Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2191
Peer-review started: May 27, 2023
First decision: June 14, 2023
Revised: June 23, 2023
Accepted: August 17, 2023
Article in press: August 17, 2023
Published online: October 27, 2023
Processing time: 152 Days and 18.7 Hours
Rehabilitation of elderly patients with a high body mass index (BMI) after cholecystectomy carries risks and requires the adoption of effective perioperative management strategies. The enhanced recovery after surgery (ERAS) protocol is a comprehensive treatment approach that facilitates early patient recovery and reduces postoperative complications.
To compare the effectiveness of traditional perioperative management methods with the ERAS protocol in elderly patients with gallbladder stones and a high BMI.
This retrospective cohort study examined data from 198 elderly patients with a high BMI who underwent cholecystectomy at the Shanghai Fourth People's Hospital from August 2019 to August 2022. Among them, 99 patients were mana
The comparison results between the two groups of patients in terms of age, sex, BMI, underlying diseases, surgical type, and preoperative hospital stay showed no statistically significant differences. However, the ERAS group had a significantly shorter preoperative fasting time than the non-ERAS group (4.0 ± 0.9 h vs 7.6 ± 0.9 h). Regarding intraoperative indicators, there were no significant differences between the two groups of patients. However, in terms of postoperative recovery, the ERAS protocol group exhibited significant advantages over the non-ERAS group, including a shorter hospital stay, lower postoperative pain scores and postoperative hunger scores, and higher satisfaction levels. The readmission rate was lower in the ERAS protocol group than in the non-ERAS group (3.0% vs 8.1%), although the difference was not significant. Furthermore, there were significant differences between the two groups in terms of postoperative nausea and vomiting severity, postoperative abdominal distention at 24 h, and daily life ability scores.
The findings of this study demonstrate that the ERAS protocol confers significant advantages in postoperative outcomes following cholecystectomy, including reduced readmission rates, decreased postoperative nausea and vomiting, alleviated abdominal distension, and enhanced functional capacity. While the protocol may not exhibit significant improvement in early postoperative symptoms, it does exhibit advantages in long-term postoperative symptoms and recovery. These findings underscore the importance of implementing the ERAS protocol in the postoperative management of cholecystectomy patients, as it contributes to improving patients' recovery and quality of life while reducing health care resource utilization.
Core Tip: This study compared the effectiveness of the enhanced recovery after surgery (ERAS) protocol with traditional perioperative management methods in elderly patients with gallbladder stones and a high body mass index. The results showed that the ERAS protocol demonstrated significant advantages in postoperative outcomes, including reduced readmission rates, improved postoperative nausea and vomiting, alleviated abdominal distension, and enhanced daily living ability. However, the protocol may not exhibit significant improvement in early postoperative symptoms but demonstrates advantages in long-term symptoms and recovery. Implementing the ERAS protocol in the postoperative management of cholecystectomy patients can contribute to improved recovery and quality of life while reducing health care resource utilization.
- Citation: Gu YX, Wang XY, Chen Y, Shao JX, Ni SX, Zhang XM, Shao SY, Zhang Y, Hu WJ, Ma YY, Liu MY, Yu H. Optimizing surgical outcomes for elderly gallstone patients with a high body mass index using enhanced recovery after surgery protocol. World J Gastrointest Surg 2023; 15(10): 2191-2200
- URL: https://www.wjgnet.com/1948-9366/full/v15/i10/2191.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i10.2191
Due to the increasingly ageing population, there are a growing number of patients with a high body mass index (BMI) and gallstones, which are two factors that pose risks for surgical treatment. To mitigate these risks, enhanced recovery after surgery (ERAS) has been widely implemented in clinical practice for gallbladder surgery. The ERAS protocol emphasizes comprehensive perioperative management, including preoperative preparation, intraoperative management, and postoperative recovery, thus aiming to reduce surgical risks, shorten hospital stays, and improve rehabilitation outcomes[1-4]. Although the effectiveness of the ERAS protocol has been demonstrated in young and healthy patients, its application and effectiveness in elderly patients with a high BMI and gallstones warrant further investigation.
Patients with a high BMI have more prominent surgical risks, such as longer surgical duration, larger incisions, greater blood loss, and prolonged postoperative hospital stays[5,6]. Therefore, the implementation of an ERAS protocol to optimize the surgical treatment of elderly patients with gallbladder stones and a high BMI holds significant clinical significance.
Previous studies have demonstrated the widespread utilization and effectiveness of ERAS protocols in the management of gallbladder surgical procedures[7,8]. However, the majority of these investigations have predominantly focused on young and healthy patient populations, and there is a lack of specialized research concerning elderly patients with a high BMI and gallstone pathology[9,10]. In this retrospective analysis, we collected pertinent clinical data from elderly patients with a high BMI who underwent cholecystectomy at the Fourth People's Hospital of Shanghai from August 2019 to August 2022. By comparing the surgical outcomes between the ERAS protocol group and the conventional non-ERAS protocol group, we aimed to provide a comprehensive understanding of the application of ERAS protocols in the surgical treatment of elderly patients with a high BMI and gallstone pathology.
This study employed a retrospective research design and included a total of 198 elderly patients with a high BMI who underwent cholecystectomy at the Fourth People's Hospital of Shanghai from August 2019 to August 2022. Among them, 99 patients were managed with the traditional non-ERAS protocol for perioperative care, while the remaining 99 patients were managed with the ERAS protocol. We specifically chose elderly patients with a high BMI because this population carries certain risks related to postoperative recovery and is more sensitive to factors related to perioperative management. This study obtained approval from the institutional ethics committee and adhered to relevant ethical principles and privacy protection measures (No. 2019047). All participating patients provided informed consent and agreed to the use of their data for research analysis.
The inclusion criteria were as follows: (1) Nonurgent patients scheduled for gallbladder removal; (2) age ≥ 65 years, regardless of sex; (3) no contraindications for biliary surgery or general anaesthesia; (4) absence of significant gallbladder enlargement or gallbladder discharge on ultrasound or magnetic resonance imaging; (5) no concomitant choledocholithiasis or other conditions requiring surgical intervention, no acute or chronic gastrointestinal obstruction, and no symptoms of delayed gastric emptying; (6) willingness of the patient to undergo gallbladder removal; (7) absence of significant mental or psychological disorders, hearing impairment, or language barriers, ability to communicate normally during treatment, possessing independent legal capacity, and ability to express oneself clearly; and (8) agreement from the patient to receive ERAS treatment.
Elderly patients with a high BMI typically refer to patients aged 65 years and above with a BMI equal to or greater than 28 kg/m². Baseline comorbidities refer to preexisting or existing chronic conditions such as hypertension and diabetes. The Hunger score is an indicator used to assess the degree of hunger among patients during the perioperative period. It is generally rated on a scale of 0-2, where 0 indicates no hunger at all, 1 indicates mild hunger that is tolerable, and 2 indicates intolerable hunger or hypoglycaemia requiring intravenous fluid therapy[11]. The postoperative nausea and vomiting (PONV) score is a quantification tool used to assess the severity of PONV[12]. It is scored as follows: 0 points indicate no nausea or vomiting; 1 point indicates mild nausea or vomiting, with patients reporting mild nausea [Visual Analogue Scale (VAS) score < 3 cm] or one episode of vomiting or short-duration (less than 10 min) persistent nausea that resolves without antiemetic medication; and 2 points indicate moderate nausea or vomiting, with patients experiencing 1-2 episodes of vomiting or nausea with a VAS score > 3 cm due to endogenous stimuli, requiring one dose of antiemetic medication for relief. The abdominal distension score is an indicator used to assess the sensation of abdominal bloating in patients and is often used in postoperative or other relevant conditions[13,14]. It is typically described using a scoring system ranging from 0-2 to indicate the degree of abdominal distension. A score of 0 points indicates no abdominal distension, 1 point indicates mild abdominal distension that is tolerable, and 2 points indicate intolerable abdominal distension. The Barthel Index is a scale used to assess activities of daily living[15]. The VAS is also a commonly used pain assessment method, and in this study, the VAS was used to evaluate patients' pain levels. The satisfaction score is a method used to assess patients' satisfaction with medical care or treatment processes[16]. It is typically represented using a numerical range to indicate the degree of satisfaction, with 100 points representing the highest level of satisfaction.
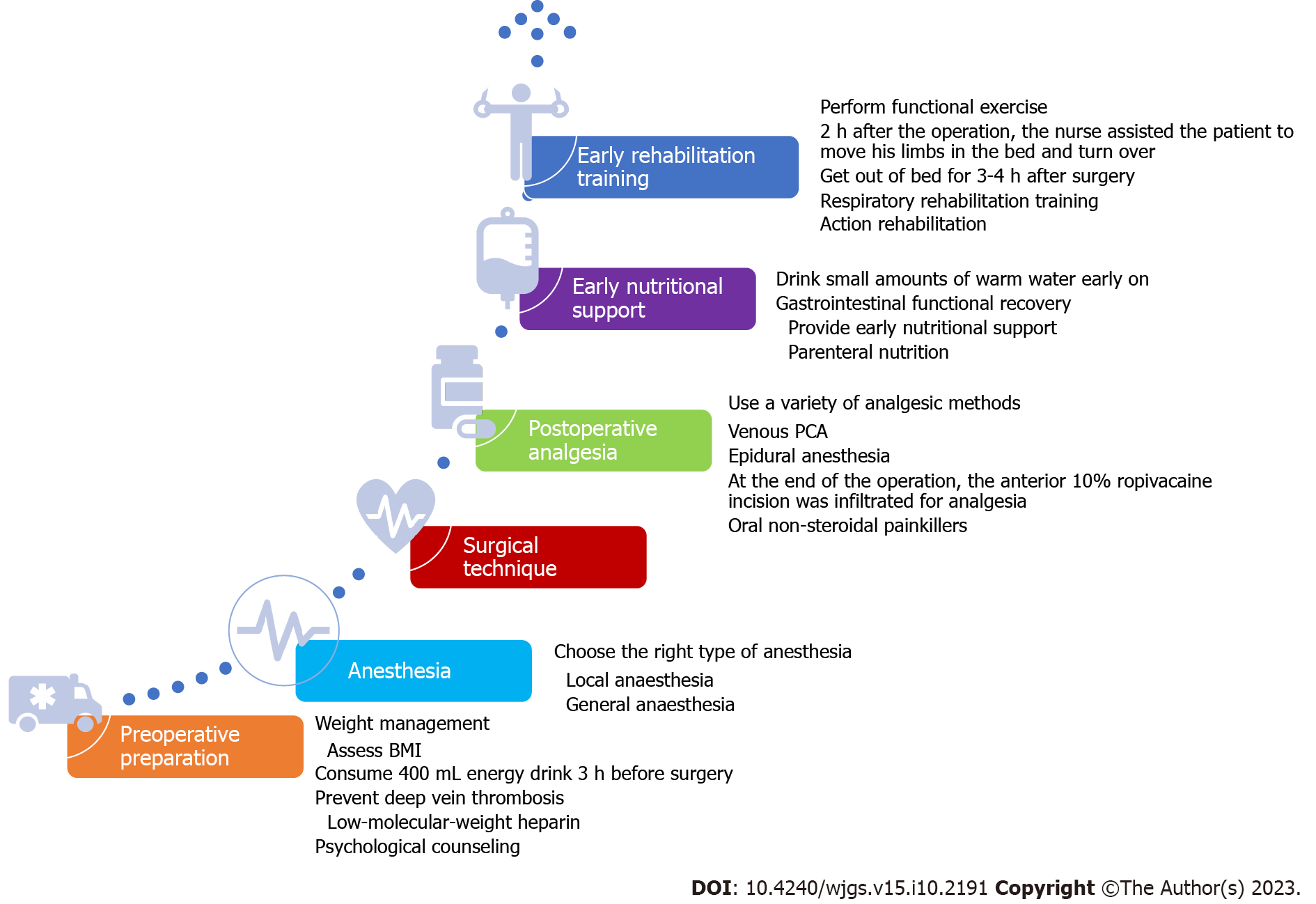
The ERAS protocol is a comprehensive treatment approach aimed at promoting early recovery and reducing postoperative complications through strategies such as minimally invasive surgery, thorough preoperative preparation, early postoperative nutritional support, and early rehabilitation training. Specifically, the ERAS protocol encompasses various aspects, including preoperative preparation, anaesthesia, surgical techniques, postoperative pain management, and early nutritional support, among others, providing patients with high-quality perioperative care in a multidimensional manner. The specific protocol flow is detailed in Figure 1.
We collected relevant data on preoperative, intraoperative, and postoperative indicators of the patients by reviewing their medical records, surgical records, and follow-up records. Preoperative indicators included age, sex, underlying medical conditions, BMI, and preoperative fasting score at 1 h. Intraoperative indicators included surgical duration, incision length, and blood loss. Postoperative indicators included the incidence of complications, length of hospital stay, pain score at 24 h, fasting score at 6 h postoperatively, satisfaction level, readmission rate, degree of nausea and vomiting at 6 and 24 h postoperatively, degree of abdominal distension at 6 and 24 h postoperatively, and daily living ability score at 24 h postoperatively. These indicators reflected the surgical risk and postoperative recovery of the patients.
Data analyses were performed using SPSS 23.0 software (IBM, 2015, United States). Normality tests were conducted for all continuous variables in this study. Normally distributed variables are reported as the mean ± SD and were compared using independent sample t tests. Nonnormally distributed variables are reported as medians (25th-75th percentile). Categorical data were analysed using Pearson's chi-square test. A P-value of < 0.05 was considered statistically significant.
A total of 198 elderly patients with a high BMI were included in this study, with 99 patients in the traditional non-ERAS protocol group and another 99 patients in the ERAS protocol group. The basic characteristics of the two groups, including age, sex, BMI, preoperative hunger score, and other variables, are presented in Table 1. There were no significant differences between the two groups in terms of age, sex, BMI, underlying diseases, surgical type, and preoperative hospital stay (P > 0.05). However, there was a significant difference in preoperative fasting time between the two groups, with an average fasting time of 4.0 ± 0.9 h in the ERAS group compared to 7.6 ± 0.9 h in the non-ERAS group (P < 0.001).
| Characteristic | ERAS group (n = 99) | Non-ERAS group (n = 99) | P value |
| Age (yr), mean ± SD | 69.5 ± 3.6 | 69.4 ± 3.0 | 0.746 |
| Gender, male, n (%) | 49 (49.5) | 46 (46.5) | 0.670 |
| BMI (kg/m²), mean ± SD | 29.3 ± 1.2 | 29.1 ± 1.4 | 0.276 |
| Underlying diseases, n (%) | 20 (20.2) | 25 (25.3) | 0.386 |
| Surgical procedure (laparoscopic/open) | 85/14 | 83/16 | 0.692 |
| Preoperative hunger score, n (%) | 0.052 | ||
| 0 | 41 (41.4) | 25 (25.3) | |
| 1 | 49 (49.5) | 61 (61.6) | |
| 2 | 9 (9.1) | 13 (13.1) | |
| Preoperative hospitalization time (d) | 2.4 ± 0.9 | 2.3 ± 0.8 | 0.223 |
| Preoperative fasting time (h) | 4.0 ± 0.9 | 7.6 ± 0.9 | < 0.001 |
The comparison of surgical process variables, including operative time, incision length, blood loss, number of drainage tubes, extubation time, postoperative complications, and pain score at 6 h postoperatively, showed no statistically significant differences between the two groups. However, the ERAS protocol group demonstrated significantly better postoperative recovery than the non-ERAS protocol group. The length of hospital stay (4.62 ± 1.01 vs 5.51 ± 1.15), pain score at 24 h postoperatively (3.43 ± 1.19 vs 4.43 ± 1.21), hunger score, and satisfaction at 6 h postoperatively (98.42 ± 1.13 vs 93.72 ± 2.76) were all significantly better in the ERAS protocol group (Table 2).
| Characteristic | ERAS group (n = 99) | Non-ERAS group (n = 99) | P value |
| Surgical duration (min) | 81.27 ± 23.17 | 82.97 ± 24.13 | 0.614 |
| The incision length (cm) | 10.33 ± 2.84 | 10.46 ± 2.81 | 0.744 |
| Blood loss (mL) | 93.52 ± 28.64 | 93.68 ± 24.39 | 0.966 |
| No. of drainage tubes, n (%) | 0.754 | ||
| 0 | 37 (37.4) | 32 (32.3) | |
| 1 | 30 (30.3) | 33 (33.3) | |
| 2 | 32 (32.3) | 34 (34.3) | |
| Extubation time (h) | 39.72 ± 18.00 | 40.96 ± 18.61 | 0.634 |
| Postoperative complication rate, n (%) | 5 (5.1) | 10 (13.1) | 0.048 |
| Length of hospital stay (d) | 4.62 ± 1.01 | 5.51 ± 1.15 | < 0.001 |
| Postoperative pain score at 6 h | 1.96 ± 1.11 | 2.21 ± 0.82 | 0.07 |
| Postoperative pain score at 24 h | 3.43 ± 1.19 | 4.43 ± 1.21 | < 0.001 |
| Postoperative 6-h hunger score | < 0.001 | ||
| 0 | 45 | 32 | |
| 1 | 51 | 35 | |
| 2 | 3 | 32 | |
| Satisfaction (%) | 98.42 ± 1.13 | 93.72 ± 2.76 | < 0.001 |
The aim of this study was to compare the differences in hospital readmission rates and postoperative nausea, vomiting, bloating, and activities of daily living scores between the ERAS group and the non-ERAS group. The results showed that the hospital readmission rate was lower in the ERAS protocol group than in the non-ERAS protocol group (3.0% vs 8.1%, P > 0.05), but the difference did not reach statistical significance. Significant differences were observed between the two groups in terms of PONV at 24 h, bloating at 24 h, and activities of daily living scores. However, there was no statistically significant difference between the two groups in terms of PONV at 6 h and bloating (Table 3). Taking all the results into consideration, the ERAS protocol group demonstrated a significant advantage in terms of rehospitalization rate, with a reduced rehospitalization rate compared to the non-ERAS protocol group. These findings suggest that the ERAS protocol may effectively reduce the rehospitalization rate in patients undergoing cholecystectomy. There may not be significant improvements in early postoperative symptoms, but the protocol may have advantages in terms of long-term symptoms and recovery. These findings emphasize the importance of the ERAS protocol in postcholecystectomy care, as it helps improve patients' recovery and quality of life while reducing health care resource utilization. In addition, rehospitalization rates were not statistically associated with surgical complications or patient comorbidities.
| Characteristic | ERAS group (n = 99) | Non-ERAS group (n = 99) | P value |
| Rehospitalization rate | 3 (3.0) | 8 (8.1) | 0.12 |
| PONV at 6 h | 0.322 | ||
| 0 | 43 (43.4) | 49 (49.5) | |
| 1 | 40 (40.4) | 30 (30.3) | |
| 2 | 16 (16.2) | 20 (20.2) | |
| PONV at 24 h | 0.005 | ||
| 0 | 39 (39.4) | 32 (32.3) | |
| 1 | 50 (50.5) | 39 (39.4) | |
| 2 | 10 (10.1) | 28 (28.3) | |
| Postoperative bloating score at 6 h | 0.178 | ||
| 0 | 40 (40.4) | 53 (53.5) | |
| 1 | 52 (52.5) | 41 (41.4) | |
| 2 | 7 (7.1) | 5 (5.1) | |
| Postoperative bloating score at 24 h | 0.006 | ||
| 0 | 47 (47.5) | 34 (34.3) | |
| 1 | 38 (38.4) | 32 (32.3) | |
| 2 | 14 (14.1) | 33 (33.4) | |
| ADL score | 85.75 ± 5.83 | 83.87 ± 6.72 | 0.037 |
In recent years, with the increasing population of elderly individuals and patients with a higher BMI, perioperative management for this specific population has become particularly important[17-19]. The aim of this study was to compare the differences in surgical outcomes between traditional perioperative management methods and the ERAS protocol in elderly patients with a high BMI and gallbladder stones. Through a retrospective study design, we included a total of 199 elderly patients with a high BMI for comparative analysis.
Our research findings indicate that there were no significant differences between the two groups in terms of age, sex, BMI, underlying diseases, surgical type, and preoperative hospital stay, indicating comparability between the two groups at baseline. However, the ERAS protocol group had a significantly shorter preoperative fasting time than the non-ERAS group, which aligns with the characteristic of the ERAS protocol to reduce unnecessary fasting time and alleviate preoperative hunger sensation in patients[20-22].
In terms of intraoperative indicators, there were no significant differences between the two patient groups, indicating that the ERAS protocol did not have a significant impact on the surgical procedure itself. However, in terms of postoperative recovery, the ERAS protocol group showed significant advantages over the non-ERAS protocol group. Patients in the ERAS protocol group exhibited superior outcomes in terms of hospital stay duration, postoperative pain scores, postoperative hunger scores, and satisfaction levels compared to patients in the non-ERAS protocol group. These findings suggest that the ERAS protocol can facilitate early patient recovery, alleviate postoperative pain and hunger, and improve patient satisfaction[10,23-26].
The readmission rate is one of the important indicators for evaluating surgical treatment outcomes. Our study found that the readmission rate in the ERAS protocol group was lower than that in the non-ERAS protocol group. Although there was no significant difference, this result still demonstrates the potential advantage of the ERAS protocol in reducing readmission rates. Additionally, significant differences were observed between the two groups in terms of PONV, bloating, and daily living ability scores. This indicates the clear advantages of the ERAS protocol in reducing postoperative complications and promoting patient recovery[19,27,28].
Although the ERAS group showed a lower readmission rate, the small sample size might lead to a limited ability to observe significant differences in the statistical analysis. Second, while the ERAS group received a series of optimized postoperative care measures, the non-ERAS group might have also received certain effective nursing interventions, resulting in a lack of significant differences in readmission rates. Last, there might be potential confounding factors that influence readmission rates in addition to ERAS interventions, such as patients' underlying diseases, postoperative rehabilitation support, and adherence to medical instructions. These factors might differ between the two groups, affecting readmission rates without being statistically significant.
Based on the aforementioned results, this study demonstrates significant advantages of implementing the ERAS protocol following cholecystectomy. The application of the ERAS protocol is associated with a reduction in readmission rates, improvement in postoperative nausea, vomiting, and abdominal distention, and enhancement of patients' daily life functionality. While there may not be a significant improvement in early postoperative symptoms, it exhibits advantages in terms of improvement of long-term symptoms and recovery[29-31]. These findings emphasize the importance of the ERAS protocol in postcholecystectomy care, as it contributes to the improvement of patients' rehabilitation and quality of life while reducing the utilization of health care resources[28].
Although this study has yielded some meaningful results, there are still some limitations that need to be acknowledged. First, the study design employed in this research is retrospective, which might have introduced selection bias and information bias. Further prospective randomized controlled trials would provide stronger evidence. Second, this study is limited to the experience of a single medical centre, and the results may not be widely applicable. Multicentre studies with larger sample sizes would better assess the effectiveness of the ERAS protocol in elderly patients with a high BMI and gallstones. Additionally, this study did not include long-term follow-up data, thus limiting the evaluation of the long-term effects and survival rates associated with the ERAS protocol.
In future studies, we recommend incorporating a broader range of clinical indicators and postoperative follow-up data to further evaluate the application of the ERAS protocol in the surgical treatment of elderly patients with gallbladder stones and a high BMI. Additionally, comparative research with other treatment approaches should be considered to further substantiate the advantages and scope of the ERAS protocol.
The findings of this study demonstrate that the adoption of the ERAS protocol in elderly patients with a high BMI who are undergoing cholecystectomy provides significant advantages over traditional perioperative management methods. The ERAS protocol is associated with reduced readmission rates, improved PONV symptoms, alleviated abdominal distension, and enhanced functional capacity in these patients. Although there may not be significant improvement in early postoperative symptoms, the ERAS protocol exhibits advantages in terms of long-term postoperative symptoms and recovery. These findings underscore the importance of implementing the ERAS protocol in the postoperative management of cholecystectomy patients, as it contributes to improving patients' recovery and quality of life while reducing health care resource utilization.
The rehabilitation of elderly patients with a high body mass index (BMI) after cholecystectomy poses risks and requires effective perioperative management strategies. The enhanced recovery after surgery (ERAS) protocol is a comprehensive treatment approach that promotes early patient recovery and reduces postoperative complications.
The aim of this study was to compare the effectiveness of traditional perioperative management methods with the ERAS protocol in elderly patients with gallbladder stones and a high BMI.
The study aimed to assess and compare the outcomes of elderly patients with a high BMI undergoing cholecystectomy using the ERAS protocol and traditional perioperative care, focusing on various indicators, including fasting time, surgical outcomes, hospital stay, pain scores, satisfaction levels, readmission rates, postoperative symptoms, and functional capacity.
A retrospective cohort study design was employed, involving 198 elderly patients with a high BMI who underwent cholecystectomy. The patients were divided into two groups: One managed using traditional perioperative care (non-ERAS protocol) and the other managed using the ERAS protocol. Data on relevant indicators were collected preoperatively, intraoperatively, and postoperatively, and a comparison of surgical outcomes was conducted.
The comparison results showed no statistically significant differences between the two groups in terms of age, sex, BMI, underlying diseases, surgical type, and preoperative hospital stay. However, the ERAS group had a significantly shorter preoperative fasting time. In terms of postoperative recovery, the ERAS protocol group exhibited significant advantages over the non-ERAS group, including shorter hospital stay, lower postoperative pain scores, hunger scores, and higher satisfaction levels. The readmission rate was also significantly lower in the ERAS protocol group. Furthermore, there were significant differences in postoperative nausea and vomiting (PONV) severity, postoperative abdominal distention at 24 h, and daily life ability scores between the two groups.
The study findings demonstrate that the ERAS protocol provides significant benefits in postoperative outcomes following cholecystectomy. It reduces readmission rates, improves PONV, alleviates abdominal distension, and enhances patients' functional capacity. Although the ERAS protocol may not show significant improvement in early postoperative symptoms, it exhibits advantages in long-term postoperative symptoms and recovery. Implementing the ERAS protocol in postoperative management is crucial for improving patients' recovery and quality of life while reducing health care resource utilization.
The results highlight the importance of incorporating the ERAS protocol in the postoperative management of cholecystectomy patients. Further research can explore the long-term effects of the ERAS protocol on patient outcomes and assess its applicability in other surgical procedures or patient populations.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): E
P-Reviewer: Gad EH, Egypt; Hori T, Japan; Ji ZL, China; Kim BS, South Korea; Kumar M, India S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Yin M, Yan Y, Fan Z, Fang N, Wan H, Mo W, Wu X. The efficacy of Enhanced Recovery after Surgery (ERAS) for elderly patients with intertrochanteric fractures who received surgery: study protocol for a randomized, blinded, controlled trial. J Orthop Surg Res. 2020;15:91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Zhu W, Yan Y, Sun Y, Fan Z, Fang N, Zhang Y, Yin M, Wan H, Mo W, Lu W, Wu X. Implementation of Enhanced Recovery After Surgery (ERAS) protocol for elderly patients receiving surgery for intertrochanteric fracture: a propensity score-matched analysis. J Orthop Surg Res. 2021;16:469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Noba L, Rodgers S, Chandler C, Balfour A, Hariharan D, Yip VS. Enhanced Recovery After Surgery (ERAS) Reduces Hospital Costs and Improve Clinical Outcomes in Liver Surgery: a Systematic Review and Meta-Analysis. J Gastrointest Surg. 2020;24:918-932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 157] [Cited by in RCA: 135] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 4. | Puccetti F, Klevebro F, Kuppusamy M, Han S, Fagley RE, Low DE, Hubka M. Analysis of Compliance with Enhanced Recovery After Surgery (ERAS) Protocol for Esophagectomy. World J Surg. 2022;46:2839-2847. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Deiner S, Fleisher LA, Leung JM, Peden C, Miller T, Neuman MD; ASA Committee on Geriatric Anesthesia and the ASA Perioperative Brain Health Initiative. Adherence to recommended practices for perioperative anesthesia care for older adults among US anesthesiologists: results from the ASA Committee on Geriatric Anesthesia-Perioperative Brain Health Initiative ASA member survey. Perioper Med (Lond). 2020;9:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Raglan O, MacIntyre DA, Mitra A, Lee YS, Smith A, Assi N, Nautiyal J, Purkayastha S, Gunter MJ, Gabra H, Marchesi JR, Bennett PR, Kyrgiou M. The association between obesity and weight loss after bariatric surgery on the vaginal microbiota. Microbiome. 2021;9:124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Kauffman JD, Nguyen ATH, Litz CN, Farach SM, DeRosa JC, Gonzalez R, Amankwah EK, Danielson PD, Chandler NM. Laparoscopic-guided versus transincisional rectus sheath block for pediatric single-incision laparoscopic cholecystectomy: A randomized controlled trial. J Pediatr Surg. 2020;55:1436-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Zhang Y, Wang YP, Wang HT, Xu YC, Lv HM, Yu Y, Wang P, Pei XD, Zhao JW, Nan ZH, Yang JJ. Ultrasound-guided quadratus lumborum block provided more effective analgesia for children undergoing lower abdominal laparoscopic surgery: a randomized clinical trial. Surg Endosc. 2022;36:9046-9053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Yu J, Lin X, Chen H. Study on the Application Effect of Fast Track Surgery Care Combined With Continuous Care After Discharge in Patients With Laparoscopic Cholecystectomy. Front Surg. 2022;9:848234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Li S, Bai J, Wei W, Liu X, Shen Y. Effect of systematic nursing on the stress response and recovery of gastrointestinal function in patients undergoing laparoscopic cholecystectomy. Am J Transl Res. 2021;13:9647-9654. [PubMed] |
| 11. | Weiji Q, Shitong L, Yu L, Tianfang H, Ning K, Lina Z. The predictive value of hunger score on gastric evacuation after oral intake of carbohydrate solution. BMC Anesthesiol. 2018;18:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Balyan R, Kumar S, Lalitha K, Aneja S, George J. A Randomised Study To Compare Palonosetron With Ondansetron for Prophylaxis of Postoperative Nausea and Vomiting (PONV) Following Laparoscopic Gynecological Surgeries. Cureus. 2022;14:e23615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Barba E, Sánchez B, Burri E, Accarino A, Monclus E, Navazo I, Guarner F, Margolles A, Azpiroz F. Abdominal distension after eating lettuce: The role of intestinal gas evaluated in vitro and by abdominal CT imaging. Neurogastroenterol Motil. 2019;31:e13703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Barba E, Burri E, Quiroga S, Accarino A, Azpiroz F. Visible abdominal distension in functional gut disorders: Objective evaluation. Neurogastroenterol Motil. 2023;35:e14466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Okamoto M, Kito M, Yoshimura Y, Aoki K, Suzuki S, Tanaka A, Takazawa A, Yoshida K, Ido Y, Ishida T, Kawasaki K, Kato H. Using the Barthel Index to Assess Activities of Daily Living after Musculoskeletal Tumour Surgery: A Single-centre Observational Study. Prog Rehabil Med. 2019;4:20190010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | A Rahim AI, Ibrahim MI, Musa KI, Chua SL. Facebook Reviews as a Supplemental Tool for Hospital Patient Satisfaction and Its Relationship with Hospital Accreditation in Malaysia. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Cua S, Humeidan M, Beal EW, Brethauer S, Pervo V, Papio J, Husain S, Moffatt-Bruce S. The Effect of an Enhanced Recovery Protocol on Colorectal Surgery Patients With Diabetes. J Surg Res. 2021;257:153-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Talutis SD, Lee SY, Cheng D, Rosenkranz P, Alexanian SM, McAneny D. The impact of preoperative carbohydrate loading on patients with type II diabetes in an enhanced recovery after surgery protocol. Am J Surg. 2020;220:999-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Alimena S, Falzone M, Feltmate CM, Prescott K, Contrino Slattery L, Elias K. Perioperative glycemic measures among non-fasting gynecologic oncology patients receiving carbohydrate loading in an enhanced recovery after surgery (ERAS) protocol. Int J Gynecol Cancer. 2020;30:533-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Gao B, Chen J, Liu Y, Hu S, Wang R, Peng F, Fang C, Gan Y, Su S, Han Y, Yang X, Li B. Efficacy and safety of enhanced recovery after surgery protocol on minimally invasive bariatric surgery: a meta-analysis. Int J Surg. 2023;109:1015-1028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 21. | Stangl-Kremser J, Lambertini L, Di Maida F, Martinez-Fundichely A, Ferro M, Pradere B, Soria F, Albisinni S, Wu Z, Del Giudice F, Cacciamani GE, Valerio M, Briganti A, Rouprêt M, Shariat SF, Lee C, Minervini A, Moschini M, Mari A; European Association of Urology-Young Academic Urologists Urothelial Carcinoma Working Group. Enhancing Recovery After Major Bladder Cancer Surgery: Comprehensive Review and Assessment of Application of the Enhanced Recovery After Surgery Guidelines. Eur Urol Focus. 2022;8:1622-1626. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Cavallaro P, Bordeianou L. Implementation of an ERAS Pathway in Colorectal Surgery. Clin Colon Rectal Surg. 2019;32:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 103] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 23. | Joliat GR, Kobayashi K, Hasegawa K, Thomson JE, Padbury R, Scott M, Brustia R, Scatton O, Tran Cao HS, Vauthey JN, Dincler S, Clavien PA, Wigmore SJ, Demartines N, Melloul E. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations 2022. World J Surg. 2023;47:11-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 100] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 24. | Macías-Valle A, Rodríguez-López C, González-Senac NM, Mayordomo-Cava J, Vidán MT, Cruz-Arnés ML, Jiménez-Gómez LM, Dujovne-Lindenbaum P, Pérez-Menéndez ME, Ortiz-Alonso J, Valenzuela PL, Rodríguez-Romo G, Serra-Rexach JA. Exercise effects on functional capacity and quality of life in older patients with colorectal cancer: study protocol for the ECOOL randomized controlled trial. BMC Geriatr. 2023;23:314. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, de Boer HD, Urman RD, Chang GJ, Fichera A, Kessler H, Grass F, Whang EE, Fawcett WJ, Carli F, Lobo DN, Rollins KE, Balfour A, Baldini G, Riedel B, Ljungqvist O. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS(®)) Society Recommendations: 2018. World J Surg. 2019;43:659-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1071] [Cited by in RCA: 1218] [Article Influence: 203.0] [Reference Citation Analysis (0)] |
| 26. | Palomba G, Dinuzzi VP, Capuano M, Anoldo P, Milone M, De Palma GD, Aprea G. Robotic versus laparoscopic colorectal surgery in elderly patients in terms of recovery time: a monocentric experience. J Robot Surg. 2022;16:981-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Liu JY, Perez SD, Balch GG, Sullivan PS, Srinivasan JK, Staley CA, Sweeney J, Sharma J, Shaffer VO. Elderly Patients Benefit From Enhanced Recovery Protocols After Colorectal Surgery. J Surg Res. 2021;266:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Gao Y, Huang J, Zheng Y, Han J. Effect of comfort nursing on postoperative quality of life, negative emotions and nursing satisfaction in patients undergoing laparoscopic surgery. Am J Transl Res. 2021;13:13825-13834. [PubMed] |
| 29. | Hu QL, Liu JY, Hobson DB, Cohen ME, Hall BL, Wick EC, Ko CY. Best Practices in Data Use for Achieving Successful Implementation of Enhanced Recovery Pathway. J Am Coll Surg. 2019;229:626-632.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Zhang M, Wang X, Chen X, Song Z, Wang Y, Zhou Y, Zhang D. A Scientometric Analysis and Visualization Discovery of Enhanced Recovery After Surgery. Front Surg. 2022;9:894083. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 31. | Bongers BC, Dejong CHC, den Dulk M. Enhanced recovery after surgery programmes in older patients undergoing hepatopancreatobiliary surgery: what benefits might prehabilitation have? Eur J Surg Oncol. 2021;47:551-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (1)] |