INTRODUCTION
Diabetic retinopathy (DR) is a leading cause of vision loss in the working-age population and one of the most common and serious microvascular complications of diabetes mellitus. The estimated prevalence of DR exceeds 40% after 5 years of diabetes onset, further increasing to 87% after > 20 years[1]. The International Clinical Classification Criteria classifies DR into the following five stages based on the increasing risk of retinopathy: (1) Stage 1, characterized by the absence of apparent DR; (2) Stage 2, defined as mild non-proliferative DR (NPDR) with only microaneurysms; (3) Stage 3, moderate NPDR between mild and severe NPDR; (4) Stage 4, severe NPDR, encompassing lesions that adhere to the “4:2:1 principle”; and (5) Stage 5, proliferative DR (PDR), which encompasses all lesions that display clear neovascularization[2]. The development of DR lesions in the macula can result in varying degrees of vision loss[3]. DR is a multifactorial disease with a complex pathogenesis, with inflammation, persistent hyperglycemia, angiogenesis, apoptosis, and advanced glycosylation end products as its primary pathogenic mechanisms. However, at present, the role of oxidative stress and the interactions between these factors remain unclear[4,5].
At present, clinical strategies for the treatment of DR focus mainly on the modes of drugs, lasers, and surgery. In fact, intravitreal anti-vascular endothelial growth factor (VEGF) drugs have emerged as the first line of treatment for severe NPDR and PDR[6]. However, these treatments have limitations and complications. Owing to the need for frequent injections, financial burden, and poor patient compliance, the use of anti-VEGF drugs is limited[7]. Furthermore, frequent intravitreal injections of anti-VEGF drugs, such as ranibizumab and bevacizumab, can have adverse effects, such as endophthalmitis and traumatic cataracts[8], while laser and surgical treatments can lead to uveitis and worsening macular edema[9]. Therefore, there is a need to identify new anti-DR drugs or complementary and alternative therapies with improved efficacy and fewer adverse effects.
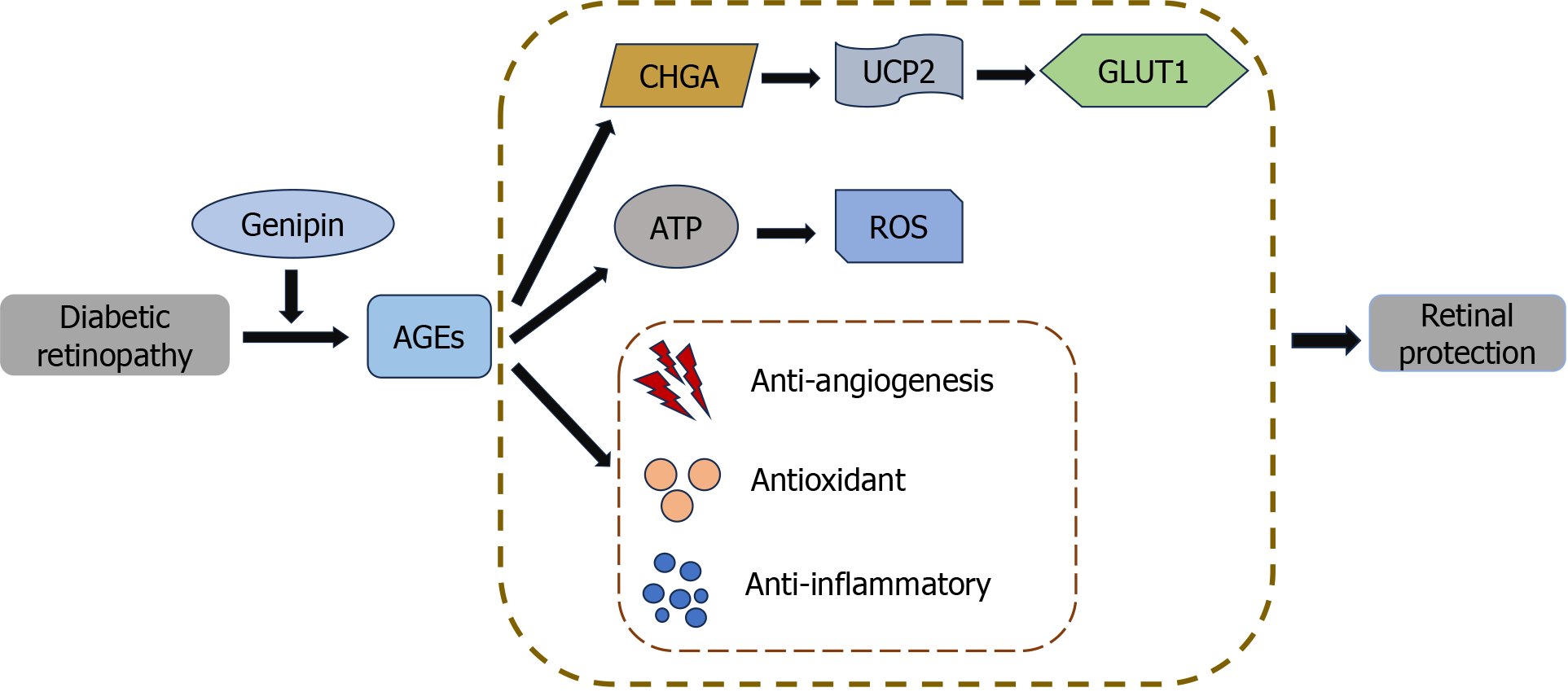
Genipin, a traditional Chinese medicine (TCM) that is isolated from the fruits of Gardenia jasminoides, has been extensively studied for its antidiabetic and neuroprotective activities[10]. Sun et al[11], in 2023, in their study, have provided new insights into the molecular dynamics and therapeutic modalities of the potential effects of genipin on diabetic microangiopathy. Their findings indicated that the intravitreal injection of genipin protects the retina of diabetic mice from high-glucose-induced damage in vivo. Furthermore, the CHGA/UCP2/glucose transporter protein 1 signaling pathway plays an important role in this process. In addition, in vitro studies support these findings, indicating that genipin reverses AGE-induced cell proliferation and apoptotic damage in vitro, while reducing high glucose-induced energy metabolism, oxidative stress, and inflammatory damage. Based on these experimental findings, the authors propose that regulating advanced glycosylation through intraocular injection of genipin may be a potential strategy to mitigate severe retinopathy and prevent vision loss (Figure 1).
Figure 1 The retinal protection mechanism of genipin.
AGEs: Advanced glycation end products; CHGA: Chromogranin-A; UCP2: Uncoupling protein 2; GLUT1: Glucose transporters type 1; ATP: Adenosine-triphosphate; ROS: Reactive oxygen species.
APPLICATION OF TRADITIONAL CHINESE MEDICINE IN DIABETES RETINOPATHY
The prevention and treatment of DR using TCM has recently gained considerable attention in research on fundus diseases. The active ingredients of TCM, which are derived by activating blood circulation, removing blood stasis, tonifying qi, and nourishing blood, have significant antioxidant, anti-inflammatory, anti-apoptotic, and other pharmacological effects that can block DR progression through various mechanisms[12]. Chinese medicine has amassed a substantial body of clinical evidence and research data for the prevention and treatment of DR. Many TCM extracts have been extensively studied in this context. Polyphenolic compounds, such as curcumin, puerarin, and resveratrol prevent and treat DR through various mechanisms. Additionally, herbal single-drug extracts, including Fructus arctii, Dendrobium, Scutellaria, Gypenoside, and Radix trichosanthis, are commonly utilized in research on diseases associated with diabetes-related vascular complications[13].
Among these drugs, curcumin, puerarin, Fructus arctii, and resveratrol have been used in animal experiments and in vitro studies. They regulate various pathogenic mechanisms of DR and inhibit its progression. This provides an experimental foundation for their potential clinical use in treating DR. For instance, curcumin treatment decreases leukocyte adhesion and vascular leakage in the retinas of diabetic rats and reduces the expression of pro-inflammatory mediators in retinal tissues. Furthermore, curcumin regulates VEGF-mediated angiogenesis and improves glucose and lipid metabolism[14]. In addition to its anti-inflammatory and anti-angiogenic effects, puerarin treatment reduces the expression of Bax and caspase-3 and inhibits the production of reactive oxygen species, as well as NMDA-induced iNOS and nNOS release, reflecting its anti-apoptotic and anti-oxidative stress capacity[15]. Resveratrol has been experimentally demonstrated to exert antioxidant effects by increasing the levels of naturally occurring antioxidants, enzymes, and molecular defenses in various cell types in the eye. In addition, resveratrol exerts an anti-VEGF effect and inhibits the proliferation and migration of vascular endothelial cells, exerting a combined anti-PDR effect[16].
TCM treatment for DR has demonstrated certain advantages. Previous studies have elucidated the molecular mechanisms and potential of TCM against DR from the perspective of signaling pathways. The results showed that the key signaling pathways of TCM for the treatment of DR include anti-inflammatory, anti-angiogenic, and anti-oxidative stress-based pathways, such as NF-κB, MAPK/NF-κB, TLR4/NF-κB, VEGF/VEGFR2, HIF-1α/VEGF, STAT3, and Nrf2/HO-1. Relevant Chinese medicines can regulate the interactions between signaling pathways through multitarget synergistic effects to inhibit DR progression. Many herbal medicines counteract DR by affecting various pathological processes. For example, curcumin can inhibit retinal inflammation via the p38 MAPK/NF-κB signaling pathway and angiogenesis via the VEGF/VEGFR2 signaling pathway, thereby exerting beneficial effects on DR[17]. Considering the complexity of the pathological mechanisms of DR, multi-component, multi-target, and multi-pathway Chinese medicines are promising drug candidates for the treatment of DR. However, a lack of documentation on the corresponding side effects is a major limitation of TCM therapeutic studies in relation to DR. With the increasing popularity of herbal medicines, their side effects have become more common. For example, some animal studies have indicated that the mega-dose administration of curcumin causes a decrease in testosterone levels and may affect reproductive function[18]. Wang et al[19] reported 33 cases of hemolytic reactions due to puerarin injection. These findings highlight the need to collate and analyze the adverse effects of TCM treatment, implement appropriate control measures, and leverage its pleiotropic effects to identify TCM as a promising candidate for the prevention and treatment of eye diseases.
However, at present, the majority of TCM treatments are administered orally, and the use of intraocular injections remains rare[14]. With substantial advances in macromolecular biologics for ophthalmic purposes, vitreous cavity injections have become a crucial treatment option for a broad range of fundus diseases. Patients with diabetes often have various underlying diseases and require various systemic medications[20]. Topical ocular medications can reduce the systemic drug burden in patients, especially their impact on liver and kidney functions. In their article, the authors propose an innovative conclusion: Controlling advanced glycation through the intraocular injection of genipin to mitigate severe retinopathy and prevent vision loss. However, this clinical application has room for improvement, including a need to enhance the drug transduction of genipin[12]. As such, a gap exists between the experimental and clinical applications.
SAFETY OF OPHTHALMIC INJECTIONS
In the pursuit of clinical efficacy, considerable attention should be paid to drug safety. In this respect, quality standards and standardized management operations for ophthalmic injections should be emphasized. The international quality standards for ophthalmic injections include pH, osmolality, molar concentration, and cytotoxicity. Among these factors, the special route of administration limits sterility, and the number of insoluble particles is a key factor affecting the quality standards of ophthalmic injections. Notably, owing to the physiological and anatomical characteristics of the ophthalmic site, its tolerance to particles may be lower. Therefore, the United States Pharmacopoeia has established more stringent standards for insoluble particles in ophthalmic injections than those for small-volume intravenous injections[21]. Monoclonal antibody injections have the characteristics of biological products. Biological and immunological methods must be applied to complete the identification and consistency analysis and to assess purity, impurities, potency, and other relevant factors. Moreover, conducting inspections for “substances related to TCM injection” and “residues of heavy metals and harmful elements” is mandatory for TCM formulations used as general injections.
At present, the available dosage forms of ophthalmic preparations in TCM are fewer than those of chemical medicines, particularly ophthalmic injections[22]. This could be attributed to the inherent complexity of TCM and the rigorous quality control standards for ophthalmic preparations. When developing drugs, in addition to ensuring that the original herbs meet legal standards, attention should be paid to the method of crushing the herbs and the particle size of the powder. In addition, the selection of additives, sterility checks, and eye irritation tests must be standardized and monitored. In addition to safety concerns, ensuring the quality of ophthalmic preparations requires consideration of the specific drug varieties used in clinical practice, and a comprehensive evaluation of raw materials, excipients, processes, and other factors. Nevertheless, certain critical considerations regarding ophthalmic preparations of TCM need to be addressed, including its maximum frequency of daily use, specifying indications, and evaluating efficacy by incorporating the unique characteristics of TCM ophthalmic preparations. We believe that the local application of TCM can be anticipated to emerge as a new trend and holds promise as an effective approach for the treatment of DR.
CONCLUSION
The intraocular injection of genipin to control advanced glycation may represent an effective strategy for the prevention of severe retinopathy and vision loss. More generally, the prevention and treatment of DR using TCM is gradually becoming an important focus in advancing research on fundus diseases. Given the stringent quality standards required for intraocular injectable drugs, conducting high-quality pilot studies is imperative. Comprehensive studies on topical intraocular injections of herbal medicines may also facilitate further advances in therapeutic approaches for the treatment of fundus diseases.
ACKNOWLEDGEMENTS
Anonymous reviewers provided helpful and constructive comments that greatly improved the manuscript. Finally, the National Natural Science Foundation of China, and the Scientific Research Project Foundation of Zhejiang Chinese Medical University provided funding for this work, for which I am deeply grateful.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Satapathy T S-Editor: Li L L-Editor: A P-Editor: Che XX