Published online Jun 27, 2021. doi: 10.4240/wjgs.v13.i6.574
Peer-review started: January 10, 2021
First decision: February 14, 2021
Revised: February 26, 2021
Accepted: June 1, 2021
Article in press: June 1, 2021
Published online: June 27, 2021
Processing time: 158 Days and 20.4 Hours
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is responsible for the ongoing pandemic of coronavirus disease 2019 (COVID-19), and has caused more than 80 million infections and 1.7 million deaths worldwide. Although it is primarily a respiratory virus, SARS-CoV-2 also has extra-pulmonary effects. Pancreatic injury and cases of acute pancreatitis (AP) have been recognized and attributed to SARS-CoV-2, but the mechanisms of pancreatic injury are still a subject of debate. There is also controversy on whether SARS-CoV-2 can cause AP or if it is an epiphenomenon.
To review and to explore the relationship between SARS-CoV-2 infection and AP, and to provide an overview of the existing literature on possible mechanisms of SARS-CoV-2-induced pancreatic lesion.
A systematic review was conducted in accordance with PRISMA guidelines for papers on SARS-CoV-2 infection and AP. A narrative review on possible mechanisms of SARS-CoV-2-induced pancreatic lesion was also performed.
A literature review revealed a growing body of evidence on SARS-CoV-2-induced pancreatic lesions including the mechanisms of direct virus-mediated injury, systemic inflammatory response and circulating pro-inflammatory interleukins, virus-induced lipotoxicity, and drug-induced injury. A systematic review of the literature revealed 22 cases of AP in COVID-19 patients. However, limitations of the reported cases make it difficult to establish a causal relationship between SARS-CoV-2 infection and AP. All of the studies agreed on special monitoring and surveillance of this subset of patients due to the still unknown clinical progression, therapeutic implications, and prognosis.
AP should be considered in COVID-19 patients, especially in those exhibiting abdominal pain and systematic, and complete reporting of these cases should be general practice. However, there is still insufficient evidence showing that COVID-19 can cause AP or negatively impact prognosis. Additional studies are needed to clarify the relationship between these two entities and their therag
Core Tip: Recently, an association between acute pancreatitis (AP) and coronavirus disease 2019 (COVID-19) has been proposed, but the mechanisms of pancreatic injury of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are not fully understood. Although viral-induced AP is an established diagnosis, there is still insufficient evidence clearly showing COVID-19 as AP etiology. We conducted an in-depth analysis on the mechanisms of pancreatic injury by SARS-CoV-2 and reviewed published cases of AP in COVID-19 patients.
- Citation: Correia de Sá T, Soares C, Rocha M. Acute pancreatitis and COVID-19: A literature review. World J Gastrointest Surg 2021; 13(6): 574-584
- URL: https://www.wjgnet.com/1948-9366/full/v13/i6/574.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i6.574
Coronavirus disease 2019 (COVID-19) emergence in December 2019 brought unprece
The most common clinical manifestations of COVID-19 are respiratory, particularly fever and cough[2], but as cases have increased of widespread severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) across the globe, other symptoms and clinical scenarios have emerged. Gastrointestinal (GI) and hepatic involvement, among others, have been recognized and are mediated by the expression of angiotensin-converting enzyme 2 (ACE2) on the GI tract, the main receptor of SARS-CoV-2[3,4]. A recent systematic review and meta-analysis by Mao et al[5] showed that the estimated prevalence of digestive symptoms is 15%. Nausea, vomiting, diarrhea, and loss of appetite are the most frequent symptoms. Nineteen percent of patients present with liver injury, which may be more prevalent in fatal cases[5]. Furthermore, approximately 10% of COVID-19-positive patients may present with only GI symptoms. This clinical presentation may be associated with the delayed diagnosis of COVID-19 and a tendency of the disease to progress to more severe forms[5].
The expression of ACE2 in pancreatic cells (both exocrine glands and islets) renders the pancreas a potential target for SARS-CoV-2, but only recently has it received attention for its role in the COVID-19 clinical picture. Several case reports of pancreatic injury and acute pancreatitis (AP) caused by the novel coronavirus have been reported. About 1%-2% of non-severe and 17% of severe cases of COVID-19 exhibit pancreatic injury, which may have developed before the patient’s admission[6]. However, there is still uncertainty about the physiopathological mechanisms involved and the precise etiology of pancreatic injury in the reported cases.
We conducted a literature review to clarify the relationship between SARS-CoV-2 infection and AP.
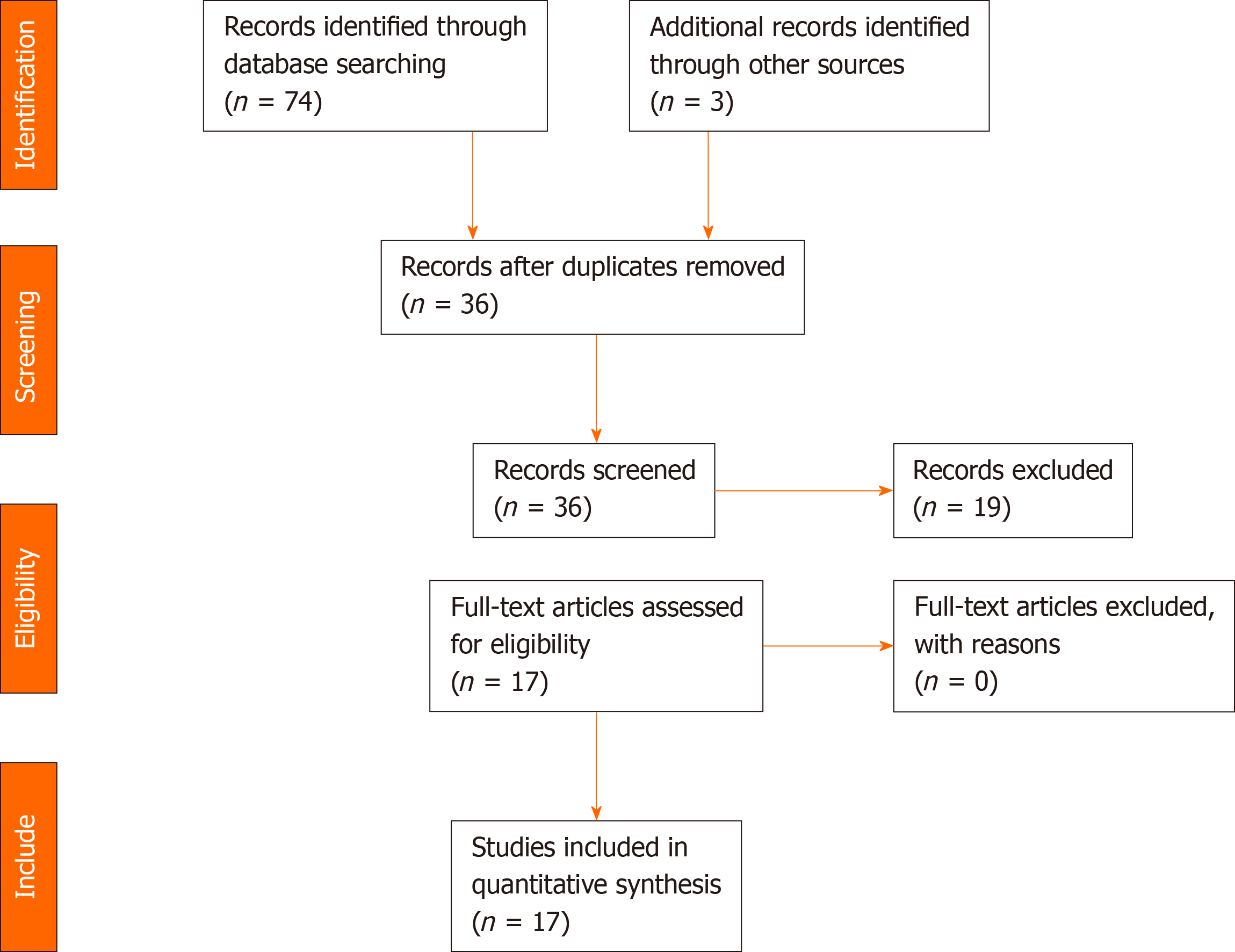
A systematic review was conducted according to PRISMA guidelines[7]. We searched the PubMed and EMBASE databases on November 1, 2020 for published articles using the medical subject headings keywords “COVID-19” and “pancreatitis.” Considering the urgency of the topic, a grey literature search using the same keywords was done on Google Scholar to increase the sensitivity of the search. Articles were included if they reported AP cases in COVID-19 patients. Review studies and articles dealing with pediatric patients and COVID-19 patients without the diagnosis of AP, even if pancreatic lesion was suspected, were excluded from our systematic review. References of eligible manuscripts were screened for additional articles. The literature search was restricted to articles published in English, Spanish, and Portuguese.
The titles and abstracts of studies retrieved by the search strategy and those from additional sources, namely by cross-referencing, were screened independently by all authors to identify studies that potentially met the inclusion criteria. Then full texts of these potentially eligible studies were retrieved and independently assessed for eligibility. Any disagreements between them over the eligibility of particular studies was resolved through discussion with the three authors, and a consensus was met in all included papers. When not available, the full texts were requested from the authors, and only full text articles were included in this review. Records were managed with Zotero (version 5.0) to exclude duplicates.
Data were extracted from each of the papers undergoing full text review, and included authors, study design, population number, gender of included patients, age, co-morbidities, symptoms on admission, AP etiology, severity and both local and systemic complications reported, method for COVID-19 diagnosis, intensive care unit admission, and need for mechanical ventilation. Descriptive statistics were used to analyze the data. Given the heterogeneity of the study population and design, a meta-analysis was not possible to perform. The results have been reported according to PRISMA and AMSTAR guidelines.
Secondary literature on the physiopathology of pancreatic involvement by SARS-CoV-2 was conducted and the review of paper titles, abstracts, and filtering for those requiring full text evaluation was made by the lead author. A cross-referencing search was done for additional articles.
For the systematic review, the initial search yielded 74 papers. After duplicate removal, abstract screening, cross-referencing search, and individual paper analysis, 17 were included in the study. The PRISMA flow diagram in Figure 1 depicts the reasons for paper exclusion.
Data were collected and the results are summarized in Table 1. A total of 22 cases of AP in COVID-19 patients was reported in 17 articles (11 case reports, 2 case series and 4 letters to Editor). Some of the included cases do not include important medical data, including patient previous medical history, a complete characterization and classification of the AP episode or of the COVID-19 infection. While all cases of AP were diagnosed based on the Atlanta guidelines, in many, the severity of the AP episode was not adequately recorded or there was insufficient available data to support the given severity score (mild, moderately severe, and severe). Even so, when clearly stated, we used the indicated severity score in this review. In very few reports, COVID-19 severity was assessed and different criteria were used, so we decided to remove this item from our review.
| Ref. | Study design | Population, No. | Gender | Age (yr) | Co-morbidities | Symptoms on admission | AP etiology | AP severity | Local complications | Systemic complications | COVID-19 diagnosis | ICU | Mechanical ventilation | |
| Resp | GI | |||||||||||||
| Kumar et al[30], 2020 | Case report | 1 | F | 67 | HT, abdominal surgery | X | √ | Unknown | (Moderately) severe1 | Pancreatic necrosis | Respiratory dysfunction | NP swabRT-PCR2 | √ | X |
| Ibrahim et al[31], 2020 | Case report | 23 | M | 33 | NA | √ | √ | Unknown | Severe | None | Respiratory and renal failureIleus | NP swabRT-PCR2 | √ | √ |
| Elhence et al[24], 2020 | Case series | 5 | F | 31 | NA | √ | √ | Biliary | Severe | Infected WON | Respiratory failure | NA4 | NA | X |
| M | 40 | Chronic alcoholism | √ | √ | Alcohol | Severe | Infected WON | Respiratory and renal failures | RT-PCR5 | NA | X | |||
| M | 42 | NA | √ | √ | Biliary | Severe | Infected WON | Respiratory failure | NA6 | NA | NA | |||
| NA | NA | NA | √ | √ | Unknown | Mild | X | NA | NA2 | NA | NA | |||
| NA | NA | NA | √ | √ | Unknown | Mild | X | NA | NA2 | NA | NA | |||
| Cheung et al[32], 2020 | Case report | 1 | M | 38 | None | X7 | √ | Unknown | Mild8 | X | X | NP swab; RT-PCR2 | X | NA |
| Brikman et al[33], 2020 | Case report | 1 | M | 61 | None | √ | √ | Unknown | NA | X | NA | NP swab; RT-PCR9 | NA | X |
| Liaquat et al[34], 2020 | Case report | 1 | M | 53 | None | √ | √ | Type 1 AIP due to elevated IgG4 levels | Severe | Acute infected necrotic collection7 | NA | NP swab; RT-PCR10 | NA | X |
| Bokhari and Mahmood[35], 2020 | Case report | 1 | M | 32 | None | √ | √ | Unknown | NA | Acute peripancreatic fluid collection | NA | RT-PCR11 | X | NA |
| Gonzalo-Voltas et al[36], 2020 | Case report | 1 | F | 76 | GERD, dislipidemia | √ | √ | Unknown | Mild | X | None | RT-PCR2 | X | NA |
| Gadiparthi et al[28], 2020 | Letter to editor | 1 | M | 40 | Obesity (grade II) | X | √ | Metabolic (hypertriglyceridemia) | Moderately severe | Acute fluid collections | Respiratory | NP swab; RT-PCR2 | √ | X |
| Karimzadeh et al[37], 2020 | Case report | 1 | F | 65 | HT, asthma | X | √ | Unknown | NA | X | Respiratory failure | RT-PCR2 | √ | X |
| Pinte and Baicus[38], 2020 | Letter to editor | 1 | M | 47 | None | √ | X | Unknown | NA | X | NA | NA | NA | NA |
| Schepis et al[21], 2020 | Case report | 1 | F | 67 | NA | X | √ | Unknown | Moderately severe | Pseudocyst | NA | NP swab and pseudocyst fluid RT-PCR2 | NA | NA |
| Miao et al[39], 2020 | Letter to editor | 1 | F | 26 | None | X | √ | Unknown | NA | X | NA | RT-PCR2 | NA | NA |
| Aloysius et al[40], 2020 | Case report | 1 | F | 36 | Obesity (grade II), chronic anxiety | √ | √ | Unknown | Severe | X | Respiratory | NP swab; RT-PCR12 | √ | X |
| Hadi et al[41], 2020 | Case series | 313 | F | 47 | None | √ | X | Unknown | Severe | X | Respiratory and renal failure | NP swab and tracheal aspirates RT-PCR2 | √ | √ |
| F | 68 | HT, hypothyroidism, osteoporosis | √ | √ | Unknown | Severe | NA | Respiratory and renal failure | NP swab and tracheal aspirates RT-PCR2 | √ | √ | |||
| Anand et al[42], 2020 | Letter to editor | 1 | F | 59 | Thrombophilia, cholecystectomy | √ | X14 | Unknown | NA | X | NA | RT-PCR15 | X | NA |
| Meireles et al[43], 2020 | Case report | 1 | F | 36 | CKD, HT | √ | X | Unknown | NA | X | NA | NA16 | X | NA |
In the narrative review, expert opinions, review articles, and experimental studies, including in vitro experiments were included. Several plausible explanations on pancreatic injury by SARS-CoV-2 are noted and can be grouped into direct virus-mediated injury, systemic inflammatory response and circulating pro-inflammatory interleukins and cytokines, virus-induced lipotoxicity, and drug-induced injury. These mechanisms are further explored in the Discussion.
Pancreatic lesions, usually defined by serum amylase and/or lipase elevations, and cases of AP have been reported in COVID-19 patients. Autopsy studies in patients previously infected by SARS-CoV-2 identified areas of focal pancreatitis and pancreatic and/or peripancreatic necrosis and calcifications, but only two-thirds of these patients had exhibited symptoms suggestive of AP[8]. The diagnosis of AP, based on the modified Atlanta criteria, requires two of the following three features: Abdominal pain consistent with AP (acute onset of a persistent, severe, epigastric pain often radiating to the back), serum lipase activity (or amylase activity) at least three times greater than the upper limit of normal, and characteristic findings of AP on contrast-enhanced computed tomography (CECT) and less commonly magnetic resonance imaging or transabdominal ultrasonography[9]. This classification also divides AP into interstitial edematous pancreatitis and necrotizing pancreatitis and identifies local and systemic complications, which have a clear impact on disease progression, morbidity, and mortality[9]. All cases included in our study fulfilled the above criteria for the diagnosis of AP, but only a few included AP classification and local and systemic complications in the case report.
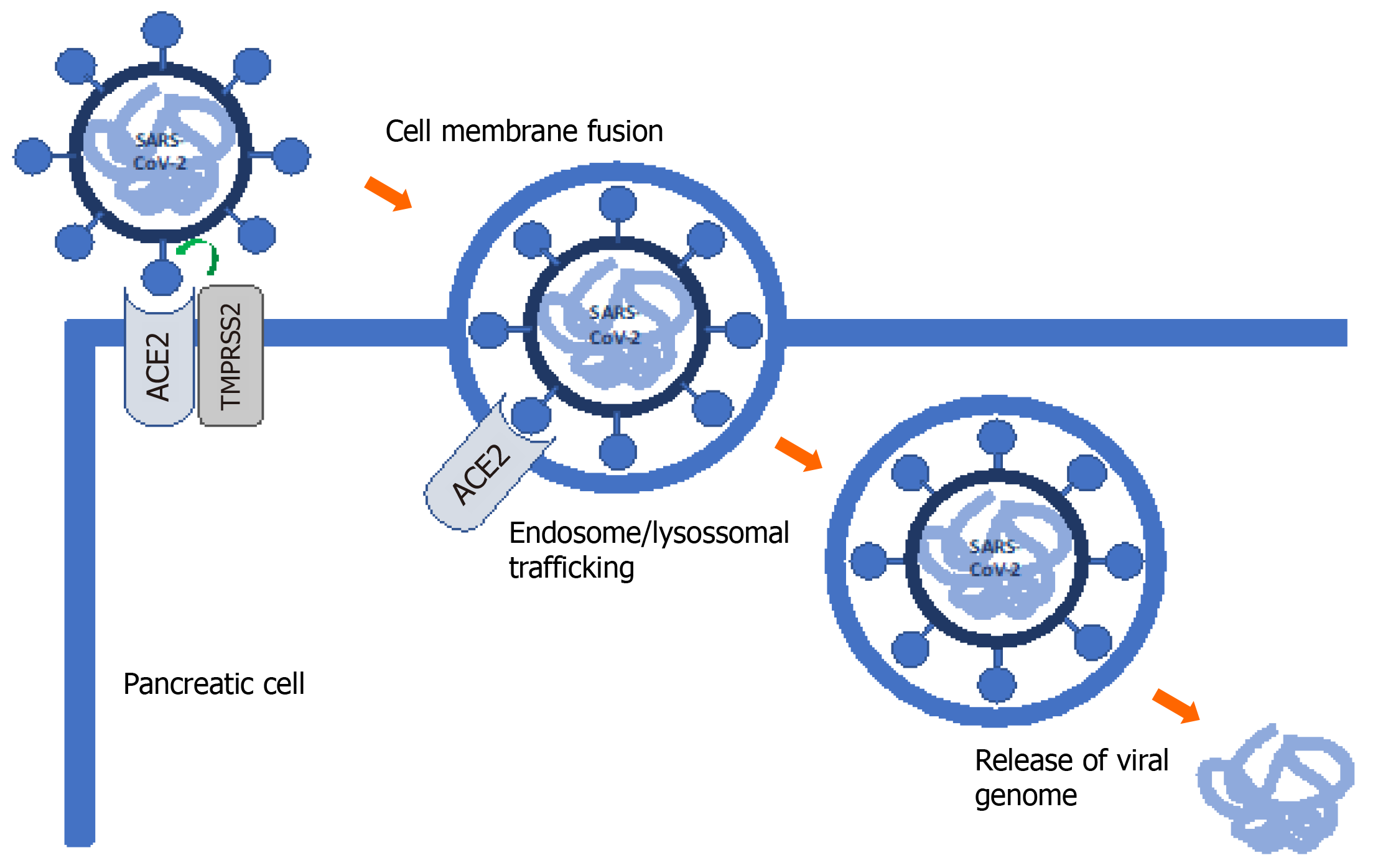
SARS-CoV-2 infection requires entry of the virus into the host cell. Metallopeptidase ACE2 has been identified as the cell receptor. Transmembrane serine protease 2 (TMPRSS2) facilitates viral entry at the plasma membrane surface. As such, co-expression of both ACE2 and TMPRSS2 is critical for successful SARS-CoV-2 infection (Figure 2)[10].
ACE2 is normally expressed in the pancreas. Liu et al[6] explored its expression and distribution, finding higher levels of ACE2 in the pancreas than in the lung and ACE2 expression in both exocrine glands and islets. Most studies have focused on ACE2 expression and there are few reports on TMPRSS2 expression in the pancreas. In one of these studies, Coate et al[11] found that ACE2 is mainly expressed in islet and exocrine tissue capillaries and some ductal cells, while TMPRSS2 is mainly expressed in ductal cells. However, ACE2 and TMPRSS2 are rarely co-expressed in pancreatic ducts. Pancreatic beta cells do not co-express ACE2 and TMPRSS2 and several authors have questioned the direct cytotoxic effects of SARS-CoV-2 on beta cells. It is still unknown whether SARS-CoV-2 directly and/or indirectly affects beta cell function[11]. However, COVID-19-associated glucose metabolism changes and diabetes appear to be multifactorial, resulting from systemic inflammation and metabolic changes in other organs, including the liver, muscle and adipose tissues, and are not exclusively the result of pancreatic damage. Further studies evaluating SARS-CoV-2 entry into beta cells and not only receptor expression are needed[11].
Severe cases of AP and COVID-19 are characterized by a cytokine storm, which ultimately leads to multiorgan failure and increased mortality. A recent meta-analysis by Hegyi et al[12] found similar patterns of cytokine expression in both COVID-19 and AP. In this scenario, pancreatic damage may result in interstitial leakage of pancreatic lipase and consequently fat tissue lipolysis increasing unsaturated fatty acid levels, which in turn causes mitochondrial injury and excessive production and release of proinflammatory mediators–a cytokine storm. Levels of interleukin (IL)-6, IL-8, and IL-10 were increased in severe cases of both AP and COVID-19 compared to non-severe cases[12]. Consequently, some authors have hypothesized a beneficial role of extracorporeal cytokine absorption in severe cases[13]. At this point, there are insufficient data to differentiate between severe AP caused by COVID-19 from severe AP with COVID-19.
After the cytokine storm associated with severe COVID-19 cases, there is a migration of inflammatory cells to the inflammation/infection site, promoting a pro-inflammatory feedback loop. Tissue factor is upregulated on platelets, white blood and endothelial cells, leading to activation of both extrinsic and intrinsic coagulation pathways and thrombin generation. This microthrombotic event described in lung vasculature[14] can also take place in the pancreatic vasculature, causing hypoperfusion and ischemia[15] with the subsequent induction of an inflammatory response and AP.
After reviewing the clinical cases, certain issues are worth analyzing: Abdominal pain, a cardinal symptom in most cases of AP, may be due to SARS-CoV-2 injury to the GI tract, and it may not be possible to differentiate it from the AP pain; SARS-CoV-2 pancreatic injury causing serum lipase and/or amylase elevation has been recognized, mainly in severe cases, but per se it is not diagnostic of AP; serum lipase elevation is not specific of pancreatic pathology, and can be seen in other GI pathology, including gastroparesis, gastritis, enteritis and colitis[16], which are also recognized to be part of the COVID-19 clinical picture; and although infrequent, there are cases of severe AP due to respiratory dysfunction in COVID-19 patients without abnormalities on CECT scan (most severe cases exhibit local peripancreatic complications).
A multiple-hit theory in AP has been recognized and multiple etiological factors can contribute to AP development. However, a complete work-up determining AP etiology is of utmost importance, to avoid deeming cases as idiopathic or establishing an incorrect diagnosis. Viral-attributed AP is rare, but well described, more frequently affecting immunocompromised patients[17,18]. The underlying pathophysiology varies with the type of virus involved. Although still controversial, the main receptors of SARS-CoV-2 are expressed in the pancreas and pancreatic injury has been recognized in COVID-19 patients, especially in severe cases. The thrombogenic state of COVID-19 can also contribute to pancreatic hypoperfusion and ischemia, another established etiology of AP. However, in some cases, it is difficult to exclude other cau
Even SARS-CoV-2 detection in pseudocyst fluid, as reported by Schepis and colleagues[21], is not unequivocal evidence of AP caused by the novel coronavirus, and several hypotheses arise, including retrograde contamination from the GI tract and/or SARS-CoV-2 infection through inflammatory cells, as a Trojan horse. In a retrospective multicenter study on unusual manifestations of COVID-19, Miró et al[22] did not find an increased frequency of AP in these patients.
Furthermore, idiopathic AP (IAP) is an exclusion diagnosis, which indicates that no etiology has been determined after a complete diagnostic evaluation, including a detailed history, laboratory serum tests, and adequate imaging. Numerous studies have suggested that microlithiasis and sludge may be the cause of a large subset of previously diagnosed IAP and endoscopic ultrasound imaging and magnetic resonance cholangiopancreatography can detect biliary etiology in one-third of patients diagnosed with IAP[23]. The etiologic evaluation of the reported cases is highly heterogeneous and doubts may arise in their classification as IAP, viral-attributed AP cases or even SARS-CoV-2 induced AP. The controversy broadens when determining the role of SARS-CoV-2 in cases of AP with a defined etiology.
It is also important to consider the temporal relationship between COVID-19 diagnosis and AP. In some cases, COVID-19 was diagnosed several days after AP admission, which leads us to question the impact of COVID-19 in these cases.
In a case series, published by Elhence et al[24], three cases of severe AP with respiratory failure (systemic complication of AP) tested positive for COVID-19 several days after the diagnosis of AP (34 to 91 d from admission). These patients did not develop severe respiratory complications due to the novel coronavirus. A marked inflammatory response early in the course of AP can lead to organ failure and the development of a compensatory anti-inflammatory response syndrome, a state of immune exhaustion[9], preventing a strong inflammatory response to SARS-CoV-2. It has also been postulated that the immune response in AP, determined by individual genetic factors, can also modulate the inflammatory response to SARS-CoV-2 and that COVID-19 may be associated with a milder course in most of these cases, especially in younger patients.
In relation to AP treatment in COVID-19 patients, currently no guidelines are available and no specific recommendations can be made. General supportive measures and fluid resuscitation guided by the patient’s hemodynamic status are the mainstay of AP treatment. However, careful monitoring is advised as many COVID-19 patients may pose specific and unpredictable challenges. Drugs known to cause pancreatic lesion should be considered for suspension, based on their indication, the patient´s clinical status, and their risk-benefit relationship.
Several sequelae of AP including new onset diabetes and exocrine insufficiency are more frequent in severe cases of AP, alcohol-induced pancreatitis, and when pancrea
The paucity of published literature associated with short follow-up periods and some inconsistent findings, have rendered prognostic evaluation in this subset of patients difficult to determine. At this moment, no considerations in the prognosis of AP in COVID-19 patients can be drawn.
This review had some limitations. The case reports included in our review have a risk of bias, as certain clinical information was not included and none of the case reports were written according to CARE guidelines[29]. The etiologic work-up of some of these patients was also incomplete when considering current guidelines, and the attribution of SARS-CoV-2 as the causative agent of AP in some causes may be abusive.
Despite the trend in recent literature of trying to establish or refute the role of SARS-CoV-2 in AP cases, currently, there is no sufficient evidence showing that COVID-19 can cause AP or negatively impact prognosis. Adherence to AP guidelines, namely diagnosis and etiological work-up, and careful monitoring of patients are of utmost importance to ensure the most adequate orientation and avoid convenience diagnosis. Prediction of disease course, assessment of disease severity in the background of COVID-19 and overall outcome when these two entities coexist are some of the most pertinent open research questions. Further studies are needed to clarify SARS-CoV-2 pancreatic injury and to directly exploit a causal relation between SARS-CoV-2 and AP. Furthermore, patients with suspected SARS-CoV-2-induced AP should be followed in a timely manner to assess patient’s recovery and/or associated complications including new-onset diabetes, pancreatic exocrine insufficiency, pancreatitis-induced local complications, and/or chronic pancreatitis.
There is increasing literature connecting acute pancreatitis (AP) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, but whether SARS-CoV-2 can cause AP or is an epiphenomenon remains a subject of debate.
To explore current literature and provide a concise overview of the current evidence as well as possible mechanisms of pancreatic injury in coronavirus disease 2019 (COVID-19) patients.
To provide an overview of current evidence on AP in COVID-19 patients and to promote and enhance future studies on this special subset of patients.
Systematic and narrative review of the literature.
Available studies on AP in COVID-19 patients present important limitations and mechanisms of pancreatic injury are debatable and not completely understood.
Currently there is insufficient evidence showing that SARS-CoV-2 infection can cause AP and the therapeutic and prognostic significance of AP in COVID-19 patients is largely unknown.
This is a very important issue, requiring ongoing research.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: Sociedade Portuguesa de Cirurgia; Asociación Española de Cirujanos; Sociedade Portuguesa de Cirurgia Minimamente Invasiva; Sociedade Portuguesa da Hérnia e Parede Abdominal.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Portugal
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Badovinac D, Fujino Y, Zhan Q, Zhao CF S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li JH
| 1. | Worldometer W. Coronavirus Update (live)-Worldometer. [cited 25 December 2020]. Available from: https://www.worldometers.info/coronavirus/?. |
| 2. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18875] [Article Influence: 3775.0] [Reference Citation Analysis (7)] |
| 3. | Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831-1833. e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1985] [Cited by in RCA: 1994] [Article Influence: 398.8] [Reference Citation Analysis (1)] |
| 4. | Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol. 2020;251:228-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 661] [Cited by in RCA: 738] [Article Influence: 147.6] [Reference Citation Analysis (0)] |
| 5. | Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J, Zhu LR, Chen Y, Iacucci M, Ng SC, Ghosh S, Chen MH. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:667-678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 741] [Cited by in RCA: 754] [Article Influence: 150.8] [Reference Citation Analysis (0)] |
| 6. | Liu F, Long X, Zhang B, Zhang W, Chen X, Zhang Z. ACE2 Expression in Pancreas May Cause Pancreatic Damage After SARS-CoV-2 Infection. Clin Gastroenterol Hepatol 2020; 18: 2128-2130. e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 343] [Cited by in RCA: 473] [Article Influence: 94.6] [Reference Citation Analysis (0)] |
| 7. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8049] [Article Influence: 536.6] [Reference Citation Analysis (2)] |
| 8. | Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, Vander K, Bargfrieder U, Trauner M. Pulmonary Arterial Thrombosis in COVID-19 With Fatal Outcome : Results From a Prospective, Single-Center, Clinicopathologic Case Series. Ann Intern Med. 2020;173:350-361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 600] [Cited by in RCA: 619] [Article Influence: 123.8] [Reference Citation Analysis (0)] |
| 9. | Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4932] [Cited by in RCA: 4330] [Article Influence: 360.8] [Reference Citation Analysis (45)] |
| 10. | Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Cui X, Xiao J, Zhan J, Meng T, Zhou W, Liu J, Xu H. Digestive system is a potential route of COVID-19: an analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut. 2020;69:1010-1018. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 314] [Cited by in RCA: 380] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 11. | Coate KC, Cha J, Shrestha S, Wang W, Gonçalves LM, Almaça J, Kapp ME, Fasolino M, Morgan A, Dai C, Saunders DC, Bottino R, Aramandla R, Jenkins R, Stein R, Kaestner KH, Vahedi G; Consortium H; Brissova M, Powers AC. SARS-CoV-2 Cell Entry Factors ACE2 and TMPRSS2 are Expressed in the Pancreas but are Not Enriched in Islet Endocrine Cells. bioRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 144] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 12. | Hegyi P, Szakács Z, Sahin-Tóth M. Lipotoxicity and Cytokine Storm in Severe Acute Pancreatitis and COVID-19. Gastroenterology. 2020;159:824-827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 13. | Convertino I, Tuccori M, Ferraro S, Valdiserra G, Cappello E, Focosi D, Blandizzi C. Exploring pharmacological approaches for managing cytokine storm associated with pneumonia and acute respiratory distress syndrome in COVID-19 patients. Crit Care. 2020;24:331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Price LC, McCabe C, Garfield B, Wort SJ. Thrombosis and COVID-19 pneumonia: the clot thickens! Eur Respir J. 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 15. | Hackert T, Hartwig W, Fritz S, Schneider L, Strobel O, Werner J. Ischemic acute pancreatitis: clinical features of 11 patients and review of the literature. Am J Surg. 2009;197:450-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Kahil K, El Halabi M, Bou Daher H, Rustom LBO, Marrache M, Ichkhanian Y, El Sayed M, Sharara AI. Significant elevations in serum lipase in the emergency department: When it is not pancreatitis! Am J Emerg Med. 2020;38:1033-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Rawla P, Bandaru SS, Vellipuram AR. Review of Infectious Etiology of Acute Pancreatitis. Gastroenterology Res. 2017;10:153-158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 112] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 18. | Simons-Linares CR, Imam Z, Chahal P. Viral-Attributed Acute Pancreatitis: A Systematic Review. Dig Dis Sci. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Morrison AR, Johnson JM, Ramesh M, Bradley P, Jennings J, Smith ZR. Acute hypertriglyceridemia in patients with COVID-19 receiving tocilizumab. J Med Virol. 2020;92:1791-1792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 20. | Rubel AR, Chong PL, Abdullah MS, Asli R, Momin RN, Mani BI, Chong VH. Lipemic serum in patients with Coronavirus Disease 2019 (COVID-19) undergoing treatment. J Med Virol. 2020;92:1810-1811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Schepis T, Larghi A, Papa A, Miele L, Panzuto F, De Biase L, Annibale B, Cattani P, Rapaccini GL. SARS-CoV2 RNA detection in a pancreatic pseudocyst sample. Pancreatology. 2020;20:1011-1012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 22. | Miró Ò, Llorens P, Jiménez S, Piñera P, Burillo-Putze G, Martín A, Martín-Sánchez FJ, González Del Castillo J; Spanish Investigators in Emergency Situations TeAm (SIESTA) network. Frequency of five unusual presentations in patients with COVID-19: results of the UMC-19-S1. Epidemiol Infect. 2020;148:e189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 23. | Wan J, Ouyang Y, Yu C, Yang X, Xia L, Lu N. Comparison of EUS with MRCP in idiopathic acute pancreatitis: a systematic review and meta-analysis. Gastrointest Endosc 2018; 87: 1180-1188. e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 24. | Elhence A, Mahapatra SJ, Vajpai T, Garg PK. Acute pancreatitis and nosocomial COVID-19: Cause specific host responses may determine lung injury. Pancreatology. 2020;20:1258-1261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Zhi M, Zhu X, Lugea A, Waldron RT, Pandol SJ, Li L. Incidence of New Onset Diabetes Mellitus Secondary to Acute Pancreatitis: A Systematic Review and Meta-Analysis. Front Physiol. 2019;10:637. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 77] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 26. | Jawaid S, Forsmark CE. Exocrine Pancreatic Insufficiency Following Acute Pancreatitis: True Association or EPIphenomenon? Dig Dis Sci. 2019;64:1731-1733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Wang F, Wang H, Fan J, Zhang Y, Zhao Q. Pancreatic Injury Patterns in Patients With Coronavirus Disease 19 Pneumonia. Gastroenterology. 2020;159:367-370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 276] [Cited by in RCA: 325] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 28. | Gadiparthi C, Bassi M, Yegneswaran B, Ho S, Pitchumoni CS. Hyperglycemia, Hypertriglyceridemia, and Acute Pancreatitis in COVID-19 Infection: Clinical Implications. Pancreas. 2020;49:e62-e63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 29. | Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, Kiene H, Helfand M, Altman DG, Sox H, Werthmann PG, Moher D, Rison RA, Shamseer L, Koch CA, Sun GH, Hanaway P, Sudak NL, Kaszkin-Bettag M, Carpenter JE, Gagnier JJ. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 741] [Cited by in RCA: 1021] [Article Influence: 127.6] [Reference Citation Analysis (0)] |
| 30. | Kumaran NK, Karmakar BK, Taylor OM. Coronavirus disease-19 (COVID-19) associated with acute necrotising pancreatitis (ANP). BMJ Case Rep. 2020;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 31. | Ibrahim YS, Karuppasamy G, Parambil JV, Alsoub H, Al-Shokri SD. Case Report: Paralytic Ileus: A Potential Extrapulmonary Manifestation of Severe COVID-19. Am J Trop Med Hyg. 2020;103:1600-1603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 32. | Cheung S, Delgado Fuentes A, Fetterman AD. Recurrent Acute Pancreatitis in a Patient with COVID-19 Infection. Am J Case Rep. 2020;21:e927076. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 33. | Brikman S, Denysova V, Menzal H, Dori G. Acute pancreatitis in a 61-year-old man with COVID-19. CMAJ. 2020;192:E858-E859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 34. | Liaquat H, Shupp B, Kapoor S, Matin A. High-Dose Prednisone for Treatment of Autoimmune Pancreatitis in a Patient with Coronavirus Disease 2019 (COVID-19) due to Infection with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Am J Case Rep. 2020;21:e926475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Bokhari SMMA, Mahmood F. Case Report: Novel Coronavirus-A Potential Cause of Acute Pancreatitis? Am J Trop Med Hyg. 2020;103:1154-1155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 36. | Gonzalo-Voltas A, Uxia Fernández-Pérez-Torres C, Baena-Díez JM. Acute pancreatitis in a patient with COVID-19 infection. Med Clin (Engl Ed) 2020; 155: 183-184. . [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Karimzadeh S, Manzuri A, Ebrahimi M, Huy NT. COVID-19 presenting as acute pancreatitis: Lessons from a patient in Iran. Pancreatology. 2020;20:1024-1025. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 38. | Pinte L, Baicus C. Pancreatic involvement in SARS-CoV-2: case report and living review. J Gastrointestin Liver Dis. 2020;29:275-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 39. | Miao Y, Lidove O, Mauhin W. First case of acute pancreatitis related to SARS-CoV-2 infection. Br J Surg. 2020;107:e270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 40. | Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H. COVID-19 presenting as acute pancreatitis. Pancreatology. 2020;20:1026-1027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 141] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 41. | Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL. Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members. Pancreatology. 2020;20:665-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 169] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 42. | Anand ER, Major C, Pickering O, Nelson M. Acute pancreatitis in a COVID-19 patient. Br J Surg. 2020;107:e182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 43. | Meireles PA, Bessa F, Gaspar P, Parreira I, Silva VD, Mota C, Alvoeiro L. Acalculous Acute Pancreatitis in a COVID-19 Patient. Eur J Case Rep Intern Med. 2020;7:001710. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |