Published online Jan 27, 2024. doi: 10.4240/wjgs.v16.i1.186
Peer-review started: August 22, 2023
First decision: November 20, 2023
Revised: November 30, 2023
Accepted: December 13, 2023
Article in press: December 13, 2023
Published online: January 27, 2024
Processing time: 156 Days and 1.8 Hours
Prophylactic loop ileostomy is an effective way to reduce the clinical severity of anastomotic leakage following radical resection of rectal cancer. Incisional surgical site infection (SSI) is a common complication after ileostomy closure.
To evaluate the efficacy and safety of the micro-power negative pressure wound technique (MPNPWT) in preventing incisional SSI.
This was a prospective, randomized controlled clinical trial conducted at a single center. A total of 101 consecutive patients who underwent ileostomy closure after rectal cancer surgery with a prophylactic ileostomy were enrolled from January 2019 to December 2021. Patients were randomly allocated into an MPNPWT group and a control group. The MPNPWT group underwent intermittent suturing of the surgical incision with 2-0 Prolene and was covered with a micro-power negative pressure dressing. The surgical outcomes were compared between the MPNPWT (n = 50) and control (n = 51) groups. Risk factors for incisional SSI were identified using logistic regression.
There were no differences in baseline characteristics between the MPNPWT (n = 50) and control groups (n = 51). The incisional SSI rate was significantly higher in the control group than in the MPNPWT group (15.7% vs 2.0%, P = 0.031). However, MPNPWT did not affect other surgical outcomes, including intra-abdominal complications, operative time, and blood loss. Postoperative hospital stay length and hospitalization costs did not differ significantly between the two groups (P = 0.069 and 0.843, respectively). None of the patients experienced adverse effects of MPNPWT, including skin allergy, dermatitis, and pain. MPNPWT also helped heal the infected incision. Our study indicated that MPNPWT was an independent protective factor [odds ratio (OR) = 0.005, P = 0.025)] and diabetes was a risk factor (OR = 26.575, P= 0.029) for incisional SSI.
MPNPWT is an effective and safe way to prevent incisional SSI after loop ileostomy closure.
Core Tip: This is the first study to apply the micro-power negative pressure wound technique (MPNPWT) to postoperative incision for incisional surgical site infection (SSI) prevention. The efficacy and safety of MPNPWT in preventing incisional SSI after ileostomy closure were evaluated. Our study showed that MPNPWT significantly reduced the incisional SSI rate to a low level (2.0%). No patients suffered adverse effects with MPNPWT. MPNPWT is an effective and safe way to prevent incisional SSI after loop ileostomy closure.
- Citation: Xu DY, Bai BJ, Shan L, Wei HY, Lin DF, Wang Y, Wang D. Micro-power negative pressure wound technique reduces risk of incision infection following loop ileostomy closure. World J Gastrointest Surg 2024; 16(1): 186-195
- URL: https://www.wjgnet.com/1948-9366/full/v16/i1/186.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i1.186
Prophylactic loop ileostomy is an effective way to reduce the clinical severity of anastomotic leakage following radical resection for rectal cancer[1]. Afterward, the digestive tract can be reconstructed through ileostomy closure. Although ileostomy closure is technically easy, it is associated with a non-negligible overall morbidity rate (11%-37%), with incisional surgical site infection (SSI) being the most common[2]. Incisional SSI is responsible for increased pain, longer hospital stays, and higher treatment costs. Surgeons have attempted to implement effective techniques to prevent incisional SSI. For example, purse-string skin closure is used as a substitute for conventional linear skin closure[3], and subcutaneous closedsuction drainage or negative-pressure technology (NPT) has been introduced to achieve adequate drainage[4]. These are valid techniques but have some limitations. Purse-string skin closure results in a circular open incision that requires frequent dressing changes. Applying a subcutaneous suction drain or a negative-pressure system has an adverse effect on patient mobility.
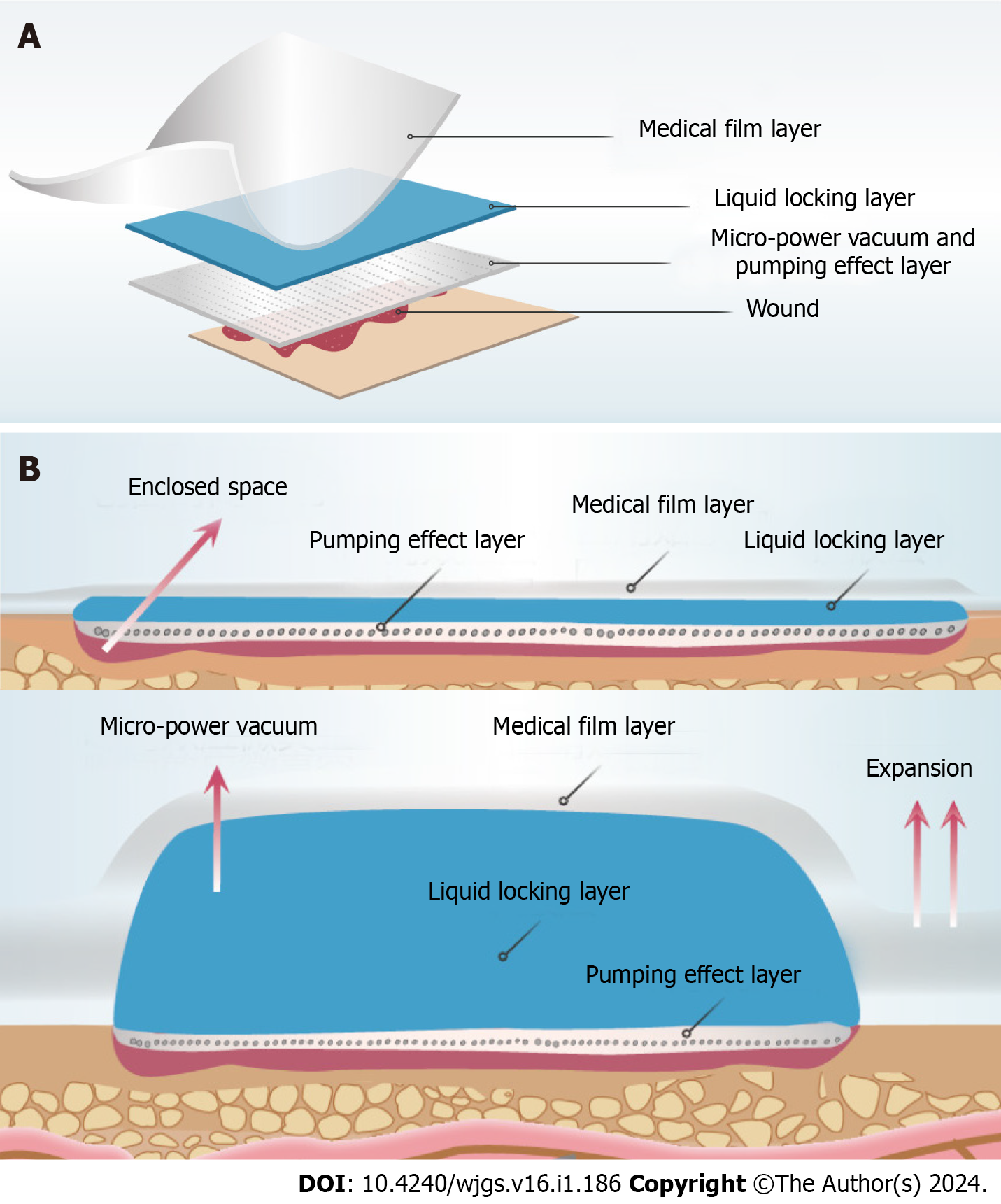
The micro-power negative pressure wound technique (MPNPWT) is a new approach to wound treatment in China[5]. This technique is based on a wound dressing that is made of a special polyvinyl alcohol foam material. When covering the wound, the material is completely sealed with a medical transparent film. Thus, a closed environment is formed at the local wound. Then, this kind of medical, biological material can produce the "siphonic effect" and "pumping effect" through compression, thus generating micro-power negative pressure that can quickly absorb exudates from the wound surface and achieve wound drainage (Figure 1). The micro-power negative pressure dressing can spare frequent dressing changes or an external device. This technique has been successfully applied in wound healing[6-8]. It reduces wound edema and stimulates epithelial cell proliferation and granulation tissue growth, thus shortening wound healing time. However, it is seldom used in the postoperative incisions to prevent incisional SSI. According to our previous experience with MPNPWT in patients with loop ileostomy closure, the postoperative incision could heal satisfactorily.
The primary objective of this prospective, randomized controlled trial (RCT) was to evaluate the efficacy and safety of MPNPWT in preventing incisional SSI after loop ileostomy closure.
This was a single-center prospective, RCT conducted at Sir Run Run Shaw Hospital, Hang Zhou, China, between January 2019 and December 2021. The trial was registered at Chinese Clinical Trial Registry (registration number: ChiCTR
Patients were enrolled according to the following inclusion criteria: (1) Age over 18 years; (2) history of radical resection of a rectal tumor with protective loop ileostomy; (3) scheduled to undergo an elective procedure of ileostomy closure; and (4) provision of signed informed consent. The exclusion criteria were as follows: (1) Age < 18 years; (2) loop ileostomy due to other surgeries; (3) end ileostomy; (4) emergency surgery; (5) other surgical procedures performed during the ileostomy period; and (6) no provision of informed consent. Patients can withdraw from the study without any reason or condition. The enrolled patients were randomly assigned to either an MPNPWT or a control group using sealed envelopes.
The sample size calculation was based on an unpublished prospective observational study conducted at our center, in which 38 patients were evaluated for incision SSI after ileostomy. The overall incidence of incisional SSI was 10.5%. Incisional SSI occurred in four of the 25 patients (16%) in the control group, while no incisional SSI was observed in 13 patients using MPNPWT (incisional SSI incidence was 0). A total of 44 patients were required in each group to achieve a type I error of 0.05 with a power of 0.8. Assuming a 10% dropout rate, the expected 50 patients were recruited in each arm, with a sample size of 100 patients.
An independent statistician randomly assigned eligible patients in a 1:1 ratio using sequentially sealed envelopes to the control or MPNPWT groups without stratification. Randomization was done after admission to the hospital and before ileostomy closure. The sealed envelopes contained allocations from a computer-generated table of random numbers and were opened before surgery. This study did not permit the use of blinding methods because the application of the MPNPWT could not be concealed. However, the analysis was done by a blinded statistician.
Each patient underwent the same procedure of ileostomy closure at the Department of Colorectal Surgery, Sir Run Run Shaw Hospital. During the operation, the ileum was reconstructed with mechanical side-to-side anastomosis using an easyEndoTM endoscopic linear cutter stapler (60 mm length, blue cartridge). Hand-sewn end-to-end anastomosis can also be chosen. All patients received reinforcement sutures for anastomotic stoma. The fascia of the rectus abdominis muscle was closed using continuous suturing. The subcutaneous tissues were not sutured. The skin was intermittently sutured with 2–0 Prolene in both groups. Needle spacing was 6–8 mm in the control group and 10–12 mm in the MPNPWT group. A micro-power negative pressure dressing (MJ-01B3, Guangdong Meiji Biotechnology Co. Ltd.) was filled on the skin surface of the patients in the MPNPWT group by nurses from the wound care clinic. As displayed in Figure 2, the incision was covered with two pieces of polyvinyl alcohol foam material and then sealed and fixed with a transparent film. The material expanded as it absorbed exudates. The dressing was removed after 72 h. If excessive exudates caused negative pressure failure, the dressing was removed earlier and changed to a new one.
Cefmetazole was administered intravenously as a preoperative prophylactic antibiotic. Etimicin sulfate was injected in patients allergic to penicillin or cephalosporin. Typically, the same antibiotics were used postoperatively until the C-reactive protein dropped below 50 mg/L (usually three continuous days). If there was other evidence of infection, the type and duration of antibiotics were adjusted according to clinical experience. In the experimental group, the micro-power negative-pressure dressing was maintained for 72 h and then changed to a traditional dressing material. The negative pressure dressing should be replaced if there was excessive leakage or if the negative pressure failed within 72 h. In the control group, the traditional dressing material was routinely changed in 72 h. In addition, the dressing was changed whenever it became wet. The stitches were removed 2 wk after surgery in both groups. The patients were followed for 30 d postoperatively. The surgical wounds were routinely monitored by the surgical team for 30 d.
The primary outcome of this study was incisional SSI. The infection occurred within 30 d after the operation and involved only the skin or subcutaneous tissue of the incision. It was defined according to the standard of the Center for Disease Control and Prevention (1999)[9], following at least one of the criteria: Purulent drainage, with or without positive culture; laboratory confirmation of the incision exudate; or any one of the following signs or symptoms of infection: Pain or tenderness, localized swelling, and redness or heat.
Continuous variables with a normal or non-normal distribution are presented as the mean ± SD or median and 25th–75th percentiles, respectively. Continuous variables were compared using Student's t-test or Mann–Whitney U test. Categorical variables were compared using Pearson's chi-squared test or Fisher's exact test. Logistic regression was used to detect risk factors for incisional SSI. Statistical significance was set at P < 0.05. The data were statistically analyzed using SPSS software (version 25.0.0.2; SPSS Inc., Chicago, IL, United States).
This study enrolled 101 consecutive patients: 51 in the control group and 50 in the MPNPWT group (Figure 3). Table 1 displays no significant differences in the demographic and clinical features of the patients between the two groups. Most enrolled patients were male (65.3%). Most patients were in good health, with an average body mass index within the normal range for Chinese people (18.5–24). The majority had an American Society of Anaesthesiology (ASA) score of 1-2 (96.0%), with normal values of preoperative albumin and hemoglobin. There were no significant differences in the medical history, including hypertension and diabetes, between the two groups. Since a considerable proportion of patients received perioperative chemoradiotherapy, the waiting time until ileostomy closure was almost 6 mo.
| Variable | Control group (n = 51) | MPNPWT group (n = 50) | P value |
| Gender, n (%) | 0.487 | ||
| Male | 34 (66.7) | 30 (60.0) | |
| Female | 17 (33.3) | 20 (40.0) | |
| Age (yr) | 64.43 ± 9.06 | 61.66 ± 14.22 | 0.247 |
| BMI (kg/m2) | 21.82 ± 2.90 | 22.61 ± 3.06 | 0.184 |
| Hypertension, n (%) | 22 (43.1) | 19 (38.0) | 0.599 |
| Diabetes, n (%) | 7 (13.7) | 8 (16.0) | 0.748 |
| ASA score, n (%) | 0.362 | ||
| 1-2 | 50 (98.0) | 47 (94.0) | |
| 3 | 1 (2.0) | 3 (6.0) | |
| HB (g/L) | 130.78 ± 14.67 | 132.36 ± 13.32 | 0.573 |
| Albumin (g/L) | 43.10 ± 4.00 | 43.95 ± 3.75 | 0.275 |
| Perioperative, n (%), CRT | 32 (62.7) | 27 (54.0) | 0.373 |
| Parastomal hernia, n (%) | 7 (13.7) | 5 (10.0) | 0.563 |
| Time duration from ileostomy to closure (mo) | 6.13 ± 2.45 | 5.51 ± 2.67 | 0.232 |
We compared the surgical outcomes between the two groups to evaluate the efficacy and safety of MPNPWT. The surgical outcomes did not differ significantly between them (Table 2). These two different surgical procedures shared similar operative time (78.14 ± 20.02 vs 81.36 ± 17.64, P = 0.393) and blood loss (17.35 ± 4.40 vs 19.70 ± 7.45, P = 0.056) in the control and MPNPWT groups. Moreover, postoperative intra-abdominal complications, including anastomotic inflammation and bowel obstruction, did not differ significantly between the two groups. No anastomotic leakage or bleeding was observed in either group. The patients complained of no pain or discomfort with a micro-power negative pressure dressing. In addition, in the MPNPWT group, no patients had skin allergy or dermatitis potentially caused by the micro-power negative pressure dressing. The above evidence indicates that MPNPWT is a safe procedure without side effects on ileostomy closure.
| Variable | Control group (n = 51) | MPNPWT group (n = 50) | P value |
| Operative time (min) | 78.14 ± 20.02 | 81.36 ± 17.64 | 0.393 |
| Blood loss (mL) | 17.35 ± 4.40 | 19.70 ± 7.45 | 0.056 |
| Complications, n (%) | |||
| Anastomotic inflammation | 3 (5.9) | 0 (0.0) | 0.243 |
| Bowel obstruction | 3 (5.9) | 5 (10.0) | 0.487 |
| Incisional SSI, n (%) | 8 (15.7) | 1 (2.0) | 0.031 |
| Postoperative hospital stays (d) | 8.51 ± 4.03 | 7.34 ± 2.06 | 0.069 |
| Hospitalization costs (yuan) | 26168.84 ± 6627.74 | 26419.4 ± 6019.23 | 0.843 |
Importantly, the incisional SSI rate was significantly lower in the MPNPWT group than in the control group (2.0% vs 15.7%, P = 0.031). In the MPNPWT group, only one patient developed SSI on postoperative day 5. However, eight patients in the control group experienced incisional SSI within 9 d after surgery. Three patients underwent MPNPWT after opening the infected incision. The incisions were then cleaned and subsequently closed. In addition, there were 15 patients with a medical history of diabetes. The incisional SSI rate among diabetic patients was lower in the MPNPWT group (1/8) than in the control group (3/7), but the difference was not statistically significant (12.5% vs 42.9%, P = 0.282). Postoperative hospital stay length and hospitalization cost did not differ significantly between the two groups (P = 0.069 and 0.843, respectively).
Logistic regression was performed to identify the risk factors associated with incisional SSI. Table 3 shows that those patients who underwent ileostomy closure with MPNPWT had a significantly lower incisional SSI rate than those who underwent traditional procedures [odds ratio (OR) = 0.110, P = 0.041)]. Moreover, patients with diabetes were more likely to suffer incisional SSI (OR = 5.891, P = 0.017). Multivariate analysis further confirmed that MPNPWT was an independent protective factor (OR = 0.005, P = 0.025) and diabetes was a risk factor (OR = 26.575, P = 0.029) for incisional SSI.
| Variable | Univariate | Multivariate | ||
| OR (95%CI) | P value | OR (95%CI) | P value | |
| Female gender | 0.465 (0.091–2.367) | 0.357 | ||
| Age (yr) | 1.034 (0.965–1.107) | 0.343 | ||
| BMI (kg/m2) | 1.115 (0.929–1.337) | 0.241 | ||
| ASA score 3 | 3.708 (0.345–39.908) | 0.28 | ||
| Hypertension | 3.257 (0.765–13.863) | 0.11 | ||
| Diabetes | 5.891 (1.371–25.311) | 0.017 | 26.575 (1.391–507.694) | 0.029 |
| HB (g/L) | 0.967 (0.921–1.016) | 0.189 | ||
| Albumin (g/L) | 1.053 (0.883–1.254) | 0.567 | ||
| MPNPWT | 0.110 (0.013–0.913) | 0.041 | 0.005 (0.000–0.515) | 0.025 |
| Perioperative CRT | 0.880 (0.222–3.492) | 0.855 | ||
| Blood loss (mL) | 1.010 (0.910–1.122) | 0.849 | ||
| Operative time (min) | 1.007 (0.973–1.043) | 0.677 | ||
Incisional SSI is the main complication of loop ileostomy closure. In the present study, we introduced a new technique, MPNPWT, to prevent postoperative incision infection after loop ileostomy closure. This technique significantly reduced the incisional SSI rate to a low level (2.0%).
Surgical incisions are classified into four classes. Class I or class II wounds are clean or relatively clean, with an infection risk of < 2% or < 10%, respectively[10]. Although the surgical incision for ileostomy closure is a class II wound, the incisional SSI rate is much higher than those of other intestinal surgeries, ranging from 2% to 40%[11-13]. In this study, the incisional SSI rate in the control group was also higher than 10%. Adequate drainage is the most effective way to deal with an infected or potentially infected incision and can greatly reduce the incisional SSI rate[14]. Current methods for incisional SSI prevention involve increasing drainage, including subcutaneous suction drainage, negative-pressure system, and purse-string skin closure. However, each of these technologies has its limitations.
MPNPWT is a new technique that has been improved by the NPT. It does not require the configuration of external negative pressure equipment, whether connected to the wall or portable. The suction efficiency of traditional NPT depends on pressure regulation. If the negative pressure is too low, it may be unable to absorb the effusion effectively, yet if it is too high, it may cause tissue damage. Moreover, high pressure may induce the exfoliation of regenerative cells in the wound[15]. However, MPNPWT uses a special material that produces micro-negative pressure by absorbing exudates rather than a suction device. The material expands when the exudates are absorbed. Then, the medical film is gradually elevated, leading to a larger closed space and local vacuum, resulting in a negative pressure suction effect. The suction mechanism is different from the capillary action caused by the adhesive and cohesive forces interacting between the liquid and the surface. Due to the unique design of the material, the more exudates it absorbs, the more powerful the micro-negative pressure. Obviously, excess exudates can invalidate the negative pressure. Meanwhile, it only maintains a relatively low pressure (–0.1 to –0.3 kPa) that may not cause tissue damage. Consequently, MPNPWT can be used to prevent incisional infection because it works on incisions with exudates. The liquid-locking layer of the material has a high liquid absorption efficiency. According to the test, a material with 7.0 cm × 10 cm × 0.1 cm dimension can absorb and preserve up to 70 mL of liquid[6]. After applying MPNPWT to the incision, the exudate may be quickly absorbed by the liquid-locking layer, thereby keeping the incision clean. In the MPNPWT group, we used 2–0 Prolene to close the incision with a wide needle distance so that the micro-negative pressure could effectively absorb the effusion and create a favorable condition for incision healing.
In this study, the MPNPWT group had a 2.0% incisional SSI rate, which was significantly lower than that of the control group. Moreover, MPNPWT may be superior to other techniques in preventing incision infection[3,13,16-18]. Serracant et al[13] inserted contralateral drainage into the subcutaneous space to reduce the incisional SSI rate after loop ileostomy closure, achieving an 8.6% rate in 35 patients. Wierdak et al[18] designed a RCT to assess the role of prophylactic negative-pressure wound therapy in preventing wound healing complications. In that study, negativepressure wound therapy reduced the incidence of SSI to 5.71%. Another study by Lee et al[3] introduced a purse-string skin closure in which a circular suture was performed on the dermal layer with absorbable sutures. Purse-string skin closure contributed to a significantly lower wound infection rate (5.6%) than conventional linear skin closure. Although the incisional SSI rate may vary among studies, it is presumed that MPNPWT is a more efficient and convenient technique. A recent RCT study recruited patients undergoing reoperative open colorectal resections to investigate the effect of NPT on SSIs[19]. The results indicated that the 30-d SSI rate did not differ significantly between the NPT group and control groups (9.4% vs 14.1%, P = 0.28). Therefore, that study concluded that NPT was unrelated to a significant reduction in SSI. There were several reasons for this contradictory conclusion. First, the high SSI rate in the NPT group could be explained by the selection criteria that included high-risk factors for SSI. Second, we have noticed that the incision was closed with skin staples in that study. Generally, the needle spacing of skin staples was narrower than that of Prolene, which might lead to poor drainage. Moreover, the narrow needle spacing would cause the epidermis to heal earlier than the subcutaneous tissue, which might prevent NPT from absorbing exudates. Therefore, our MPNPWT accompanied with wider needle spacing would be more effective for incisional SSI.
Several factors are associated with incisional SSI, such as ASA score and operative time[9]. Diabetes is likely to induce poor wound healing. Our results demonstrated that diabetes was an independent risk factor for incisional SSI. Moreover, MPNPWT could decrease the incisional SSI rate in diabetic patients. Additionally, MPNPWT was appropriate for infected incisions. Patients with MPNPWT spared the trouble of dressing change and suffered less pain than patients with open incisions. Previous studies have confirmed the efficacy of MPNPWT in open wounds such as diabetic foot, open fracture, and burn wounds[6,8]. Notably, MPNPWT is not recommended for wounds with excessive exudates because of the special mechanism of this material.
In our center, we do not choose subcutaneous suction drainage or purse-string skin closure to prevent incisional SSI. We believe that these techniques are cumbersome and increase patient suffering. In contrast, MPNPWT is simple and convenient. It can be performed in a post-anesthesia care unit by a wound care clinic at our center or performed by trained surgeons during the surgery. Furthermore, we confirmed that MPNPWT is safe. Specifically, patients in the MPNPWT group did not suffer from skin allergy, dermatitis, or any pain. In addition, MPNPWT did not affect hospitalization costs (P = 0.843). Moreover, MPNPWT shortened the length of hospital stays to a certain extent, though not significantly. Surgical outcomes such as operative time, hospitalization cost, and length of hospital stay are important factors associated with patient recovery and feelings. Previous studies have often lacked investigations into these aspects. Lee et al[3] reported that the median hospitalization period in the purse-string skin closure group was 7 d, which was significantly shorter than that in the linear skin closure group. However, according to our center's experience, it takes longer than 7 d to heal the incision with purse-string skin closure, implying that patients still need dressing changes even after hospital discharge.
The main limitation of this study was that it was a single-center clinical trial with a relatively small sample size. In addition, needle spacing was different between the two groups, which may be a bias when analyzing the effectiveness of MPNPWT. Finally, some other less significant confounders that were not recorded in our study may have introduced bias. A larger multicenter clinical study with a better design should be conducted in the future.
As a prospective RCT, our study introduced a novel technique, MPNPWT, to prevent incisional SSI after loop ileostomy closure. MPNPWT reduces the incidence of incisional SSI and helps patients recover during hospitalization.
Although ileostomy closure is technically easy, it is associated with a non-negligible overall morbidity rate (11%-37%), with incisional surgical site infection (SSI) being the most common.
The incisional SSI rate after ileostomy closure is much higher than those of other intestinal surgeries, ranging from 2% to 40%. Incisional SSI is responsible for increased pain, longer hospital stays, and higher treatment costs. Current methods for incisional SSI prevention have limitations. Finding a new approach to prevent incisional SSI is urgent for patients receiving ileostomy closure.
Micro-power negative pressure wound technique (MPNPWT) contains a special material that produces micro-negative pressure by absorbing exudates rather than suction device. It reduces wound edema and stimulates epithelial cell proliferation and granulation tissue growth, thus shortening wound healing time. This study aimed to evaluate the efficacy and safety of MPNPWT in preventing incisional SSI. The results of our study will provide foundation for future application of MPNPWT.
This was a single-center, prospective, randomized controlled trial (RCT). An independent statistician randomly assigned eligible patients in a 1:1 ratio using sequentially sealed envelopes to a control group or an MPNPWT group without stratification. Micro-power negative pressure dressing was filled on the skin surface of patients in the MPNPWT group by nurses from wound care clinic.
MPNPWT significantly reduced incisional SSI rate (2.0%). MPNPWT is a safe technique without any side effect. MPNPWT could also help heal the infected incision.
Our study introduces a novel technique, MPNPWT, to prevent incisional SSI after loop ileostomy closure. MPNPWT reduces the incidence of incisional SSI after loop ileostomy closure.
A larger RCT with a larger sample is the direction of the future research.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Komatsu S, Japan S-Editor: Lin C L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Mrak K, Uranitsch S, Pedross F, Heuberger A, Klingler A, Jagoditsch M, Weihs D, Eberl T, Tschmelitsch J. Diverting ileostomy versus no diversion after low anterior resection for rectal cancer: A prospective, randomized, multicenter trial. Surgery. 2016;159:1129-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 99] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 2. | Akiyoshi T, Fujimoto Y, Konishi T, Kuroyanagi H, Ueno M, Oya M, Yamaguchi T. Complications of loop ileostomy closure in patients with rectal tumor. World J Surg. 2010;34:1937-1942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Lee JR, Kim YW, Sung JJ, Song OP, Kim HC, Lim CW, Cho GS, Jung JC, Shin EJ. Conventional Linear versus Purse-string Skin Closure after Loop Ileostomy Reversal: Comparison of Wound Infection Rates and Operative Outcomes. J Korean Soc Coloproctol. 2011;27:58-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Fukuoka K, Koyama F, Kuge H, Obara S, Nakamoto T, Iwasa Y, Takei T, Matsumoto Y, Sadamitsu T, Sho M. A combination of subcuticular sutures and subcutaneous closed-suction drainage reduces the risk of incisional surgical site infection in loop ileostomy closure. Surg Today. 2021;51:605-611. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Zheng XP, Chen J, Chen TS, Jiang YN, Shen T, Xiao SC, Hu XY. [Preliminary effect observation on the application of micro-negative pressure in children with small-area deep partial-thickness burn]. Zhonghua Shao Shang Za Zhi. 2019;35:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Liu XB, Pan BH, Li HH, Wang KA, Xu DY, Sun Y, Zhu SH. Clinic effects of micro-dynamic negative pressure wound technique on deep partial burn wounds in infants and young children. Zhonghua Sunshangyuxiufu Zazhi (Dianziban). 2016;11:346-349. |
| 7. | Ma CH, Hu X, Cheng GB, Zhu XS. Study on formation process of vacuum negative pressure of micro power negative pressure technology. Yiliao Weisheng Zhuangbei. 2017;38:25-27. |
| 8. | Bo Z, Chen XL, Cheng H, Fang X, Liu S, Wang F, Wang C, Qiu L. Effect of micropower vacuum dressings on the healing of rabbit second degree burn wound. Zhonghua Sunshangyuxiufu Zazhi (Dianziban). 2015;10:103-106. |
| 9. | Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250-78; quiz 279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2944] [Cited by in RCA: 2797] [Article Influence: 107.6] [Reference Citation Analysis (0)] |
| 10. | Cruse PJ, Foord R. The epidemiology of wound infection. A 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 979] [Cited by in RCA: 850] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 11. | Lahat G, Tulchinsky H, Goldman G, Klauzner JM, Rabau M. Wound infection after ileostomy closure: a prospective randomized study comparing primary vs. delayed primary closure techniques. Tech Coloproctol. 2005;9:206-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Milanchi S, Nasseri Y, Kidner T, Fleshner P. Wound infection after ileostomy closure can be eliminated by circumferential subcuticular wound approximation. Dis Colon Rectum. 2009;52:469-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Serracant A, Serra-Aracil X, Mora-López L, Pallisera-Lloveras A, Serra-Pla S, Zárate-Pinedo A, Navarro-Soto S. The Effectiveness of Contralateral Drainage in Reducing Superficial Incisional Surgical Site Infection in Loop Ileostomy Closure: Prospective, Randomized Controlled Trial. World J Surg. 2019;43:1692-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Scalise A, Calamita R, Tartaglione C, Pierangeli M, Bolletta E, Gioacchini M, Gesuita R, Di Benedetto G. Improving wound healing and preventing surgical site complications of closed surgical incisions: a possible role of Incisional Negative Pressure Wound Therapy. A systematic review of the literature. Int Wound J. 2016;13:1260-1281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 157] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 15. | Upton D, Andrews A. Pain and trauma in negative pressure wound therapy: a review. Int Wound J. 2015;12:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Li LT, Hicks SC, Davila JA, Kao LS, Berger RL, Arita NA, Liang MK. Circular closure is associated with the lowest rate of surgical site infection following stoma reversal: a systematic review and multiple treatment meta-analysis. Colorectal Dis. 2014;16:406-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Haase O, Raue W, Böhm B, Neuss H, Scharfenberg M, Schwenk W. Subcutaneous gentamycin implant to reduce wound infections after loop-ileostomy closure: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum. 2005;48:2025-2031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Wierdak M, Pisarska-Adamczyk M, Wysocki M, Major P, Kołodziejska K, Nowakowski M, Vongsurbchart T, Pędziwiatr M. Prophylactic negative-pressure wound therapy after ileostomy reversal for the prevention of wound healing complications in colorectal cancer patients: a randomized controlled trial. Tech Coloproctol. 2021;25:185-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 19. | Sapci I, Camargo M, Duraes L, Jia X, Hull TL, Ashburn J, Valente MA, Holubar SD, Delaney CP, Gorgun E, Steele SR, Liska D. Effect of Incisional Negative Pressure Wound Therapy on Surgical Site Infections in High-Risk Reoperative Colorectal Surgery: A Randomized Controlled Trial. Dis Colon Rectum. 2023;66:306-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |