Published online Feb 27, 2023. doi: 10.4240/wjgs.v15.i2.287
Peer-review started: November 14, 2022
First decision: November 30, 2022
Revised: December 13, 2022
Accepted: January 10, 2023
Article in press: January 10, 2023
Published online: February 27, 2023
Processing time: 105 Days and 2.7 Hours
Primary malignant melanoma of the esophagus is a rare malignant tumor of the esophagus, and its combination with squamous cell carcinoma is also rare. Here, we report the diagnosis and treatment of a case of primary esophageal malignant melanoma combined with squamous cell carcinoma.
A middle-aged man underwent gastroscopy for dysphagia. Gastroscopy revealed multiple bulging esophageal lesions, and after pathologic and immunohistochemical analyses, the patient was finally diagnosed with "malignant melanoma with squamous cell carcinoma". This patient received comprehensive treatment. After one year of follow-up, the patient was in good condition, and the eso
When multiple esophageal lesions are present, the possibility of multiple pathological sources should be considered. This patient was diagnosed with primary esophageal malignant melanoma combined with squamous cell carcinoma.
Core Tip: Here, we report a 53-year-old man with primary malignant melanoma of the esophagus combined with squamous cell carcinoma diagnosed by endoscopy, biopsy, imaging evaluation, and physical examination; this diagnosis was confirmed by immunohistochemistry. The patient was treated with immunotherapy, radiotherapy, and chemotherapy. As of now, the patient has recovered well.
- Citation: Zhu ML, Wang LY, Bai XQ, Wu C, Liu XY. Primary malignant melanoma of the esophagus combined with squamous cell carcinoma: A case report. World J Gastrointest Surg 2023; 15(2): 287-293
- URL: https://www.wjgnet.com/1948-9366/full/v15/i2/287.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i2.287
Among malignant tumors, esophageal cancer currently ranks seventh worldwide in terms of incidence and sixth in terms of mortality rate. More than 90% of esophageal cancers in China are of the esophageal squamous cell carcinoma pathological type. In contrast, melanoma accounts for only 0.1% of all esophageal malignancies[1]. Although both types of malignant tumors can occur in the esophagus, no case of esophageal malignant melanoma combined with squamous cell carcinoma has been reported. Here, a case of primary esophageal malignant melanoma combined with squamous cell carcinoma is reported.
A 53-year-old man underwent esophagogastroduodenoscopy for dysphagia.
The patient had a history of progressive dysphagia for more than 1 mo.
The patient had no past medical problems.
He smoked 30 cigarettes per day for 30 years but only rare drinks alcohol. He is a farmer by profession and has other bad habits. No significant personal or family history was noted.
He was 1.76 m tall, weighs 72 Kg and has a BMI of 23.2 Kg/m2. During physical examination, no specific physical signs were found.
Routine blood, liver function, renal function and prothrombin tests were normal. Alpha-fetoprotein, carcinoembryonic antigen, carbohydrate antigen 19-9, carbohydrate antigen 724, neuron-specific enolase and cytokeratin-19-fragment were normal.
