a past history of chronic constipation presented to the Emergency Department of a local hospital complaining of worsening colicky pain in the right upper quadrant of the abdomen, as well as for flustering and dizziness. He had repeatedly experienced right upper quadrant abdominal pain for one week with nausea, vomiting and referred pain in the right shoulder. On September 11, 2022, the patient was taken to the local hospital because his symptoms had worsened dramatically. At the same time, he also exhibited an insufficient blood volume, which caused him to be flustered and to experience dizziness.
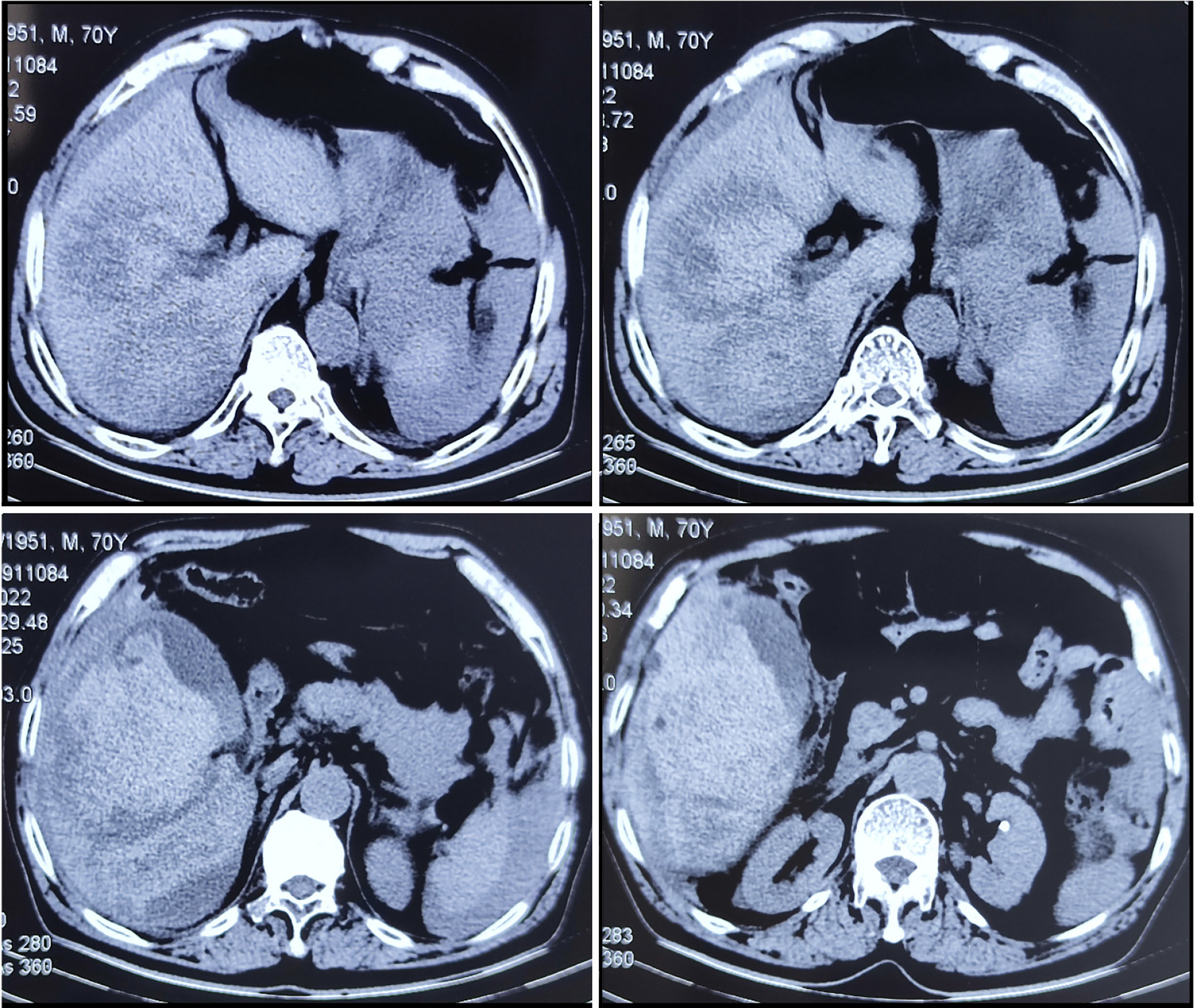
After admission, emergency abdominal computed tomography (CT) revealed a mixed density shadow in the right lobe of the liver combined with abdominopelvic effusion and an enlarged gallbladder adjoining the mass, suggesting that the liver tumor had ruptured, bled and invaded the gallbladder (Figure 1). The laboratory results showed that the hemoglobin (Hb) level had decreased to 9.4 g/dL and the serum carbohydrate antigen-199 (CA-199) level had increased to 1972 U/mL. Then, he planned to receive hepatic artery embolization, but angiography revealed no active bleeding artery. This might suggest that the bleeding vessel was a vein or that the hemorrhage had stopped. The patient was transferred to our hospital for further treatment on the evening of September 12, 2022, after his general condition had stabilized.
The patient denied a history of trauma or falls, chronic hepatitis, alcoholic liver disease, cirrhosis, hemangioma, other liver tumors, or cholecystolithiasis.
On admission, the patient’s hemodynamics were stable, with a heart rate of 99 beats per minute, a blood pressure of 18.5/10.4 kPa, and an oxygen saturation of 95%. Physical examination revealed abdominal distension and marked tenderness in the right upper quadrant of the abdomen.
The laboratory results (Table 1) revealed low Hb levels (8.7 g/dL), elevated white blood cell (WBC) counts (14.56 × 109/L), elevated alanine aminotransferase (ALT) levels (2509 U/L) and total bilirubin levels (37.8 μmol/L). Additionally, the levels of serum CA-199 and protein induced by vitamin K absence or antagonist-II (PIVKA-II) had elevated to 106.5 U/mL and 59.02 mAu/mL, respectively. The serum alpha fetoprotein level was 2.76 ng/mL. After admission, the patient underwent a blood transfusion and intravenous infusion of analgesics, hemostatic agents and antibiotics. After treatment, his condition stabilized, and the laboratory parameters gradually improved.
| Parameters | On admission | Postoperative |
| White blood cell (109/L) | 14.56 | 5.20 |
| Hemoglobin (g/L) | 87 | 105 |
| Platelet (109/L) | 72 | 158 |
| Alanine aminotransferase (U/L) | 2509 | 80 |
| Aspartate aminotransferase (U/L) | 2403 | 44 |
| Total bilirubin (µmol/L) | 37.8 | 13.5 |
| γ-glutamyl transferase (U/L) | 89 | 123 |
| Prothrombin time (second) | 15.7 | 12.8 |
| Alpha fetoprotein (ng/mL) | 2.76 | NA |
| Carcinoembryonic antigen (ng/mL) | 3.74 | NA |
| Carbohydrate antigen-199 (U/mL) | 106.5 | NA |
| Protein induced by vitamin K absence or antagonist-II (mAu/mL) | 59.02 | NA |
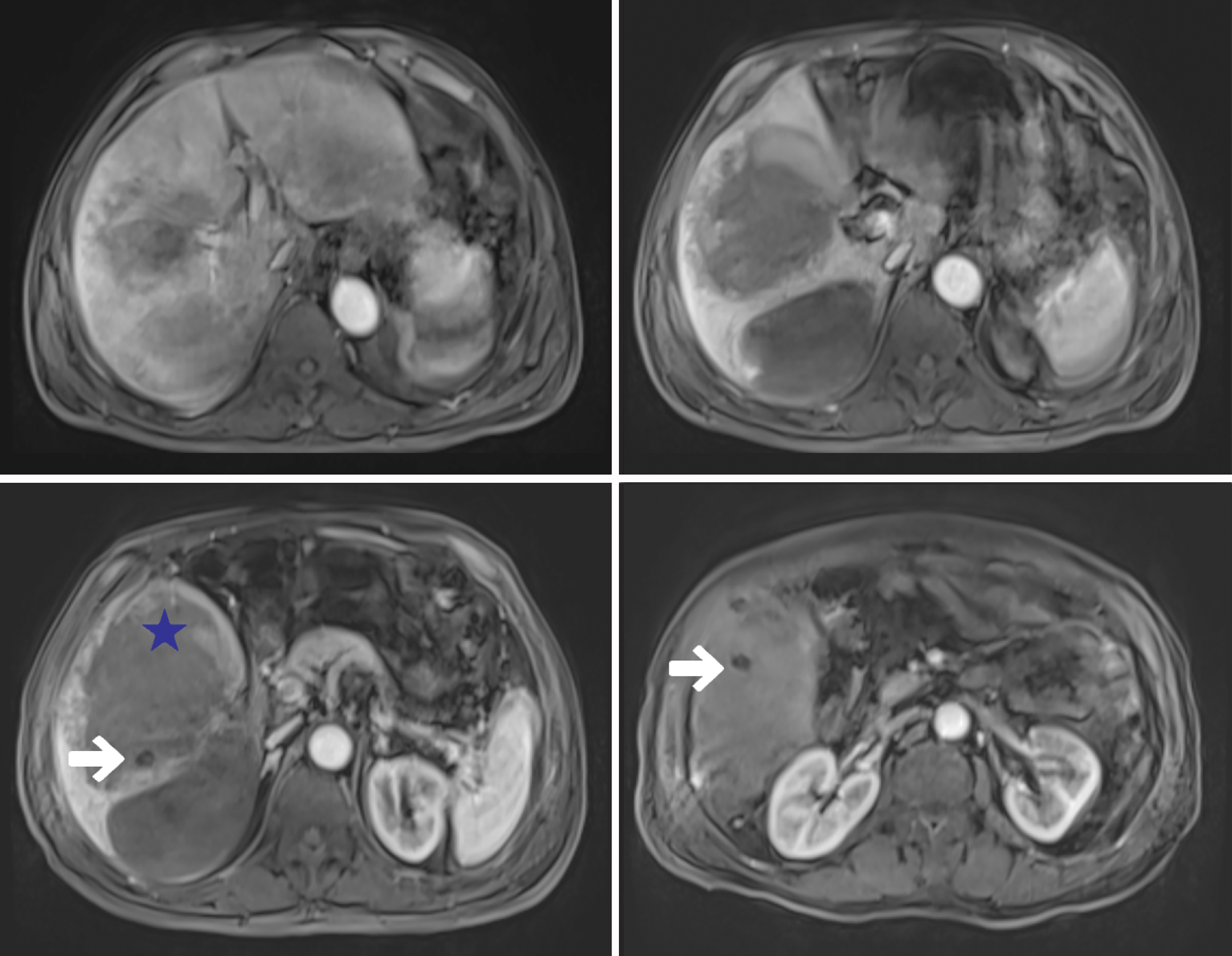
Magnetic resonance imaging (MRI) of the abdomen performed on September 16, 2023, revealed a mass with mixed signals in the right lobe of the liver, with a large cross-sectional area of 114 mm × 131 mm. There were several rounded long T1 signals in the mixed-signal mass. The parenchymal region showed hyperintensity on diffusion-weighted imaging (b = 1000), and no obvious enhancement was found on dynamic contrast-enhanced MRI (DCE-MRI). The gallbladder was distended, with a thickened wall, and was poorly demarcated from the mass (Figure 2).
Based on the results of MRI and the elevated tumor markers (CA-199, PIVKA-II), we initially determined that the patient had a ruptured malignant liver tumor with invasion of the gallbladder.
The patient underwent surgery on September 26, 2022, after other examinations were completed and contraindications were excluded.
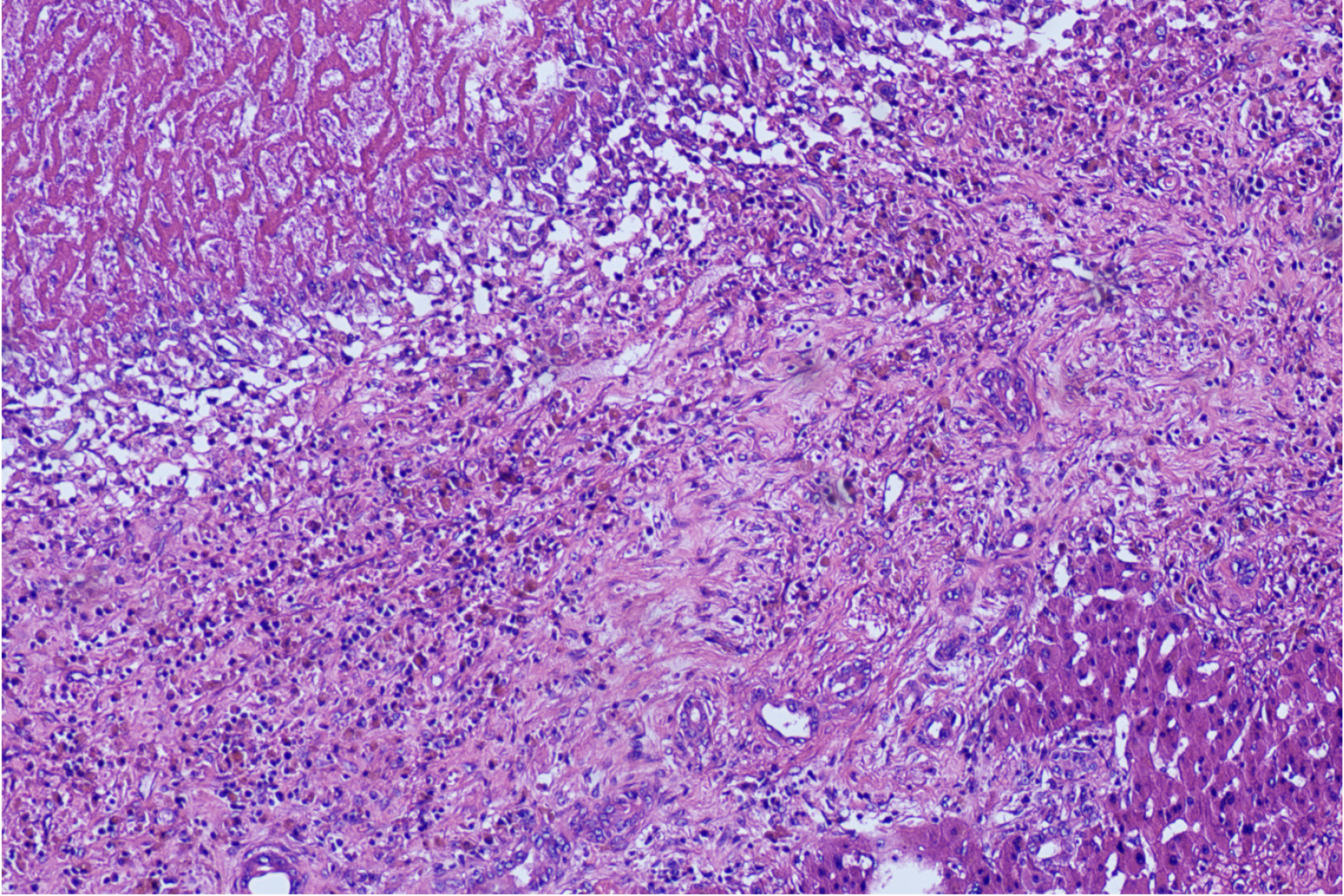
Laparotomy revealed the following findings: bloody ascites in the abdominal cavity and a 14 cm × 10 cm dark-red mass located in the segments V and VI of the liver (Couinaud segment). The mass was adherent to the transverse colon, omentum and gallbladder which was enlarged to 12 cm × 4 cm. During the surgery, the Calot triangle was first dissected to ligate the cystic duct and the cystic artery. Second, we prepositioned the blocking bands at the first hepatic portal and the inferior vena cava to control bleeding during partial liver resection. Third, we planned to remove the mass and gallbladder completely. However, during the resection, we found that there was no capsule or boundary between the mass and the liver parenchyma. Unexpectedly, there was no solid tissue but many blood clots as well as several hard yellow stones inside the mass, indicating that the lumen of the mass was connected to the gallbladder cavity. The gallbladder seemed to be the root of the disease. At this point, we suspected that the hemorrhage was caused by gallbladder cancer invading the liver. However, upon exploration of the resected specimen, we found that there was no obvious malignant tumor in the liver. Instead, the mass appeared to be a simple hematoma that was connected to the gallbladder. The gallbladder body was perforated, and the area around the perforation felt firm upon palpation. Surprisingly, the histopathologic examination revealed that the liver mass was a hematoma and that there was no cancer but an ulcer of the gallbladder with fibrosis and inflammatory cell infiltration (Figure 3).
The patient was discharged on the fifteenth postoperative day without any complications. During the 1-year follow-up, neither cholelithiasis recurrence nor death occurred.
A systematic review of the literature was conducted to identify published cases of intrahepatic GBP. The terms ‘gallbladder’, ‘perforation’, ‘liver’, ‘intrahepatic’ and ‘transhepatic’ were searched in various combinations with the Boolean operators AND and OR via the OVID databases and PubMed databases. The abstracts of all the full-text English articles were scrutinized. The reference lists of the articles obtained were also searched to identify further relevant citations. Six publications were excluded because they were not available for online access owing to their publication in an older era. Ultimately, 30 publications containing 40 patients were included (Table 2)[4-33]. The majority of these publications (n = 24) were single patient case studies. A summary of the clinical cases of intrahepatic GBP is presented in Table 2. Among all patients, the mean age was 59.6 years ± 18.1 years (range 13-95 years) old. Males accounted for the majority of cases (n = 33, 82.5%). In total, 22.5% of patients (n = 9) had a past history of confirmed cholelithiasis, 17.5% (n = 7) had hypertension, 15% (n = 6) had diabetes mellitus (DM), 5% (n = 2) had coronary arterial disease (CAD), 5% (n = 2) had chronic obstructive pulmonary disease and 5% (n = 2) consumed alcohol. Interestingly, there was one particular patient with a ruptured liver hemangioma caused by GBP[10].
| Ref. | Year | Age | Sex | Classification1 | Past history | Abdominal pain | Fever | Neusa or vomiting | Shock | Jaundice | Abnormal laboratory tests | Examinations | Treatment |
| Paramythiotis et al[4] | 2022 | 69 | Female | B | DM, hypertension | 1 | 1 | CRP, ALT, AST, TBIL | US, MRCP | S2 | |||
| Paramythiotis et al[4] | 2022 | 79 | Male | B | Chronic abdominal pain | 1 | 1 | 1 | 1 | WBC, CRP, TBIL, GGT | CT, MRI | S1 | |
| Paramythiotis et al[4] | 2022 | 54 | Male | B | Chronic alcohol consumption | 1 | 1 | WBC, CRP, ALP | CT | D1+S1 | |||
| Mach et al[5] | 2022 | 55 | Male | A | Ccholelithiasis | 1 | 1 | HB | CT | S1 | |||
| Nikumbh et al[6] | 2020 | 55 | Male | B | Rheumatoid arthritis | 1 | 1 | N/A | US, CT, MRCP | D3+S2 | |||
| Nikumbh et al[6] | 2020 | 28 | Female | B | Cholelithiasis | 1 | N/A | CT, MRCP | D3+S2 | ||||
| Chikamori et al[7] | 2020 | 87 | Male | A, B | Cholelithiasis, CAD | 1 | 1 | 1 | WBC, CRP, ALT, AST, ALP | CT, cholangiography | D1 | ||
| Lan et al[8] | 2019 | 53 | Male | A | N/A | 1 | 1 | WBC, ALT, AST, TBIL, carbohydrate antigen-199 | CT | S1 | |||
| Parekh et al[9] | 2019 | 68 | Female | B | N/A | 1 | 1 | N/A | CT | D3 | |||
| Ke et al[10] | 2017 | 44 | Male | A | Hepatic hemangiomas, cholelithiasis | 1 | HB | CT | S1 | ||||
| Williams et al[11] | 2017 | 61 | Male | B | N/A | 1 | 1 | 1 | CRP, ALP | CT | D3+S2 | ||
| Hussain et al[12] | 2016 | 72 | Male | B | Cholelithiasis | 1 | 1 | 1 | WBC, CRP | CT | D1+S2 | ||
| Hussain et al[12] | 2016 | 62 | Male | B | Cholelithiasis | 1 | 1 | WBC, CRP | US, CT | D1+S2 | |||
| Cristian et al[13] | 2014 | 76 | Male | B | Hypertension, a repaired inguinal hernia | 1 | 1 | 1 | WBC, CRP | X-ray, US, CT | S2 | ||
| Donati et al[14] | 2014 | 62 | Male | B | Inguinal hernia | 1 | WBC | US, CT, MRI | S3 | ||||
| Alessiani et al[15] | 2014 | 77 | Male | B | Alzheimer's disease, hypertension, atrial fibrillation | 1 | 1 | WBC, ALT, AST | US, CT | D1 | |||
| Agarwal et al[16] | 2013 | 18 | Male | B | N/A | 1 | N/A | US, CT | S3 | ||||
| Agarwal et al[16] | 2013 | 40 | Male | B | N/A | 1 | N/A | US | D1+S2 | ||||
| Agarwal et al[16] | 2013 | 42 | Male | B | N/A | 1 | N/A | US, MRCP | S2 | ||||
| Singh et al[17] | 2013 | 50 | Male | B | Chronic abdominal pain | 1 | N/A | US, CT | S1 | ||||
| Hollanda et al[18] | 2013 | 50 | Male | C | N/A | 1 | 1 | 1 | 1 | WBC, ALT, AST, TBIL | US, CT | S1 | |
| Coulier et al[19] | 2012 | 68 | Male | A | Epigastric pain | 1 | 1 | HB, CRP, ALT, AST | CT, MRI | S1 | |||
| Taneja et al[20] | 2012 | 62 | Male | C | N/A | 1 | 1 | WBC, ALT, AST, ALP | US, CT | D1+S1 | |||
| Kalfadis et al[21] | 2011 | 95 | Male | C | Cholelithiasis, hypertension | 1 | 1 | WBC, GGT | US, CT | D1 | |||
| Göbel et al[22] | 2011 | 30 | Female | B | Hypertension, nephrectomy, hypernephroma, cholelithiasis | 1 | 1 | WBC, CRP | US, CT | S1 | |||
| Shakya et al[23] | 2010 | 60 | Male | N/A | Epigastric pain | 1 | 1 | 1 | WBC, ALT, AST, TBIL, ALP | X-ray, US | S1 | ||
| Tsai et al[24] | 2010 | 66 | Male | C | COPD, chronic kidney disease | 1 | 1 | 1 | WBC, ALP | US, CT | D2 | ||
| Kochar et al[25] | 2008 | 67 | Male | B | DM, diverticular disease, stroke | 1 | 1 | WBC, CRP, ALP | US, CT, abscessogram,MRCP | D1+S1 | |||
| Łebkowski et al[26] | 2008 | 80 | Male | A | Hypertension | 1 | 1 | N/A | US | S1 | |||
| Nural et al[27] | 2007 | 73 | Male | A | COPD, CAD, DM, hypertension | 1 | 1 | WBC, ALT | CT | S1 | |||
| Kang et al[28] | 2007 | 70 | Male | B | Stroke | 1 | 1 | N/A | CT | D1+D3 | |||
| Ceylan et al[29] | 2003 | 13 | Male | N/A | N/A | 1 | 1 | 1 | WBC, ALT, AST, TBIL, ALP | US | conservative drug treatment | ||
| Peer et al[30] | 1994 | 69-81 | 2 males, 2 females | B | DM | 1 | 1 | WBC, ALP | CT | D1+S1 | |||
| Chen et al[31] | 1990 | 60 | Male | B | Alcohol consumption | 1 | 1 | 1 | WBC, AST, ALP | US | S1 | ||
| Syme et al[32] | 1989 | 74 | Female | A | Cholelithiasis | 1 | 1 | N/A | N/A | S1 | |||
| Teefey et al[33] | 1987 | 69 | Male | B | DM | 1 | WBC, AST, TBIL, ALP | US, CT | S1 | ||||
| Teefey et al[33] | 1987 | 55 | Male | B | N/A | 1 | 1 | WBC, ALP | US, CT | D1+S1 |
In these cases, except for two cases in which GBP occurred in the hospital and no further complications developed, intrahepatic GBP could be divided into three categories: (1) Type A, GBP leading to the formation and rupture of a liver hematoma manifesting as hemorrhage and shock; (2) Type B, GBP leading to a liver abscess; and (3) Type C, GBP manifesting as a liver biloma. The most common form of intrahepatic GBP was type B (n = 27, 67.5%), followed by type A (n = 8, 20%) and type C (n = 4, 10%). Specifically, there was one case in which an intrahepatic GBP led to hemoperitoneum and abscess formation at the same time[7]. The majority of the patients presented with right upper quadrant abdominal pain (n = 34, 91.9%). The remaining symptoms were fever (n = 22, 59.5%), nausea or vomiting (n = 10, 27%), shock (n = 7, 18.9%), and jaundice (n = 5, 13.5%). The common abnormal laboratory tests included WBC, c-reactive protein (CRP), ALT, aspartate aminotransferase (AST) and alkaline phosphatase (ALP). The remaining abnormal results included Hb, total bilirubin, γ-glutamyl transferase (GGT) and CA-199. Ultrasound (US) and abdominal CT were the common approaches for identifying cholecystitis and intrahepatic GBP. Most of the patients (n = 32, 80%) eventually underwent surgery, including open surgery (n = 22, 68.75%), laparoscopic surgery (n = 8, 25%) and laparoscopic conversion to open surgery
GBP is usually associated with the presence of gallbladder stones but can also be encountered in acute acalculous cholecystitis, although this occurs rarely[2]. Occlusion of the cystic duct (most frequently by stones), which leads to biliary stasis and gallbladder distension with consequential increased pressure and impaired circulation in the gallbladder, combined with bacterial colonization and infection, causes necrosis and perforation of the gallbladder[21,34]. The gallbladder fundus is the most common position of GBP owing to the poor blood supply[2,35]. Generally, perforation in the fundus leads to bile drainage into the peritoneal space without protective adhesions. In our patient, the perforation was located in the gallbladder body, which contacts the liver. The occurrence of GBP is more common in males over 60 years old, whereas acute uncomplicated cholecystitis is more common among females[2]. The literature review revealed similar results. Other risk factors related to GBP include previous cholecystitis, hypertension, DM, CAD and long-term use of steroids. As our study showed, many patients had a past history of cholecystitis, hypertension or DM. GBP was based on cholecystitis. Hypertension and DM could lead to poor microcirculation in the gallbladder because of changes in arterioles.
There are considerable debates in the literature regarding the modification of Niemeier’s classification. Anderson and Nazem[36] and Ibrarullah et al[37] recommended labeling the cholecystobiliary fistula as type IV GBP, considering the unique operative approach needed in such cases. However, Kochar et al[25] argued that GBP with fistula formation or a demonstrable communication, including cholecystobiliary and cholecystohepatic connections, should be divided into Niemeier type III perforations, to maintain uniformity in reporting. However, uniformity cannot be achieved, as intrahepatic GBP with liver abscess formation is usually considered as a Niemeier type II perforation[22,38]. In addition, intrahepatic GBP with hemorrhage is an urgent and life-threatening condition that is not suitable for Niemeier’s classification. Therefore, a new classification of GBP must be formulated. Here, we propose the following conceptions: (1) Type I, perforation into the peritoneal cavity with (IA, acute perforation) or without (IB, subacute or chronic perforation) adhesions; (2) Type II, intrahepatic perforation including three subcategories (IIA, acute perforation with the formation and rupture of a liver hematoma; IIB, subacute or chronic perforation leading to a liver abscess; IIC, chronic perforation leading to a liver biloma); and (3) Type III, chronic perforation with the formation of a fistula that can communicate with the outside, including cholecystobiliary, cholecystoenteric and cholecystocutaneous fistulas. This classification is simple and unlikely to cause confusion in the diagnosis.
There are no classical symptoms or signs related to intrahepatic GBP. Patients usually present right upper quadrant abdominal pain, fever and nausea. In our case, the patient also exhibited insufficient blood volume, with symptoms that included feeling flustered and experiencing dizziness. Increased levels of inflammation indicators, such as WBC and CRP, and elevated liver enzymes, including ALT, AST, ALP and GGT, are commonly observed. However, it is difficult to clinically distinguish GBP from an uncomplicated acute cholecystitis, as the majority of the above features are present in both of them. There were two characteristics in our case. One was extremely elevated ALT and AST levels due to the formation and rupture of a huge liver hematoma. Considering the high risk of post-hepatectomy liver failure, emergency surgery was excluded. The other was increased CA-199, which was most commonly used as a tumor marker to help diagnose hepatobiliary and pancreatic malignancies[39]. A ruptured mass on medical imaging combined with increased CA-199 caused us to misdiagnose this case, which was similar to the findings of Lan et al[8]. Previous studies have shown that high CA-199 levels can be detected in patients with calculous cholecystitis and are associated with the degree of gallbladder inflammation[40]. This phenomenon deserves more attention from clinicians to avoid a misdiagnosis.
The preoperative diagnosis of GBP depends on radiological examinations, including US, CT, and MRI. The findings of acute cholecystitis, such as gallbladder stones, distention and wall thickening, can also be presented in GBP. The reliable sign of GBP is a defect in the gallbladder wall (the “hole sign”)[25,35,41]. CT is superior to US in depicting the hole sign[41]. However, both US and CT may not be useful for diagnosing some cases with perforation[2,27,42]. Kim et al[43] reported that defects could not be visualized via CT in 54% of patients. In our case, the hole sign could be identified via MRI (Figure 2) but failed to be detected on CT. Several rounded long T1 signals in the mass were confirmed to be gallbladder stones after the operation. No obvious enhancement was found on DCE-MRI, which also indicated that the mass was not a malignancy. Intrahepatic perforations with the formation of a liver abscess or biloma could be diagnosed more easily than perforations with ruptured liver hematomas. According to our review, all cases were accurately diagnosed except for two cases of GBP with liver rupture[5,8]. The diagnosis rate was much higher than that in previous reports. This might be due to a publication bias.
Regarding treatments for type A intrahepatic GBP, emergency laparotomy is the first consideration for patients who are in good general condition[19,26]. For patients in poor condition, transarterial embolization combined with secondary hepatectomy and cholecystectomy is an ideal treatment strategy. According to the literature review, percutaneous transhepatic drainage combined with secondary cholecystectomy is the most common treatment for intrahepatic GBP of types B and C. Laparoscopic cholecystectomy is challenging because of severe inflammation and adhesions in the abdominal cavity. Among the 10 patients who chose laparoscopic cholecystectomy, two cases were eventually converted to open surgery[14,16]. Additionally, ENBD is a safe and effective treatment for patients who are not suitable for surgery[9,24].
In summary, intrahepatic GBP is difficult to diagnose preoperatively. Radiological examinations play a crucial role in diagnosis only for partial cases. How to improve the diagnostic rate needs further investigation. Early diagnosis and appropriate surgery are key to managing this rare condition.
The authors thank the patient for his collaboration.
| 1. | Niemeier OW. Acute Free Perforation of the Gall-Bladder. Ann Surg. 1934;99:922-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 175] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol. 2006;12:7832-7836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 116] [Cited by in RCA: 139] [Article Influence: 7.3] [Reference Citation Analysis (1)] |
| 3. | Ong CL, Wong TH, Rauff A. Acute gall bladder perforation--a dilemma in early diagnosis. Gut. 1991;32:956-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Paramythiotis D, Karakatsanis A, Karlafti E, Bareka S, Psoma E, Hatzidakis AA, Michalopoulos A. Pyogenic Liver Abscess Complicating Acute Cholecystitis: Different Management Options. Medicina (Kaunas). 2022;58:782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Mach, Moláček J, Skalický T, Třeška V. Transhepatic perforation of the gallbladder with massive intraperitoneal hemorrhage as a rare complication of acute cholecystitis. Rozhl Chir. 2022;100:603-606. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Nikumbh T, Bhandarwar A, Sanap S, Wagholikar G. Laparoscopic management of intra-hepatic gallbladder perforation. J Minim Access Surg. 2020;16:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Chikamori F, Yukishige S, Ueta K, Takasugi H, Mizobuchi K, Matsuoka H, Hokimoto N, Yamai H, Onishi K, Tanida N, Hamaguchi N, Iwasaki T. Hemoperitoneum and sepsis from transhepatic gallbladder perforation of acute cholecystitis: A case report. Radiol Case Rep. 2020;15:2241-2245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Lan X, Xiang Y, Liu F, Li B, Wei Y, Zhang H. Massive hemoperitoneum and upper gastrointestinal hemorrhage following liver rupture secondary to gallbladder perforation: A case report and literature review. Medicine (Baltimore). 2019;98:e14729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Parekh PJ, Shakhatreh MH, Desai MR, Yeaton P. Endoscopic Drainage of an Intrahepatic Abscess Secondary to a Perforated Gallbladder. ACG Case Rep J. 2019;6:e00108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Ke QH, Zhang CJ, Huang HF. Rupture of hepatic hemangioma with hemoperitoneum due to spontaneous gallbladder perforation: A unique case report. Medicine (Baltimore). 2017;96:e6110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Williams P, Dosani A, Morgan-Jones R. Endoscopic cystic duct stent as primary treatment for intrahepatic gallbladder perforation with abscess formation. Ann R Coll Surg Engl. 2017;99:e118-e120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Hussain T, Adams M, Ahmed M, Arshad N, Solkar M. Intrahepatic perforation of the gallbladder causing liver abscesses: case studies and literature review of a rare complication. Ann R Coll Surg Engl. 2016;98:e88-e91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Cristian D, Grama F, Burcoş T. Laparoscopic treatment of a hepatic subcapsular abscess secondary to gallbladder perforation: case report. Chirurgia (Bucur). 2014;109:132-135. [PubMed] |
| 14. | Donati M, Biondi A, Basile F, Gruttadauria S. An atypical presentation of intrahepatic perforated cholecystitis: a modern indication to open cholecystectomy. Report of a case. BMC Surg. 2014;14:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Alessiani M, Peloso A, Tramelli P, Magnani E. Successful non-operative management of spontaneous type II gallbladder perforation in a patient with Alzheimer's disease. BMJ Case Rep. 2014;2014:bcr2014204337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Agarwal N, Saini P, Gupta A, Kaur N, Shreshtha S, Faridi MS. Chronic hepatic abscess due to gallbladder perforation: three cases and exact nomenclature. Trop Gastroenterol. 2013;34:199-202. [PubMed] [DOI] [Full Text] |
| 17. | Singh K, Singh A, Vidyarthi SH, Jindal S, Thounaojam CK. Spontaneous Intrahepatic Type II Gallbladder Perforation: A Rare Cause of Liver Abscess - Case Report. J Clin Diagn Res. 2013;7:2012-2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Hollanda ESD, Torres UDS, Gual F, Oliveira EPD, Cardoso LV, Criado DAB. Spontaneous perforation of gallbladder with intrahepatic biloma formation: sonographic signs and correlation with computed tomography. Radiol Bras. 2013;46:320-322. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Coulier B, Maldague P, Pierard F. Spontaneous transhepatic rupture of the gallbladder with massive hemoperitoneum. JBR-BTR. 2012;95:92-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Taneja S, Sharma A, Duseja AK, Kalra N, Chawla Y. Spontaneous perforation of gallbladder with intrahepatic bilioma. J Clin Exp Hepatol. 2011;1:210-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Kalfadis S, Ioannidis O, Botsios D, Lazaridis C. Subcapsular liver biloma due to gallbladder perforation after acute cholecystitis. J Dig Dis. 2011;12:412-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Göbel T, Kubitz R, Blondin D, Häussinger D. Intrahepatic type II gall bladder perforation by a gall stone in a CAPD patient. Eur J Med Res. 2011;16:213-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Shakya VC, Agrawal CS, Khaniya S, Paudel G, Shrestha KR, Adhikary S. Transhepatic perforation of the gallbladder: rare complication of a common disease. J Surg Case Rep. 2010;2010:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Tsai MC, Chen TH, Chang MH, Chen TY, Lin CC. Gallbladder perforation with formation of hepatic subcapsular biloma, treated with endoscopic nasobiliary drainage. Endoscopy. 2010;42 Suppl 2:E206-E207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Kochar K, Vallance K, Mathew G, Jadhav V. Intrahepatic perforation of the gall bladder presenting as liver abscess: case report, review of literature and Niemeier's classification. Eur J Gastroenterol Hepatol. 2008;20:240-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Łebkowski Ł, Bialek P, Proczka RM, Polanski JA. Haemorrhage to the peritoneal cavity. Rare complication of gallbladder perforation. VSJ. 2008;3:142-145. |
| 27. | Nural MS, Bakan S, Bayrak IK, Baydin A, Danaci M. A rare complication of acute cholecystitis: transhepatic perforation associated with massive intraperitoneal hemorrhage. Emerg Radiol. 2007;14:439-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Kang MS, Park DH, Kwon KD, Park JH, Lee SH, Kim HS, Park SH, Kim SJ. Endoscopic transcystic stent placement for an intrahepatic abscess due to gallbladder perforation. World J Gastroenterol. 2007;13:1458-1459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Ceylan H, Sirikci A, Ozokutan BH, Bayram M, Sivasli E. Conservative management of intrahepatic perforation of the gallbladder secondary to acalculous cholecystitis. Eur J Pediatr Surg. 2003;13:337-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Peer A, Witz E, Manor H, Strauss S. Intrahepatic abscess due to gallbladder perforation. Abdom Imaging. 1995;20:452-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Chen JJ, Lin HH, Chiu CT, Lin DY. Gallbladder perforation with intrahepatic abscess formation. J Clin Ultrasound. 1990;18:43-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Syme RG, Thomas EJ. Massive hemoperitoneum from transhepatic perforation of the gallbladder: a rare complication of cholelithiasis. Surgery. 1989;105:556-559. [PubMed] |
| 33. | Teefey SA, Wechter DG. Sonographic evaluation of pericholecystic abscess with intrahepatic extension. J Ultrasound Med. 1987;6:659-662. [PubMed] [DOI] [Full Text] |
| 34. | Morris BS, Balpande PR, Morani AC, Chaudhary RK, Maheshwari M, Raut AA. The CT appearances of gallbladder perforation. Br J Radiol. 2007;80:898-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Date RS, Thrumurthy SG, Whiteside S, Umer MA, Pursnani KG, Ward JB, Mughal MM. Gallbladder perforation: case series and systematic review. Int J Surg. 2012;10:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 36. | Anderson BB, Nazem A. Perforations of the gallbladder and cholecystobiliary fistulae: a review of management and a new classification. J Natl Med Assoc. 1987;79:393-399. [PubMed] |
| 37. | Ibrarullah M, Saxena R, Sikora SS, Kapoor VK, Kaushik SP. Unusual gall bladder perforation--definition of a new type. Indian J Gastroenterol. 1992;11:170. [PubMed] |
| 38. | Judd ES, Phillips JR. Perforation of the Gall-Bladder in Acute Cholecystitis. Ann Surg. 1933;98:359-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Qin XL, Wang ZR, Shi JS, Lu M, Wang L, He QR. Utility of serum CA19-9 in diagnosis of cholangiocarcinoma: in comparison with CEA. World J Gastroenterol. 2004;10:427-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 103] [Cited by in RCA: 127] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 40. | Chen W, Wang S, Zhao H, Wang G, Qin R, Huang F, Geng W, Liu Z, Wang W, Wu R, Hou L, Ye Z, Zhang X, Geng X, Yu X. High level of tumor marker CA19-9 returned to normal after cholecystectomy in calculous cholecystitis patients. Scand J Gastroenterol. 2023;58:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Neimatullah MA, Rasuli P, Ashour M, Lewandowski BJ. Sonographic diagnosis of gallbladder perforation. J Ultrasound Med. 1998;17:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 42. | Stefanidis D, Sirinek KR, Bingener J. Gallbladder perforation: risk factors and outcome. J Surg Res. 2006;131:204-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 43. | Kim PN, Lee KS, Kim IY, Bae WK, Lee BH. Gallbladder perforation: comparison of US findings with CT. Abdom Imaging. 1994;19:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 71] [Article Influence: 2.3] [Reference Citation Analysis (0)] |