Published online Dec 27, 2023. doi: 10.4240/wjgs.v15.i12.2774
Peer-review started: October 23, 2023
First decision: November 8, 2023
Revised: November 20, 2023
Accepted: December 1, 2023
Article in press: December 1, 2023
Published online: December 27, 2023
Processing time: 65 Days and 9.9 Hours
Rectal carcinoma (RC) treatment primarily involves laparoscopic surgery, which may induce significant hemodynamic changes and weaken immune function. Certain anesthetic approaches using opioid drugs (including remifentanil and sufentanil) pose risks, such as hypotension.
To determine the effects of remifentanil combined with propofol on hemodynamics and oxidative stress in patients undergoing RC resection.
A total of 211 patients one hundred and four patients with RC treated at the First Affiliated Hospital of Dalian Medical University between November 2018 and November 2022 were retrospectively analyzed. Among them, the remifentanil group included 45 patients receiving remifentanil with propofol anesthesia and the sufentanil group included 59 patients receiving sufentanil with propofol anesthesia. Changes in the hemodynamic index, oxidative stress index, general data, consumption of remifentanil, and use of vasoactive drugs were compared. The incidences of adverse reactions were calculated.
The two groups did not significantly differ in terms of operation, anesthesia, and extubation times (P > 0.05). At 1 min after intubation, the sufentanil group showed a notably higher heart rate, systolic blood pressure (SBP), diastolic blood pressure, and mean arterial pressure (MAP) compared with the remifentanil group (P < 0.05), whereas the sufentanil group showed a notably higher SBP and MAP compared with the remifentanil group at 5 min after pneumoperitoneum (P < 0.05). Thirty minutes after surgery, the remifentanil group showed significantly lower plasma cortisol, noradrenaline, and glucose levels than the sufentanil group (P < 0.001). The remifentanil group consumed significantly less remifentanil than the sufentanil group (P < 0.05), and the adoption frequency of ephedrine was lower in the remifentanil group than that in the sufentanil group (P < 0.05). The incidence of hypotension was notably higher in the sufentanil group than that in the remifentanil group (P < 0.05).
Remifentanil combined with propofol can improve hemodynamics and relieve oxidative stress in patients undergoing RC resection.
Core Tip: This study evaluated the effects of remifentanil combined with propofol on the hemodynamics and oxidative stress in patients undergoing rectal carcinoma surgery. These findings indicate that this combination improves hemodynamic stability, reduces oxidative stress, and results in a lower incidence of hypotension compared with sufentanil alone. Furthermore, the remifentanil-propofol combination requires less remifentanil consumption and reduced use of ephedrine, suggesting that it is a more effective and potentially safer anesthetic approach for these surgeries.
- Citation: Huang J, Tian WJ. Effects of remifentanil combined with propofol on hemodynamics and oxidative stress in patients undergoing resection of rectal carcinoma. World J Gastrointest Surg 2023; 15(12): 2774-2782
- URL: https://www.wjgnet.com/1948-9366/full/v15/i12/2774.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i12.2774
Rectal carcinoma (RC) has gradually increased and become the third most frequently diagnosed cancer worldwide owing to the influences of eating habits, obesity, and lifestyle[1]. Laparoscopic surgery has become the primary surgical method for treating RC[2]. As a traumatic procedure, laparoscopic surgery for RC may trigger hemodynamic changes and weaken immune function, affecting the postoperative rehabilitation of patients[3]. With an aging population, the number of older patients with RC is increasing annually. A growing number of studies show that RC mostly occurs in middle-aged and older people (40-60 years old) with declining physical functions; therefore, they have poor tolerance to surgery and anesthesia[4,5]. Cancer may cause various complications without proper treatment, further aggravating the patient’s hemodynamic and oxidative stress processes and triggering body dysfunction[6]. Therefore, it is crucial to maintain stable hemodynamics during surgery because it helps reduce postoperative morbidity and mortality and can improve patient prognosis.
Opioid drugs act on the central nervous system, which can reduce sympathetic nerve tension and enhance vagal and parasympathetic nerve tension; therefore, they are extensively used in surgical anesthesia to reduce the stress response[7,8]. Sufentanil is the most potent opioid analgesic, with 5-10 times the analgesic effect of fentanyl and a quick and long-lasting effect[9]. However, approximately one-third of intraoperative hypotension cases occur after anesthesia induction and before incision[10], and the continuous action of sufentanil may lead to hypotension and bradycardia. Remifentanil is an opioid with the fastest onset and metabolism; however, its analgesic effect rapidly fades, and high-dose administration may trigger hyperalgesia[11]. Therefore, it is probably necessary to administer sufentanil before pneumoperitoneum. Currently, sufentanil combined with propofol, a powerful analgesic with a long-acting time is usually used in clinical anesthesia induction for laparoscopic surgery of RC[12]. However, sufentanil combined with propofol induces hypotension in 36.5% of patients, and intraoperative hypotension is closely associated with acute kidney injury and 30-day postoperative mortality[13,14].This study determined the effects of remifentanil combined with propofol on hemodynamics and oxidative stress in patients undergoing RC resection.
A total of 211 patients with RC treated at the First Affiliated Hospital of Dalian Medical University between November 2018 and November 2022 were retrospectively analyzed. However, 104 patients were included based on the inclusion and exclusion criteria. Among them, 45 patients who were anesthetized with remifentanil combined with propofol were assigned to the remifentanil group, and the remaining 59 patients who were anesthetized with sufentanil combined with propofol were assigned to the sufentanil group.
Inclusion criteria: patients who met the requirements of RC and were diagnosed with RC according to pathological examination; patients in class I–II in terms of American Society of Anesthesiologists (ASA) classification; patients between 40-70 years old; patients with a body mass index (BMI) of 18-30 kg/m2; and patients with detailed pathological data.
Exclusion criteria: Patients with severe hypertension or cardio-cerebrovascular disease; patients who have undergone surgery; patients with severe liver or kidney disease; patients allergic to opioid drugs; and patients with long-term use of analgesic drugs, comorbidities with other tumor diseases, coagulation dysfunction, and immune deficiency.
After the patient entered the room, a venous channel in the upper limb was established, and the patient was monitored using an electrocardiogram for blood pressure and oxygen saturation. Parameters, such as blood pressure, stroke volume, cardiac output, cardiac index, and stroke index were dynamically monitored using the LiDCO system (LIDCO, England). The doses of remifentanil and sufentanil were calculated in advance and diluted in a 20-mL syringe: (1) During anesthesia induction, each patient in the remifentanil group was given 1 μg/kg remifentanil (concentration: 5 μg/mL) through intravenous administration, and each patient in the sufentanil group was given 0.3 μg/kg sufentanil (concentration: 1.5 μg/mL) through intravenous administration. The drugs were injected through the pump within 60 min. Subsequently, each patient in the two groups was injected with 2 mg/kg propofol through a pump (within 30 s) and then given 0.6 mg/kg rocuronium after losing consciousness. Tracheal intubation was performed using a video laryngoscope when the Tetralogy of Fallot was 0; (2) Mechanical ventilation was performed after tracheal intubation, with a tidal volume of 8 mL/kg and a breathing frequency of 10-14 times/min. The respiratory parameters were adjusted to maintain pressure of CO2 at the end of respiration (PETCO2) in the range of 35-45 mmHg according to the partial PETCO2. The oxygen flow rate of the inhaled air was adjusted to 2 L/min, and the ratio of O2 to N2O was adjusted to 1:1 (FiO2 = 0.5). The sevoflurane was inhaled into the minimum alveolar concentration at 0.8-1.0%; (3) At 3 min before pneumoperitoneum, 0.3 μg/kg sufentanil was added to the remifentanil group, and the same amount of normal saline was given to the sufentanil group. Both groups received propofol at 50 μg/kg/min and remifentanil at 0.1 μg/kg/min through pumping injection. During the surgery, intravenous inhalation combined with anesthesia was used to maintain muscle relaxation, with 0.2 mg/kg rocuronium added intermittently. After the operation, the pump dose of remifentanil was adjusted according to blood pressure and heart rate (HR), and the pump dose of propofol was adjusted to maintain a Bispectral index between 40 and 60; (4) Ramosetron and ketorolac tromethamine were administered 30 min before the end of the surgery, and local infiltration of ropivacaine was postoperatively administered to the wound. Multimode analgesia methods, such as in
The clinical data and laboratory indices of the patients were analyzed based on pathology records and reexamination. The clinical data included sex, age, ASA classification, BMI value, and medical history. General data included operation time, anesthesia time, extubation time, consumption of remifentanil, and the frequency and dosage of vasoactive drugs for maintenance during surgery. The incidence of anesthesia-related adverse reactions was also recorded. Outcome measures included HR, arterial systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), cortisol (Cor), norepinephrine (NE), and glucose (Glu).
Primary outcome measures: The two groups were compared in the changes in hemodynamic indices before anesthesia (T0), at 1 min after intubation (T1), before pneumoperitoneum (T2), 5 min after pneumoperitoneum (T3), and after surgery (T4). Changes in oxidative stress indices before and 30 min after surgery were compared. Secondary outcome measures: The clinical data, general characteristics, consumption of remifentanil and the use of vasoactive drugs, and the adverse reactions of the two groups were compared.
The Kolmogorov-Smirnov normality of continuous variables was tested using SPSS 26.0. Normally distributed measurement data are described as mean ± SD deviation. An independent-sample T-test was used for intergroup comparisons. Hemodynamic indices were analyzed using repeated-measures analysis of variance, and the post hoc test was performed using the Bonferroni test. Counting data were analyzed using the chi-square test. The number of cases was recorded, and the incidence rate was calculated. A P value < 0.05 suggests a significant difference.
There were no significant differences in sex, age, BMI, ASA classification, or medical history based on the comparison of baseline data between the two groups (P > 0.05, Table 1).
| Factors | Remifentanil group (n = 45) | Sufentanil group (n = 59) | χ2 value | P value |
| Sex | 0.035 | 0.850 | ||
| Male | 26 | 33 | ||
| Female | 19 | 26 | ||
| Age | 0.373 | 0.541 | ||
| < 60 yr old | 24 | 35 | ||
| ≥ 60 yr old | 21 | 24 | ||
| BMI | 0.148 | 0.700 | ||
| ≥ 25 kg/m2 | 20 | 24 | ||
| < 25 kg/m2 | 25 | 35 | ||
| ASA classification | 3.141 | 0.208 | ||
| I | 21 | 18 | ||
| II | 22 | 39 | ||
| III | 2 | 2 | ||
| History of diabetes mellitus | 3.083 | 0.079 | ||
| Yes | 17 | 13 | ||
| No | 28 | 46 | ||
| History of hypertension | 1.590 | 0.207 | ||
| Yes | 40 | 47 | ||
| No | 5 | 12 | ||
| History of smoking | 0.035 | 0.850 | ||
| Yes | 26 | 33 | ||
| No | 19 | 26 |
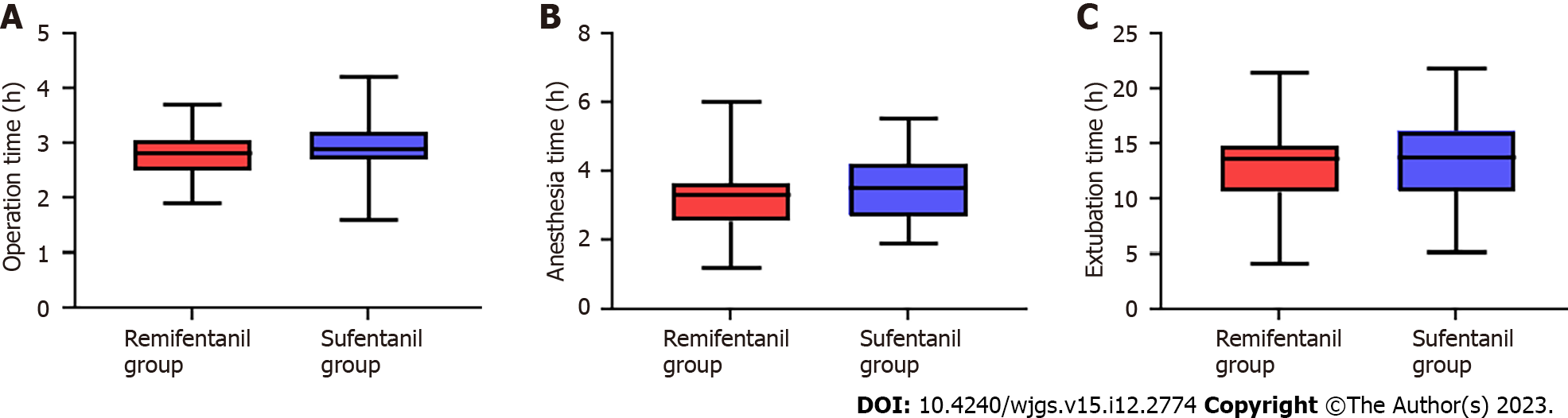
Surgical, anesthesia, and extubation times were not significantly different between the two groups (P > 0.05, Figure 1, Table 2).
| Group | Operation time | Anesthesia time | Extubation time |
| Remifentanil group (n = 45) | 2.76 ± 0.44 | 3.25 ± 0.89 | 12.95 ± 3.49 |
| Sufentanil group (n = 59) | 2.94 ± 0.49 | 3.49 ± 0.95 | 13.71 ± 3.67 |
| t value | 1.942 | 1.312 | 1.059 |
| P value | 0.055 | 0.192 | 0.292 |
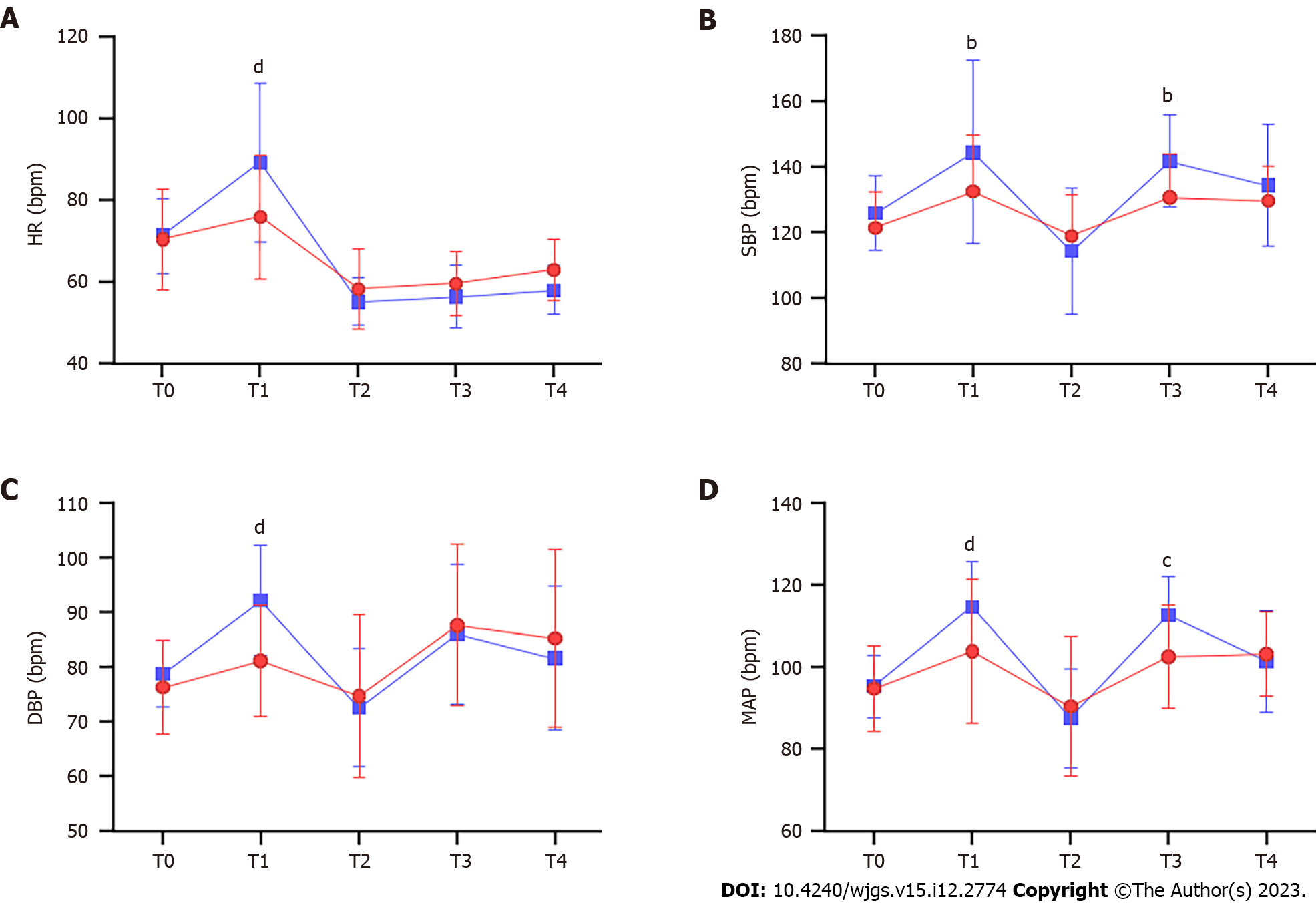
The two groups were not significantly different in the levels of HR, SBP, DBP, and MAP at T0, T2, and T4 (P > 0.05, Figure 2); however, the sufentanil group showed significantly higher levels of HR, SBP, DBP, and MAP compared with the remifentanil group at T1 (P < 0.05, Figure 2). The sufentanil group showed significantly higher levels of SBP and MAP than the remifentanil group at T3 (P < 0.05, Figure 2), although the levels of HR and DBP were not significantly different between the two groups (P > 0.05, Figure 2).
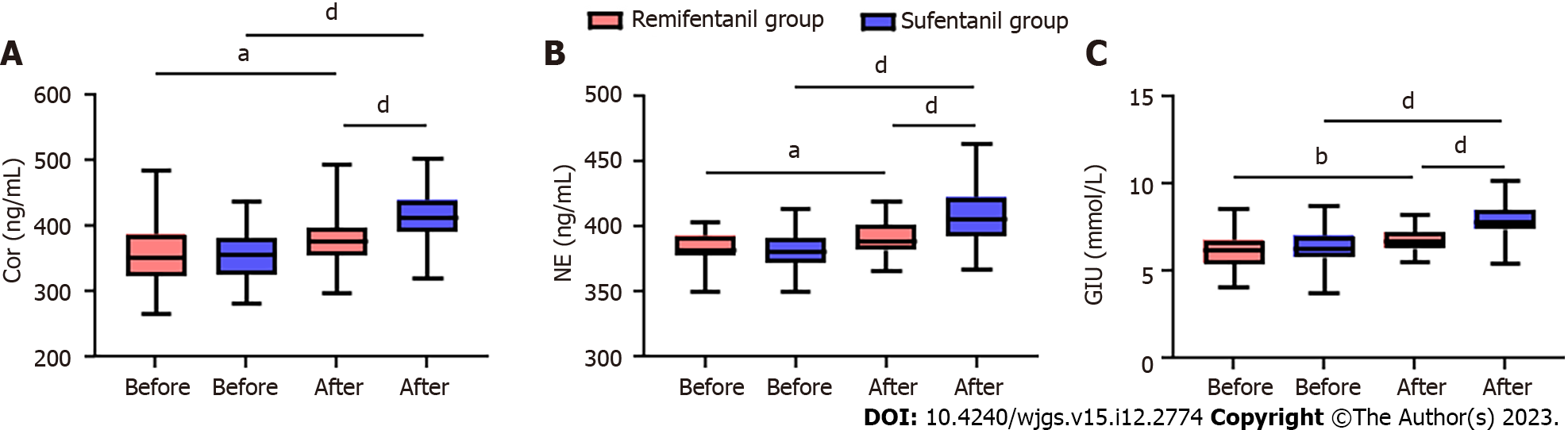
The levels of Cor, NE, and Glu were not significantly different between the two groups (P > 0.05, Figure 3), whereas Cor, NE, and Glu significantly increased in both groups 30 minutes after surgery (P < 0.001, Figure 3). In addition, the remifentanil group showed significantly lower levels of Cor, NE, and Glu compared with the sufentanil group 30 minutes after surgery (P < 0.001, Figure 3).
This study evaluated the consumption of remifentanil and vasoactive drugs in the two groups. The remifentanil group consumed significantly less remifentanil than the sufentanil group (P < 0.05, Table 3), and the frequency of ephedrine use was lower in the remifentanil group than in the sufentanil group (P < 0.05, Table 3).
| Indices | Remifentanil group (n = 45) | Sufentanil group (n = 59) | χ2/t | P value |
| Consumption of remifentanil (μg/kg/h) | 2.68 ± 0.51 | 3.89 ± 1.10 | 6.881 | < 0.001 |
| Adoption frequency of ephedrine | 10 | 31 | 9.827 | 0.002 |
| Adoption frequency of atropine | 11 | 7 | 2.823 | 0.092 |
The statistical analysis of the incidence of adverse reactions in the two groups showed no significant differences in the incidences of nausea and vomiting, choking cough, hypotension, and bradycardia between the remifentanil and sufentanil groups (P > 0.05). However, it is worth noting that the remifentanil group had a significantly lower incidence of hypotension compared to that in the sufentanil group (P = 0.002, Table 4).
| Group | Nausea and vomiting | Choking cough | Hypotension | Bradycardia |
| Remifentanil group (n = 45) | 3 | 1 | 10 | 8 |
| Sufentanil group (n = 59) | 5 | 2 | 30 | 18 |
| χ2 value | 0.117 | 0.124 | 8.838 | 2.207 |
| P value | 0.731 | 0.724 | 0.002 | 0.137 |
The incidence of RC is high[15]. Over the past few years, RC has shown an increasing incidence and has become one of the main human health-endangering diseases with the improvement of living standards and changes in diet structure[16]. Laparoscopic surgery is the primary method to treat RC, with a high success rate and rapid postoperative recovery that can effectively prevent disease progression[17]. However, it is an invasive procedure that may trigger a strong stress reaction and hemodynamic changes, ultimately reducing the immune function of patients and increasing the risk of postoperative infections. Accordingly, it is of great importance to find a scientific and safe anesthetic method for successful surgeries[18]. The choice of an anesthesia method directly affects surgical outcomes.
Propofol is an intravenous drug with many advantages, such as the ability to protect tissues and organs, regulate immunity, calm, inhibit platelet aggregation, and relieve pain[19]. It is widely favored owing to its short awakening time, strong control, and low harm[20]. However, there are some shortcomings to analgesia with a single drug. A low dose makes achieving the ideal analgesic effect difficult, while a high dose increases the risk of adverse reactions, such as respiratory depression[21]. Therefore, multimodal analgesia is advocated in clinical practice to achieve optimal anesthetic effects. Sufentanil and remifentanil are two kinds of opioid analgesics. Their main function is to bind to the μ opioid receptor, which has higher opioid receptor affinity than the traditional opioid analgesic drug, fentanyl; therefore, they provide stronger analgesic intensity and longer action time[22]. The autonomic nervous system is stimulated during anesthesia induction, laryngoscope implantation, and endotracheal intubation, resulting in a reflex increase in blood pressure and HR[23]. In addition, anesthetic drugs can dilate the blood vessels and inhibit the central nervous system, and tracheal intubation without surgical stimulation can lead to hypotension[24]. Therefore, the key in general anesthesia is to reduce the fluctuation of hemodynamics as much as possible to reduce the sharp increase in blood pressure and HR during intubation and pneumoperitoneum and to avoid the obvious decrease in blood pressure and HR before pneumoperitoneum after intubation. In this study, the blood pressure (SBP, DBP, and MAP) and HR of the sufentanil group were significantly higher than those of the remifentanil group at T1. However, Xue et al[25] revealed that 0.3 µg/kg sufentanil can completely eliminate the cardiovascular response during intubation; therefore, old age and poor cardiovascular reserve capacity in our study may have led to more severe hemodynamic fluctuations. In the remifentanil group, sufentanil was administered 3 min before pneumoperitoneum, which played a preemptive analgesic role; therefore, the increase in blood pressure and HR at T3 was not obvious. In addition, the consumption of remifentanil in the remifentanil group was lower, which may be because sufentanil was given before pneumoperitoneum, which inhibited the stress response after pneumoperitoneum more completely and relatively lowered the requirement of remifentanil during surgery.
Remifentanil combined with propofol can inhibit the secretion of pituitary and adrenal cortical hormones during anesthesia and can also reduce surgical trauma-induced stimulation, stress response, and adverse reactions[26,27]. In this study, the stress response indices (serum Cor, NE, and Glu levels) of the two groups increased during the surgery, but the range of increase in the remifentanil group was relatively small, suggesting that the combined application of propofol and sufentanil can significantly reduce the stress response of patients undergoing RC resection. We believe this is because remifentanil has an antioxidant effect that can neutralize free radicals and reduce oxidative damage, thus reducing the occurrence of oxidative stress[26,28]. In addition, remifentanil can inhibit inflammatory reactions and cytokine production, thus weakening the immune and inflammatory reactions in the body and reducing oxidative stress[29]. Moreover, the use of ephedrine before the induction of pneumoperitoneum in this study was statistically different between the two groups, and both usage methods reduced the occurrence of hypotension after induction, indicating that low-dose remifentanil combined with sufentanil could lower the occurrence of hypotension to some extent compared with sufentanil induction.
This study verified that remifentanil combined with propofol can improve hemodynamics and relieve oxidative stress in patients undergoing RC resection. However, this study had some limitations. First, the medical records of this study were selected from patients undergoing abdominal laparoscopic surgery, and patients with severe hypertension or cardiovascular or cerebrovascular diseases were excluded; therefore, the conclusions of this study may not apply to situations outside the research object. Second, we only analyzed the samples from our center, which led to a small sample size. Therefore, we hope to conduct prospective research with more samples to validate the research conclusions.
Remifentanil combined with propofol improved hemodynamics and relieved oxidative stress in patients undergoing RC resection. Therefore, a combination of the remifentanil and propofol can be a more effective anesthetic strategy for RC resection.
Rectal carcinoma (RC) is a major health problem with an increasing incidence. The primary treatment is laparoscopic surgery, which can induce significant hemodynamic changes and weaken immune function. Anesthesia often involves opioid drugs such as remifentanil and sufentanil that may cause hypotension.
It is necessary to understand the impact of different anesthesia methods on hemodynamics and oxidative stress during RC. Investigating the effects of remifentanil combined with propofol may offer insights into the best management of patient health during and after surgery.
The primary objective of this study was to determine the effects of remifentanil combined with propofol on hemodynamics and oxidative stress in patients undergoing RC resection.
A retrospective analysis was conducted using the data of 104 patients with RC who were treated at a hospital between November 2018 and November 2022. Patients were divided into two groups based on the type of anesthesia received: Remifentanil and sufentanil. Various factors were compared between the two groups, including changes in hemodynamic indices, oxidative stress indices, general data, consumption of remifentanil, and use of vasoactive agents.
The remifentanil group had a notably lower heart rate (HR), systolic blood pressure, diastolic blood pressure, mean arterial pressure, plasma cortisol, noradrenaline, and glucose levels during different stages of surgery than the sufentanil group. The remifentanil group also consumed less remifentanil and showed lower adoption of ephedrine. Moreover, the sufentanil group showed a notably higher incidence of hypotension compared with the remifentanil group.
The combined use of remifentanil and propofol can improve hemodynamics and relieve oxidative stress for patients undergoing RC resection. Specifically, the remifentanil group demonstrated lower HR, blood pressure, and stress hormone levels and experienced fewer instances of hypotension than the sufentanil group. In addition, the remifentanil group consumed less remifentanil and had a lower frequency of ephedrine use. These findings suggest that a combination of remifentanil and propofol may be a feasible and beneficial anesthetic approach for such surgical procedures. However, the applicability of these conclusions to patients with severe hypertension or cardiovascular or cerebrovascular disease remains unclear and requires further investigation.
Remifentanil combined with propofol can improve hemodynamics and relieve oxidative stress in patients undergoing RC resection. However, the conclusions of this study might not apply to patients with severe hypertension or cardiovascular or cerebrovascular diseases owing to the research limitations. Further research with a more diverse patient sample and a prospective study design is recommended to verify these findings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ernst M, Australia; Haidich AB, Greece S-Editor: Qu XL L-Editor: A P-Editor: Yu HG
| 1. | Sun R, Dai Z, Zhang Y, Lu J, Xiao Y. The incidence and risk factors of low anterior resection syndrome (LARS) after sphincter-preserving surgery of rectal cancer: a systematic review and meta-analysis. Support Care Cancer. 2021;29:7249-7258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 2. | Guan X, Wei R, Yang R, Lu Z, Liu E, Zhao Z, Chen H, Yang M, Liu Z, Jiang Z, Wang X. Association of Radiotherapy for Rectal Cancer and Second Gynecological Malignant Neoplasms. JAMA Netw Open. 2021;4:e2031661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 3. | Stoffel EM, Murphy CC. Epidemiology and Mechanisms of the Increasing Incidence of Colon and Rectal Cancers in Young Adults. Gastroenterology. 2020;158:341-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 379] [Article Influence: 75.8] [Reference Citation Analysis (1)] |
| 4. | Ye YJ. [Surgical treatment of presacral recurrent rectal cancer]. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23:445-450. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Salibasic M, Pusina S, Bicakcic E, Pasic A, Gavric I, Kulovic E, Rovcanin A, Beslija S. Colorectal Cancer Surgical Treatment, our Experience. Med Arch. 2019;73:412-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Yang Y, Wang HY, Chen YK, Chen JJ, Song C, Gu J. Current status of surgical treatment of rectal cancer in China. Chin Med J (Engl). 2020;133:2703-2711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Nath TS. Effectiveness of Low-Dose Ketamine Infusion in Opioid Refractory Cancer Pain: A Case Report. Cureus. 2022;14:e31662. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Sasada S, Ukon K, Sato Y. [A patient continued anti-cancer treatment because of effective colostomy against pain with defecation by local recurrence of rectal cancer]. Gan To Kagaku Ryoho. 2013;40:811-813. [PubMed] |
| 9. | Liang M, Xv X, Ren C, Yao Y, Gao X. Effect of ultrasound-guided transversus abdominis plane block with rectus sheath block on patients undergoing laparoscopy-assisted radical resection of rectal cancer: a randomized, double-blind, placebo-controlled trial. BMC Anesthesiol. 2021;21:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Lyu SG, Lu XH, Sun XT, Li CJ, Miao C. [Effects of S(+)-ketamine combined with sufentanil for patient-controlled intravenous analgesia on the early recovery in elderly patients undergoing laparoscopic radical resection of rectal cancer]. Zhonghua Yi Xue Za Zhi. 2021;101:3238-3243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Ping-Chen, Lin QS, Lin XZ. Optimal concentration of the transversus abdominis plane block in enhanced recovery after surgery protocols for patients of advanced age undergoing laparoscopic rectal cancer surgery. J Int Med Res. 2018;46:4437-4446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Uchida K, Yasunaga H, Miyata H, Sumitani M, Horiguchi H, Matsuda S, Yamada Y. Impact of remifentanil use on early postoperative outcomes following brain tumor resection or rectal cancer surgery. J Anesth. 2012;26:711-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Maheshwari K, Turan A, Mao G, Yang D, Niazi AK, Agarwal D, Sessler DI, Kurz A. The association of hypotension during non-cardiac surgery, before and after skin incision, with postoperative acute kidney injury: a retrospective cohort analysis. Anaesthesia. 2018;73:1223-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 175] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 14. | Monk TG, Bronsert MR, Henderson WG, Mangione MP, Sum-Ping ST, Bentt DR, Nguyen JD, Richman JS, Meguid RA, Hammermeister KE. Association between Intraoperative Hypotension and Hypertension and 30-day Postoperative Mortality in Noncardiac Surgery. Anesthesiology. 2015;123:307-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 402] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 15. | Wilkinson N. Management of Rectal Cancer. Surg Clin North Am. 2020;100:615-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 16. | Bachet JB, Benoist S, Mas L, Huguet F. [Neoadjuvant treatment for rectal cancer]. Bull Cancer. 2021;108:855-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Fernandes MC, Gollub MJ, Brown G. The importance of MRI for rectal cancer evaluation. Surg Oncol. 2022;43:101739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 79] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 18. | Quezada-Diaz FF, Smith JJ. Nonoperative Management for Rectal Cancer. Hematol Oncol Clin North Am. 2022;36:539-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Enlund M, Berglund A, Andreasson K, Cicek C, Enlund A, Bergkvist L. The choice of anaesthetic--sevoflurane or propofol--and outcome from cancer surgery: a retrospective analysis. Ups J Med Sci. 2014;119:251-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 140] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 20. | Stogiannou D, Protopapas A, Tziomalos K. Is propofol the optimal sedative in gastrointestinal endoscopy? Acta Gastroenterol Belg. 2018;81:520-524. [PubMed] |
| 21. | Gao X, Mi Y, Guo N, Luan J, Xu H, Hu Z, Wang N, Zhang D, Gou X, Xu L. The mechanism of propofol in cancer development: An updated review. Asia Pac J Clin Oncol. 2020;16:e3-e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 22. | Sridharan K, Sivaramakrishnan G. Comparison of Fentanyl, Remifentanil, Sufentanil and Alfentanil in Combination with Propofol for General Anesthesia: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Curr Clin Pharmacol. 2019;14:116-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 23. | Liu YH, Hu XB, Yang XM, Wang YW, Deng M. Comparing remifentanil and sufentanil in stress reduction during neurosurgery: a randomised controlled trial. Int J Clin Pharm. 2020;42:1326-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Qin Z, Xu Y. Effects of Remifentanil and Sufentanil Anesthesia on Cardiac Function and Serological Parameters in Congenital Heart Surgery. J Healthc Eng. 2021;2021:4650291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Xue FS, Xu YC, Liu Y, Yang QY, Liao X, Liu HP, Zhang YM, Liu JH, Luo MP. Different small-dose sufentanil blunting cardiovascular responses to laryngoscopy and intubation in children: a randomized, double-blind comparison. Br J Anaesth. 2008;100:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Cheng M, Wu X, Wang F, Tan B, Hu J. Electro-Acupuncture Inhibits p66Shc-Mediated Oxidative Stress to Facilitate Functional Recovery After Spinal Cord Injury. J Mol Neurosci. 2020;70:2031-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Zhou M, Xu W, Wang J, Yan J, Shi Y, Zhang C, Ge W, Wu J, Du P, Chen Y. Boosting mTOR-dependent autophagy via upstream TLR4-MyD88-MAPK signalling and downstream NF-κB pathway quenches intestinal inflammation and oxidative stress injury. EBioMedicine. 2018;35:345-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 260] [Cited by in RCA: 254] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 28. | Yoon JY, Park CG, Park BS, Kim EJ, Byeon GJ, Yoon JU. Effects of Remifentanil Preconditioning Attenuating Oxidative Stress in Human Dermal Fibroblast. Tissue Eng Regen Med. 2017;14:133-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Li X, Xiang H, Zhang W, Peng C. The effects of remifentanil combined with propofol on the oxidative damage and the stress and inflammatory responses in cardiac surgery patients. Am J Transl Res. 2021;13:4796-4803. [PubMed] |