Published online Dec 27, 2023. doi: 10.4240/wjgs.v15.i12.2709
Peer-review started: September 20, 2023
First decision: October 20, 2023
Revised: October 26, 2023
Accepted: November 24, 2023
Article in press: November 24, 2023
Published online: December 27, 2023
Processing time: 97 Days and 15.2 Hours
Post-cholecystectomy iatrogenic bile duct injuries (IBDIs), are not uncommon and although the frequency of IBDIs vary across the literature, the rates following the procedure of laparoscopic cholecystectomy are much higher than open cho
Core Tip: Post-cholecystectomy iatrogenic bile duct injuries are not uncommon and hence deserve paying attention from surgeons, gastroenterologists and interventional radiologists. Multidisciplinary team is advised aiming to early and appropriately diagnose such injuries, tailor treatment for cases on an individual base. Surgical treatment is the immediate solution for bile duct injuries diagnosed intraoperative in the context of available experienced hepato-biliary surgeon. Endoscopic treatment looks promising and effective treatment options for injuries diagnosed after the surgery, while interventional endoscopic procedures looks valuable for patients with failed endoscopy and patients who had altered anatomy.
- Citation: Emara MH, Ahmed MH, Radwan MI, Emara EH, Basheer M, Ali A, Elfert AA. Post-cholecystectomy iatrogenic bile duct injuries: Emerging role for endoscopic management. World J Gastrointest Surg 2023; 15(12): 2709-2718
- URL: https://www.wjgnet.com/1948-9366/full/v15/i12/2709.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i12.2709
Iatrogenic bile duct injuries (IBDIs) refer to the injuries that affect the biliary system due to many interventions particularly surgery, but these injuries may also follow other invasive procedures including endoscopy and interventional radiology. The frequency of IBDIs parallel the advancements achieved in the hepato-biliary surgeries although also described after other abdominal surgeries. It is obvious from many reports in the literature that post-cholecystectomy IBDIs showed a remarkable rise with the introduction of laparoscopic cholecystectomy (LC)[1] decades back and that is why reports of IBDIs emerged from different geographic locations. It seems that the frequency of IBDIs following LC is on the rise because of many reasons including the widespread popularity of the procedure globally and that is why practice guidelines were developed in order not only to reduce the frequency of such injuries, but also to secure optimal diagnosis and effective management plans which ultimately reduces the morbidity and mortality associated with such injuries and improves the quality of life among those patients[2].
The prevalence of IBDIs vary in the literature. After cholecystectomy the cumulative incidence across the literature is 0.1% to 3%. Following an open cholecystectomy the frequency range between 0.1 and 0.5 %, while after the LC the risk is even doubled[3-5], and the frequency is increased in the setting of acutely inflamed gallbladder (GB), while bile duct injuries after biliary endoscopy, interventional radiology and liver biopsy is incidentally reported[6].
There are many systems for classification of IBDIs. However, the most commonly used are Bismuth scale and Strasberg classification[1].
The clinical manifestations are usually linked to the surgical event and the presenting manifestations vary. Early in the post-operative period, manifestations may include abdominal pain, abdominal distension, fever, bile flow from the surgical drains, peritonitis, biliary ascites, and cholangitis[4,7-10]. While, later jaundice may be the leading manifestation[9-12]. However, most of the cases present with a combination of these of manifestations[4,8,13]. Complicated and improperly treated cases are associated with severe adverse events including biliary cirrhosis, liver failure, high health care related cost and even mortality[1,9]. Consequently, IBDIs are a real challenge to the quality of life and is associated with negative psychological impact on patients and their relatives[2].
Risk factors associated with IBDIs vary and can be categorized mainly into operator and patient related factors. Operator’s years of experience, ability to efficiently perform LC, as well as effectiveness of managing complication fall among the most important operator factors. Most IBDIs are due to misidentification of biliary anatomy during clipping or ligature or abnormal anatomy e.g. anomalous cystic duct insertion and these are usually common following LC[1,8]. Another important cause of IBDIs is ischemia that commonly complicate open procedures when over devascularization deprives the bile ducts from its blood supply[2,5,8]. On the other hand, disease related factors impact directly the IBDIs, for example operating upon acutely inflamed and fibrotic wall GB on an emergency setting is more risky than operating elective on non-fibrotic GB[1,2]. Furthermore, the workplace environment had an indirect impact, for instance a tertiary referral center with high volume of cholecystectomies and structured training program for junior surgeons is associated with lower risk of injuries and in addition it is associated with better outcomes on dealing with such injuries. Other patient related factors e.g. obesity, bleeding profile and male gender were associated with the increased risk of IBDIs[1].
Accurate diagnosis of IBDIs is ideally through witnessing the injury[10], this is only achievable in 30% of cases during the surgery and consequently most cases are diagnosed post-operatively[7]. However, it is sometimes challenging to determine the nature and site of the biliary injury especially during the operation and that is why final diagnosis is based on a combination of clinical and imaging data.
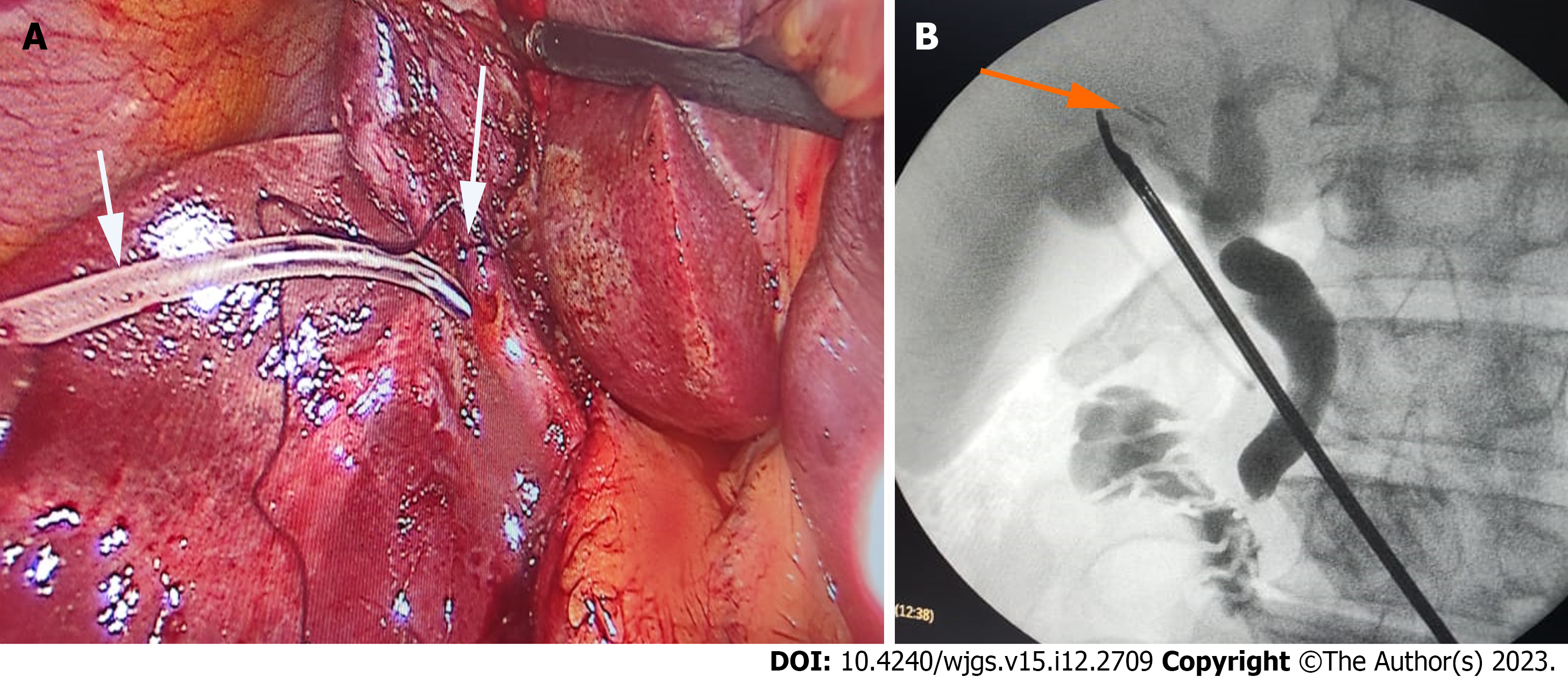
During the past decades the preferred intra-operative investigation was cholangiography (Figure 1), although con
Of the imaging modalities used, abdominal ultrasonography (US) is usually the first choice for diagnosis of suspected IBDIs after surgery because it is readily available, cheap, reproducible, and can detect intra-abdominal free fluid and collections in the surgical bed together with comment on the intrahepatic biliary radicles but its major limitation is, its inability to determine the site of the injury[3,4,7-9].
Consequently, another modality is usually needed. Endoscopic Retrograde Cholangio-Pancreatography (ERCP) was the diagnostic modality despite the lack of the 100% specificity[1,2]. Since its development, Magnetic Resonance Cholangio-Pancreatography (MRCP) (Figure 2) had been the imaging modality of choice for mapping the biliary tree with sensitivity and specificity up to 100%, at the expense of ERCP role as a diagnostic modality[15]. In addition to MRCP or ERCP, in severe IBDIs (e.g. a complete transection) a CT-angiography should also be performed, in order to diagnose concomitant vascular injury, which is often missed.
The optimal timing for managing IBDIs vary according to the time of its diagnosis. Injuries diagnosed intra-operatively per the current practice guidelines are treated surgically in the operating theater if an experienced hepatobiliary surgeon is available. Injuries diagnosed early (within 1-2 wk) in the postoperative period can be managed conservatively, endoscopically, surgically and sometimes by intervention radiology. In many instances the management of such injuries is multidisciplinary and tailored case by case.
The surgical management of IBDIs depend upon the timing of its diagnosis as described in Figure 3. When biliary injuries are recognized during the operation, with available experienced hepatobiliary surgeon, laparoscopic CBD exploration provides direct visualization of the relevant anatomy, repair of all biliary injuries with T-tube drainage, or the surgeon may convert to open technique to explore carefully and biliary injuries are treated by Roux-en-Y hepatico-jejunostomy[16]. If the surgeon lacks experience, the operation should be finished immediately with placement of a drain and the patient be transferred to a suitable hepatobiliary surgery center[17].
If IBDIs are diagnosed early postoperative with sever peritonitis the abdominal cavity needs prompt early drainage with either intervention radiology by US or CT-guided tube drainage or open surgical drainage may be an alternative. If there is no peritonitis the bile duct system can be evaluated laparoscopically, and the clips causing partial or complete biliary occlusions be removed at the same time. If there are ischemic lesions after clip removal, stents may be placed endoscopically to minimize the risk of stenosis formation[18]. When peritonitis with severe sepsis are encountered, several weeks (2-3 wk) are needed for resolution of the acute inflammatory phase and hence the corrective surgery should be postponed[2].
For patients with complete bile duct ligation with lost ductal continuity confirmed by MRCP (Figure 2) or whose IBDIs diagnosed late postoperative, surgery is indicated without delay; the extrahepatic part of the bile duct system is to be replaced with a Roux-en-Y hepatico-jejunostomy[19].
Usually, Roux-en-Y hepatico-jejunostomy is preferable to direct reconstruction with an end-to-end anastomosis with low complication rate and good prognosis[19]. Although such reconstructions can still lead to major problems such as biliary stenosis, liver cirrhosis and may require further interventional measures such as dilatation or further surgical correction, or even liver transplantation[19].
The introduction of ERCP in management of IBDIs, reduced the need for secondary surgical interventions especially for cases with low flow biliary leaks[10,20] with acceptable long term outcomes.
Several reports in the literature figured out the efficacy of ERCP in the management of iatrogenic biliary injuries, with rates of success ranging from 80% to 100%[4,7-10]. However, the efficacy varies according to the nature of the injury with higher success rates reported for low flow leaks, and the lowest success rates for complete bile duct ligation and modest for biliary strictures.
The timing of intervention by ERCP for IBDIs management is still a matter of discussion[21], with time intervals vary from intraoperative ERCP to months after the time of the offending surgery as shown in Table 1. Most of the published literature lacks clear guidelines, and it seems that the endoscopist decision when to intervene based on the circumstances case by case is the actual practice[10].
| Ref. | Time to ERCP/day | ERCP success rate | ERCP management | Comments |
| Hii et al[10] | 8 (1-35) | 93.1% | Of the successful cases 100% of cases had stents, 63% had EST, 66.7% had 10 Fr stents | 2 cases of PEP; median time of leak resolution was 4 d (1-35) |
| Abdel-Raouf et al[7] | 29 (2-54) | 93.9% | Endoscopic therapy is safe and effective in the management of postoperative bile duct leak. For postoperative bile ductal strictures, ERCP is a less favorable option | Complications include mild acute pancreatitis, cholangitis and post-sphinctertomy bleeding |
| Yehia[9] | - | 88.9% | ERCP was used as a diagnostic test for the site of injury in this study with success rate of 93.3%, and as therapeutic option for cases of leak and biliary strictures | Closure of the fistula and complete relieve of jaundice in all patients within 2 wk |
| Emara et al[4] | 7 (0-21) | 88.46% | It was possible to notice the site and type of injury in the 26 patients. In this study, 18 patients (69.2%) had a plastic stent inserted, whereas 8 (30.8%) had no stents and managed with sphincterotomy alone. There were no adverse events related to the ERCP procedure | There were no differences between patients treated by early (first week) versus late (after the first week) ERCP regarding the needed interventions, type of BDIs, type and diameter of the inserted stents, and the overall success |
| Ghazanfar et al[8] | 27 (2-210) | 87.8% | Patients with postoperative biliary leaks fare much better than those with complete cutoff or strictures. MRCP should be done in all patients where ERCP shows loss of biliary continuity | The leak stopped 48-72 h of combined EST and stenting |
| Mavrogiannis et al[21] | - | 100% | Endoscopic therapy of biliary leaks with a small-diameter biliary stent alone is as effective and safe as EST followed by insertion of a large-diameter stent | 7.7% complication rate; Time to clinical improvement 2-6 d |
In one recently published study by our team[4], we evaluated 26 patients with IBDIs (most of them had high flow leaks due to cystic duct problems, n = 14), and we did not notice differences between early (within one week) vs late (beyond one week) intervention by ERCP regarding the success rate, the ease of papillary cannulation, type and size of the inserted stents. But, it is noticeable that most of the cases are actually referred to ERCP after one week, both in our study and many others[3,7-9], a similar practice to the real life scenario. However, it is not known whether early (within one week) ERCP intervention would be beneficial[3,4,7-9].
We think a multidisciplinary approach and combined decision should be taken before proceeding to ERCP aiming at defining the possibility of success and the probability of failure in addition to determining the next step.
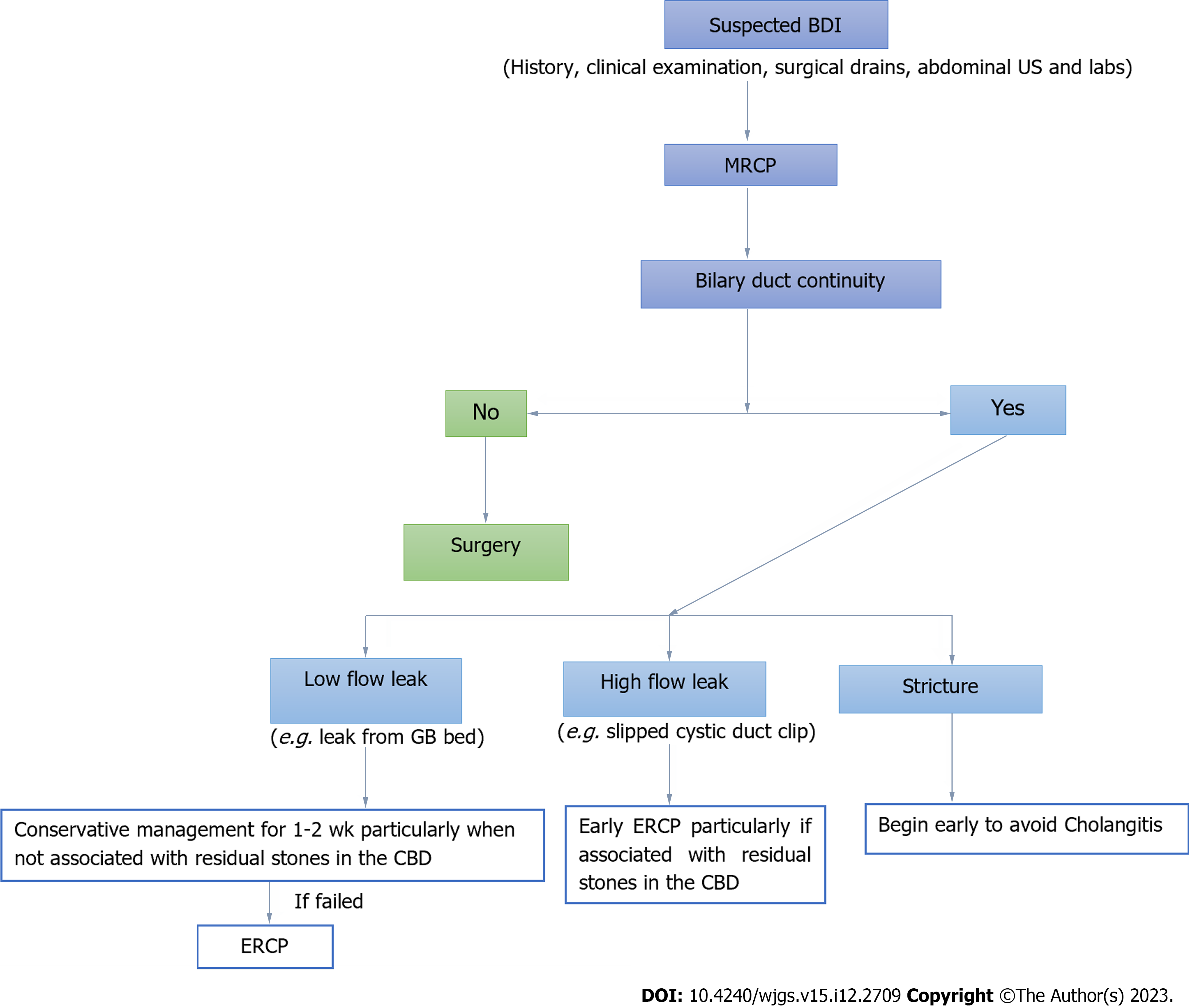
Depending on the current evidence we suggested an algorithm shown in Figure 4 for the optimal timing of ERCP management. For the simplicity, suspected IBDIs should be evaluated by full history taking, complete clinical examination, assessment of the post-operative surgical drains, laboratory investigations including liver biochemistry and abdominal US. The decision for the next step should rely on the MRCP assessment addressing the continuity and patency of biliary ductal system[15].
Lack of bile duct continuity (e.g. complete ligation or clipping of the CBD, Figures 2 and 5): Those patients should go directly to surgery without further delay, nor exposure to unnecessary ERCP. Sometimes, for lost ductal continuity without loss of tissue, a non-surgical approach can still be tried, for example combined endoscopy/interventional radiology with Rendezvous procedure followed by progressive stenting.
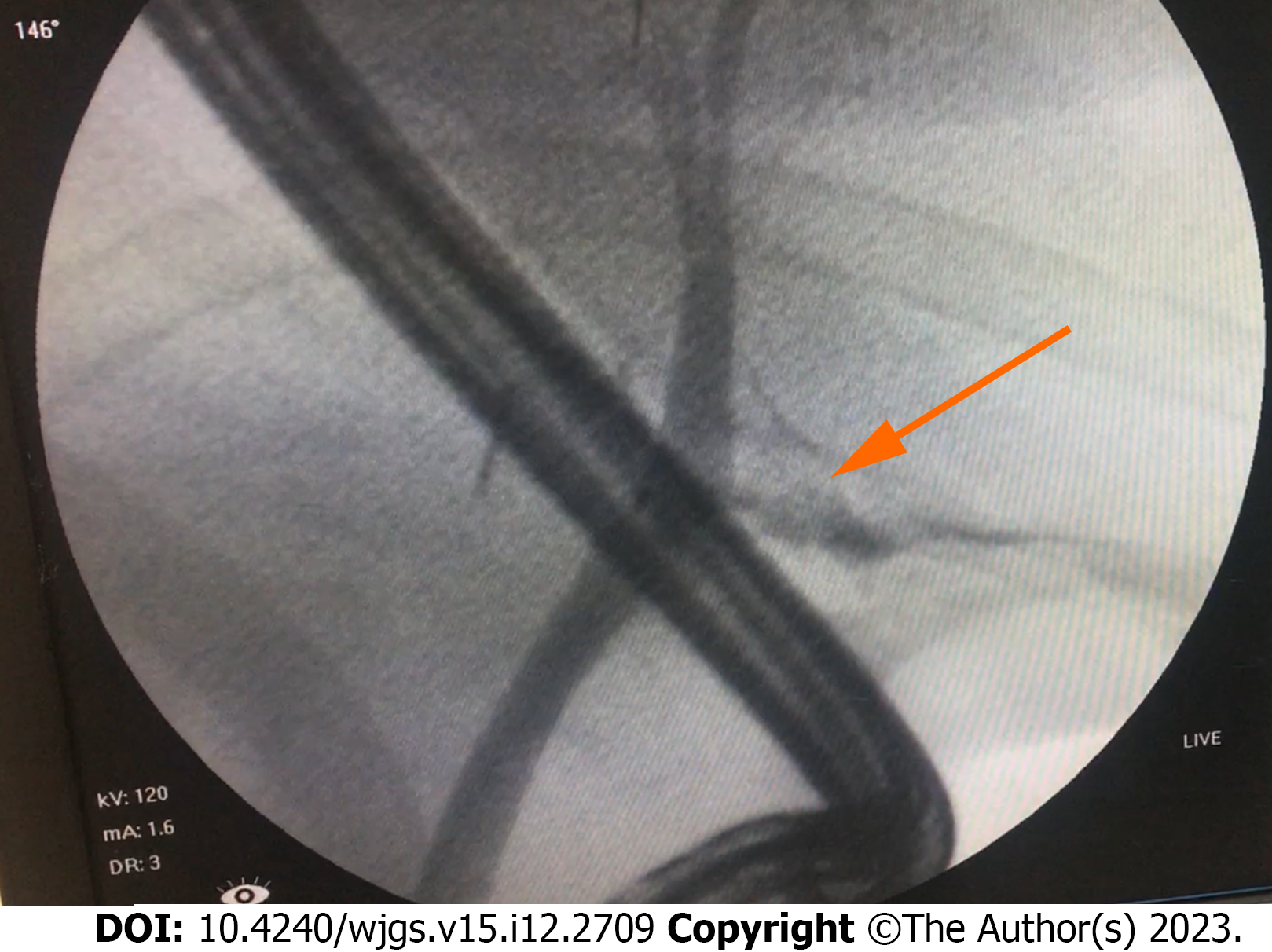
Bile duct continuity confirmed: Those patients can be further sub-divided into three categories: (1) Low-flow biliary leak (e.g. leak from the GB bed): In those patients the surgical drains output is usually mild and the associated liver biochemical abnormalities are minor ad hence lower frequency of sepsis. Previous reports showed that 4.3%[9], 6.8%[8], and 19.1%[10] of those patients may heal spontaneously over a period of 1-2 wk with conservative methods[10,22,23]. Consequently, we can recommend against early ERCP in these cases especially if associated with no residual stones in the CBD which means that the CBD pressure is not high and the bile flow across the leak is not high and there is a real chance for healing. Late ERCP may be tried for cases with continuous leak beyond 2 wk[4,8]; (2) High flow bile leaks [e.g. slipped cystic duct clips (Figure 6)]: In those patients the amount of leak is high and the output from the surgical drains is also high and ultimately the risk of sepsis is enhanced. We recommend against delay of ERCP in those cases, especially if associated with residual CBD stones, because this will increase the CBD pressure and hence increase the amount of the leak and lowers the chance of healing. In fact, those patients will benefit from both lowering CBD/duodenal pressure gradient following the limited sphincterotomy and securing the site of the leak by the positioning of a stent beyond the site of the leak; and (3) Strictures: The data about timing of ERCP for suspected or confirmed strictures are controversial. However, when a biliary stricture lesion is confirmed we recommend proceeding to ERCP due to many reasons. With strictures, there may be proximal leaks and also there may be a risk of cholangitis. Another important issue is that, this category of patients need many sessions of ERCP with balloon dilations and upgrading the inserted stents, over a period up to 24 mo[7]. Whether early ERCP may overcome early development of tight stricture is not known, but our experience favors early ERCP in those patients because it is associated with favorable outcomes.
A number of endoscopic interventions have been associated with improved outcomes in the management of IBDIs. Sphincterotomy alone has been associated with success rates up to 87.1% in the management of IBDIs; however it seems that this procedure does not fit all IBDIs. For low flow leaks, limited sphincterotomy will reduce the pressure exerted by the sphincter of Oddi and preserve the sphincter function at the same time, this will be sufficient for management of such cases[3,7,23].
However, cases of high flow leaks will not benefit from this intervention alone. In fact, those patients when treated with sphincterotomy alone up to 12% of them required reexamination with ERCP and stenting[7,24].Consequently, limited sphincterotomy plus stenting is highly recommended for treatment of IBDIs with high flow[3,7,25]. Sphincterotomy will diminish the pressure exerted over the stent while the properly inserted stent will secure the site of the leak and give chance for healing. IBDIs cases treated with stent insertion alone without sphincterotomy were associated with an increased risk of pancreatitis[7,21], and hence it seems that combined sphincterotomy plus stent insertion is the ideal management for those patients. The diameter of the inserted stents in this category of patients is also a matter of discussion. In our experience the larger 10 Fr inserted stents secure appropriate drainage and are associated with better outcomes. Mavrogianni et al[21], showed that small 7 Fr plastic stents were comparable to 10 Fr stents in the final outcomes. Other authors[4,10] reported non-significant better results with wider stents in comparison to narrower stents.
Cases with strictures are somewhat problematic, in part due to the multiple sessions of ERCP with multiple dilatations and upgrading in the number and size of the inserted stents over a period up to 24 mo, and in part due to unsatisfactory short term response rates to dilations with complications in a proportion of patients. Those cases were usually treated surgically by Roux-en-Y-hepaticojejunostomy, however after the introduction of ERCP, the majority of those cases are amenable for endoscopic management with satisfactory results. Several reports in the literature showed comparable efficacy of ERCP to bilio-enteric bypass surgery, however with less morbidity and mortality. Strictures following bile duct injury or post-exploration seem better in its response to management than ischemic stricture do[7,26,27].
In parallel with the major advancements reported in the endoscopic management of IBDIs, several interventional radiology techniques have been associated with improved outcomes among those patients. The interventional radiologic procedures can simply be categorized to either managing the consequences of IBDIs through either flow diversion e.g. percutaneous drainage of retained intrahepatic bile through catheter[28] or leak drainage e.g. drainage of biloma or peritoneal abscess[29], under guidance of US or CT or definitive treatment for the IBDIs itself and this include percutaneous insertion of stents for biliary strictures, or adjunctive role for endoscopic management through helping to gain access to the difficult cases of biliary cannulation e.g. by Rendezvous technique[28,29]. Innovative percutaneous techniques for treating refractory bile duct injuries include covered biliary stents, bile duct embolization with glue, and percutaneous hepaticojejunostomy and hepaticogastrostomy[28,29]. The complications associated with these procedures vary from technical difficulties, failures, leaks, and cholangitis to fever[28-30]. The interventional radiology procedures are superior over endoscopic procedures in patients with altered enteric passage, high up obstruction or leakage where endoscopic approach becomes impossible[28,29]. Its advantages compared to surgery were its minimal invasive nature, reduced risk of complications, and the fact that all options remain open in case of failure[28-31].
IBDIs diagnosed intraoperatively are ideally treated surgically whenever expert hepatobiliary team is available. Endoscopic management for IBDIs is promising with favorable outcomes. There is no agreement in the literature for the optimal timing to intervene with ERCP for cases of IBDIs. Consequently, we proposed an algorithm for management of cases with IBDIs; all patients with suspected IBDIs should be examined by MRCP before ERCP. Following MRCP patients with bile duct discontinuity should be referred to surgery without delay while cases with bile duct continuity should go to ERCP. For cases with low-flow leak, observation for 1-2 wk is advised, unlike cases with high-flow leak and biliary stricture; they should go to ERCP without delay. Sphincterotomy plus stenting is the ideal management of cases with IBDIs. Interventional radiologic techniques are promising options especially for cases of failed endoscopy and also for cases with altered anatomy.
The authors would thank all colleagues who helped to conduct this study. We also grateful to Ms. Stephanie Elaine Jucaba, for the help offered in figures production.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dedemadi G, Greece; Kordzaia D, Georgia S-Editor: Lin C L-Editor: A P-Editor: Cai YX
| 1. | Jabłońska B, Lampe P. Iatrogenic bile duct injuries: etiology, diagnosis and management. World J Gastroenterol. 2009;15:4097-4104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 96] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (2)] |
| 2. | de'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 3. | Manouras A, Pararas N, Antonakis P, Lagoudiannakis EE, Papageorgiou G, Dalianoudis IG, Konstadoulakis MM. Management of major bile duct injury after laparoscopic cholecystectomy: a case report. J Med Case Rep. 2009;3:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Emara MH, Ali RF, Mahmoud R, Mohamed SY. Postcholecystectomy biliary injuries: frequency, and role of early vs late endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol. 2021;33:662-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Klos D, Gregořík M, Pavlík T, Loveček M, Tesaříková J, Skalický P. Major iatrogenic bile duct injury during elective cholecystectomy: a Czech population register-based study. Langenbecks Arch Surg. 2023;408:154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 6. | Emara MH, Ibrahim IM, Radwan MI, Elbast MR. Hemobilia and Melena After Liver Biopsy: A Case Report and Review of Literature. Gastroenterology Res. 2013;6:200-203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Abdel-Raouf A, Hamdy E, El-Hanafy E, El-Ebidy G. Endoscopic management of postoperative bile duct injuries: a single center experience. Saudi J Gastroenterol. 2010;16:19-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Ghazanfar S, Qureshi S, Leghari A, Taj MA, Niaz SK, Quraishy MS. Endoscopic management of post operative bile duct injuries. J Pak Med Assoc. 2012;62:257-262. [PubMed] |
| 9. | Yehia AM. Management of cholecystectomy-induced biliary injuries at Zagazig University Hospital. Egypt J Surg. 2018;37:223-229. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Hii MW, Gyorki DE, Sakata K, Cade RJ, Banting SW. Endoscopic management of post-cholecystectomy biliary fistula. HPB (Oxford). 2011;13:699-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Schmidt SC, Settmacher U, Langrehr JM, Neuhaus P. Management and outcome of patients with combined bile duct and hepatic arterial injuries after laparoscopic cholecystectomy. Surgery. 2004;135:613-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 79] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Cameron JL, Gadacz TR. Laparoscopic cholecystectomy. Ann Surg. 1991;213:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Tonolini M, Ierardi AM, Patella F, Carrafiello G. Early cross-sectional imaging following open and laparoscopic cholecystectomy: a primer for radiologists. Insights Imaging. 2018;9:925-941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Elsheikh M, Hablus MA. Two-year experience with selective intraoperative cholangiography in laparoscopic cholecystectomy. Egypt J Surg. 2019;38:272-276. [DOI] [Full Text] |
| 15. | Abou El-Ella KM, Mohamed ON, El-Sebayel MI, Al-Semayer SA, Al Mofleh IA. Management of postlaparoscopic cholecystectomy major bile duct injury: comparison of MRCP with conventional methods. Saudi J Gastroenterol. 2004;10:8-15. [PubMed] |
| 16. | Salama AF, Abd Ellatif ME, Abd Elaziz H, Magdy A, Rizk H, Basheer M, Jamal W, Dawoud I, El Nakeeb A. Preliminary experience with laparoscopic common bile duct exploration. BMC Surg. 2017;17:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Mischinger HJ, Bernhard G, Cerwenka H, Hauser H, Werkgartner G, Kornprat P, Shabrawi AE, Bacher H. Management of bile duct injury after laparoscopic cholecystectomy. Eur Surg. 2011;43:342-350. [DOI] [Full Text] |
| 18. | Renz BW, Bösch F, Angele MK. Bile Duct Injury after Cholecystectomy: Surgical Therapy. Visc Med. 2017;33:184-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Pesce A, Palmucci S, La Greca G, Puleo S. Iatrogenic bile duct injury: impact and management challenges. Clin Exp Gastroenterol. 2019;12:121-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 20. | Karvonen J, Gullichsen R, Laine S, Salminen P, Grönroos JM. Bile duct injuries during laparoscopic cholecystectomy: primary and long-term results from a single institution. Surg Endosc. 2007;21:1069-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Mavrogiannis C, Liatsos C, Papanikolaou IS, Karagiannis S, Galanis P, Romanos A. Biliary stenting alone vs biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: a prospective randomized study. Eur J Gastroenterol Hepatol. 2006;18:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Zerem E, Omerović S. Minimally invasive management of biliary complications after laparoscopic cholecystectomy. Eur J Intern Med. 2009;20:686-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Coté GA, Ansstas M, Shah S, Keswani RN, Alkade S, Jonnalagadda SS, Edmundowicz SA, Azar RR. Findings at endoscopic retrograde cholangiopancreatography after endoscopic treatment of postcholecystectomy bile leaks. Surg Endosc. 2010;24:1752-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Aksoz K, Unsal B, Yoruk G, Buyrac Z, Haciyanli M, Akpinar Z, Alper E. Endoscopic sphincterotomy alone in the management of low-grade biliary leaks due to cholecystectomy. Dig Endosc. 2009;21:158-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Kaffes AJ, Hourigan L, De Luca N, Byth K, Williams SJ, Bourke MJ. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc. 2005;61:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 126] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 26. | Tringali A, Reddy DN, Ponchon T, Neuhaus H, Lladó FG, Navarrete C, Bruno MJ, Kortan PP, Lakhtakia S, Peetermans J, Rousseau M, Carr-Locke D, Devière J, Costamagna G; Benign Biliary Stenoses Working Group. Treatment of post-cholecystectomy biliary strictures with fully-covered self-expanding metal stents - results after 5 years of follow-up. BMC Gastroenterol. 2019;19:214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Csendes A, Navarrete C, Burdiles P, Yarmuch J. Treatment of common bile duct injuries during laparoscopic cholecystectomy: endoscopic and surgical management. World J Surg. 2001;25:1346-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Zhu Y, Hickey R. The Role of the Interventional Radiologist in Bile Leak Diagnosis and Management. Semin Intervent Radiol. 2021;38:309-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Thompson CM, Saad NE, Quazi RR, Darcy MD, Picus DD, Menias CO. Management of iatrogenic bile duct injuries: role of the interventional radiologist. Radiographics. 2013;33:117-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 30. | Lucatelli P, Corradini SG, Corona M, Corradini LG, Cirelli C, Saba L, Poli E, Fanelli F, Wang H, Bezzi M, Catalano C. Risk Factors for Immediate and Delayed-Onset Fever After Percutaneous Transhepatic Biliary Drainage. Cardiovasc Intervent Radiol. 2016;39:746-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Nasif HH, Shalaby MH, Abdelmaksoud MHK, Elsakka AS. Role of Interventional Radiology in the Management of Postoperative Biliary Complications. Egyt J Hosp Med. 2018;72:5153-5160. |