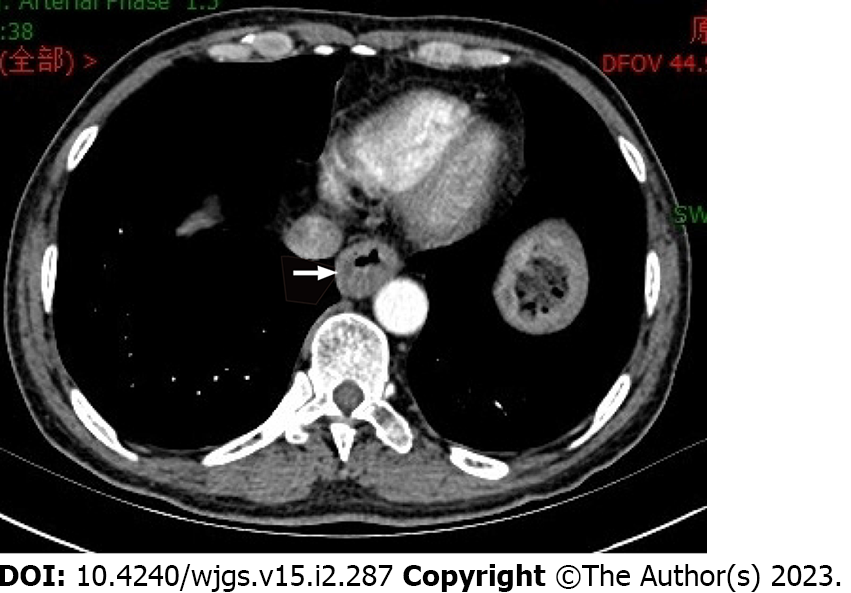
Chest and enhanced abdominal computed tomography (CT) indicated upper and lower esophageal wall thickening, and the lumen was narrow. Enhanced scanning showed the enhancement of the wall. The mediastinal lymph nodes were enlarged. Multiple small nodules were seen in both lungs, and emphysema, liver cysts, and cholecystitis were also observed (Figure 1).
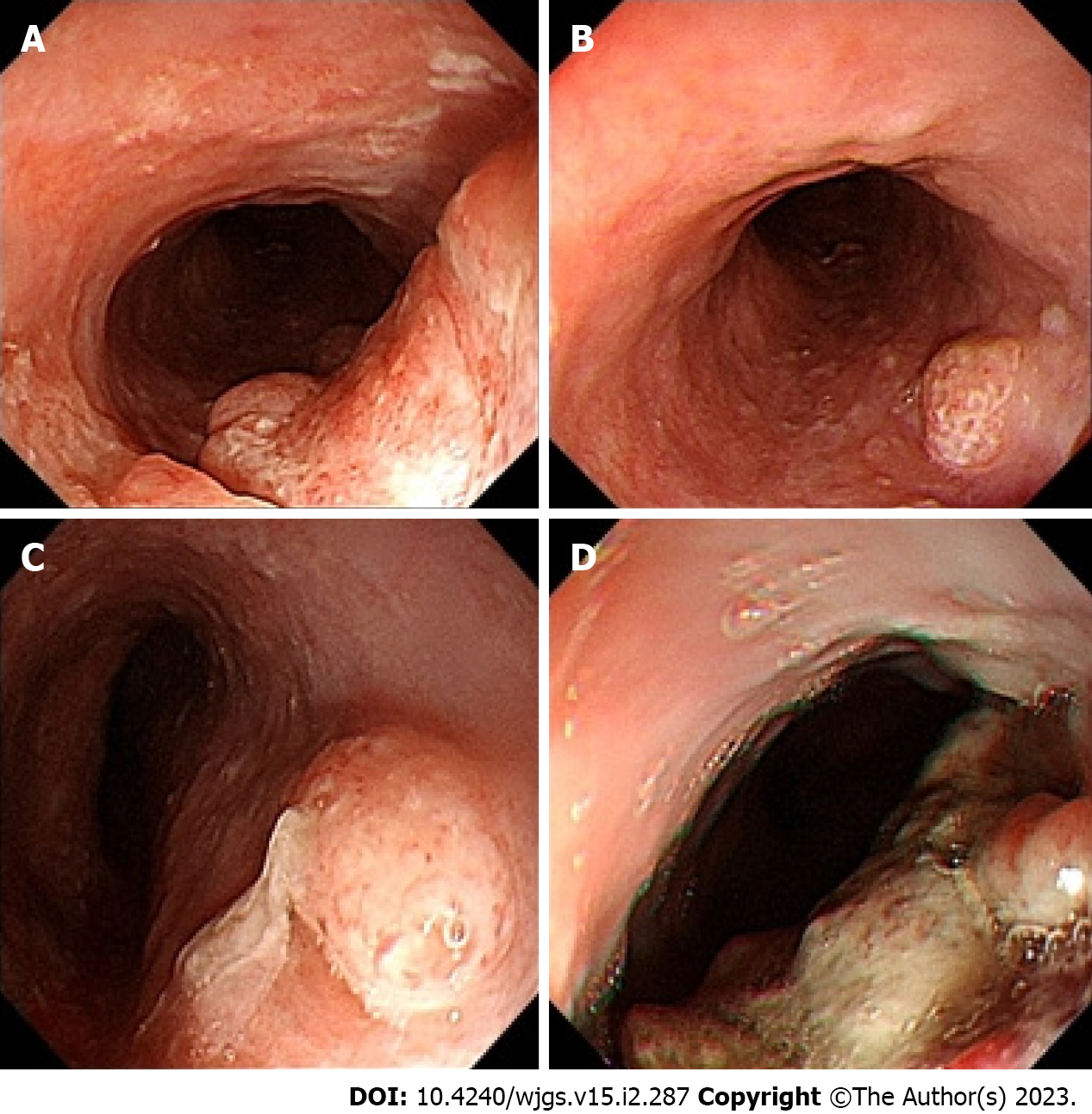
Gastroscopy observation showed irregular hyperplasia at 23-27 cm from the incisor, with no melanin deposition; hemispherical bulges at 29 cm and 32 cm from the incisor; and irregular hyperplasia at 39-43 cm from the incisor, indicating ulcers with a small amount of melanin deposition. Biopsies were performed at 23-27 cm, 32 cm, and 39-43 cm (Figure 2).
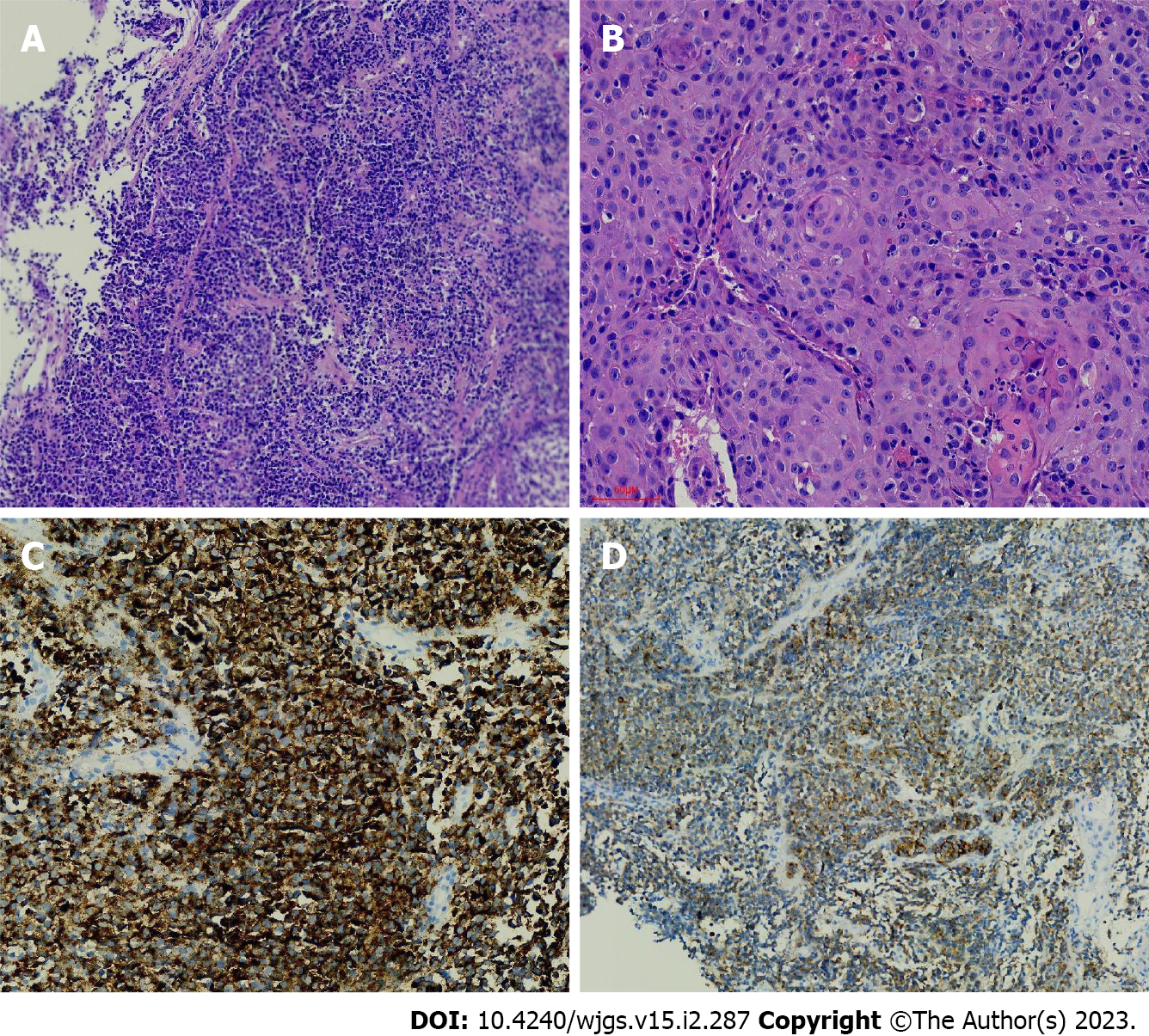
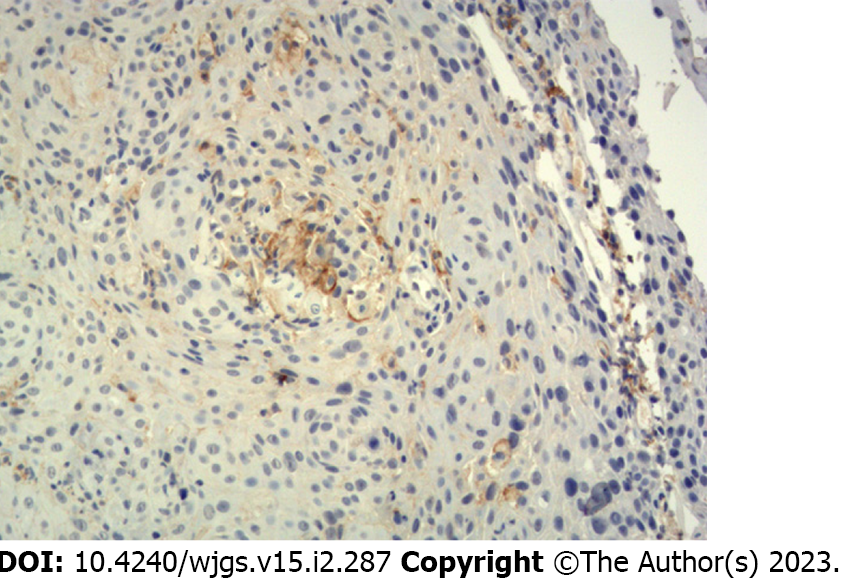
Pathologic analysis indicated malignant melanoma (23–27 cm from the incisor, 39–43 cm from the incisor) combined with squamous cell carcinoma (23–27 cm from the incisor) and solitary squamous cell carcinoma (32 cm from the incisor). Immunohistochemistry showed the following: Vimentin(+), HMB45(+), Melan-A(+), S-100(focus+); squamous cell carcinoma CK5/6(+), P40(+), P63(+), LCK(+), CD56(-), CgA(-), and Syn(-); and Ki-67(+) was approximately 30% (Figure 3).
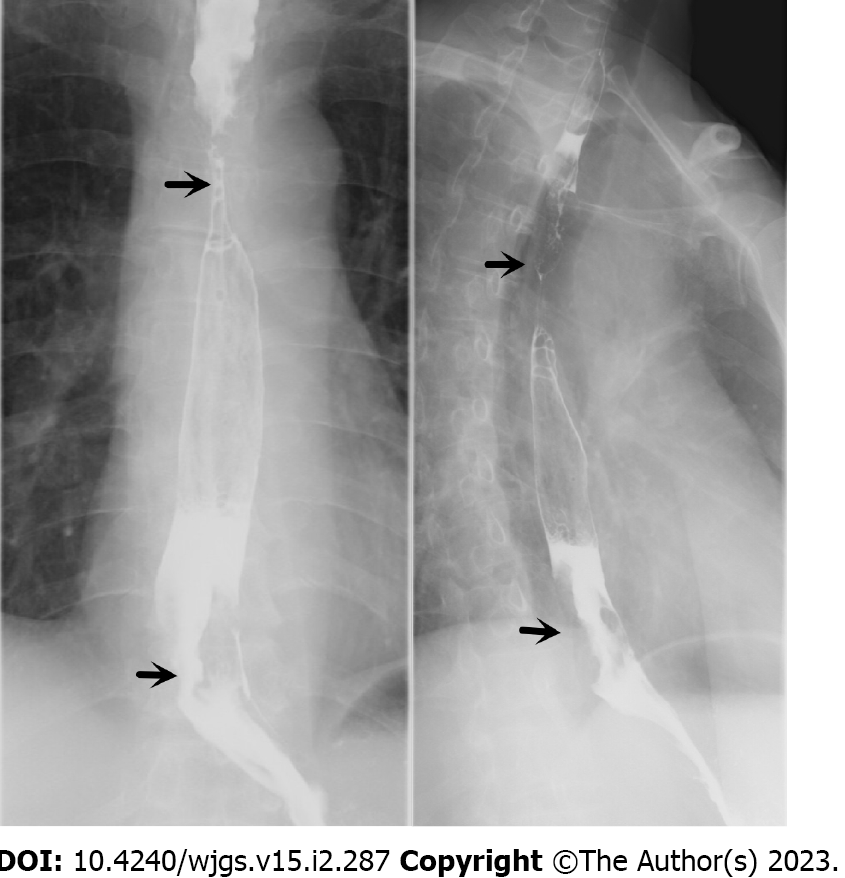
Upper gastrointestinal imaging revealed irregular filling defects approximately 4.5 cm and 5.7 cm in length in the upper and lower sections, respectively, which were accompanied by tube wall stiffness, poor expansion, restricted passage of contrast agent, and disruption of the continuity of the mucosa (Figure 4).
Positron emission tomography/computed tomography (PET/CT) showed thickening of the upper and lower thoracic walls of the esophagus, an abnormal increase in fluorodeoxyglucose (FDG) metabolism, and multiple enlarged lymph nodes in the mediastinum and right axilla. Multiple small nodules were observed in both lungs, and the FDG metabolism was increased.
No metastatic lesions were observed on brain magnetic resonance imaging (MRI).
The microsatellite instability results were MSS. Programmed death ligand-1 immunohistochemistry 22C3: The tumour proportion score results were 1%-2% (Figure 5).
The final diagnosis was esophageal malignant melanoma, esophageal squamous cell carcinoma (stage IV), bilateral lung metastases, and metastases in the mediastinal lymph nodes and right axillary lymph nodes.
The patient was first treated with 1 cycle of 200-mg camrelizumab, followed by 2 cycles of 300-mg nab-paclitaxel. Later, the patient was administered local radiotherapy, which was terminated because the patient could not tolerate it. Subsequently, he was given 2 cycles of 200-mg camrelizumab and 300-mg nab-paclitaxel.
The patient underwent another gastroscopy six months later, and no obvious space-occupying lesion was observed in the esophagus, while only a small amount of melanin deposition was seen (Figure 6). Regrettably, both enhanced CT and enhanced MRI of the patient's abdomen suggested liver metastasis. It is recommended that patients continue treatment with camrelizumab combined with apatinib. The current case has been followed-up for approximately 1 year, and he has not experienced dysphagia.
Primary malignant melanoma of the esophagus (PMME) is a rare disease that accounts for 0.5% of all nonskin melanomas[2]. Primary melanin-free melanoma is also extremely rare, with slightly more than 20 cases reported thus far[3], and combined esophageal squamous cell carcinoma is even rarer.
The average age of patients with PMME is 60.5 years, and the incidence rate is higher in male patients than in female patients, with a ratio of 2:1[4,5]. The degree of PMME malignancy is high and is associated with a poor prognosis; PMME has a median survival rate of 18.1 mo and a 5-year survival rate of less than 10%[6].
The clinical manifestations of PMME are similar to those of esophageal squamous cell carcinoma, and most patients experience the following symptoms: Dysphagia, poststernal pain, and weight loss. Hematemesis and melena are rare. Typical PMME on endoscopy is a lobular or polyp-like tumor with clear boundaries and pigmentation. More than 90% of PMME lesions are located in the distal 2/3 of the esophagus[7]. Approximately 10% to 25% of PMME cases have lesions that are different colors, including purple, brown, and white, depending on the amount of melanin[8,9]. Some tumors are composed of melanin-free cells, and the identification of other tumors by endoscopy is difficult. The pathological manifestations of primary malignant melanoma in the esophagus can represent the superficial spreading type or a nodule-like growth pattern, and a distinct Peyer’s patch-like or freckle-like melanocyte nest invasion is observed in adjacent squamous epithelium. Tumor cells are primarily composed of epithelial-like mole-like cells, which are round, oval, polygonal, or shuttle shaped and have large nuclei and large, clear nucleoli. Base film samples are dyed to show thick-walled blood vessels and tubes, which are significant features of melanoma[10]. HMB-45, S-100, vimentin, and melanoma-specific antigen (Melan-A) are specific to this diagnosis[11].
PMME mainly occurs through hematogenous metastasis and lymphatic metastasis, and common sites of metastases include the liver (31%), mediastinum (29%), lung (18%), and brain (13%)[12]. Whether mediastinal invasion, lymphadenopathy, and distant metastasis are present can be determined through chest and abdominal CT, which can be used to show and determine the stages of lesions. PET-CT plays an important role in the diagnosis of metastatic lesions.
Esophageal malignant melanoma has no specific treatment, and complete surgical removal of lesions is preferred, along with lymph node clearing. Four to six cycles of temozolomide/dacarbazine (DTIC)-based auxiliary chemotherapy are recommended. Radiation therapy is also a possibility. DTIC is the “gold standard” for the medical treatment of advanced melanoma, but its overall efficacy is poor. For targeted therapy, ipilimumab can be used to treat advanced melanoma. Anti-PD-1 and anti-CTLA-4 drugs and IL-2 are FDA-approved immunotherapy drugs that result in significant survival benefits in patients with advanced skin melanoma, but their effects on esophageal malignant melanoma require further investigation[13-15].
Esophageal squamous cell carcinoma is the most common malignant tumor of the esophagus. Patients are located in cities in China with a high incidence of esophageal cancer[16,17], which is mainly associated with diet and lifestyle habits. Radical surgery is the main approach for treating esophageal squamous cell carcinoma. PD-1 inhibitors are currently the first-line drugs for advanced melanoma and have been shown to be effective in treating squamous cell carcinoma of the esophagus[18]. Although radiotherapy and chemotherapy are not sensitive to malignant melanoma of the esophagus, the patient was treated with nab-paclitaxel in combination with squamous cell carcinoma of the esophagus and 40 Gy/20 F radiotherapy to the esophageal lesion and mediastinal lymph node area. Overall, our treatment was effective.
In this case, many lesions indicative of esophageal disease were found by gastroscopy. The lesions contained no melanin on their surfaces and were thus unsuitable for endoscopy-based diagnosis and identification. Through pathology and immunohistochemistry, esophageal malignant melanoma combined with esophageal squamous cell carcinoma was diagnosed. This case demonstrated that multiple lesions in the same location can represent different pathologies.
We report a very rare case of primary malignant melanoma of the oesophagus combined with squamous cell carcinoma. Although we do not have much experience in treating this disease, the patient's oesophageal lesions were well controlled through aggressive treatment. We hope this will provide an insight into the diagnosis and treatment of this type of disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Atanasova EG, Bulgaria; ISHIDA T, Japan; Scriba MF, South Africa S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Ito S, Tachimori Y, Terado Y, Sakon R, Narita K, Goto M. Primary malignant melanoma of the esophagus successfully treated with nivolumab: a case report. J Med Case Rep. 2021;15:237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Koga N, Kubo N, Saeki H, Sasaki S, Jogo T, Hirose K, Nakashima Y, Oki E, Koga Y, Oda Y, Oiwa H, Oiwa T, Maehara Y. Primary amelanotic malignant melanoma of the esophagus: a case report. Surg Case Rep. 2019;5:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Zhang RX, Li YY, Liu CJ, Wang WN, Cao Y, Bai YH, Zhang TJ. Advanced primary amelanotic malignant melanoma of the esophagus: A case report. World J Clin Cases. 2019;7:3160-3167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol. 1989;84:1475-1481. [PubMed] |
| 5. | Sabat J, Mannan R, Legasto A, Connery C. Long-term survivor of primary malignant melanoma of the esophagus treated with surgical resection. Int J Surg Case Rep. 2015;6C:182-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Gao S, Li J, Feng X, Shi S, He J. Characteristics and Surgical Outcomes for Primary Malignant Melanoma of the Esophagus. Sci Rep. 2016;6:23804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Sanchez AA, Wu TT, Prieto VG, Rashid A, Hamilton SR, Wang H. Comparison of primary and metastatic malignant melanoma of the esophagus: clinicopathologic review of 10 cases. Arch Pathol Lab Med. 2008;132:1623-1629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Taniyama K, Suzuki H, Sakuramachi S, Toyoda T, Matsuda M, Tahara E. Amelanotic malignant melanoma of the esophagus: case report and review of the literature. Jpn J Clin Oncol. 1990;20:286-295. [PubMed] |
| 9. | Joob AW, Haines GK 3rd, Kies MS, Shields TW. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1995;60:217-222. [PubMed] |
| 10. | Wei XJ, Zhang YN, Liu WH, Zheng XD, Zhang SH, Zhou XG. Primary malignant melanoma of esophagus. Zhonghua Binglixue Zazhi. 2018;47:548-550. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Zhou SL, Zhang LQ, Zhao XK, Wu Y, Liu QY, Li B, Wang JJ, Zhao RJ, Wang XJ, Chen Y, Wang LD, Kong LF. Clinicopathological characterization of ten patients with primary malignant melanoma of the esophagus and literature review. World J Gastrointest Oncol. 2022;14:1739-1757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Machado J, Ministro P, Araújo R, Cancela E, Castanheira A, Silva A. Primary malignant melanoma of the esophagus: a case report. World J Gastroenterol. 2011;17:4734-4738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Diagnosis And Treatment Guidelines For Colorectal Cancer Working Group CSOCOC. Chinese Society of Clinical Oncology (CSCO) diagnosis and treatment guidelines for colorectal cancer 2018 (English version). Chin J Cancer Res. 2019;31:117-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 134] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 14. | Chinese guidelines for diagnosis and treatment of melanoma 2018 (English version). Chin J Cancer Res. 2019;31:578-585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Davey MG, Miller N, McInerney NM. A Review of Epidemiology and Cancer Biology of Malignant Melanoma. Cureus. 2021;13:e15087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 16. | Medical Administration of the National Health Care Commission of the People's Republic of China. Standardization for diagnosis and treatment of esophageal cancer (2022 edition). Zhonghua Xiaohuawaike Zazhi. 2022;21:1247-1268. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 17. | Jansson C, Oh JK, Martinsen JI, Lagergren J, Plato N, Kjaerheim K, Pukkala E, Sparén P, Tryggvadottir L, Weiderpass E. Occupation and risk of oesophageal adenocarcinoma and squamous-cell carcinoma: The Nordic Occupational Cancer Study. Int J Cancer. 2015;137:590-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Teng Y, Guo R, Sun J, Jiang Y, Liu Y. Reactive capillary hemangiomas induced by camrelizumab (SHR-1210), an anti-PD-1 agent. Acta Oncol. 2019;58:388-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |