Published online Feb 27, 2021. doi: 10.4240/wjgs.v13.i2.164
Peer-review started: November 24, 2020
First decision: December 20, 2020
Revised: January 2, 2021
Accepted: January 21, 2021
Article in press: January 21, 2021
Published online: February 27, 2021
Processing time: 71 Days and 15.2 Hours
In recent years, a decrease in incidence and mortality of colorectal cancer (CRC) has been observed in developed nations, presumably through public disease awareness and increased screening efforts. However, a rising incidence of CRC in young patients below the age of 50 years has been reported in several studies.
To study tumor biology in CRC patients below 50 years of age.
All patients with CRC were prospectively enrolled in our single-center oncologic database from January 2013 to December 2018 and were grouped and analyzed according to age (≥ 50 and < 50 years). Clinical as well as histopathological features were analyzed and compared. The study was approved by the local Ethics Committee. Fisher’s exact test or t-test was used to test for differences between the groups, as appropriate. All statistical analysis was performed with IBM SPSS software Version 25 (SPSS Inc, Armonk, NY, United States) and with R-Studio using R Version 3.4.1 (RStudio, Boston, MA, United States).
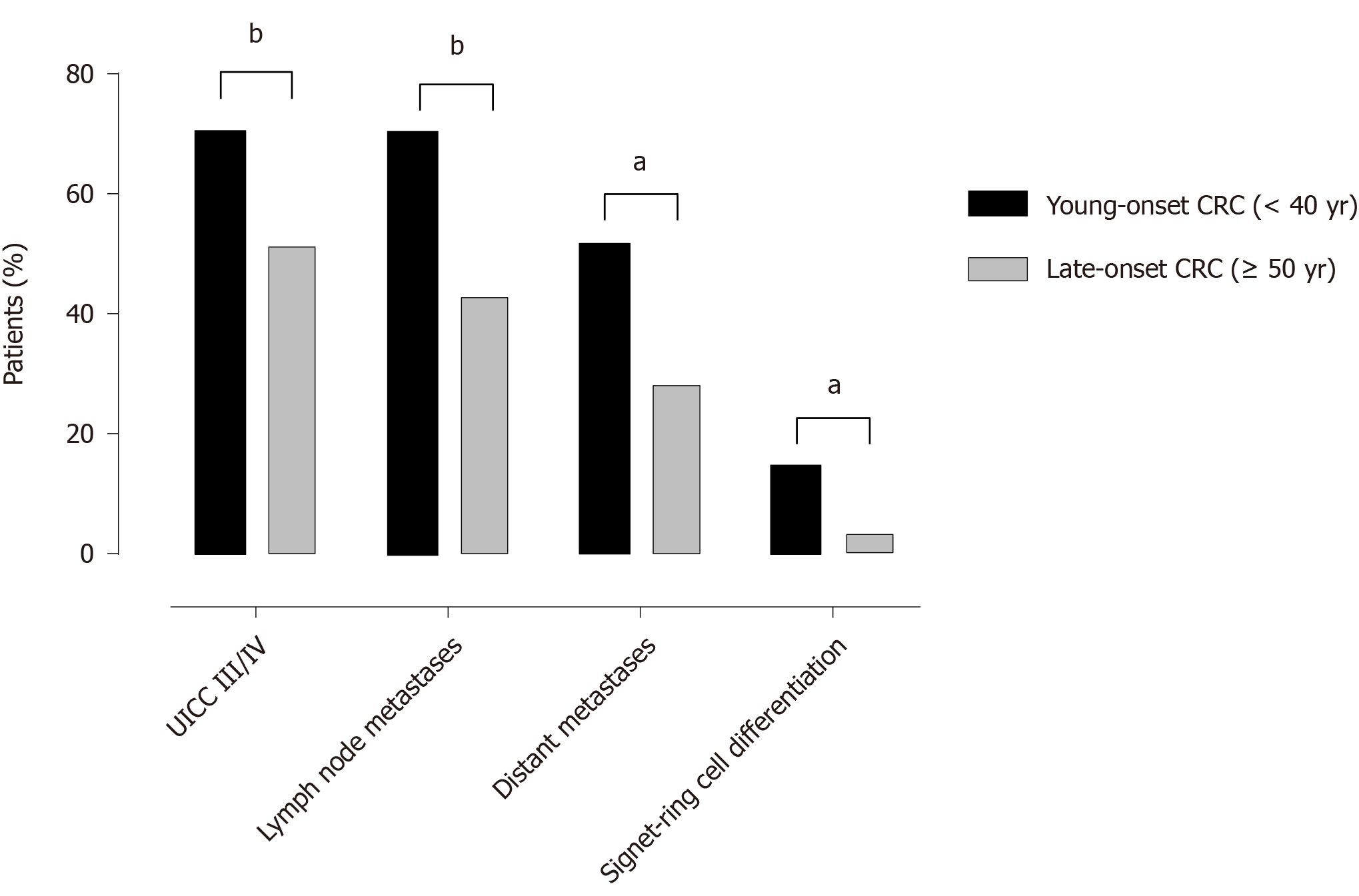
Seventeen percent of the 411 patients were younger than 50 years. Young patients were more often diagnosed with locally advanced T4-tumors and lymph node metastases (36.6% and 62% vs 17.7% and 42%; P < 0.01). In addition, a higher frequency of poorly differentiated (G3) tumors (40% vs 22.4% P < 0.05) was observed. More than every second patient below 40 years of age (51.8%) had distant metastases at diagnosis with a significant higher rate ring of signet cell differentiation compared to patients ≥ 50 years (14.8%, P < 0.05). Mutational status (KRAS, NRAS, BRAF, MSI) as well as selected behavioral risk factors showed no significant differences.
Distinct histopathologic features of increased biologic aggressiveness are found in patients with CRC of young-onset. Those patients present more frequently with more advanced tumor stages compared to older patients. Features of aggressive tumor biology underscore the need for earlier uptake of routine screening measures.
Core Tip: We evaluated differences in tumor biology between young-onset colorectal cancer patients (< 50 years of age) and late-onset colorectal cancer (CRC) patients (≥ 50 years of age) in a Swiss tertiary cancer center over a six-year period. Parameters of interest included clinical as well as histopathological characteristics. This study reports a surprisingly high rate of CRC of young-onset, while affected patients present more frequently with locally advanced tumors, lymphatic invasion and with more frequent lymphatic metastases. This work puts cancer incidence in relation to histopathological details, mutational status, surgical parameters and selected risk factors.
- Citation: Mueller M, Schneider MA, Deplazes B, Cabalzar-Wondberg D, Rickenbacher A, Turina M. Colorectal cancer of the young displays distinct features of aggressive tumor biology: A single-center cohort study. World J Gastrointest Surg 2021; 13(2): 164-175
- URL: https://www.wjgnet.com/1948-9366/full/v13/i2/164.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i2.164
Recent studies reported a rising incidence of colorectal cancer (CRC) in the younger population below the age of 50 years[1,2]. In 2030, more than 1 in 10 colon cancers and nearly 1 in 4 rectal cancers are projected to be diagnosed in an age group for whom routine screening is currently not recommended[3-5]. Although the adherence to screening programs for CRC is insufficient yet[6], screening has led to a decrease in the incidence of CRC with a considerable reduction of the cancer-related mortality in the population over 50 years of age[7].
In the population below 50 years, CRC not only shows a rising incidence but also appears to display a more aggressive phenotype. Young-onset CRC are more likely to have mucinous or signet ring cell differentiation and are typically diagnosed at a more advanced stage[8,9]. On one side, later stage at diagnosis could possibly be related to the lack of screening programs and lower awareness for symptoms typical for CRC. On the other hand, more aggressive tumor biology suggested by histopathological findings could play a role, since non-hereditary young-onset CRC patients seem to have unique genetic profiles (key differences in somatic gene mutations and gene methylation)[1,8,10,11].
There are further observations that incidence rates may correlate with a birth cohort effect, suggesting that exposures to environmental or life-style related factors in early childhood or adolescence may contribute to young-onset CRC[12]. However, the mechanisms or risk factors leading to young-onset CRC are poorly understood. Early type II diabetes, childhood obesity and antibiotics influencing microbial diversity, are discussed as potential risk factors for the development of CRC in the young population[12-14].
The purpose of our present study was to compare histopathologic features of CRC diagnosed in young compared to old patients at our institution. It is our hypothesis that distinct histologic features of young-onset CRC may explain the different clinical course of disease typically seen in this cohort.
All adult patients (18 years and older) with a CRC diagnosed at or referred to our center were prospectively recorded in our institutional CRC registry. Patient records from January 2013 to December 2018 were included in this study. Patients were divided into two groups (age ≥ 50 and < 50 years) based on the current recommendations to begin screening at an age of 50 years in many western countries. In addition, a second analysis was carried out including only patients < 40 years. Parameters of interest included clinical as well as histopathological characteristics. Additional parameters of interest not obtained by our CRC registry were obtained from operative notes, imaging reports and external consultation and endoscopy reports. The study was approved by the local Ethics Committee of the Canton of Zurich (KEK-ZH-Nr. 2019-00208).
For statistical analysis, t-test or Fisher’s exact test were used to test for differences between the groups, as appropriate. A P value < 0.05 is considered statistically significant. All statistical analysis was performed with IBM SPSS software Version 25 (SPSS Inc, Armonk, NY, United States) and with R-Studio using R Version 3.4.1 (RStudio, Boston, MA, United States).
A total of 411 patients with CRC have been treated at our institution between January 2013 and December 2018. Of these patients, 17% were diagnosed at an age of 49 or younger and 6.6% were below the age of 40 at time of diagnosis. The median age at diagnosis in the group < 50 years was 42 years (IQR, 35-46), compared to 68 in the group ≥ 50 years of age (IQR, 61-77) (Table 1). While there was no difference regarding gender and body mass index (BMI) (median BMI 24.7 and 25 kg/m2, respectively), there was a significant difference in terms of worse preoperative physical status in the older group as shown by the American Society of Anesthesiologist (ASA) Classification. The younger population not only had significantly lower ASA scores, they also had a lower rate of high-risk drinking (according to the 2015-2020 Dietary Guidelines for Americans[15]) (4.7% vs 15.2%, P < 0.05) and had higher preoperative albumin levels than the older population (median albumin level 41.5 g/L and 38.5 g/L respectively, P < 0.05), reflecting better physical status and a lower perioperative risk. However, there was no significant difference between the groups regarding current smoking habits.
| Demographic factors | CRC patients < 50 yr of age, n (%) | CRC patients ≥ 50 yr of age, n (%) | P value |
| Total number (%) | 70 (17) | 341 (83) | - |
| Gender | |||
| Male | 44 (62.9) | 209 (61.3) | 0.89 |
| Female | 26 (37.1) | 132 (38.7) | |
| BMI (kg/m2) | |||
| Median (IQR) | 24.7 (22.9-27) | 25 (22.4-28.9) | 0.3 |
| NA | 7 | 24 | |
| Obesity (BMI > 30kg/m2) | 7 (10) | 60 (21.3) | 0.154 |
| Inflammatory bowel disease1 | 3 (4.2) | 6 (1.8) | 0.19 |
| Hereditary CRC Syndrome2 | 5 (7.1) | 7 (2.1) | 0.04a |
| Neoadjuvant Treatment | 17 (24.3) | 65 (19.1) | 0.33 |
| ASA Class | |||
| I | 7 (11.3) | 9 (2.9) | < 0.01b |
| II | 43 (69.4) | 182 (58.9) | |
| III | 9 (14.5) | 110 (35.6) | |
| IV | 3 (4.8) | 8 (2.6) | |
| NA | 8 | 32 | |
| High-risk drinking3 | |||
| Yes | 3 (4.8) | 48 (15.4) | 0.03a |
| No | 60 (95.2) | 267 (84.8) | |
| NA | 7 | 26 | |
| Current smoker | 0.52 | ||
| Yes | 18 (28.6) | 76 (24.1) | |
| No | 45 (71.4) | 239 (75.9) | |
| NA | 7 | 26 | |
| Preoperative albumine level (g/L) | |||
| Median (IQR) | 41.5 (37.3-45) | 38.5 (33-42) | < 0.01b |
| NA | 32 | 159 |
The proportion of colon and rectal cancers was similarly distributed between the two age groups (40% vs 36.4% rectal cancer, P = 0.58). CRC of the colon were predominantly found on the left side (descending colon, sigmoid colon), without a significant difference between the age groups (68.1% and 68.7% respectively). There was no significant difference in the rate of neoadjuvant treatment between the groups (24.3% and 19.1% respectively) including neoadjuvant treatment for rectal cancer (36% vs 44% respectively).
The histopathological assessment of the colorectal tumors illustrated a higher proportion of locally advanced tumors invading adjacent structures (pT4) in younger patients < 50 (36.6% vs 17.7%, P < 0.01). Moreover, lymph node metastases were more frequent in young patients with an overall significantly higher mean lymph node ratio among the young (16.5% vs 8.2%, P < 0.01). Nearly one third of young patients had 4 or more positive lymph nodes (N2), as opposed to only 16% in the older population (P < 0.05). In line with this finding, lymphatic invasion (L1) was more frequent in young patients (61.1% vs 41.4%, P < 0.05). Regarding lymph node yield, a median of 22 lymph nodes were resected in young patients compared to a median of 18 lymph nodes in the cohort over 50 years (P < 0.05). Concerning synchronous distant metastases (M1) there was a tendency towards more frequent distant metastases in young patients (38.6% vs 27.9%, P = 0.08). In patients below 40 years of age significantly more distant metastases were diagnosed (< 40 years: 51.9% vs patients > 50 years: 27.9%, P = 0.014). With respect to Union for International Cancer Control (UICC) stage, young patients more frequently suffered from advanced stages at the time of diagnosis (UICC Stage III and IV 68.6% vs 51.1%, P < 0.05). Data from those with sporadic CRC in young (without inflammatory bowel disease or hereditary CRC syndromes) revealed the same trend with significantly higher incidence of lymph node metastases and distant metastases (65% vs 43% N+ status (P < 0.01) and 42% vs 28% M+ status (P = 0.05 respectively).
Regarding tumor grading, 40% of the tumors in the age group below 50 years of age showed a poor differentiation (G3) compared to only 22.4% in the older cohort (P < 0.05). In line with this finding, signet ring cell differentiation was significantly more frequent in patients below 40 years of age (14.8% vs 3.3% of patients ≥ 50 years, P = 0.015, Figure 1) even though this did not reach statistical significance in the cohort < 50 years compared to patients over 50 years (8.7% vs 3.3%, P = 0.12) (Table 2). Regarding mutational analysis of KRAS, NRAS, BRAF, Her2 or microsatellite instability (MSI) we found no significant differences in those patients whose mutational status was known (Table 3). However, a subgroup analysis of young patients with a molecular mutation (incl. MSI, K/NRAS, BRAF, HER2) vs young patients without mutations, revealed a significantly higher incidence of distant metastases in those with a mutation (60% vs 30% M+ respectively, P = 0.03). Additionally, individuals > 50 years with a molecular mutation showed a significantly higher incidence of N+ (57% vs 37% respectively, P < 0.01) and M+ status (45% vs 22% respectively, P < 0.001) compared to non-mutated CRC patients in the same age group. MSI related to hereditary non-polyposis colorectal cancer in the two groups was not significantly different (40% and 15.8%, P = 0.23).
| Tumor characteristics & histopathologic features | CRC patients < 50 yr of age, n (%) | CRC patients ≥ 50 yr of age, n (%) | P value |
| Tumor location | |||
| Colon | 42 (60) | 217 (63.6) | 0.58 |
| Rectum | 28 (40) | 124 (36.4) | |
| Right sided | 21 (30.4) | 92 (27.1) | 0.74 |
| Left sided (incl. rectum) | 47 (68.1) | 233 (68.7) | |
| Transverse colon | 1 (1.5) | 6 (1.8) | |
| Multiple locations | - (-) | 8 (2.36) | |
| UICC Tumor Stage | |||
| I | 12 (17.1) | 75 (22.1) | 0.04a |
| II | 10 (14.3) | 91 (26.8) | |
| III | 21 (30) | 83 (24.4) | |
| IV | 27 (38.6) | 91 (26.8) | |
| T-Status | |||
| T1 | 7 (10.6) | 48 (14.7) | < 0.01b |
| T2 | 11 (16.7) | 45 (13.8) | |
| T3 | 24 (36.4) | 176 (53.8) | |
| T4 | 24 (36.4) | 58 (17.7) | |
| NA | 4 | 14 | |
| Lymph node metastasis | |||
| N0 | 26 (38.2) | 184 (57.1) | < 0.01b |
| N1 | 20 (29.4) | 86 (26.7) | |
| N2 | 22 (32.4) | 52 (16.2) | |
| NA | 2 | 19 | |
| M-Status | |||
| M0 | 43 (61.4) | 238 (72.1) | 0.08 |
| M1 | 27 (38.6) | 92 (27.9) | |
| NA | - | 11 | |
| Vascular invasion | |||
| V0 | 22 (64.7) | 116 (65.9) | 1 |
| V1 | 12 (35.3) | 60 (34.1) | |
| NA | 36 | 165 | |
| Lymphatic invasion | |||
| L0 | 14 (38.9) | 116 (65.9) | 0.04a |
| L1 | 22 (61.1) | 60 (34.1) | |
| NA | 36 | 155 | |
| Histological grading | |||
| G1 | 2 (4.4) | 10 (4.1) | 0.03a |
| G2 | 25 (55.6) | 181 (73.6) | |
| G3 | 18 (40) | 55 (22.7) | |
| NA | 25 | 95 | |
| Histological type | |||
| Intestinal type | 53 (76.8) | 276 (82.1) | 0.12 |
| Signet ring cell type | 6 (8.7) | 11 (3.3) | |
| Mucinous type | 10 (14.5) | 49 (14.6) | |
| NA | 1 | 5 | |
| Stoma | |||
| Yes | 30 (46.9) | 163 (51.9) | 0.49 |
| No | 34 (53.1) | 151 (48.1) | |
| NA | 6 | 27 | |
| Lymph nodes removed | |||
| mean ± SD | 27.5 (17.1) | 20.1 (15.8) | 0.03a |
| Median (IQR) | 22 (15-33.8) | 18 (14-25) | |
| NA | 8 | 36 | |
| Lymph nodes positive | |||
| mean ± SD | 5 (10.1) | 1.61 (3.2) | 0.01a |
| Median (IQR) | 2 (0-5) | 0 (0-2) | |
| NA | 8 | 36 | |
| Lymph node ratio | |||
| mean ± SD | 0.1654 | 0.0817 | < 0.01b |
| Reoperation within 30 d | |||
| Yes | 5 (7.5) | 23 (7.2) | 1 |
| No | 59 (92.5) | 291 (91.8) | |
| NA | - | 3 |
| Molecular or immunohistochemical feature | CRC patients < 50 yr of age, n (%) | CRC patients ≥ 50 yr of age, n (%) | P value |
| Microsatellite stability | |||
| Stable | 56 (91.8) | 213 (84.9) | 0.21 |
| Unstabile | 5 (8.2) | 38 (15.1) | |
| NA | 9 | 90 | |
| KRAS mutation | |||
| Negative | 23 (65.7) | 48 (51.1) | 0.17 |
| Positive | 12 (34.3) | 46 (48.9) | |
| NA | 35 | 247 | |
| NRAS mutation | |||
| Negative | 27 (90) | 74 (94.9) | 0.39 |
| Positive | 3 (10) | 4 (5.1) | |
| NA | 40 | 263 | |
| BRAF mutation | |||
| Negative | 29 (90.6) | 87 (86.1) | 0.76 |
| Positive | 3 (9.4) | 14 (13.9) | |
| NA | 38 | 240 | |
| HER 2 | |||
| Negative | 8 (80) | 24 (70.6) | 0.70 |
| Positive | 2 (20) | 10 (29.4) | |
| NA | 60 | 307 |
Our study shows that a considerable number (17%) of CRCs are diagnosed before the age of 50. Other studies reported slightly lower rates of CRC patients below the age of 50, ranging from 7.5%-13%[16-20]. Although possibly being related to a referral bias, this high rate should certainly raise concerns especially in light of the fact that Switzerland appears to have one of the highest incidences of young-onset CRC worldwide[21].
Although our population does not provide the power to conclusively show an increase of CRC among the young of the same region, a rising incidence of CRC in young patients has been described by others[16,22,23]. For example, the work of Araghi and colleagues reported a rise in incidence of young-onset CRC of up to 3.1% over the most recent 10-year period in high-income countries[23]. Another international cohort study including nearly 2 million CRC cases of all 5 continents also reported an increase in CRC diagnoses in patients below 50 of up to 9% between 1988 and 2007[22]. Furthermore, as shown by Overholt et al[24], there is evidence that the formation of colonic adenoma seems to begin earlier than the recommended screening-age of 50 with a similar incidence of adenomas in the age groups 40-49 compared to 50-59 years. These observations have led to an update of the American Cancer Society guidelines recommending to commence general screening at the age of 45[25]. However, despite these developments, the majority of cancer or gastroenterology associations worldwide still adhere to a CRC screening program starting at the age of 50 for average risk individuals[4,5,26].
To better understand the phenomenon of CRC development in the younger population, a detailed investigation of the clinicopathologic characteristics of CRC is necessary and was the focus of our present study. Although we found no significant difference regarding tumor location (which may be due to type II error), other reports from western countries including North America, Europe and Australia demonstrate a clear predilection for the left colon and rectum in young patients[3,8,23,27]. Different mutation rates compared to right sided CRC[28] resulting in different tumor biology and pathogenesis may derive from a different embryologic origin of the rectum (hindgut) compared to the colon (midgut)[29]. However, the exact cause of the increased incidence of rectal cancer in the younger population is still unclear and probably multifactorial.
In our cohort, affected young individuals show distinct phenotypes of more aggressive tumor behavior with a higher likelihood of lymphatic metastatic disease at time of diagnosis. Not only were tumors more advanced locally (36% T4 tumors), they also showed higher rates of lymphogenic (62% N+ status, 16.5% lymph node ratio) and distant metastases in our younger cohort (51.8% M1 status < 40 years). Similarly, overall UICC cancer stage was more advanced (UICC 3 and 4) in this population (68.6% of patients below 50 years). These phenomena are consistent in our subgroup of young individuals with sporadic CRC and are in line with other recent studies reporting more advanced cancers (UICC 3 and 4) among the young varying between 53% and 63%. This triggered discussions of different cancer biology in young CRC patients[1,9,10,16,17,30]. In fact, there is evidence that tumors in young patients show a higher rate of poorly differentiated histological features along with mucinous or signet ring cell differentiation[8,23,27,31,32]. Chang et al[8], You et al[9] and Goldvaser et al[27] reported poor differentiation (G3) in 20%-27% of patients. Our findings are in line with these reports and even exceed those rates in that 40% of tumors in our collective showed poor differentiation (G3). The rates of mucinous or signet ring cell differentiation varies between 10.2%-18.1% and 7.6%-11.5% in the reports from You et al[9], Goldvaser et al[27] and Yantiss et al[30], meaning that nearly 1 out of 6 CRC in young-onset CRC patients show signs of harmful differentiation.
However, aggressive tumor biology alone may not be the only factor that determines advanced cancer stage in young patients at time of diagnosis. Considering the possibility of treatment delay, studies have shown that first, most of CRC patients younger than 50 years only present on an emergency department with acute symptoms[33] and second, that younger-onset CRC patients have a treatment delay of nearly 6 months from symptom onset[20]. Nevertheless, it is surprising that despite the more aggressive nature and therapeutic delay normally associated with a worse prognosis[8,34], young patients in several studies showed a similar stage-dependent overall survival and recurrence-free survival compared to the older population in several studies[8,27,31]. Possible explanations are the more aggressive surgical treatment and higher rates of (neo-) adjuvant chemotherapy offered in younger patients[18,27,35]. The reasons for this more aggressive treatment remain elusive, but likely reflect common practice as younger patients may tolerate more intensive therapy better and experience less treatment-related complications. However, Birkett and colleagues state that higher rates of adjuvant chemotherapy in early-stage CRC (I-II) procure no benefit regarding overall survival[18]. The fact that lymph node dissection was reported to be far more extensive in young patients[27], a result that is concordant with operations performed at our institution, suggests a more aggressive surgical approach in younger patients. Obviously, younger patients have fewer comorbidities and a better physical/nutritional status, which also make them more suitable to more aggressive operations associated with increased perioperative morbidity.
Although we did not see a difference in oncogenic mutation between the age cohorts, the subgroup with molecular mutations showed a more aggressive tumor behavior with more lymphatic and/or distant metastasis irrespective of age. Recent literature shows that especially in young-onset CRC patients, rates and types of gene mutations respective repression of transcription by DNA-methylation seems to differ from the cohort over 50 years of age[36]. Although other groups showed a similar tendency towards lower mutation rates of the pro-oncogene KRAS among young CRC patients[8,30], there is no clear difference in KRAS mutations in CRC patients under and over 50 years of age[37]. Data on BRAF mutation prevalence among young-onset CRC is conflicting as well, in a way that there is no unequivocal picture regarding RAS/RAF mutations at present[38]. A better understanding of the molecular make-up of young-onset cancers is being achieved by recent advances in decoding the genome with next-generation sequencing. With depicting differences in mutations of somatic genes and DNA methylation, different groups have provided better understanding of the epigenetics in young-onset CRC and highlight the importance of multigene assays and biobanking[10,11]. Connell and colleagues emphasize that young-onset CRC patients are treated similarly compared to the regular age CRC patients, despite unique molecular alterations. They clearly advocate individualized cancer therapies for this unique cancer population to have a real impact on outcome[10].
It appears unlikely that genetic changes alone are solely responsible for the increase in sporadic young-onset CRC given the sudden increase and geographical variances[22]. Trying to shed more light on risk factors favoring young-onset carcinogenesis, we studied rates of obesity, active smoking or regular alcohol intake between groups. Although we failed to show relevant differences between the young and “regular-aged” CRC patients in our single-center cohort, there is evidence that a birth cohort effect exists suspecting harmful exposure to environmental or life-style related factors in early life as shown by Murphy et al[12]. The global pandemic of obesity and diabetes type II, especially among the young[39], could fit to this trend considering the potential risk of obesity for development of a gastrointestinal cancer[40-42]. However, other authors have shown that besides BMI, exercise and particularly dietary factors play an important role in CRC carcinogenesis, favoring a Mediterranean diet to a diet with high intake of red und processed meats[43-46]. This could partly explain the geographical discrepancies with higher rates of young-onset cancer in South American countries compared to Mediterranean regions[22,45]. Similarly, early life exposures to antibiotics, nutritional colorants and preservatives may lead to a transformation of the gut microbiota, whereby the critical interaction of dysbiotic microbiota with the epithelium could promote cancerogenesis as suggested by others[13,14,38].
The weaknesses of our present study need to be noted. Due to the retrospective design of this study, residual confounders cannot be ruled out. Most notably, a type 2 error caused by the low numbers of this single-center analysis may have caused underreporting of several factors not reaching statistical significance. Regarding oncological outcome, long-term survival and recurrence data may by definition not be drawn from the recent time period studied. Further, data on histologic grade was not available for the entire dataset. Additionally, being a tertiary cancer center, the rates of younger patients with more advanced cancer stages could be higher due to preferred referrals from regional hospitals and private practitioners.
In summary, our study supports the hypothesis of greater biologic aggressiveness in CRC of young-onset. Affected patients present more frequently with locally advanced tumors, lymphatic invasion and with more frequent lymphatic metastases, suggesting worse prognosis[47]. These findings challenge the timing of the currently conducted CRC screening programs. The high rate of 17% of cancers diagnosed in patients younger than 50 years in itself highlights the need to lower the age threshold for government-based CRC screening programs. Future multi-centric studies will have to focus on identifying risk factors that put younger individuals at risk for CRC in an age before screening programs commence.
Over the last decade studies reported a rising incidence of colorectal cancer (CRC) in the younger population below the age of recommended screening thresholds. Alongside a higher incidence of young-onset CRC, there is more and more evidence of advanced tumors among younger patients. Reasons for increased tumor aggressiveness are the subject of active debate. Besides genetic risk factors, environmental factors may also play a decisive role.
Several studies tried to shed more light on risk factors favoring young-onset cancer. To date, there is more speculation than strong evidence on what may lead to advanced CRC in young individuals. With our analysis of clinicopathologic parameters we intended to make a contribution to better understand the tumor biology of CRC of the young.
The purpose of this work was to compare histopathologic features of CRC diagnosed in young compared to patients over 50 years of age at our institution.
The present study is a monocentric retrospective cohort analysis from a Swiss tertiary center hospital. Patient records covering a time period of 6 year (2013–2018) were included and analyzed according to age based on current CRC screening programs (< 50 and ≥ 50 years of age). The study was approved by the responsible ethics committee.
The histopathological assessment of the CRC showed a higher proportion of locally advanced tumors in younger patients below 50 years of age. In addition, lymph node metastases were more frequent in young patients with more distant metastases diagnosed among the youngest in our center (< 40 years of age). Mutational status and behavioral risk factors depicted no difference among the groups.
Patients younger than 50 years of age suffer from more advanced CRC, and show more frequently lymphatic invasion and with more frequent lymphatic metastases than the cohort over 50 years.
Our study highlights the need to identify young individuals at risk of developing early-onset CRC. Future research should be directed towards identification of individual risk factors for colorectal carcinogenesis at young age and reasons for the early metastatic behavior of tumors in affected patients. Finally, studies such as ours question the current age limit for government-driven CRC screening programs, which may have to start before the age of 50.
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: Switzerland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Akingboye AA, Fan RY, Rathnaswami A S-Editor: Zhang H L-Editor: A P-Editor: Li JH
| 1. | Ahnen DJ, Wade SW, Jones WF, Sifri R, Mendoza Silveiras J, Greenamyer J, Guiffre S, Axilbund J, Spiegel A, You YN. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc. 2014;89:216-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 345] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 2. | Siegel RL, Miller KD, Jemal A. Colorectal Cancer Mortality Rates in Adults Aged 20 to 54 Years in the United States, 1970-2014. JAMA. 2017;318:572-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 198] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 3. | Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, Cantor SB, Chang GJ. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015;150:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 777] [Article Influence: 77.7] [Reference Citation Analysis (0)] |
| 4. | US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW Jr, García FAR, Gillman MW, Harper DM, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Owens DK, Phillips WR, Phipps MG, Pignone MP, Siu AL. Screening for Colorectal Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:2564-2575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1249] [Cited by in RCA: 1388] [Article Influence: 154.2] [Reference Citation Analysis (1)] |
| 5. | Bénard F, Barkun AN, Martel M, von Renteln D. Systematic review of colorectal cancer screening guidelines for average-risk adults: Summarizing the current global recommendations. World J Gastroenterol. 2018;24:124-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 228] [Cited by in RCA: 204] [Article Influence: 29.1] [Reference Citation Analysis (7)] |
| 6. | Spaeth A, Zwahlen M. Use of lower gastrointestinal endoscopy and fecal occult blood test in the 2007 Swiss Health Interview Survey respondents aged 50 years and older. Endoscopy. 2013;45:560-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Shaukat A, Mongin SJ, Geisser MS, Lederle FA, Bond JH, Mandel JS, Church TR. Long-term mortality after screening for colorectal cancer. N Engl J Med. 2013;369:1106-1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 552] [Cited by in RCA: 646] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 8. | Chang DT, Pai RK, Rybicki LA, Dimaio MA, Limaye M, Jayachandran P, Koong AC, Kunz PA, Fisher GA, Ford JM, Welton M, Shelton A, Ma L, Arber DA, Pai RK. Clinicopathologic and molecular features of sporadic early-onset colorectal adenocarcinoma: an adenocarcinoma with frequent signet ring cell differentiation, rectal and sigmoid involvement, and adverse morphologic features. Mod Pathol. 2012;25:1128-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 261] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 9. | You YN, Xing Y, Feig BW, Chang GJ, Cormier JN. Young-onset colorectal cancer: is it time to pay attention? Arch Intern Med. 2012;172:287-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 215] [Article Influence: 15.4] [Reference Citation Analysis (1)] |
| 10. | Connell LC, Mota JM, Braghiroli MI, Hoff PM. The Rising Incidence of Younger Patients With Colorectal Cancer: Questions About Screening, Biology, and Treatment. Curr Treat Options Oncol. 2017;18:23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 156] [Article Influence: 19.5] [Reference Citation Analysis (1)] |
| 11. | Kirzin S, Marisa L, Guimbaud R, De Reynies A, Legrain M, Laurent-Puig P, Cordelier P, Pradère B, Bonnet D, Meggetto F, Portier G, Brousset P, Selves J. Sporadic early-onset colorectal cancer is a specific sub-type of cancer: a morphological, molecular and genetics study. PLoS One. 2014;9:e103159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 12. | Murphy CC, Singal AG, Baron JA, Sandler RS. Decrease in Incidence of Young-Onset Colorectal Cancer Before Recent Increase. Gastroenterology 2018; 155: 1716-1719. e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 13. | Cao Y, Wu K, Mehta R, Drew DA, Song M, Lochhead P, Nguyen LH, Izard J, Fuchs CS, Garrett WS, Huttenhower C, Ogino S, Giovannucci EL, Chan AT. Long-term use of antibiotics and risk of colorectal adenoma. Gut. 2018;67:672-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 99] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 14. | Dik VK, van Oijen MG, Smeets HM, Siersema PD. Frequent Use of Antibiotics Is Associated with Colorectal Cancer Risk: Results of a Nested Case-Control Study. Dig Dis Sci. 2016;61:255-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 15. | Casavale KO, Stoody EE, Rihane C, Olson R. Recommendations of the 2015-2020 Dietary Guidelines for Americans. Faseb J. 2016;30:423. [DOI] [Full Text] |
| 16. | Virostko J, Capasso A, Yankeelov TE, Goodgame B. Recent trends in the age at diagnosis of colorectal cancer in the US National Cancer Data Base, 2004-2015. Cancer. 2019;125:3828-3835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 17. | Myers EA, Feingold DL, Forde KA, Arnell T, Jang JH, Whelan RL. Colorectal cancer in patients under 50 years of age: a retrospective analysis of two institutions' experience. World J Gastroenterol. 2013;19:5651-5657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 104] [Cited by in RCA: 128] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 18. | Birkett RT, Chamely E, Concors SJ, Bleier JI, Aarons CB, Shanmugan S, Saur NM, Paulson EC. Overuse and Limited Benefit of Chemotherapy for Stage II Colon Cancer in Young Patients. Clin Colorectal Cancer. 2019;18:292-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Patel SG, Ahnen DJ. Colorectal Cancer in the Young. Curr Gastroenterol Rep. 2018;20:15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 20. | Scott RB, Rangel LE, Osler TM, Hyman NH. Rectal cancer in patients under the age of 50 years: the delayed diagnosis. Am J Surg. 2016;211:1014-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 21. | Lu XQ, Li Y, Wang W, Feng WT, Shi OM, Wang Q. International incidence trends in early- and late-onset colorectal cancer: a population-based study. Int J Colorectal Dis. 2020;35:1077-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Lui RN, Tsoi KKF, Ho JMW, Lo CM, Chan FCH, Kyaw MH, Sung JJY. Global Increasing Incidence of Young-Onset Colorectal Cancer Across 5 Continents: A Joinpoint Regression Analysis of 1,922,167 Cases. Cancer Epidemiol Biomarkers Prev. 2019;28:1275-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 23. | Araghi M, Soerjomataram I, Bardot A, Ferlay J, Cabasag CJ, Morrison DS, De P, Tervonen H, Walsh PM, Bucher O, Engholm G, Jackson C, McClure C, Woods RR, Saint-Jacques N, Morgan E, Ransom D, Thursfield V, Møller B, Leonfellner S, Guren MG, Bray F, Arnold M. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol. 2019;4:511-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 294] [Article Influence: 49.0] [Reference Citation Analysis (1)] |
| 24. | Overholt BF, Brooks-Belli L, Grace MG, Rankin K, Harrell R, Turyk M, Rosenberg FB, Barish RW, Gilinsky NH; Benchmark Colonoscopy Group. Evaluating screening age for colonoscopy: a quality assurance assessment. J Clin Gastroenterol. 2010;44:e147-e153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, Etzioni R, McKenna MT, Oeffinger KC, Shih YT, Walter LC, Andrews KS, Brawley OW, Brooks D, Fedewa SA, Manassaram-Baptiste D, Siegel RL, Wender RC, Smith RA. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 945] [Cited by in RCA: 1315] [Article Influence: 187.9] [Reference Citation Analysis (0)] |
| 26. | European Colorectal Cancer Screening Guidelines Working Group, von Karsa L, Patnick J, Segnan N, Atkin W, Halloran S, Lansdorp-Vogelaar I, Malila N, Minozzi S, Moss S, Quirke P, Steele RJ, Vieth M, Aabakken L, Altenhofen L, Ancelle-Park R, Antoljak N, Anttila A, Armaroli P, Arrossi S, Austoker J, Banzi R, Bellisario C, Blom J, Brenner H, Bretthauer M, Camargo Cancela M, Costamagna G, Cuzick J, Dai M, Daniel J, Dekker E, Delicata N, Ducarroz S, Erfkamp H, Espinàs JA, Faivre J, Faulds Wood L, Flugelman A, Frkovic-Grazio S, Geller B, Giordano L, Grazzini G, Green J, Hamashima C, Herrmann C, Hewitson P, Hoff G, Holten I, Jover R, Kaminski MF, Kuipers EJ, Kurtinaitis J, Lambert R, Launoy G, Lee W, Leicester R, Leja M, Lieberman D, Lignini T, Lucas E, Lynge E, Mádai S, Marinho J, Maučec Zakotnik J, Minoli G, Monk C, Morais A, Muwonge R, Nadel M, Neamtiu L, Peris Tuser M, Pignone M, Pox C, Primic-Zakelj M, Psaila J, Rabeneck L, Ransohoff D, Rasmussen M, Regula J, Ren J, Rennert G, Rey J, Riddell RH, Risio M, Rodrigues V, Saito H, Sauvaget C, Scharpantgen A, Schmiegel W, Senore C, Siddiqi M, Sighoko D, Smith R, Smith S, Suchanek S, Suonio E, Tong W, Törnberg S, Van Cutsem E, Vignatelli L, Villain P, Voti L, Watanabe H, Watson J, Winawer S, Young G, Zaksas V, Zappa M, Valori R. European guidelines for quality assurance in colorectal cancer screening and diagnosis: overview and introduction to the full supplement publication. Endoscopy. 2013;45:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 204] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 27. | Goldvaser H, Purim O, Kundel Y, Shepshelovich D, Shochat T, Shemesh-Bar L, Sulkes A, Brenner B. Colorectal cancer in young patients: is it a distinct clinical entity? Int J Clin Oncol. 2016;21:684-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6773] [Cited by in RCA: 6674] [Article Influence: 513.4] [Reference Citation Analysis (0)] |
| 29. | Sadler TW, Langman J. Langman's medical embryology. 12th ed. Philadelphia: Wolters Kluwer, 2012: 208-231. |
| 30. | Yantiss RK, Goodarzi M, Zhou XK, Rennert H, Pirog EC, Banner BF, Chen YT. Clinical, pathologic, and molecular features of early-onset colorectal carcinoma. Am J Surg Pathol. 2009;33:572-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 31. | Schellerer VS, Merkel S, Schumann SC, Schlabrakowski A, Förtsch T, Schildberg C, Hohenberger W, Croner RS. Despite aggressive histopathology survival is not impaired in young patients with colorectal cancer : CRC in patients under 50 years of age. Int J Colorectal Dis. 2012;27:71-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 32. | O'Connell JB, Maggard MA, Livingston EH, Yo CK. Colorectal cancer in the young. Am J Surg. 2004;187:343-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 254] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 33. | Law JH, Koh FH, Tan KK. Young colorectal cancer patients often present too late. Int J Colorectal Dis. 2017;32:1165-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 34. | Yun SO, Cho YB, Lee WY, Kim HC, Yun SH, Park YA, Huh JW. Clinical Significance of Signet-Ring-Cell Colorectal Cancer as a Prognostic Factor. Ann Coloproctol. 2017;33:232-238. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Steele SR, Park GE, Johnson EK, Martin MJ, Stojadinovic A, Maykel JA, Causey MW. The impact of age on colorectal cancer incidence, treatment, and outcomes in an equal-access health care system. Dis Colon Rectum. 2014;57:303-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 36. | Pearlman R, Frankel WL, Swanson B, Zhao W, Yilmaz A, Miller K, Bacher J, Bigley C, Nelsen L, Goodfellow PJ, Goldberg RM, Paskett E, Shields PG, Freudenheim JL, Stanich PP, Lattimer I, Arnold M, Liyanarachchi S, Kalady M, Heald B, Greenwood C, Paquette I, Prues M, Draper DJ, Lindeman C, Kuebler JP, Reynolds K, Brell JM, Shaper AA, Mahesh S, Buie N, Weeman K, Shine K, Haut M, Edwards J, Bastola S, Wickham K, Khanduja KS, Zacks R, Pritchard CC, Shirts BH, Jacobson A, Allen B, de la Chapelle A, Hampel H; Ohio Colorectal Cancer Prevention Initiative Study Group. Prevalence and Spectrum of Germline Cancer Susceptibility Gene Mutations Among Patients With Early-Onset Colorectal Cancer. JAMA Oncol. 2017;3:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 517] [Article Influence: 64.6] [Reference Citation Analysis (0)] |
| 37. | Watson R, Liu TC, Ruzinova MB. High frequency of KRAS mutation in early onset colorectal adenocarcinoma: implications for pathogenesis. Hum Pathol. 2016;56:163-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 38. | Mauri G, Sartore-Bianchi A, Russo AG, Marsoni S, Bardelli A, Siena S. Early-onset colorectal cancer in young individuals. Mol Oncol. 2019;13:109-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 196] [Cited by in RCA: 409] [Article Influence: 58.4] [Reference Citation Analysis (0)] |
| 39. | Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2895] [Cited by in RCA: 2951] [Article Influence: 210.8] [Reference Citation Analysis (0)] |
| 40. | Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K; International Agency for Research on Cancer Handbook Working Group. Body Fatness and Cancer--Viewpoint of the IARC Working Group. N Engl J Med. 2016;375:794-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2163] [Cited by in RCA: 2425] [Article Influence: 269.4] [Reference Citation Analysis (0)] |
| 41. | Cani PD, Jordan BF. Gut microbiota-mediated inflammation in obesity: a link with gastrointestinal cancer. Nat Rev Gastroenterol Hepatol. 2018;15:671-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 277] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 42. | Frezza EE, Wachtel MS, Chiriva-Internati M. Influence of obesity on the risk of developing colon cancer. Gut. 2006;55:285-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 242] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 43. | Farinetti A, Zurlo V, Manenti A, Coppi F, Mattioli AV. Mediterranean diet and colorectal cancer: A systematic review. Nutrition. 2017;43-44:83-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 106] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 44. | Larsson SC, Wolk A. Meat consumption and risk of colorectal cancer: a meta-analysis of prospective studies. Int J Cancer. 2006;119:2657-2664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 390] [Article Influence: 20.5] [Reference Citation Analysis (1)] |
| 45. | Sierra MS, Forman D. Burden of colorectal cancer in Central and South America. Cancer Epidemiol. 2016;44 Suppl 1:S74-S81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 46. | Willett WC, Stampfer MJ, Colditz GA, Rosner BA, Speizer FE. Relation of meat, fat, and fiber intake to the risk of colon cancer in a prospective study among women. N Engl J Med. 1990;323:1664-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 840] [Cited by in RCA: 722] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 47. | Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149:659-669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 449] [Cited by in RCA: 439] [Article Influence: 25.8] [Reference Citation Analysis (0)] |