Copyright
©The Author(s) 2024.
World J Diabetes. Jun 15, 2024; 15(6): 1162-1177
Published online Jun 15, 2024. doi: 10.4239/wjd.v15.i6.1162
Published online Jun 15, 2024. doi: 10.4239/wjd.v15.i6.1162
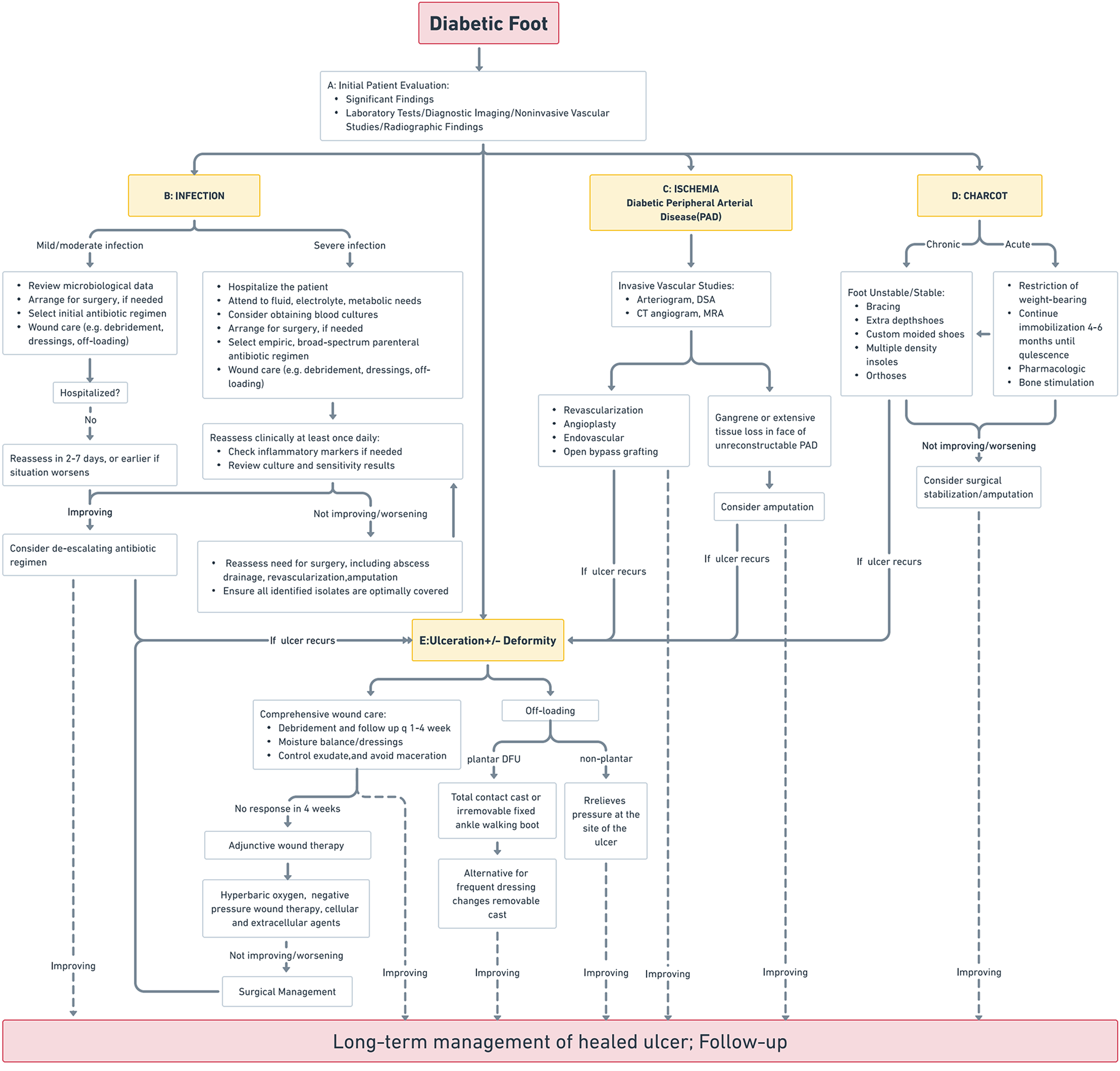
Figure 1 Standard clinical protocols for diabetic foot.
This figure illustrates a detailed algorithm for managing diabetic foot complications, with a focus on infection, ischemia resulting from peripheral arterial disease, and Charcot neuroarthropathy. A: Initial evaluation: Incorporates diagnostic testing and imaging to guide therapeutic decisions; B: Infection management: Encompasses a spectrum from antibiotic therapy and localized wound care to hospitalization for advanced cases. Surgical intervention is considered for non-responsive infections; C: Ischemia treatment: Strategies include revascularization and angioplasty, with amputation reserved for critical cases; D: Charcot neuroarthropathy management: Ranges from conservative orthopedic approaches to surgical correction, based on disease progression and treatment response; E: Ulceration and deformity management: Emphasizes comprehensive wound care, off-loading techniques, and surgical options when necessary. The decision-making process within the algorithm is dynamic, adjusting based on the ulcer’s response to treatment and incorporating adjunctive therapies such as hyperbaric oxygen or cellular and tissue-based products where appropriate.
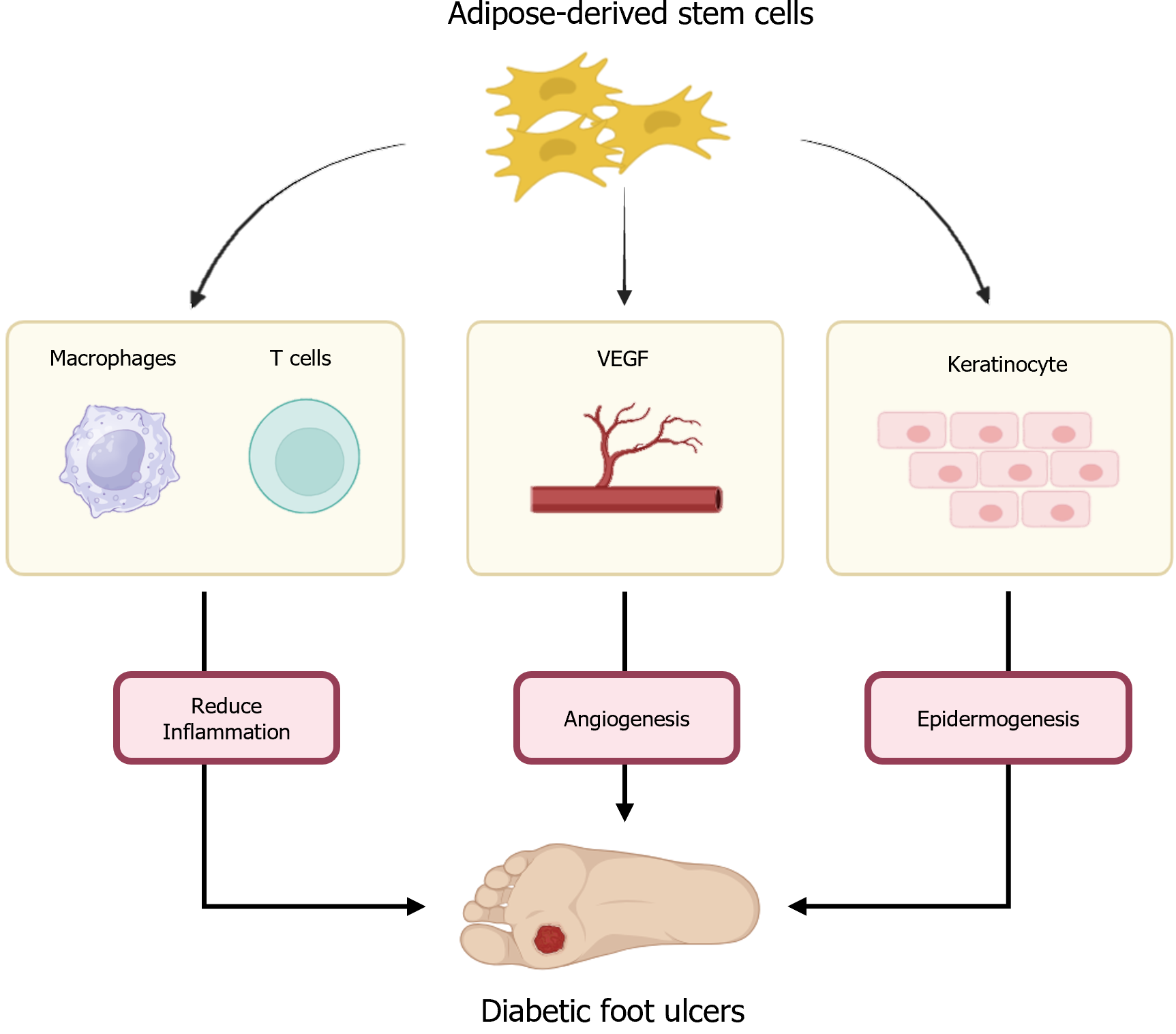
Figure 2 Therapeutic mechanisms of adipose-derived stem cells in diabetic foot Ulcer Healing.
This figure delineates the multifaceted role of adipose-derived stem cells in the healing process of diabetic foot ulcers, highlighting their interaction with various cellular and molecular pathways. This includes anti-inflammatory effects, promotion of angiogenesis, and facilitation of epidermal regeneration. VEGF: Vascular endothelial growth factor.
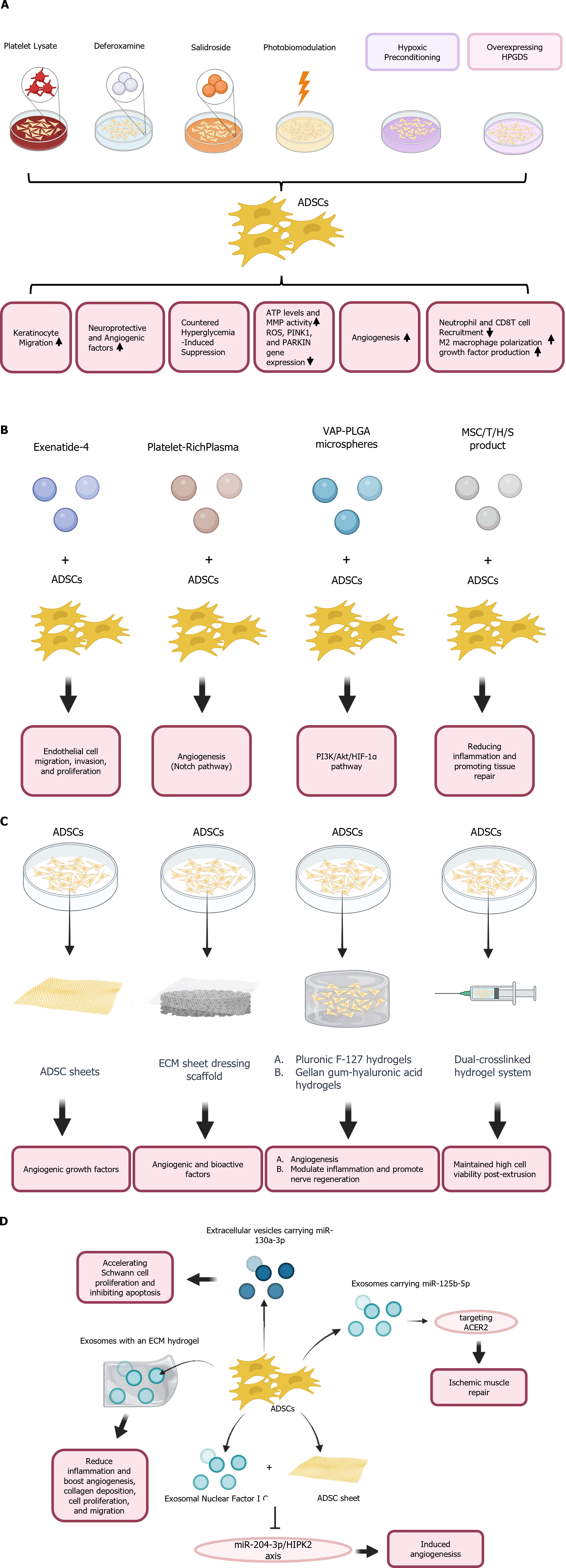
Figure 3 Multidimensional enhancement of adipose-derived stem cells for diabetic foot ulcer therapy.
This figure presents a comprehensive overview of various strategies employed to enhance the therapeutic properties of adipose-derived stem cells (ADSCs) for the treatment of diabetic foot ulcers. The strategies are categorized based on their primary mechanisms of action and delivery methods. A: Preconditioning strategies: Platelet lysate increases keratinocyte migration. Deferoxamine upregulates neuroprotective and angiogenic factors. Salidroside counters hyperglycemia-induced suppression. Photobiomodulation boosts ATP, ROS, and protective gene expressions. Hypoxic Preconditioning stimulates angiogenesis. Overexpressing HPGDS enhances immunomodulation and growth factor production; B: Combination therapies: Exenatide-4 and ADSCs promote endothelial migration and proliferation. Platelet-rich plasma combined with ADSCs enhances angiogenesis. VAP-PLGA microspheres with ADSCs activate the PI3K/Akt/HIF-1a pathway, aiding in cellular survival. MSC/T/H/S product reduces inflammation and promotes tissue repair; C: Biomaterials and bioactive molecule application: ECM sheets and hydrogels provide a scaffold for ADSCs, augmenting angiogenesis. Pluronic F-127 hydrogels deliver ADSCs, enhancing the modulation of nerve regeneration. Dual-crosslinked hydrogel systems ensure cell viability and sustained release of therapeutic factors; D: Exosome and gene therapy approaches: Exosomes with miR-133a-3p accelerate Schwann cell proliferation and inhibit apoptosis. Exosomes within an ECM hydrogel target the ACE2 receptor, aiding in ischemic tissue repair. Exosomal miR-126-5p improves vascular cell migration. Exosomal miR-204-3p/HPK2 axis enhances angiogenesis. These diverse strategies underscore the potential of ADSCs in improving the therapeutic outcomes for diabetic foot ulcers through a variety of mechanisms, including enhancing cell viability, modulating immune responses, and promoting angiogenesis and tissue regeneration. ADSCs: Adipose-derived stem cells; VAP-PLGA microspheres: Velvet antler polypeptide PLGA microspheres; MSCs: Mesenchymal stem cells.
- Citation: Tseng SL, Kang L, Li ZJ, Wang LQ, Li ZM, Li TH, Xiang JY, Huang JZ, Yu NZ, Long X. Adipose-derived stem cells in diabetic foot care: Bridging clinical trials and practical application. World J Diabetes 2024; 15(6): 1162-1177
- URL: https://www.wjgnet.com/1948-9358/full/v15/i6/1162.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i6.1162