Published online Apr 27, 2023. doi: 10.4240/wjgs.v15.i4.634
Peer-review started: December 19, 2022
First decision: January 9, 2023
Revised: January 24, 2023
Accepted: March 23, 2023
Article in press: March 23, 2023
Published online: April 27, 2023
Processing time: 124 Days and 20.6 Hours
Hypersplenism and esophageal varices bleeding are the major complications of portal hypertension (PHT). In recent years, increasing attention has been given to spleen preservation operations. The mode and long-term effects of subtotal splenectomy and selective pericardial devascularization for PHT remain controversial.
To investigate the clinical efficacy and safety of subtotal splenectomy combined with selective pericardial devascularization for the treatment of PHT.
This was a retrospective study of 15 patients with PHT who underwent subtotal splenectomy not preserving the splenic artery or vein combined with selective pericardial devascularization in the Department of Hepatobiliary Surgery, Qilu Hospital of Shandong University from February 2011 to April 2022. Fifteen propensity score-matched patients with PHT who underwent total splenectomy at the same time served as the control group. The patients were followed for up to 11 years after surgery. We compared the postoperative platelet levels, perioperative splenic vein thrombosis, and serum immunoglobulin levels between the two groups. Abdominal enhanced computed tomography was used to evaluate the blood supply and function of the residual spleen. The operation time, intraoperative blood loss, evacuation time, and hospital stay were compared between the two groups.
The postoperative platelet level of patients in the subtotal splenectomy group was significantly lower than that in the total splenectomy group (P < 0.05), and the postoperative portal system thrombosis rate in the subtotal splenectomy group was also much lower than that in the total splenectomy group. The levels of serum immunoglobulins (IgG, IgA, and IgM) showed no significant differences after surgery compared with before surgery in the subtotal splenectomy group (P > 0.05), but serum immunoglobulin IgG and IgM levels decreased dramatically after total splenectomy (P < 0.05). The operation time in the subtotal splenectomy group was longer than that in the total splenectomy group (P < 0.05), but there were no significant differences in the amount of intraoperative blood loss, evacuation time, or hospital stay between the two groups.
Subtotal splenectomy not preserving the splenic artery or vein combined with selective pericardial devascularization is a safe and effective surgical treatment for patients with PHT, not only correcting hypersplenism but also preserving splenic function, especially immunological function.
Core Tip: Partial spleen resection is beneficial for benign lesions in normal spleens. However, many issues regarding subtotal spleen resection for portal hypertension remain elusive. We performed subtotal spleen resection in situ without preserving the splenic artery and vein for portal hypertension and evaluated perioperative complications and clinical effects retrospectively. Follow-up results showed that subtotal splenectomy is a safe and effective surgical treatment for patients with portal hypertension, not only correcting hypersplenism but also preserving splenic function.
- Citation: Li HL, Ning SL, Gao YJ, Zhou T, Chen YX. In situ subtotal spleen resection combined with selective pericardial devascularization for the treatment of portal hypertension. World J Gastrointest Surg 2023; 15(4): 634-642
- URL: https://www.wjgnet.com/1948-9366/full/v15/i4/634.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i4.634
Portal hypertension (PHT) is common in China, and liver cirrhosis caused by chronic hepatitis B virus infection is the main pathogenic factor. Esophagogastric variceal hemorrhage and hypersplenism are the main causes of death and affect the quality of life of patients. For patients with esophagogastric variceal hemorrhage that cannot be controlled by endoscopic treatment, total splenectomy and selective pericardial devascularization are the main surgical methods for the treatment of PHT in China. However, a sharp increase of platelet level and portal system thrombosis after surgery is a major complication affecting the surgical outcome and can even lead to death. We summarized subtotal splenectomy not preserving the splenic artery or vein and selective pericardial devascularization for the treatment of PHT. The follow-up results showed that the clinical efficacy was rather good, and the surgical approach was safe and effective.
We retrospectively collected the clinical data of 15 patients with PHT who underwent subtotal splenectomy and selective pericardial devascularization in the Department of Hepatobiliary Surgery, Qilu Hospital of Shandong University, from February 2011 to April 2022. Among them, 6 patients were male and 9 were female, with a median age of 48 years. The causes of PHT included chronic hepatitis B in 10 patients, autoimmune hepatitis in 3 patients, and idiopathic PHT in 2 patients. Eleven patients underwent open surgery, 1 patient underwent assisted laparoscopic surgery, and 3 patients underwent complete laparoscopic surgery. Fifteen patients with PHT who underwent total splenectomy were selected as the control group after propensity score matching. The surgical protocol and postoperative follow-up were approved by the patients and their families. All procedures were conducted in accordance with the Declaration of Helsinki. This study was reviewed and approved by the Ethics Committee of Qilu Hospital of Shandong University.
The indications for study inclusion were as follows: (1) A history of upper gastrointestinal bleeding; (2) patients who were suitable for emergency surgery for severe esophageal and gastric varices bleeding; (3) Child-Pugh classification of liver function A or B; (4) number of platelets below 30 × 109/L caused by hypersplenism; and (5) patients who were not suitable for EIS or EVL or who had failed treatment.
The contraindications for study inclusion were as follows: (1) Child-Pugh classification of liver function C; (2) relative contraindications for surgery with ICG R15 > 40%; (3) main portal vein, splenic vein, or mesentery superior venous thrombosis; and (4) patients with severe dysfunction of the heart, lung, kidney, or other vital organs who could not tolerate surgery or anesthesia.
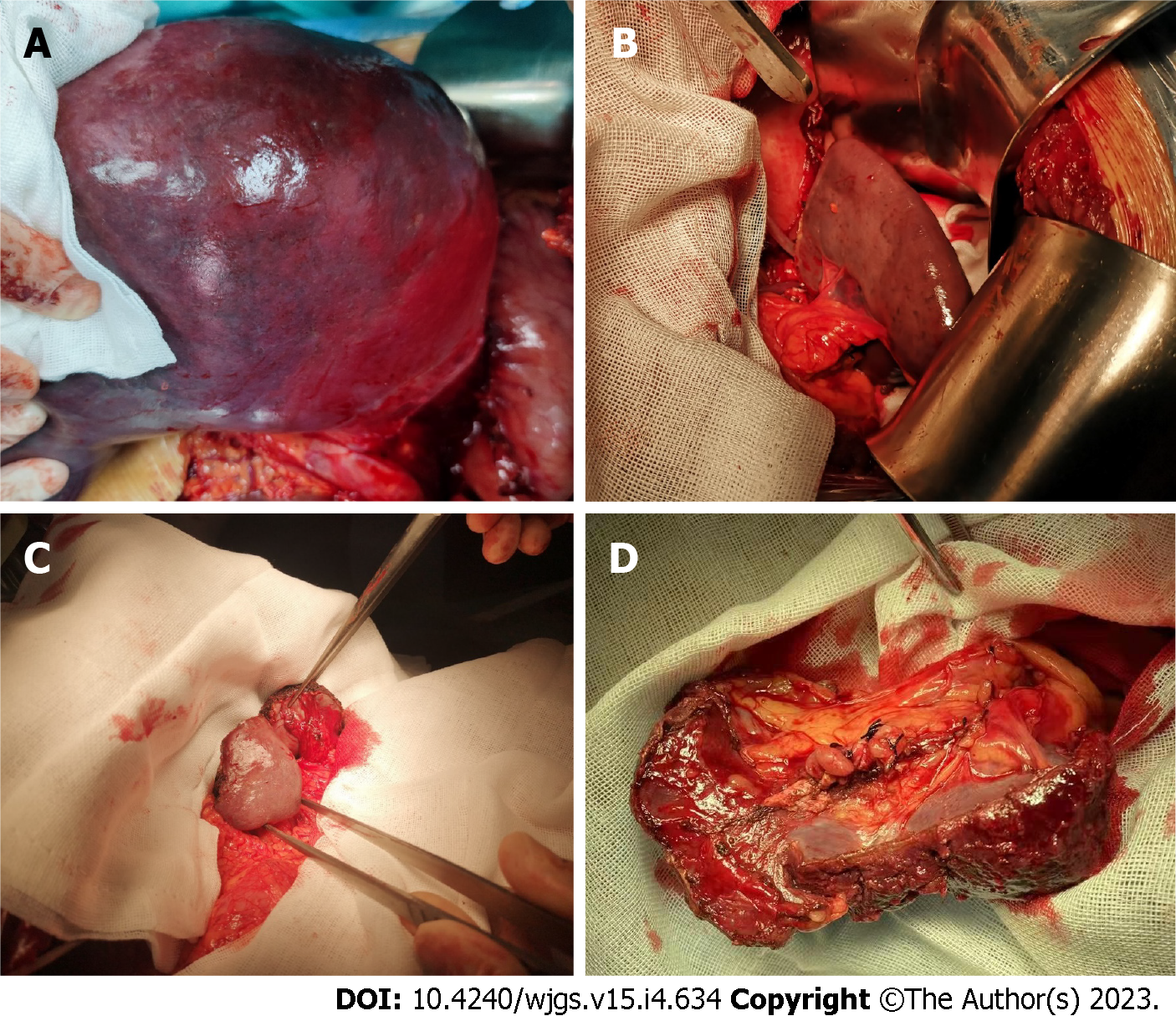
Open surgery: The left subcostal incision was favored for good surgical exposure. The gastrocolic ligament was cut, and a 0.2 cm diameter silicone tube was inserted into the right gastroepiploic vein. Then, the free portal vein pressure was dynamically measured at the level of the right atrium. The main trunk of the splenic artery was dissected along the upper edge of the pancreas and double ligated 3-5 cm away from the splenic hilum. The gastrosplenic ligament and the short gastric blood vessels were cut, and then we dissected the tail of the pancreas and the splenic hilum (Figure 1A and B). After the splenic vein was ligated and cut, we tried to preserve the integrity of the splenophrenic ligament, splenorenal ligament, and splenocolic ligament around the lower pole of the spleen as much as possible. For the total splenectomy group, the splenocolic ligament was generally disconnected first after ligation of the splenic artery, which facilitated the dissection of the large spleen from the lower pole to the upper pole. Finally, the spleen was lifted out of the abdominal cavity. The spleen was cut approximately 1 cm away from the ischemic line using an ultrasonic scalpel, and larger blood vessels were ligated or sutured on the cut surface. A splenic artery aneurysm with a size of approximately 2.5 cm was resected in one patient, followed by selective pericardial devascularization. The lower end of the esophagus was dissociated by approximately 7 cm, and the main coronary vein and vagus nerve were preserved. After checking that there was no obvious bleeding, the residual spleen was wrapped with omentum majus and placed in the retroperitoneal wound in situ. One young patient underwent distal splenorenal shunt and selective pericardial devascularization. The splenophrenic ligament at the upper pole of the spleen was thicker, and we preserved the upper pole of the spleen. In another patient, both the lower and upper poles of the spleen had blood supply after the splenic blood vessels were cut off, so both the upper and lower poles were preserved (Figure 1C). The tissue between the splenic hilum and the retroperitoneum was able to meet the blood supply in some areas of the splenic hilum after the splenic arteries and veins were separated from the tail of the pancreas, and the tissue around the splenic hilum was preserved (Figure 1D).
Laparoscopic surgery: The observation hole was selected below the umbilicus, and the position of the surgical hole was selected according to the projection of the skin surface of the spleen. After the gastrocolic ligament was severed with an ultrasonic scalpel, the main trunk of the splenic artery was dissected along the upper edge of the pancreas and double clipped 3–5 cm away from the splenic hilum. Then, the upper pole of the spleen was completely exposed after the gastrosplenic ligament and short gastric vessels were severed, and the splenic pedicle was gradually ligated from the upper pole to the lower pole. For the total splenectomy group, perisplenic ligaments were dissected from the lower pole to the upper pole. The surgeon should pay special attention to the tail of the pancreas; the splenic vein was cut off with a laparoscopic stapler. The treatment of the residual spleen was the same as that of open surgery. One patient had severe tortuous veins around the esophagus and the fundus of the stomach, and we converted to open surgery for subsequent pericardial devascularization.
Peripheral blood hemoglobin and platelet levels were measured before surgery and 1, 3, 5, and 7 d after surgery. Perioperative enhanced computed tomography (CT) and vascular ultrasound were used to evaluate whether thrombosis had formed in the portal vein system. Abdominal enhanced CT was used to assess the residual splenic blood supply and hyperplasia status. The operative time, intraoperative blood loss, postoperative gastrointestinal function recovery time, hospital stay, and other indicators were also summarized in this study.
SPSS 25.0 was used for statistical analysis. The data of the paired and unpaired groups were analyzed by t test, repetitive measurement deviation analysis was used for PLT level comparisons, and P < 0.05 was considered statistically significant.
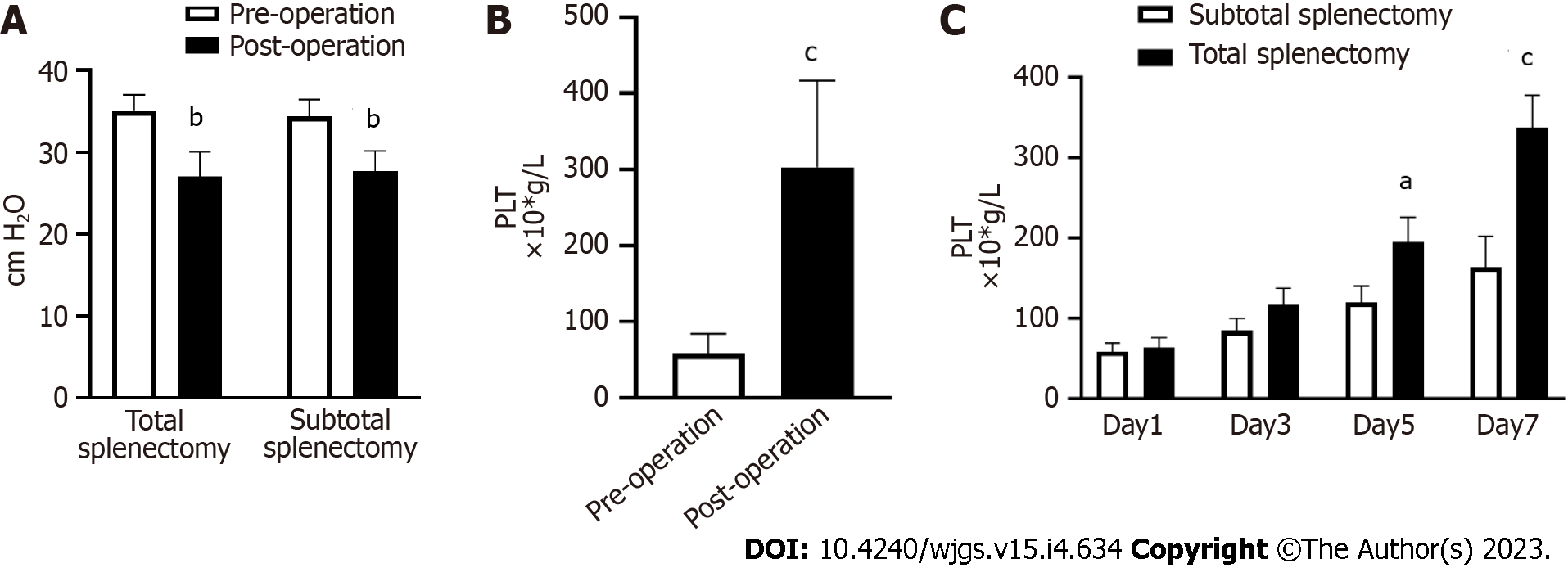
The longest postoperative follow-up time was 11 years, and the free portal vein pressure decreased significantly after surgery in both the total and subtotal splenectomy groups (Figure 2A). The platelet level increased significantly 3 mo after surgery (P < 0.05), indicating that the symptoms of hypersplenism were significantly relieved (Figure 2B). Furthermore, the postoperative platelet level of patients in the subtotal splenectomy group was significantly lower than that in the total splenectomy group (Figure 2C), indicating that subtotal splenectomy could effectively delay the sharp increase in platelets after surgery. In the subtotal splenectomy group, only one case of portal system thrombosis was found 1 mo after surgery, but 4 cases were found in the total splenectomy group. The results demonstrated that subtotal splenectomy could reduce the incidence of perioperative portal system thrombosis compared with total splenectomy.
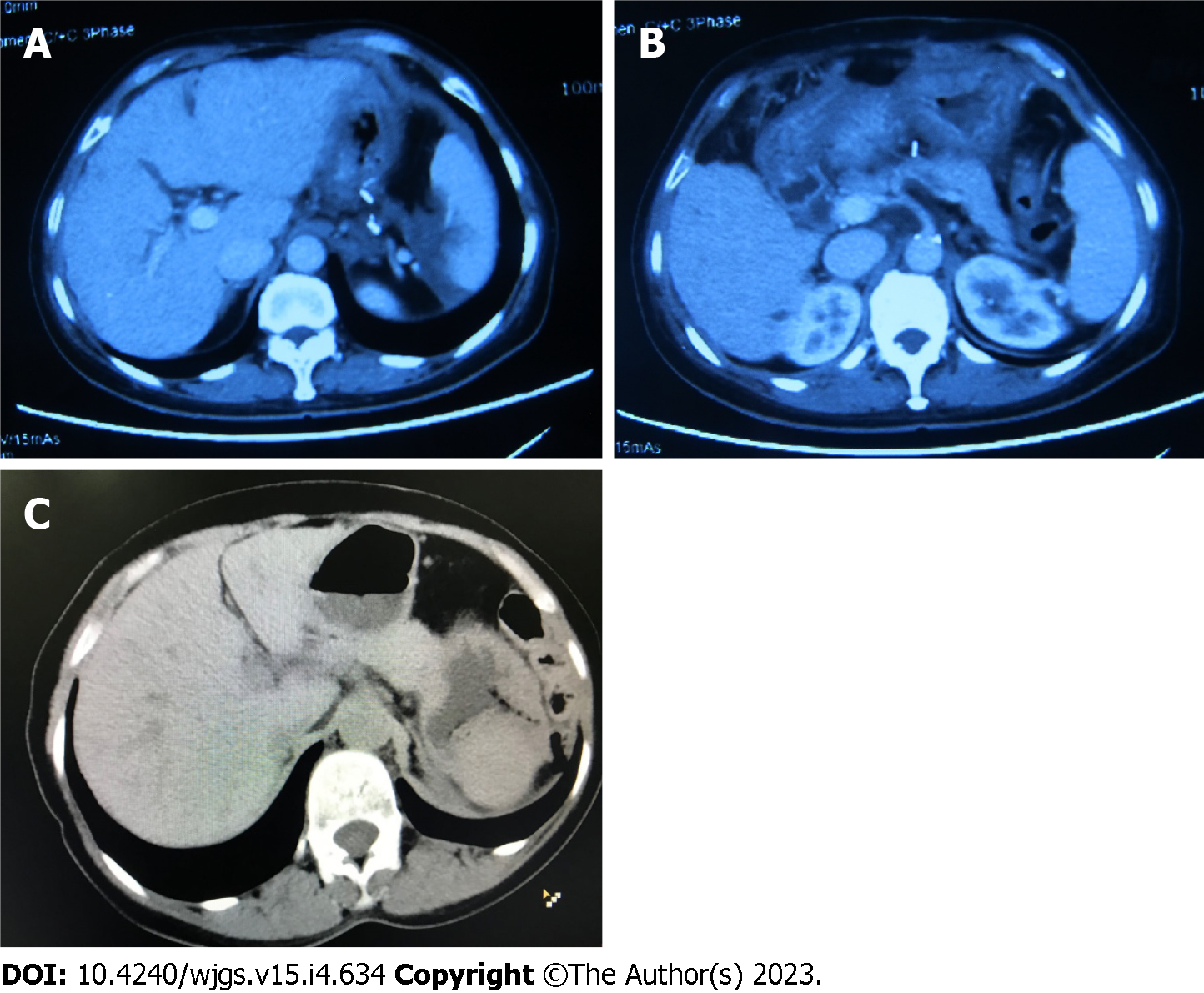
The levels of serum immunoglobulins (IgG, IgA, and IgM) 6 mo after surgery were not significantly different from those before surgery (P > 0.05) in the subtotal splenectomy group, but the levels of serum immunoglobulins IgG and IgM decreased dramatically after total splenectomy (P < 0.05) (Table 1). Although the residual spleen of one patient showed small-scale necrosis (Figure 3A), the patient had no discomfort, and collateral circulation could be seen between the residual spleen and the retroperitoneal tissue (Figure 3B), indicating that this procedure not only preserved splenic function but also acted as a shunt between the portal and systemic circulation. The remaining splenic hyperplasia of the patient, who was followed up for 11 years, was relatively significant within 3 years after surgery (Figure 3C), but the hyperplasia slowed down over time. According to our limited case study, splenic hyperplasia after subtotal resection is faster in young patients and relatively slow in elderly patients. During the follow-up period, the overall quality of life of this patient was good, and there was no hypersplenism.
| Subtotal splenectomy | Total splenectomy | |||||
| Pre-operation | Post-operation | P value | Pre-operation | Post-operation | P value | |
| IgG (g/L) | 14.5 ± 2.4 | 13.4 ± 2.9 | > 0.05 | 13.7 ± 1.6 | 8.3 ± 2.0 | < 0.05 |
| IgA (g/L) | 2.3 ± 0.4 | 2.1 ± 0.5 | > 0.05 | 2.4 ± 0.4 | 2.2 ± 0.5 | > 0.05 |
| IgM (g/L) | 0.80 ± 0.12 | 0.84 ± 0.18 | > 0.05 | 0.85 ± 0.05 | 0.60 ± 0.07 | < 0.05 |
There were no deaths during the perioperative period. The operation time of the subtotal splenectomy group was longer than that of the total splenectomy group (P < 0.05), but there were no significant differences in the amount of intraoperative blood loss, evacuation time, or hospital stay between the two groups (Table 2).
| Total splenectomy | Subtotal splenectomy | P value | |
| Operation time (min) | 168.67 ± 28.50 | 198.33 ± 29.92 | 0.010 |
| Blood loss (mL) | 117.33 ± 42.33 | 119.33 ± 38.63 | 0.893 |
| Evacuation time (d) | 2.19 ± 0.62 | 2.28 ± 0.77 | 0.736 |
| Hospital stay (d) | 8.60 ± 1.40 | 8.86 ± 1.29 | 0.613 |
PHT is a group of clinical syndromes caused by the persistent elevation of hepatic portal vein pressure, which usually presents with esophagogastric varices, hypersplenism and severe ascites. Approximately 20%–30% of patients will have upper gastrointestinal bleeding. Because of the donor liver lack and complicated postoperative management for liver transplantation, total splenectomy combined with selective pericardial devascularization is the main surgical approach for the treatment of PHT in China. This procedure not only reduces the free portal vein pressure but also decreases the chance of esophagogastric venous bleeding[1].
With further understanding of spleen anatomy and its immune function, increasing attention has recently been given to spleen preservation operations. Recent studies have shown that the spleen plays an important role in hepatic function protection, infection control, and tumor immunity in patients with PHT[2]. Total splenectomy in patients with liver cirrhosis reduces the ability of the body to remove particulate matter from the blood and aggravate immune dysfunction. These patients are more prone to postoperative infection than patients without cirrhosis[3,4]. In addition, total splenectomy can also cause a relative increase in inhibitory T lymphocytes (Ts) and a significant decrease in helper T lymphocytes (Th) and serum IgM levels, inhibiting antitumor immunity[5].
The clinical application of spleen-preserving surgery has been increasing, especially for patients with splenic trauma and benign splenic tumors. Omentum autologous spleen graft implantation is currently the most widely used spleen-preserving surgical procedure. The omentum majus can provide sufficient blood supply for splenic implants, which could meet the physiological needs of the body[6]. Because patients with PHT usually have severe cirrhosis and the coagulation function and nutritional conditions of patients are generally poor, the application of spleen-preserving surgery for cirrhosis patients remains relatively rare. We retrospectively analyzed the clinical data of 15 cases of subtotal splenectomy not preserving splenic vessels combined with selective pericardial devascularization for the treatment of PHT. The platelet levels on days 5 and 7 were significantly lower than those in the total splenectomy group, indicating that subtotal splenectomy correlated with a delayed increase in platelets and a reduced incidence of portal system thrombosis in patients with cirrhosis. There were no significant differences in serum IgG, IgA, or IgM in the subtotal splenectomy group 6 mo after surgery, indicating that the immune function of the residual spleen in patients with PHT after subtotal splenectomy was rather good. However, serum IgG and IgM decreased significantly after total splenectomy, which was consistent with previous reports[7]. Although the operation time of spleen-preserving surgery was prolonged, there were no significant differences in intraoperative blood loss, postoperative recovery time of gastrointestinal function, or hospital stay.
In addition, some scholars have conducted in-depth studies on the clinical effects of subtotal splenectomy with preservation of the upper pole of the spleen. Chu et al[7,8] found that the levels of collagen, elasticity, and reticular fibers in the residual spleen after subtotal splenectomy and retrosternal omentum fixation in patients with liver cirrhosis and hypersplenism were not significantly different from those in the preoperative spleen. Radioisotope scanning also showed normal phagocytosis of the residual spleen[7,8]. Petroianu A et al[9] performed subtotal splenectomy with preservation of the upper pole of the spleen in patients with schistosomiasis-related PHT, and the residual spleen was supplied by some short gastric vessels and was in good condition.
Since most patients with PHT have severe esophageal and gastric fundus varices, we think that preservation of the upper pole of the spleen and some short gastric vessels may increase the chance of upper gastrointestinal bleeding. However, preservation of the lower pole of the spleen will be beneficial for the long survival of patients. We recommend that the splenic artery should be ligated approximately 3 cm from the splenic hilum to avoid uncontrollable massive hemorrhage during the operation and to preserve the residual splenic blood supply from the pancreatic tail as much as possible. Traditionally, splenic vein congestion and splenic sinus dilation caused by PHT are the main causes of hypersplenism. Recent studies have shown that splenic vascular hyperplasia and fibrosis are also important reasons for hypersplenism[10]. We should be careful to keep the splenocolic ligament intact from the beginning because the splenocolic and splenorenal ligaments are the main blood supply to the residual spleen after the splenic vessels are cut off, which increases the difficulty of the operation to a certain extent. Although the splenocolic ligament thickens to varying degrees in patients with PHT, it is necessary to avoid pulling and moving the spleen during surgery. The lower part of the splenophrenic and splenorenal ligaments create conditions for the establishment of collateral circulation between the residual spleen and the retroperitoneal tissue in the later stage and ultimately play a role in shunting[11,12]. Finally, the tangent line of the spleen and the size of the residual spleen are determined by the ischemic line on the spleen surface. Generally, spleen transection approximately 1.0 cm away from the ischemic line can reduce intraoperative bleeding and maintain the tissue activity of the residual spleen. In addition, the current surgical methods for spleen preservation in patients with PHT include peritoneal dissection at the left upper pole of the kidney and insertion and proper fixation of the residual spleen[13].
For patients with PHT, there is currently no unified standard for the size of the residual spleen. Generally, preserved splenic tissue, which is slightly smaller than the normal spleen, is sufficient to maintain splenic function in patients with PHT. Some studies have demonstrated that the residual spleen should be smaller than 5 cm × 3 cm[14], but it was also reported that spleen size should be comprehensively considered based on liver cirrhosis, platelets, spleen size, and other factors[15]. In summary, in situ subtotal splenectomy and selective pericardial devascularization is safe and feasible for patients with PHT.
The study analyzed the clinical data of subtotal splenectomy not preserving splenic vessels combined with selective pericardial devascularization for patients with PHT. The platelet levels after subtotal splenectomy were significantly lower than those in the total splenectomy group and portal system thrombosis rate decreased in the subtotal splenectomy group. Consistent with previous reports, serum IgG and IgM decreased significantly after total splenectomy, however, the immune function of the residual spleen lower pole after subtotal splenectomy was rather good.
During the operation, we think that preservation of the lower pole of the spleen in situ is more suitable and beneficial for the long survival of patients. Follow-up data also demonstrated that the blood supply from splenocolic and splenorenal ligaments was enough for residual spleen and collateral circulation could be established between the residual spleen and retroperitoneal tissue spontaneously. In situ subtotal splenectomy not preserving the splenic artery or vein combined with selective pericardial devascularization is an effective and safe surgical treatment for patients with PHT.
Liver cirrhosis caused by chronic hepatitis B virus infection is the main pathogenic factor of portal hypertension (PHT) in China. For patients with serious esophagogastric variceal hemorrhage that cannot be controlled by endoscopic treatment, total splenectomy and selective pericardial devascularization are the main surgical methods for the treatment of PHT in China.
As we know, the sharp increase of platelet level and portal system thrombosis after total splenectomy is a serious complication affecting the surgical outcome and can even lead to death. More and more attention has been paid to spleen preservation operations recently. However, the long-term effects of subtotal splenectomy for PHT remain controversial.
The objective of the study was to explore the clinical efficacy and safety of subtotal splenectomy in situ combined with selective pericardial devascularization for the treatment of PHT.
The study summarized the clinical data of PHT patients who received subtotal spleen resection and selective pericardial devascularization. We compared the postoperative platelet level, perioperative spleen vein thrombosis, and serum immunoglobulin level with the control group. Abdominal enhanced computed tomography was used to evaluate the blood supply of the residual spleen. The operation time, intraoperative blood loss and other parameters were also evaluated statistically.
The follow-up results showed that the surgical approach was safe and effective. The postoperative platelet level of patients in the subtotal splenectomy group was significantly lower and the postoperative portal system thrombosis rate was also much lower than that in the total splenectomy group. The levels of serum immunoglobulins (IgG, IgA, and IgM) showed no significant difference after operation in the subtotal splenectomy group.
In situ subtotal splenectomy not preserving the splenic artery and vein combined with selective pericardial devascularization is a safe and effective surgical treatment for patients with PHT, not only correcting hypersplenism but also preserving the immunological function of spleen.
Subtotal splenectomy is suitable for specific PHT patients but the mode and long-term effects requires further study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Allon R, Israel; Honda M, Japan S-Editor: Wang JL L-Editor: A P-Editor: Zhao S
| 1. | Friedman SL, Pinzani M. Hepatic fibrosis 2022: Unmet needs and a blueprint for the future. Hepatology. 2022;75:473-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 286] [Cited by in RCA: 260] [Article Influence: 86.7] [Reference Citation Analysis (0)] |
| 2. | Zhang Y, Mao DF, Zhang MW, Fan XX. Clinical value of liver and spleen shear wave velocity in predicting the prognosis of patients with portal hypertension. World J Gastroenterol. 2017;23:8044-8052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Kondo R, Kage M, Iijima H, Fujimoto J, Nishimura T, Aizawa N, Akiba J, Naito Y, Kusano H, Nakayama M, Mihara Y, Tanigawa M, Yano H. Pathological findings that contribute to tissue stiffness in the spleen of liver cirrhosis patients. Hepatol Res. 2018;48:1000-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Allaire M, Goumard C, Lim C, Le Cleach A, Wagner M, Scatton O. New frontiers in liver resection for hepatocellular carcinoma. JHEP Rep. 2020;2:100134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 5. | Tarantino G, Savastano S, Capone D, Colao A. Spleen: A new role for an old player? World J Gastroenterol. 2011;17:3776-3784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 93] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Di Carlo I, Toro A. Splenic Autotransplantation Is Always Valid after Splenectomy. J Invest Surg. 2017;30:401-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Chu HB, Zhang TG, Zhao JH, Jian FG, Xu YB, Wang T, Wang M, Tang JY, Sun HJ, Li K, Guo WJ, Zhu XJ. Assessment of immune cells and function of the residual spleen after subtotal splenectomy due to splenomegaly in cirrhotic patients. BMC Immunol. 2014;15:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Chu H, Liu X, Zhao J, Xu Y, Wang L, Wang T, Guo W, Zhang S, Zhu X. Subtotal splenectomy for splenomegaly in cirrhotic patients. Int J Clin Exp Pathol. 2014;7:4981-4990. [PubMed] |
| 9. | Petroianu A, Resende V, Da Silva RG. Late follow-up of patients submitted to subtotal splenectomy. Int J Surg. 2006;4:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Chu H, Han W, Wang L, Xu Y, Jian F, Zhang W, Wang T, Zhao J. Long-term efficacy of subtotal splenectomy due to portal hypertension in cirrhotic patients. BMC Surg. 2015;15:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Petroianu A, Petroianu LP. Splenic autotransplantation for treatment of portal hypertension. Can J Surg. 2005;48:382-386. [PubMed] |
| 12. | Zhang H, Chen J, Kaiser GM, Mapudengo O, Zhang J, Exton MS, Song E. The value of partial splenic autotransplantation in patients with portal hypertension: a prospective randomized study. Arch Surg. 2002;137:89-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Radević B, Jesić R, Sagić D, Perisić V, Nenezić D, Popov P, Ilijevski N, Dugalić V, Gajin P, Vucurević G, Radak Dj, Trebjesanin Z, Babić D, Kastratović D, Matić P. [Partial resection of the spleen and spleno-renal shunt in the treatment of portal hypertension with splenomegaly and hypersplenism]. Acta Chir Iugosl. 2002;49:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Louis D, Duc ML, Reix P, Chazalette JP, Durieu I, Feigelson J, Bellon G. Partial splenectomy for portal hypertension in cystic fibrosis related liver disease. Pediatr Pulmonol. 2007;42:1173-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Sretenovic ALj, Perišić V, Krstić Z, Vujović D, Pavićević P, Stanisavljević D, Radević B. Warren shunt combined with partial splenectomy for children with extrahepatic portal hypertension, massive splenomegaly, and severe hypersplenism. Surg Today. 2013;43:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |