Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1159
Peer-review started: February 21, 2023
First decision: March 21, 2023
Revised: March 24, 2023
Accepted: April 28, 2023
Article in press: April 28, 2023
Published online: June 27, 2023
Processing time: 111 Days and 7.4 Hours
The case of Crohn's disease involving the duodenum is rare, and its surgical management requires a thorough understanding.
To investigate the surgical management of duodenal Crohn’s disease.
We systematically reviewed patients diagnosed with duodenal Crohn's disease who underwent surgery in the Department of Geriatrics Surgery of the Second Xiangya Hospital of Central South University from January 1, 2004, to August 31, 2022. The general information, surgical procedures, prognosis, and other information of these patients were collected and summarized.
A total of 16 patients were diagnosed with duodenal Crohn’s disease, where 6 cases had primary duodenal Crohn’s disease, and 10 had secondary duodenal Crohn’s disease. Among patients with primary disease, 5 underwent duodenal bypass and gastrojejunostomy, and 1 received pancreaticoduodenectomy. Among those with a secondary disease, 6 underwent closure of duodenal defect and colectomy, 3 received duodenal lesion exclusion and right hemicolectomy, and 1 underwent duodenal lesion exclusion and double-lumen ileostomy.
Crohn's disease involving the duodenum is a rare condition. Different surgical management should be applied for patients with Crohn's disease presenting with different clinical manifestations.
Core Tip: Crohn's disease is a chronic, incurable inflammatory disease that affects the gastrointestinal tract function and causes extraintestinal complications. Crohn's disease involving the duodenum is a rare condition and different surgical management should be applied for patients with Crohn's disease presenting with different clinical manifestations. This study mainly summarized the surgical approaches and prognosis of 16 patients with duodenal Crohn's disease, thus providing some reference for the surgical management of the disease.
- Citation: Yang LC, Wu GT, Wu Q, Peng LX, Zhang YW, Yao BJ, Liu GL, Yuan LW. Surgical management of duodenal Crohn's disease. World J Gastrointest Surg 2023; 15(6): 1159-1168
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1159.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1159
Crohn's disease is a chronic, incurable inflammatory disease that affects the gastrointestinal tract function and causes extraintestinal complications. Its prevalence is rising in adults and children with confirmed genetic susceptibility and is associated with specific environmental factors. Common symptoms include diarrhea, abdominal pain, rectal bleeding, fever, weight loss, and fatigue[1]. More than 50% of the patients have strictures or penetrating complications in the first 10 years after diagnosis. Surgery, followed by biotherapy, immunomodulators, and leukocyte isolation therapy, is the most common treatment method[2]. The stricture-induced intestinal obstruction is one of the common surgical indications, followed by intestinal obstruction, fistula, and abscess formation[3,4]. Chronic inflammation may involve any portion of the gastrointestinal tract; however, it is more common in the terminal ileum and proximal colon while it is rarely observed in the stomach and duodenum. Most cases of duodenal Crohn's disease present as a secondary disease, accounting for about 2% of all Crohn's disease cases[5]. The most common manifestation of gastroduodenal Crohn's disease is stricture, leading to obstructive symptoms. Its diagnostic criteria include typical lesions involving the whole stomach, mucosal abscesses, and sinuses connected with fissures; loose tuberculous-like lesions; no tuberculosis, fungi, foreign bodies, or parasites in the lesions; typical regional enteritis in the small intestine[6]. Treatment of the duodenal Crohn's disease includes proton pump inhibitors and biotherapy. Endo
This study mainly summarized the surgical approaches and prognosis of 16 patients with duodenal Crohn's disease who underwent surgeries in the Department of Geriatric Surgery of the Second Xiangya Hospital of Central South University between January 1, 2004, and August 31, 2022, thus providing some reference for the surgical treatment of the disease.
Data from patients with duodenal Crohn's disease undergoing surgeries in the Department of Geriatric Surgery, the Second Xiangya Hospital of Central South University between January 1, 2004, and August 31, 2022, were reviewed.
Crohn's disease diagnosed according to the Consensus Opinions on the Diagnosis and Treatment of Inflammatory Bowel Disease from the Inflammatory Bowel Disease Group of Gastroenterology Society of Chinese Medical Association in 2018); duodenal lesions have been confirmed by gastroscopy, colonoscopy, computed tomography (CT) and gastrointestinal radiography combined with intrao
Non-Crohn's disease; patients diagnosed with Crohn's disease that was not confirmed by pathology.
Patients’ clinical information, including name, gender, age, type of disease, personal history, clinical manifestations, disease behavior, location of disease, surgical approach, and prognosis was collected and analyzed. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of The Second Xiangya Hospital of Central South University, Approval No. 2022-155 (Approval date: September 28, 2022). Informed consent and consent for publication were obtained from all subjects involved in the study.
Finally, 16 patients (11 males and 5 females) were included in the study, with an average age of 30.25 years and a median age of 30 years (Table 1). All patients had a chronic relapse, and one had a history of smoking. There were 6 cases with diarrhea, 4 cases with nausea and vomiting, and 9 cases with intestinal obstruction. According to Montreal classification, 16 patients were A2 type; lesion location (L): 1 case of L1 + L4 type, 2 cases of L2 + L4 type, 7 cases of L3 + L4 type, 6 cases of L4 type; disease behavior (B): 9 cases of B2 type, 7 cases of B2 + B3 type (Table 2). Almost all the patients were transferred to our department for surgery after treatment in the Department of Gastroenterology and had received one or more treatments, including mesalamine, azathioprine, steroid, anti-tumor necrosis factor (anti-TNF), nutritional support, or anti-inflammatory treatment preoperatively.
| Classification | Sex | Age | Primary site | Manifestation | Surgical approach | Postoperative surgical recurrence |
| Primary | Female | 29 | Duodenum | Stricture | Duodenal bypass and gastrojejunostomy | No |
| Female | 35 | Duodenum | Stricture | Duodenal bypass and gastrojejunostomy | No | |
| Female | 30 | Duodenum | Stricture | Duodenal bypass and gastrojejunostomy | No | |
| Male | 20 | Duodenum | Stricture | Duodenal bypass and gastrojejunostomy | No | |
| Male | 25 | Duodenum | Stricture | Duodenal bypass and gastrojejunostomy | No | |
| Male | 29 | Duodenum | Tumor-like | Pancreaticoduodenectomy | No | |
| Secondary | Male | 26 | Ileocolon | Internal fistula (d = 0.3 cm) | Direct closure of the duodenal defect and right hemicolectomy | No |
| Male | 30 | Ascending colon | Internal fistula (d = 1 cm) | Direct closure of the duodenal defect and subtotal colectomy | No | |
| Female | 20 | Right hemicolon | Internal fistula (d = 1 cm) | Direct closure of the duodenal defect and right hemicolectomy | No | |
| Male | 37 | Right hemicolon | Internal fistula (d = 5.0 cm) | Closure of duodenal defect with pedicled terminal ileum flap, right hemicolectomy | No | |
| Male | 41 | Right hemicolon | Internal fistula (d = 3.5 cm) | Closure of duodenal defect with pedicled terminal ileum flap, right hemicolectomy | No | |
| Male | 32 | Ascending colon | Internal fistula (d = 3.5 cm) | Closure of duodenal defect with pedicled terminal ileum flap and ascending colectomy | No | |
| Female | 23 | Right hemicolon | Without internal fistula | Duodenal lesion exclusion and right hemicolectomy | No | |
| Male | 39 | Ileocolon | Without internal fistula | Duodenal lesion exclusion and right hemicolectomy | No | |
| Male | 32 | Right hemicolon | Without internal fistula | Duodenal lesion exclusion and right hemicolectomy | No | |
| Male | 36 | Ileum | Without internal fistula | Duodenal lesion exclusion and double lumen ileostomy | No |
| Item | Group | Frequency | Constituent ratio (%) |
| Diseased location (L) | L4: Upper gastrointestinal tract | 6 | 38 |
| L1 + L4: Ileum + upper gastrointestinal tract | 1 | 6 | |
| L2 + L4: Colon + upper gastrointestinal tract | 2 | 12 | |
| L3 + L4: Ileocolon + upper gastrointestinal tract | 7 | 44 | |
| Disease behavior (B) | B2: Stenotic type | 9 | 56 |
| B2 + B3: Stenotic penetration type | 7 | 44 |
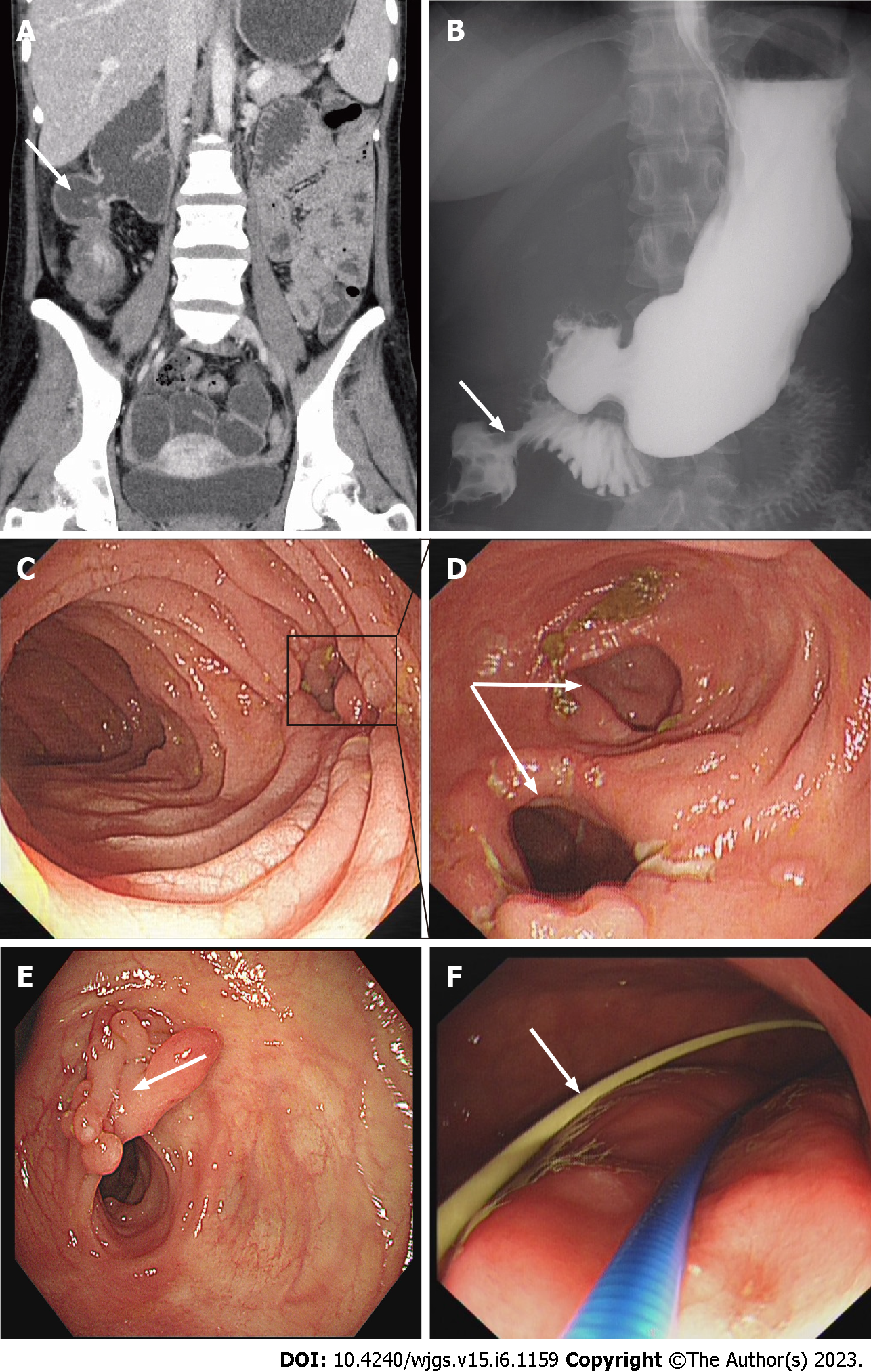
Before the hospitalization, 16 patients had received medical treatment for clinical symptoms: six patients received 5-ASA, two patients received steroid plus azathioprine, three patients received 5-ASA plus steroid plus azathioprine, and five patients received biological agents. All patients had different degrees of incomplete intestinal obstruction before the operation. Partial parenteral nutrition and dietary management were given to most patients with mild obstruction to improve their nutritional status and enhance their ability to withstand surgery. For the five patients with severe duodenal obstruction, balloon dilation and jejunal nutrient tube insertion were attempted in the stenosis segment under the endoscope before surgery. Among the 5 patients, one patient received complete parenteral nutrition due to the severe duodenal stenosis, which made the jejunal nutrition tube unable to cross the stenosis segment. The other four patients were successfully implanted with jejunal nutrition tubes (Figure 1) and received adequate enteral nutrition for 2-3 wk before surgery. All patients were transferred to our department for surgery when they were in good nutritional status, and the disease was in state of remission. Gastroscopy, colonoscopy, CT, and gastrointestinal radiography were performed in our hospital before the operation. The abdominal CT images (Figure 1A) and gastrointestinal radiography (Figure 1B) in 6 patients confirmed the existence of an internal fistula between the duodenum and colon. The internal fistula between the duodenum and colon could be seen under gastroscopy (Figure 1C) and colonoscopy (Figure 1D) in six patients.
Duodenal Crohn's disease included primary and secondary duodenal Crohn's disease. Among 16 patients, there were 6 cases with primary duodenal Crohn's disease (5 cases had duodenal strictures and 1 case had tumor-like lesions) and 10 cases of secondary duodenal Crohn's disease (6 cases had an internal fistula and 4 cases had no internal fistula). All the 16 cases had indications for surgery, without obvious contraindications. Of the 6 patients with primary duodenal Crohn's disease, 5 underwent duodenal bypass and gastrojejunostomy, and 1 underwent pancreatoduodenectomy. Of the 10 patients with secondary duodenal Crohn's disease, 6 underwent duodenal defect closure and diseased intestinal segment resection, 3 underwent duodenal lesion exclusion and right hemicolectomy, and 1 underwent duodenal lesion exclusion and double-lumen ileostomy (Table 1).
To timely manage postoperative complications, all patients need to be hospitalized in the surgical ward for a while after surgery before being transferred to the department of gastroenterology. The duration of this period mainly depends on whether there is an anastomosis in the duodenum and the healing of the anastomosis. In addition, the jejunal nutrition tube across the duodenal anastomosis could enable patients to receive enteral nutrition as early as possible after surgery, which helps to maintain the physiological homeostasis of the intestinal tract and accelerate the postoperative recovery of the body. Furthermore, if obstruction occurred, the customarily secreted gastric juice can be drawn out of the body through the gastrostomy tube to prevent fluid accumulation at the anastomotic site and reduce the risk of duodenal anastomotic leakage as much as possible. All patients had no severe complications and were successfully transferred to the department of gastroenterology for follow-up treatment. Eight patients continued to receive anti-TNF four weeks after the operation, seven patients received 5-ASA maintenance therapy, and one patient who underwent pancreaticoduodenectomy did not receive appropriate medical treatment. Due to the high postoperative recurrence rate of Crohn's disease, active follow-up was carried out for all the patients. All patients received a follow-up period of at least 6 mo, and the most extended follow-up period was about 18 years. All patients received the serological examination (Table 3) and abdominal CT examination three months after the operation, and digestive tract endoscopy six months after the procedure, and no sign of clinical recurrence was found. The patient who underwent pancreaticoduodenectomy developed severe fatty diarrhea two years after the operation and received pancreaticojejunostomy that year. Still, the effect of the process was poor, which seriously affected the patient's quality of life.
| mean ± SD | Pre-operation | Post-operation | |||
| Day 1 | Day 3 | Day 7 | The 3rd month | ||
| WBC (× 109/L) | 7.38 ± 4.44 | 16.36 ± 7.47 | 7.06 ± 2.36 | 5.56 ± 3.10 | 5.38 ± 1.09 |
| NEUT% | 67.32 ± 21.31 | 88.62 ± 4.06 | 74.11 ± 10.83 | 67.27 ± 12.37 | 67.44 ± 7.79 |
| PLT (× 109/L) | 394 ± 191.73 | 335 ± 181.17 | 273 ± 95.04 | 294 ± 96.90 | 253 ± 55.52 |
| HGB (g/L) | 107 ± 23.30 | 108 ± 27.61 | 100 ± 25.27 | 101 ± 21.16 | 128 ± 18.84 |
| ESR (mm/h) | 41.60 ± 30.59 | 20.50 ± 14.85 | 72.67 ± 27.15 | 22.00 ± 16.97 | 6.61 ± 4.22 |
| CRP (mg/L) | 34.56 ± 42.57 | 39.58 ± 23.74 | 85.47 ± 87.36 | 39.75 ± 38.52 | 1.91 ± 1.18 |
| PCT (ng/mL) | 0.07 ± 0.05 | 0.24 ± 0.24 | 1.52 ± 2.05 | 0.26 ± 0.14 | 0.02 ± 0.01 |
| ALB (g/L) | 31.31 ± 10.45 | 30.77 ± 6.48 | 32.11 ± 4.17 | 34.12 ± 4.53 | 41.71 ± 3.12 |
| BMI (kg/m2) | 15.90 ± 2.31 | NA | NA | NA | 20.83 ± 1.69 |
Duodenal strictureplasty: Resection anastomosis of duodenal stricture is suitable for horizontal or ascending duodenal strictures. End-to-end, end-to-side, or side-to-side anastomosis and early drug treatment should be used to prevent recurrence and secondary strictures. Strictureplasty, which was first performed by Lee and Papiaoannu in the 1970s, is a safe and effective surgical approach for treating duodenal Crohn's disease[8]. Strictureplasty may be suitable when the second or third portion of the duodenum is stenotic in less than two sites. For multiple strictures located in the first or distal duodenum, resection should be used as the first option[9]. There are various types of strictureplasty; the most commonly used duodenal CD strictureplasty is Heineke Mikulicz strictureplasty for strictures less than 10 cm in length and Finney strictureplasty for a longer segment of 15 to 25 cm in length[10]. In jejunoileal CD, strictureplasty is a recognized surgical technique that can relieve symptoms of obstruction, maintain intestinal length, and avoid the occurrence of short bowel syndrome[4]. Strictureplasty can treat the strictures caused by CD involving the duodenum and may be an option for the treatment of Oddi sphincter incontinence in primary duodenal Crohn's disease[11].
Duodenal stricture bypass surgery: Loop gastrojejunostomy and Roux-en-Y gastrojejunostomy are widely used to treat duodenal Crohn's disease. Racz et al[11] reported a case of duodenal Crohn's disease and found that descending, horizontal and ascending segments of the duodenum were significantly stenotic intraoperatively. Duodenojejunostomy and gastrojejunostomy were then performed, and the patients recovered well after surgery. Based on surgical treatment of duodenal Crohn's disease at our department, 5 patients underwent the bypass procedure and gastrojejunostomy; all patients recovered well after surgery. The advantage of the duodenal bypass procedure is that it excludes the duodenal strictures and reconstructs the patency and continuity of the gastrointestinal tract. Yet, duodenal bypass is also associated with complications and risks such as gastric emptying disorder, disease progression of duodenal bypass location, non-biopsy of bypass site, ulcer formation, anastomotic restructure, and so on.
Currently, the best surgical approach for duodenal Crohn’s disease is still a matter of debate. Yamamoto et al[12] suggested that duodenal bypass is better than duodenal strictureplasty when treating patients with duodenal Crohn’s disease, while Worsey et al[8] reported different results. Some studies suggested a combination of surgical resection, bypass, and strictureplasty, which maximizes the protection of the intestinal tract and allows complete remission of symptoms[11]. We believe that the surgical approach should be based on the location and degree of Crohn's disease in combination with the operation level and clinical experience of the surgeon.
Pancreaticoduodenectomy: Gastroduodenoplasty, strictureplasty, and Roux-en-Y bypass are considered effective surgical treatments for duodenal Crohn's disease. If technically feasible, it can be used to treat the strictures of the second and third portions of the duodenum with strictureplasty. Duodenectomy or pancreatoduodenectomy should be regarded as the final surgical treatment option for the disease[13]. For primary duodenal stricture with tumor-like manifestations, the surgical approach should be selected based on the location and degree of the lesion. The surgical approach can include segmental duodenectomy, partial duodenectomy, or pancreatoduodenectomy. Among patients with primary duodenal Crohn's disease receiving surgical treatment in our department, one case presented with a tumor-like lesion, which was difficult to diagnose intraoperatively. Rapid pathological examination showed a small number of heterogeneous cells; consequently, pancreatoduodenectomy was performed. The postoperative pathological report was Crohn's disease, involving a portion of the pancreas. Later, the patient developed fat diarrhea and underwent pancreaticojejunostomy, but the effect of postoperative treatment was poor. This case indicated that surgery can only solve the surgical complications of Crohn's disease, and the patients still needed standardized medical treatment. We also suggest caution in choosing pancreatoduodenectomy for primary duodenal Crohn's disease.
Other surgical approaches: In addition to duodenal strictureplasty and duodenal bypass, other procedures for the primary duodenal Crohn's disease include duodenal balloon dilatation, endoscopic stricture incision, and self-expanding metal stent[14]. Previous studies have shown that the short-term technical and clinical success rate of balloon dilatation for upper gastrointestinal Crohn's disease-related stricture is high, the long-term curative effect is relatively good, and the incidence of postoperative complications is acceptable. Although continuous balloon dilatation does not change the curative effect, it may be a feasible option to delay or prevent surgery[15].
In addition to primary duodenal Crohn's disease, Crohn's disease in other organs, such as the colon, and small intestine, can also involve the duodenum, leading to duodenal lesions, which is named secondary duodenal Crohn's disease in the clinic. In this study, 10 cases had secondary duodenal Crohn's disease, including 6 cases with and 4 cases without internal fistula. The formation of the internal fistula is one of the important factors in determining the surgical approach.
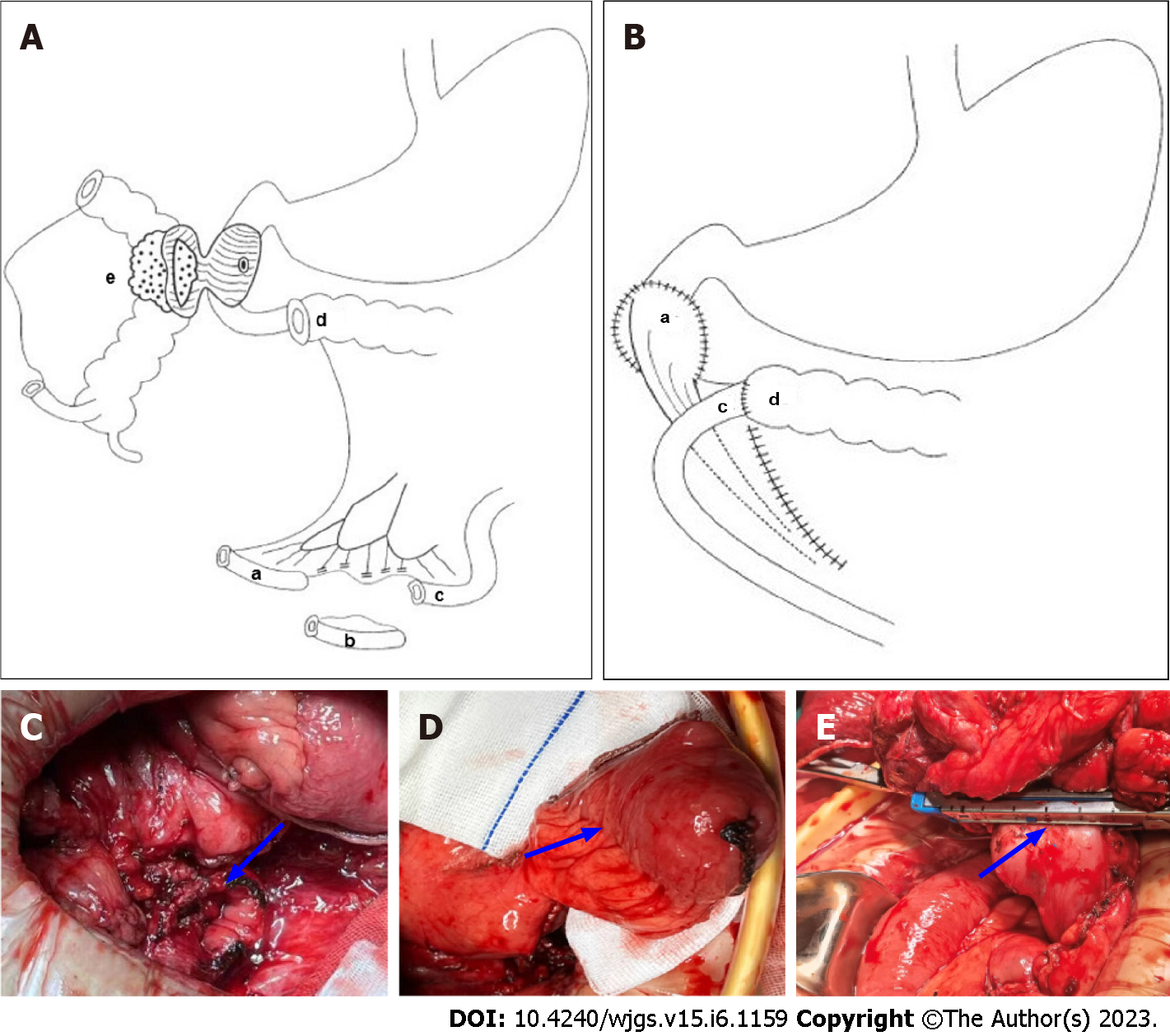
Surgical approach of secondary duodenal Crohn's disease with internal fistula: Gong et al[16] suggested that one-stage duodenal closure is safe for Crohn's disease as long as there is no duodenal stricture, and that it may even be used for large duodenal defects. Our data suggest that pathological segmental resection and internal fistula resection should be used for cases with intestinal penetration that eventually involve the duodenum and form internal fistula, while duodenal closure should be applied according to the circumstances. For patients with Crohn's disease complicated with duodenal fistula, the treatment should be based on surgery, while special attention should be paid to perioperative management, induction of remission through drug and nutrition treatment, and selection of the appropriate time to intervene by surgery. Once the duodenum is seriously involved and forms an internal fistula with other intestines, it is often necessary to close the duodenal defects. According to the size of duodenal defects, different closure techniques are used. Among 10 cases of secondary duodenal Crohn's disease in our department, 6 cases (3/5) had internal fistula formation. We summarized the basic information, including primary lesion location, duodenal defect size, and the surgical approach in Table 1. Three cases underwent direct duodenal closure and 3 duodenal closures with pedicled terminal ileal flap. Direct closure of duodenal defects was performed when the duodenal defect was ≤ 3 cm in diameter (Figure 2). When the duodenal defect was larger than 3cm in diameter, duodenal stricture could easily occur after simple closure of the defect or suture, after which pedicled flap closure of the duodenal defect was performed (Figure 2A-D)[17-19].
The main surgical approaches for duodenal defect closure include direct closure, pedicled intestinal flap closure, and sometimes additional gastrostomy and jejunal nutrition tube implantation, depending on the situation. Among 6 patients with duodenal defect closure, 4 patients had additional gastrostomy, 4 patients had an additional ileostomy, 4 patients had additional jejunal nutrition tube implantation, and 1 patient received additional ileal nutrition tube implantation.
Surgical approach of secondary duodenal Crohn's disease without internal fistula: Secondary duodenal Crohn's disease usually appears secondary to the colon, ileum, and other primary lesions. Although the duodenum is involved, there is no internal fistula or duodenal stricture. For patients with duodenal involvement but no obvious clinical manifestations, individualized surgical treatment should be performed according to the lesion location, lesion degree, duodenal fistula formation, and duodenal strictures.
Among 16 cases, there were 4 cases of secondary duodenal Crohn's disease without internal fistula, including 3 cases of duodenal lesion exclusion and right hemicolectomy. When other diseases involve the duodenum without the formation of an internal fistula, and when the ascending colon or hepatic flexure of the colon is found to involve the duodenum intraoperatively, the primary diseased intestinal segment can be resected based on our experience, and with the exclusion of duodenal lesion, which is to retain the seromuscular layer of the colon adhering to the duodenum, while removing the mucosa and submucosa of the colon. In addition, we also completed one case of duodenal lesion exclusion and double lumen ileostomy. We believe that the surgical treatment of Crohn's disease is different from that of gastrointestinal cancer. Gastrointestinal malignancies are performed over a limited period of time and require radical resection of diseased tissue, whereas Crohn's disease is benign. For patients with secondary duodenal Crohn's disease without fistula, who usually had poor nutritional status, combined with hypoproteinemia, ascites, bloody exudation, and other conditions, transitional surgery, namely double-lumen ileostomy, was considered first. Deterministic surgery was performed after nutritional support and standardized medical treatment to improve the patient's general condition.
Duodenal Crohn's disease is a rare event that can be classified into primary and secondary duodenal Crohn's disease. Surgical treatment for duodenal Crohn's disease should be performed based on the patient's condition and the surgeon's experience. However, surgery can only solve the surgical complications. Thus, patients should receive standard medical treatment preoperatively and postoperatively to obtain an ideal therapeutic effect. In addition, it is often necessary for various departments such as gastroenterology, gastrointestinal surgery, radiology, pathology, and nutrition to cooperate to fully achieve the unique advantages of comprehensive multidisciplinary treatment[20].
Treating Crohn's disease that affects the duodenum requires a personalized surgical approach that takes into account the patient's individual health status.
The involvement of the duodenum in Crohn's disease is relatively rare, so it is necessary to summarize the surgical management.
Provide surgical treatment recommendations for duodenal Crohn's disease as a reference for surgeons.
We systematically reviewed patients diagnosed with duodenal Crohn's disease who underwent surgery in the Department of Geriatrics Surgery of the Second Xiangya Hospital of Central South University from January 1, 2004, to August 31, 2022.
All patients had a chronic relapse, and one had a history of smoking. There were 6 cases with diarrhea, 4 cases with nausea and vomiting, and 9 cases with intestinal obstruction. Among 16 patients, there were 6 cases with primary duodenal Crohn's disease (5 cases had duodenal strictures and 1 case had tumor-like lesions) and 10 cases of secondary duodenal Crohn's disease (6 cases had an internal fistula and 4 cases had no internal fistula).
Surgical treatment for duodenal Crohn's disease should be performed based on the patient's condition and the surgeon's experience.
The incidence of Crohn's disease has been increasing year by year. This study explores surgical management for duodenal Crohn's disease from the perspective of surgeons.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fanaeian MM, Iran; Fujimori S, Japan S-Editor: Yan JP L-Editor: A P-Editor: Liu JH
| 1. | Veauthier B, Hornecker JR. Crohn's Disease: Diagnosis and Management. Am Fam Physician. 2018;98:661-669. [PubMed] |
| 2. | Ogino T, Mizushima T, Matsuda C, Mori M, Doki Y. Essential updates 2018/2019: Colorectal (benign): Recent updates (2018-2019) in the surgical treatment of benign colorectal diseases. Ann Gastroenterol Surg. 2020;4:30-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Chan WPW, Mourad F, Leong RW. Crohn's disease associated strictures. J Gastroenterol Hepatol. 2018;33:998-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 4. | Yamamoto T, Watanabe T. Surgery for luminal Crohn's disease. World J Gastroenterol. 2014;20:78-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Nugent FW, Richmond M, Park SK. Crohn's disease of the duodenum. Gut. 1977;18:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 94] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Pryse-Davies J. Gastro-Duodenal Crohn's Disease. J Clin Pathol. 1964;17:90-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Lightner AL, Fletcher JG. Duodenal Crohn's Disease-a Diagnostic Conundrum. J Gastrointest Surg. 2018;22:761-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Worsey MJ, Hull T, Ryland L, Fazio V. Strictureplasty is an effective option in the operative management of duodenal Crohn's disease. Dis Colon Rectum. 1999;42:596-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 63] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Tonelli F, Alemanno G, Bellucci F, Focardi A, Sturiale A, Giudici F. Symptomatic duodenal Crohn's disease: is strictureplasty the right choice? J Crohns Colitis. 2013;7:791-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Fichera A, Hurst RD, Michelassi F. Current methods of bowel-sparing surgery in Crohn's disease. Adv Surg. 2003;37:231-251. [PubMed] |
| 11. | Racz JM, Davies W. Severe stricturing Crohn's disease of the duodenum: A case report and review of surgical options. Int J Surg Case Rep. 2012;3:242-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Yamamoto T, Bain IM, Connolly AB, Allan RN, Keighley MR. Outcome of strictureplasty for duodenal Crohn's disease. Br J Surg. 1999;86:259-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Bemelman WA, Warusavitarne J, Sampietro GM, Serclova Z, Zmora O, Luglio G, de Buck van Overstraeten A, Burke JP, Buskens CJ, Colombo F, Dias JA, Eliakim R, Elosua T, Gecim IE, Kolacek S, Kierkus J, Kolho KL, Lefevre JH, Millan M, Panis Y, Pinkney T, Russell RK, Shwaartz C, Vaizey C, Yassin N, D'Hoore A. ECCO-ESCP Consensus on Surgery for Crohn's Disease. J Crohns Colitis. 2018;12:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 14. | Crespi M, Dulbecco P, De Ceglie A, Conio M. Strictures in Crohn's Disease: From Pathophysiology to Treatment. Dig Dis Sci. 2020;65:1904-1916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Singh A, Agrawal N, Kurada S, Lopez R, Kessler H, Philpott J, Shen B, Lashner B, Rieder F. Efficacy, Safety, and Long-term Outcome of Serial Endoscopic Balloon Dilation for Upper Gastrointestinal Crohn's Disease-associated Strictures-A Cohort Study. J Crohns Colitis. 2017;11:1044-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 16. | Gong J, Wei Y, Gu L, Li Y, Guo Z, Sun J, Ding C, Zhu W, Li N, Li J. Outcome of Surgery for Coloduodenal Fistula in Crohn's Disease. J Gastrointest Surg. 2016;20:976-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Lianwen Y, Jianping Z, Guoshun S, Dongcai L, Jiapeng Z. Surgical treatment for right colon cancer directly invading the duodenum. Am Surg. 2009;75:385-388. [PubMed] |
| 18. | Yuan L, Zhou J, Shu G, Liu D. Pedicled ileal flap for duodenal defect after right hemicolectomy. Hepatogastroenterology. 2010;57:493-496. [PubMed] |
| 19. | Huang G, Yuan L, Zhou J. Crohn's disease complicated with Lymphoma: A case report and Literature Review. Zhongguo Xiandai Shoushuxue Zazhi. 2012;16:110-111. |
| 20. | Wu Q, Wang X, Wu F, Peng D, Wu G, Yang L, Yuan L. Role of a multidisciplinary team (MDT) in the diagnosis, treatment, and outcomes of inflammatory bowel disease: a single Chinese center's experience. Biosci Trends. 2021;15:171-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |