Copyright
©The Author(s) 2022.
World J Gastrointest Surg. Feb 27, 2022; 14(2): 78-106
Published online Feb 27, 2022. doi: 10.4240/wjgs.v14.i2.78
Published online Feb 27, 2022. doi: 10.4240/wjgs.v14.i2.78
Figure 1 Elettra Merola, MD, PhD, Department of Gastroenterology, Santa Chiara Hospital, Azienda Provinciale per i Servizi Sanitari (APSS), Largo Medaglie D’Oro 9, Trento 38122, Italy
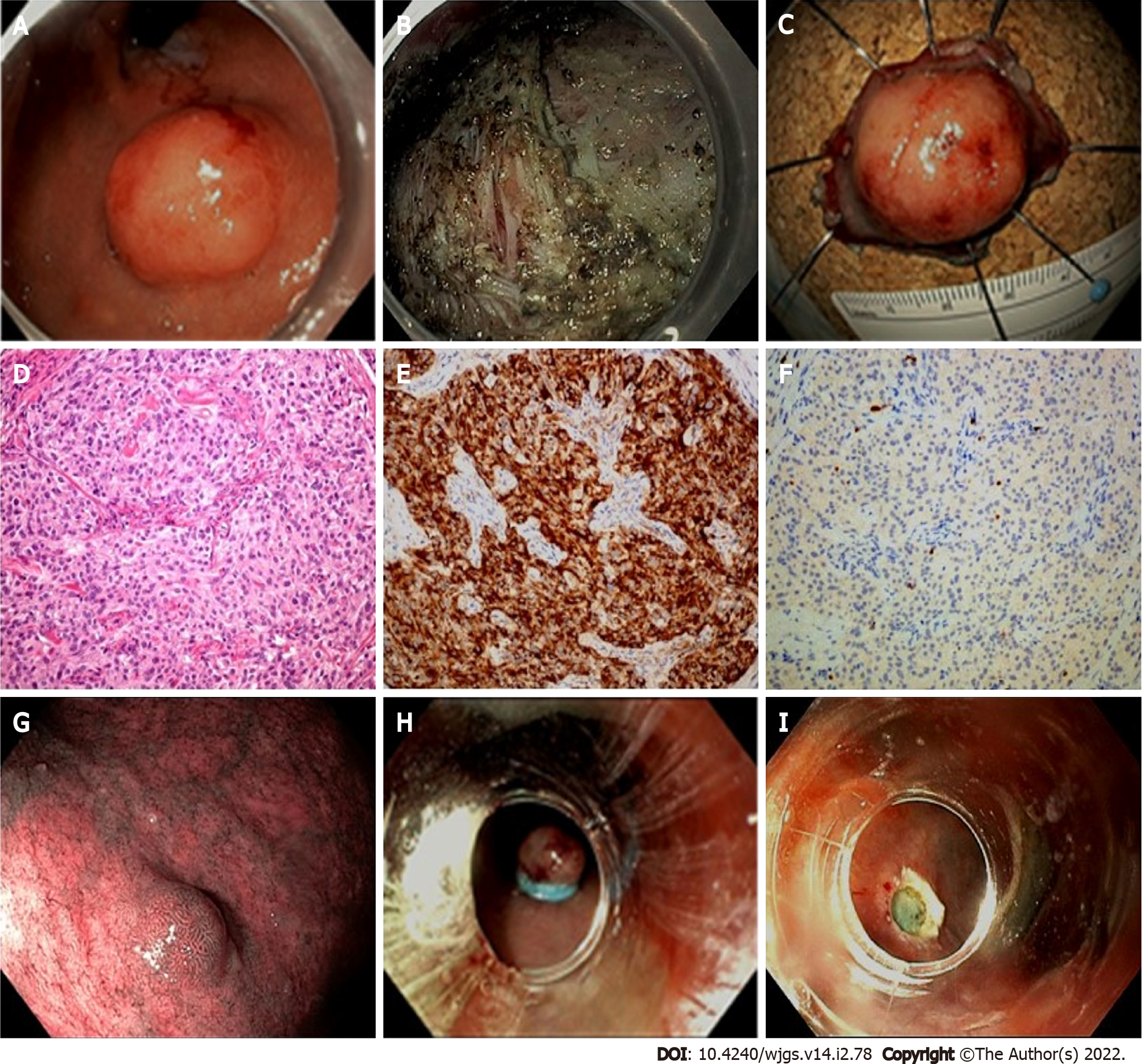
Figure 2 Endoscopic management of gastric neuroendocrine tumors presentation of a clinical case referred to our hospital.
A 78-year-old female patient was referred to our Endoscopy Unit for resection of a lesion of the gastric fundus. Staging by endoscopic ultrasound showed hypoechoic lesion of 19 mm × 12 mm, with well-defined margins, originating from the third hyperechoic layer. Fine-needle cytology diagnosed a NET G1 (Ki67 < 2%). The lesion was then resected by endoscopic submucosa dissection (ESD). Histological evaluation described a gastric NET (g-NET) G1, associated with autoimmune gastritis (Type I). During follow-up, another minor lesion (< 10 mm) suspected for NET was reported along the greater curvature, and resected by Band-ligation endoscopic mucosal resection (EMR-L). Histological report confirmed a Type I g-NET. A: Cardial area reflexed view; B: Resection base after ESD; C: Oriented and pinned specimen; D: Hematoxylin-eosin stain showing monomorphic cells in a nested architecture without necrosis; E: Corresponding Chromogranin A immunostain (20 × magnification); F: Corresponding Ki67 immunostain (20 × magnification); G: Endoscopic appearance of the lesion detected during follow-up; H: EMR-L: Rubber band release; I: Resection base after EMR-L.
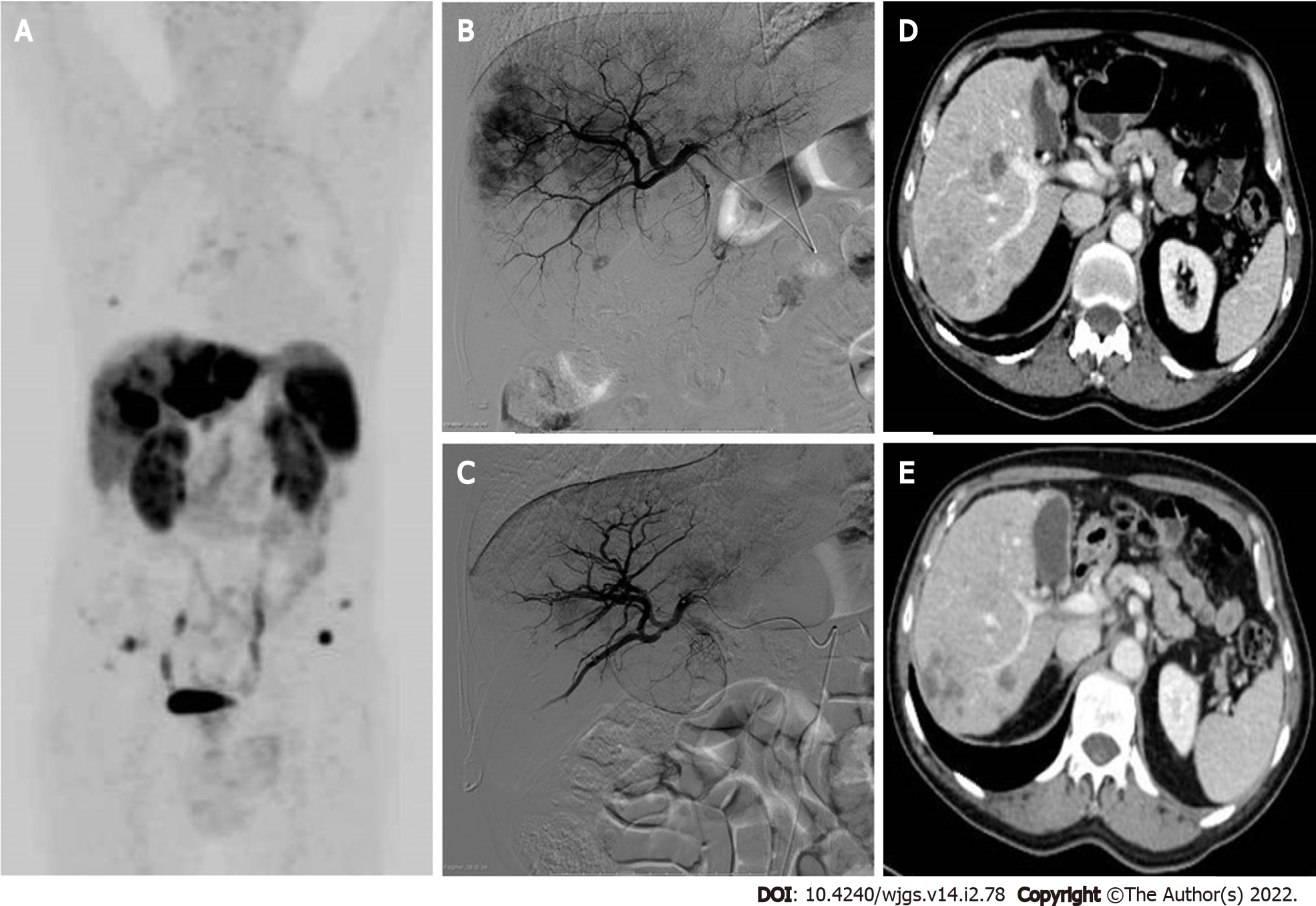
Figure 3 Locoregional treatments for neuroendocrine liver metastases-presentation of a clinical case referred to our hospital, with progressive liver disease after multiple systemic treatments.
A: 68Ga-DOTATOC-positron emission tomography/computed tomography (CT) whole-body maximum intensity projection image reveals multiple liver metastases involving both hepatic lobes, the left lobe being almost completely replaced by tumor. Bone and lymph nodal small metastases are also evident; B: Selective angiography of the right hepatic artery performed before lobar chemoembolization shows multiple hypervascular liver lesions; C: Selective angiography of the right hepatic artery performed 1 mo after two sessions of degradable starch microsphere transarterial chemoembolization (DSM-TACE). A marked reduction of the liver metastases enhancement is visible, preserved patency of the arterial intra-hepatic branches; D: Portal-phase CT scan before arterial chemoembolization: Multiple confluent hypodense lesions compared to liver parenchyma are detected in the right liver lobe; E: Portal-phase CT scan control after two DSM-TACE: Partial response of the liber metastases, which appear reduced in size and without contrast enhancement. Right portal vein branch narrowing represents an initial sign of liver/biliary toxicity.
- Citation: Merola E, Michielan A, Rozzanigo U, Erini M, Sferrazza S, Marcucci S, Sartori C, Trentin C, de Pretis G, Chierichetti F. Therapeutic strategies for gastroenteropancreatic neuroendocrine neoplasms: State-of-the-art and future perspectives. World J Gastrointest Surg 2022; 14(2): 78-106
- URL: https://www.wjgnet.com/1948-9366/full/v14/i2/78.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i2.78