Copyright
©The Author(s) 2025.
World J Gastrointest Surg. Feb 27, 2025; 17(2): 97862
Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.97862
Published online Feb 27, 2025. doi: 10.4240/wjgs.v17.i2.97862
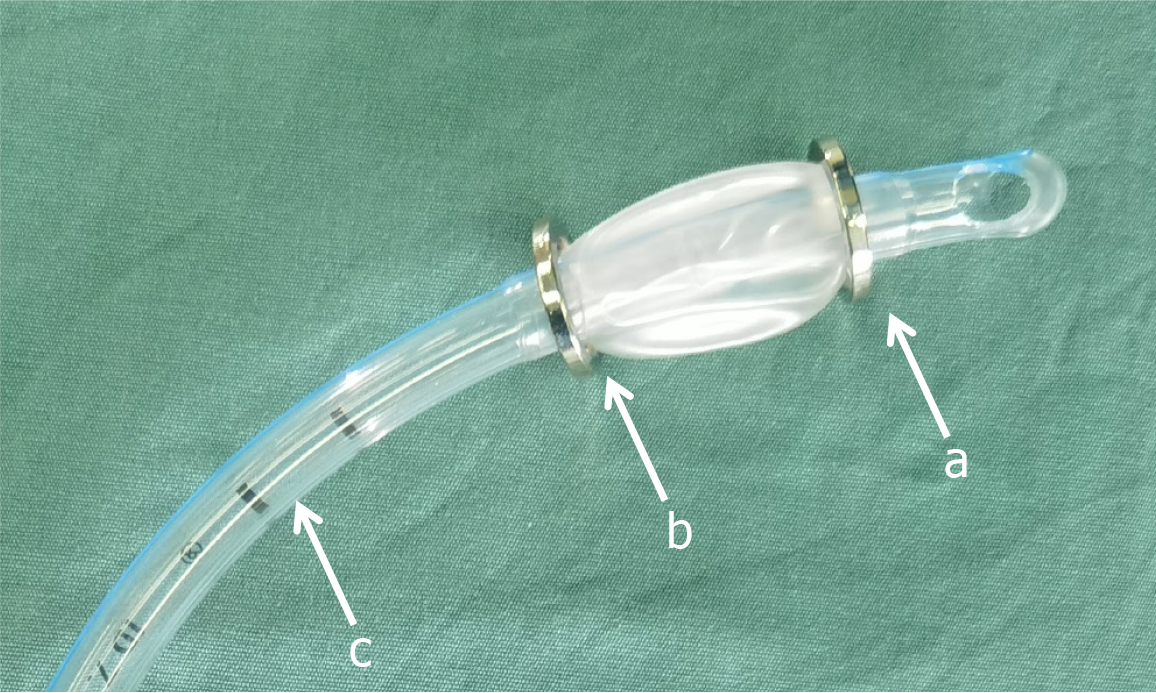
Figure 1 Magnetic device used for the rectal reconstruction.
a: The cephalad magnetic ring; b: The caudal magnetic ring; c: The tracheal tube.
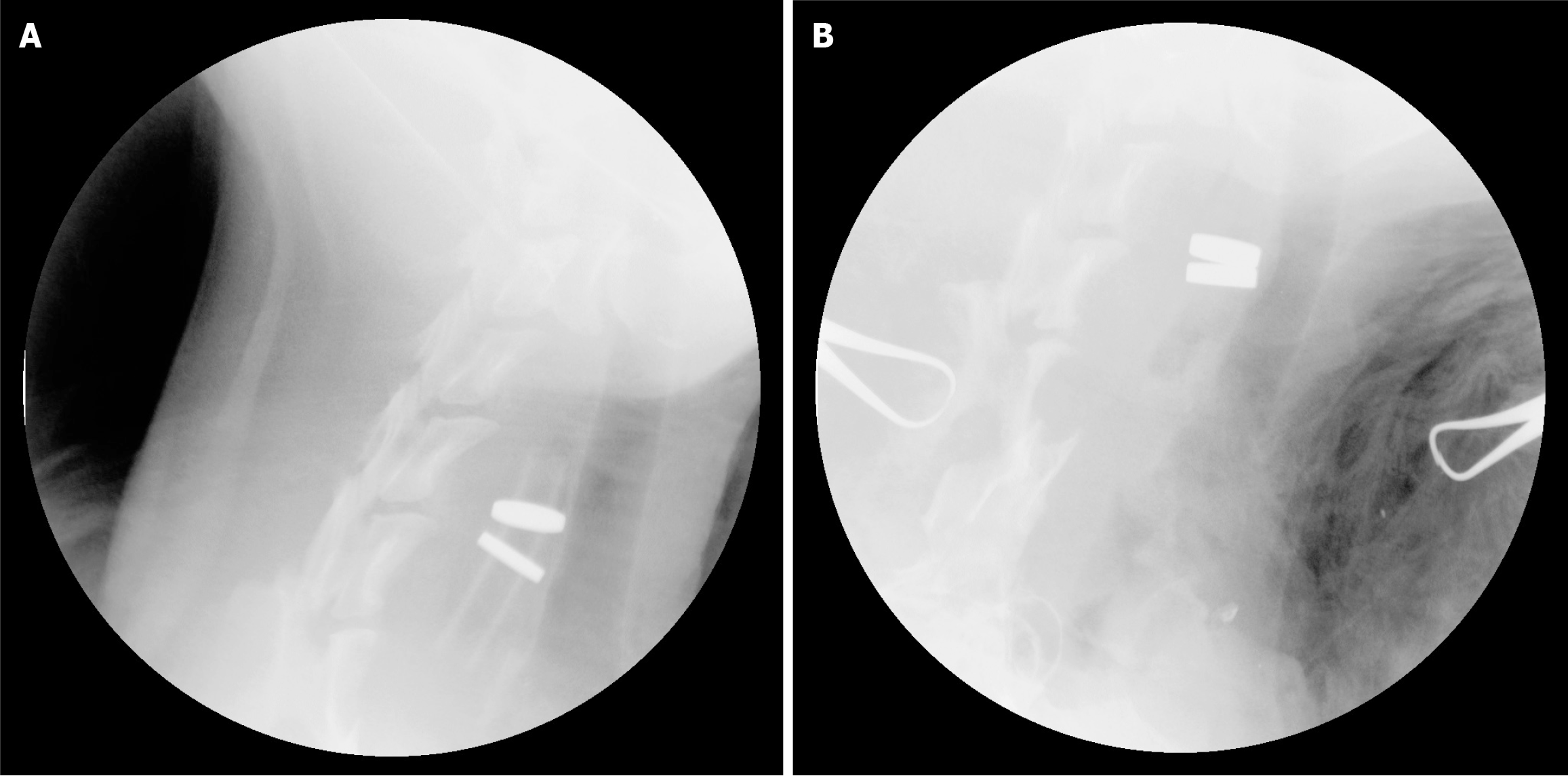
Figure 2 Plain film examination during the operation.
A: The tracheal tube was not removed after the magnets were coupled; B: Magnamosis was completed after the removal of the tracheal tube.
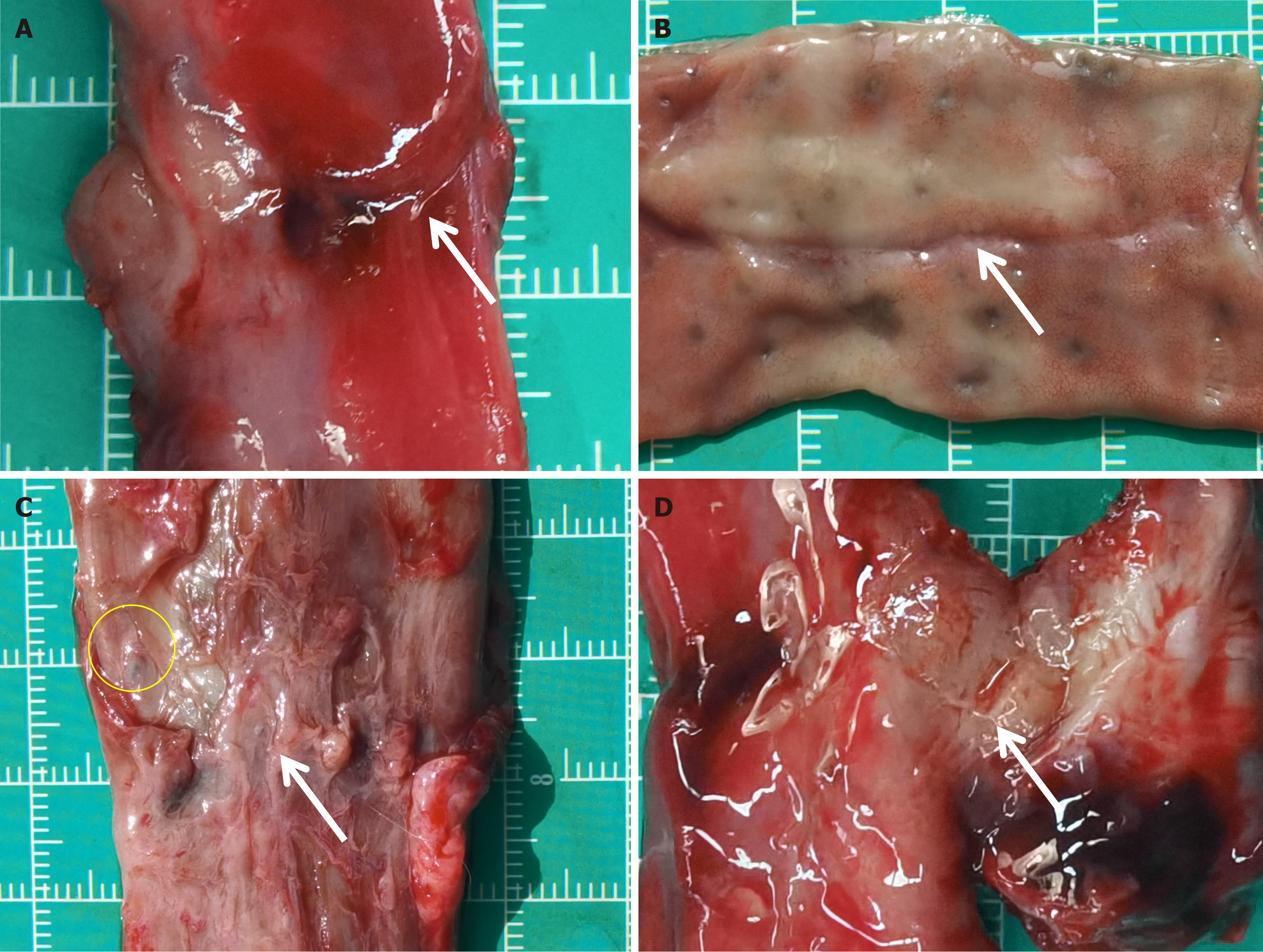
Figure 3 Gross observation of the anastomosis specimens.
A and B: The rectal anastomosis in the magnamosis group; C and D: The rectal anastomosis in the suturing anastomosis group. The white arrows indicate the anastomosis. The yellow circle shows the absorbable suture.
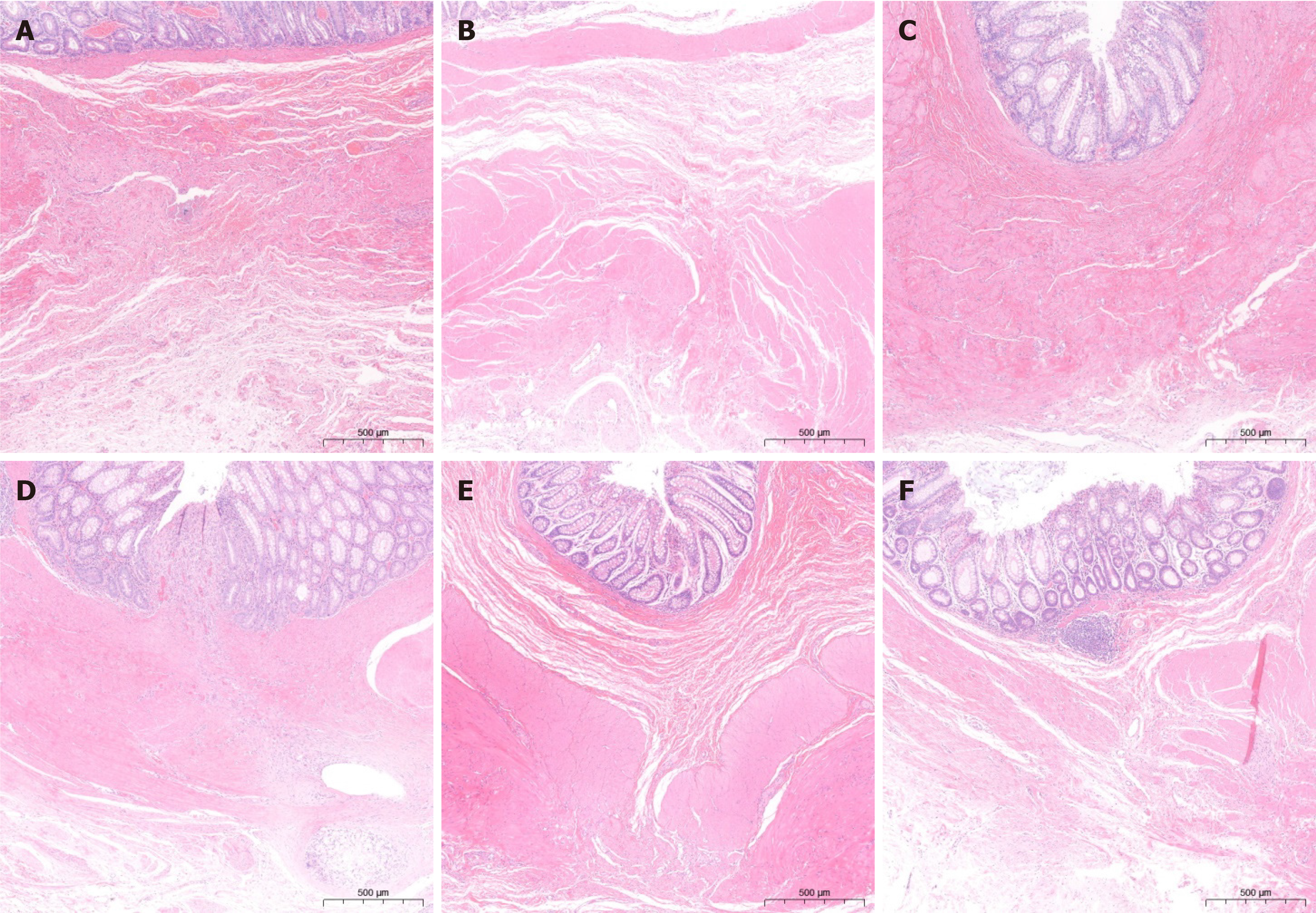
Figure 4 HE staining of the anastomosis specimens.
A: At one month after surgery, the anastomosis of the magnamosis group demonstrated an intact mucosa with minor inflammatory reactions and inadequate submucosal continuity; B: At 1-month postoperatively, the anastomosis of the suturing group showed a lack of mucosal and submucosal continuity, along with an increased inflammatory response; C: The anastomosis of the magnamosis group at 3 months postoperatively obviously improved; D: The anastomosis of the suturing anastomosis group at 3 months postoperatively also healed well, but the inflammatory responses remained; E: The anastomosis of the magnamosis group at 6 months postoperatively showed no inflammatory responses and well healing; F: The anastomosis of the suturing anastomosis group at 6 months postoperatively.
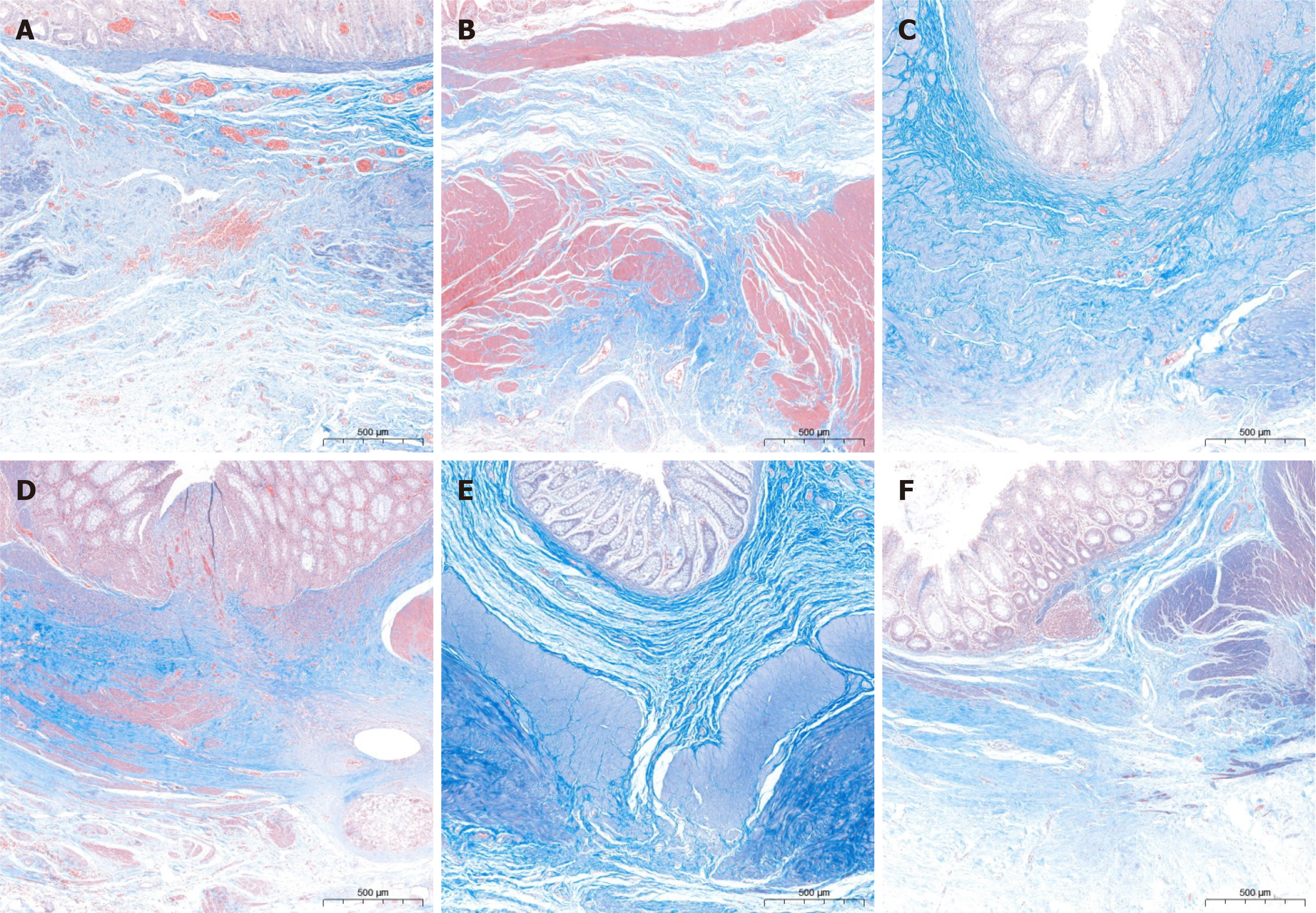
Figure 5 Masson staining of the anastomosis specimens.
A: At one month after the operation, the anastomosis of the magnamosis group exhibited an intact mucosa; however, the submucosal and muscular continuity were subpar; B: The anastomosis of the suturing anastomosis group at 1 month postoperatively showed poor mucosal, submucosal and muscular continuity with disorganized fiber arrangement; C: The anastomosis of the magnamosis group at 3 months postoperatively showed good fiber arrangement; D: The anastomosis of the suturing anastomosis group at 3 months postoperatively. The submucosal fiber arrangement was improved, but the muscular layer was separated; E: The anastomosis of the magnamosis group at 6 months postoperatively showed that the fiber arrangement was accurate; F: The anastomosis of the suturing anastomosis group at 6 months postoperatively. The submucosal fiber arrangement healed well without continuous muscular layer.
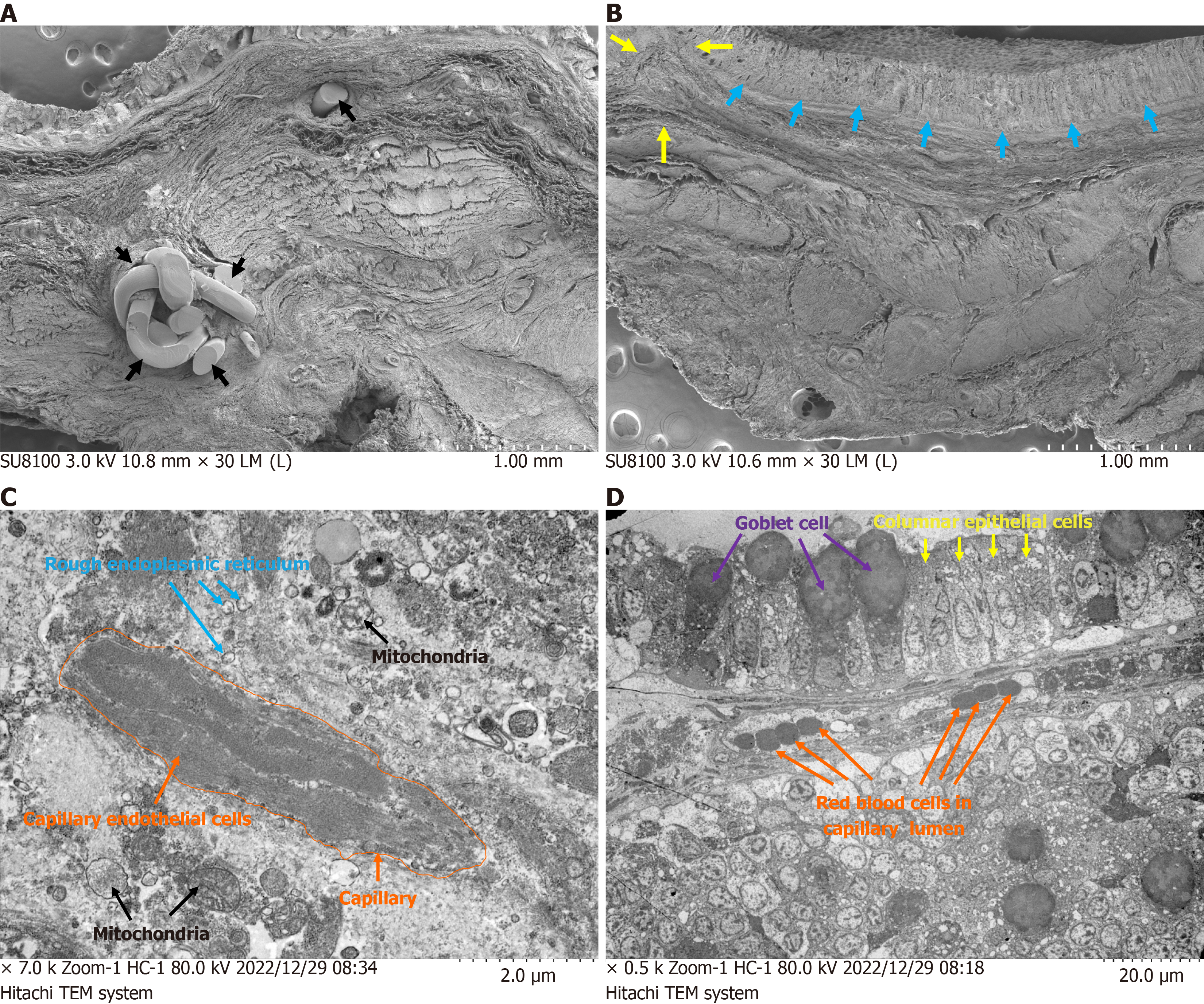
Figure 6 Scanning transmission electron microscopic results of the anastomosis specimens at 3 months postoperatively.
A: Scanning transmission electron microscopic image for the suture group. The suture foreign body remained in the anastomotic tissue (black arrows). The anastomotic structure was disordered with obvious scar hyperplasia; B: Scanning transmission electron microscopic image for the anastomosis group. The anastomosis stoma were smooth without any foreign body in the anastomotic tissue (yellow arrows) and columnar epithelial cells were arranged neatly at the anastomosis (cyan arrows); C: Scanning transmission electron microscopic image for the suture group. The endothelial cells in the anastomotic capillaries suffered serious structural damage. The nucleus displayed a greater number of heterochromatin edge sets, while the cytoplasm appeared more uniform with a decrease in the number of organelles (orange arrows). The mitochondria and intramembrane appeared slightly swollen; D: The scanning transmission electron microscope analysis of the magnamosis group revealed normal mucosal structure of the anastomosis, abundant mucus particles in the goblet cells, and tightly bound intercellular junctions. No obvious inflammatory cell infiltration was observed in the mucosa and submucosa.
- Citation: Liu SQ, Zhang HK, Lv Y, Xu XH, Li YF, Quan DW. Magnamosis for rectal reconstruction in canines. World J Gastrointest Surg 2025; 17(2): 97862
- URL: https://www.wjgnet.com/1948-9366/full/v17/i2/97862.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i2.97862