Published online Mar 15, 2017. doi: 10.4251/wjgo.v9.i3.129
Peer-review started: November 14, 2016
First decision: December 13, 2016
Revised: December 29, 2016
Accepted: February 8, 2017
Article in press: February 9, 2017
Published online: March 15, 2017
Processing time: 115 Days and 12.8 Hours
Adenocarcinoma of the lung infrequently metastasizes to the gastrointestinal tract. We report a rare case of a 65-year-old male with no respiratory symptoms diagnosed with adenocarcinoma of the lung by histopathological examination of metastatic sites which included an ulcer in the gastric body and a mass in the rectum. Metastatic disease also involved the liver as well. Patient was treated with systemic chemotherapy but unfortunately expired five months after the diagnosis was made.
Core tip: It is an extremely uncommon finding to discover lung cancer on gastric ulcer and rectal mass biopsy. Also, this patient did not have a pre-existing cancer diagnosis. Computerized tomography did reveal liver lesions as well. With increasing use of endoscopy and colonoscopy in the current era, physicians should be mindful of the uncommon differentials as well.
- Citation: Badipatla KR, Yadavalli N, Vakde T, Niazi M, Patel HK. Lung cancer metastasis to the gastrointestinal system: An enigmatic occurrence. World J Gastrointest Oncol 2017; 9(3): 129-134
- URL: https://www.wjgnet.com/1948-5204/full/v9/i3/129.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v9.i3.129
Gastrointestinal metastasis of a primary lung cancer although previously reported in literature is a rare presentation. When metastasis does occur, the small bowel appears to be the most common site[1]. Clinical presentation may vary from being asymptomatic to non-specific abdominal pain and life threatening complications like massive bleeding and perforation requiring emergent surgical interventions[2]. Our case is first of its kind where in adenocarcinoma of lung is diagnosed by histology from a mass lesion in the rectum and gastric ulcer, in a person with no prior respiratory symptoms.
A 65-year-old man presented to our hospital emergency room (ER) with complaints of bilateral flank pain. He denied nausea, vomiting and change in bowel habit. He reported decrease in appetite and loss of 15-pound (lbs.) weight in one month.
His medical history was significant for mild intermittent bronchial asthma, benign essential hypertension, major depressive disorder and prostate cancer treated with radiation therapy 5 years prior to current hospital admission which is currently in remission. He did not undergo any surgical procedures in the past. There were no gastrointestinal malignancies diagnosed in his immediate or distant family members. He never used tobacco products, alcohol or recreational drugs. He was not allergic to any medications.
On initial evaluation he was afebrile with heart rate of 75 beats per minute, respiratory rate of 18 per minute and blood pressure of 150/70 millimeters of mercury (mm of Hg). His oxygen saturation was 95% on room air. Abdomen was non-distended, soft and non-tender to palpation. On auscultation bowel sounds were noted to be normoactive. Digital rectal examination (DRE) revealed a hard palpable, non-mobile mass on the posterior rectal wall. Cardiorespiratory and neurological examination was within normal limits.
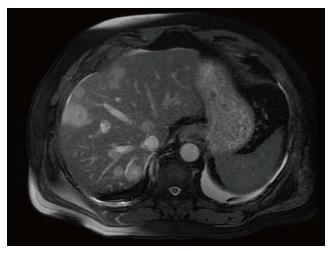
Laboratory results were significant for microcytic anemia with hemoglobin of 8.5-g percent with normal white cell counts and platelets. Coagulation parameters were within normal limits. Liver function tests showed elevated alkaline phosphatase of 482 units per liter, with remaining liver parameters being unremarkable. Tumor markers showed mildly elevated carcinoembryonic antigen level of 38.2 nanogram/milliliter and Cancer antigen-125 (CA-125) of 682.8 units/milliliter. Serum prostate specific antigen (PSA) level was 0.12 nanogram/milliliter. Computerized tomography of chest, abdomen and pelvis showed an area of opacity measuring 8.8 cm × 4.6 cm × 6.3 cm in the left upper lobe of the lung, diffuse mediastinal adenopathy and moderate to large left sided pleural effusion (Figure 1). There was diffuse osteo-sclerosis of multiple bones suspicious for osteoblastic metastatic disease. Also, noted were several intrahepatic masses suspicious for metastatic disease and shotty mesenteric and portocaval adenopathy. Magnetic resonance imaging (MRI) confirmed computed tomography (CT) findings of liver metastases (Figure 2).
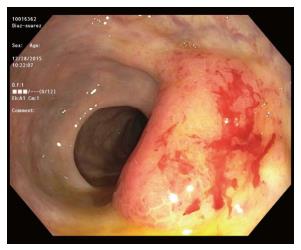
Gastroenterology consultation was obtained in view of anemia and possible liver lesions. Patient underwent upper gastrointestinal endoscopy, colonoscopy and subsequent endoscopic ultrasound under monitored anesthesia care. Upper gastrointestinal endoscopy showed a 15-millimeter crated gastric ulcer without any stigmata of recent bleeding which was biopsied (Figure 3). Colonoscopy showed a large mass in the rectum (Figure 4) and four polyps in the cecum, all of which were biopsied. Subsequent endoscopic ultrasound (EUS) of the rectal lesion revealed irregular hypoechoic lesion causing thickening of the submucosal layer and irregular out-borders suggestive of malignant nature of the lesion. Patient also underwent CT guided left thoracentesis and liver biopsy.
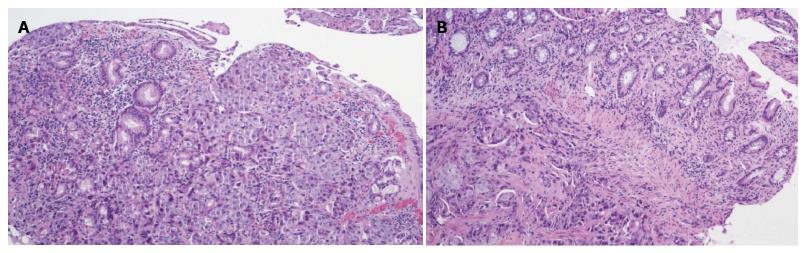
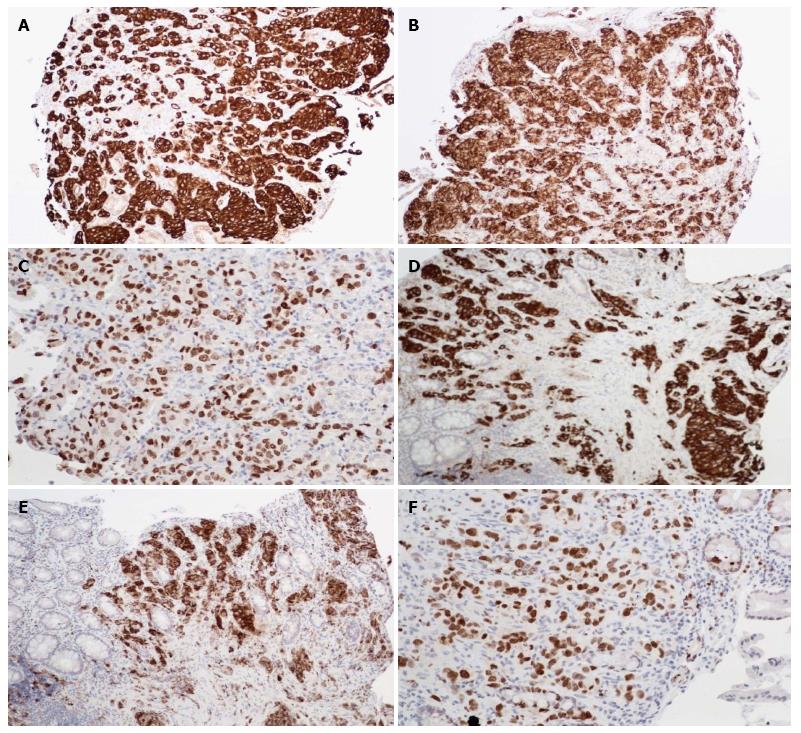
Pathology from both rectal mass and gastric ulcer showed metastatic adenocarcinoma, consistent with lung primary (Figure 5). Immuno-histochemical staining was positive for cytokeratin 7 (CK 7), thyroid transcription factor-1 (TTF-1) and napsin-A antibodies (Figure 6). It was negative for PSA, prostate specific acid phosphatase, CK 20, CDX-2, cancer antigen 19-9 (CA 19-9) and P504 antibodies consistent with lung primary. Results from thoracentesis and liver biopsy yielded similar results showing metastatic adenocarcinoma of the lung origin. Patient was started on chemotherapy with combination of Carboplatin and Paclitaxel. After receiving two cycles of chemotherapy, patient and family opted for palliative care and he expired five months after the diagnosis was made.
Lung cancer is the most common cancer worldwide accounting for 19.4% of all the cancer related deaths[3].
Adenocarcinoma of the lung is known to metastasize to liver, lung, brain and bone with half of the patients harboring metastasis at the time of presentation[4]. Gastrointestinal tract is an infrequent site of metastasis. In a large retrospective study done by Kim et al[5] gastrointestinal metastasis was found in 0.19% of all the cases with small bowel being the most common site, although autopsy studies revealed higher rates of metastatic disease[1]. Metastatic lung cancer has known to spread to any location from the oral cavity to the anus[6] with lymphatic and hematogenous routes being the possible modes of spread[7].
Symptomatology spectrum ranges from being totally asymptomatic to bleeding[8], pain and dysphagia in case of esophageal involvement[9]. Peritonitis, perforation[10] and bowel obstruction are among the acute complications that were reported[11]. Laboratory analysis may reveal iron deficiency anemia.
Diagnosis is based on endoscopy with biopsies. On gastrointestinal endoscopy variable endoscopic appearances have been described including ulcerated lesion, nodularity, diffuse mucosal involvement, polyp or mass lesions[12]. Small bowel endoscopy (SBE) may be needed for evaluation of small bowel lesions. Histological examination of post-surgical specimens usually reveals diagnosis. On colonoscopy lesions, may vary from sub-centimeter lesions to more larger mass lesions as in our case. So far, review of literature shows 15 cases of metastatic lung cancer to the colon[2,13-25] (Table 1). The most common reported histology appears to be squamous cell carcinoma followed by adenocarcinoma being the less common variant[13,14] (Table 1).
| Ref. | Histology | Prior diagnosis of lung malignancy | Presenting clinical scenario |
| Jevremovic et al[13], 2016 | Adenocarcinoma | New diagnosis | Iron deficiency anemia |
| Miyazaki et al[15], 2015 | Squamous cell | Known case | Abdominal pain and anemia |
| Kaswala et al[14], 2013 | Adenocarcinoma | Known case | Surveillance colonoscopy |
| Sakai et al[16], 2012 | Squamous cell | Known case | Abdominal pain |
| Hirasaki et al[17], 2008 | Squamous cell | Diagnosed at the same time | Asymptomatic with positive fecal occult blood testing. |
| Yang et al[2], 2006 | Squamous cell | Known case | Bloody stools |
| Stinchcombe et al[18], 2006 | Squamous cell | Diagnosed at the same time | Asymptomatic with positron emission tomography computer tomography scan done showing increased colonic uptake |
| Habeşoğlu et al[19], 2005 | Squamous cell | Cancer naive | Bowel obstruction |
| Carroll et al[20], 2001 | Squamous cell | Cancer naive | Weight loss and diarrhea |
| Bastos et al[21], 1998 | Squamous cell | Known case | Abdominal pain, diarrhea and bloody stools |
| Gitt et al[22], 1996 | Squamous cell | Known case | Bowel perforation |
| Gateley et al[23], 1993 | Squamous cell | Known case | Gastrointestinal bleeding |
| Brown et al[24], 1980 | Anaplastic carcinoma | Diagnosed at the same time | Abdominal pain, weight loss |
| Smith et al[25], 1978 (2 cases) | Histology not known | Not known | Intermittent obstruction, bleeding or anemia |
Immuno-histochemical staining of the tissue is useful in streamlining the diagnosis[26] with TTF-1 and napsin-1 being specific for lung adenocarcinoma[27].
Prognosis appears to be poor in patients with gastrointestinal metastasis. Palliative resection has been described as treatment option especially in small bowel lesions to prevent further complications.
In summary, our case describes an extremely rare occurrence of synchronous metastasis of adenocarcinoma of lung presenting as gastric ulcer and rectal mass in an asymptomatic patient. To the best of our knowledge, our case is the first case described in literature of such a presentation. This again throws light that metastasis to the gastrointestinal tract may be considered among the differential while encountering such lesions in the gastrointestinal tract and appropriate diagnosis and prompt treatment may be helpful in these cases.
A 65-year-old man with anemia, weight loss and liver lesions noted to have gastric ulcer on endoscopy and rectal mass on colonoscopy.
Lung cancer presenting as metastatic gastric ulcer and rectal mass in a cancer naïve patient.
Metastatic lung cancer to the gastrointestinal system.
Laboratory results were significant for microcytic anemia with hemoglobin of 8.5 g percent. Alkaline phosphatase was 482 units per liter. Tumor markers showed mildly elevated carcinoembryonic antigen levels of 38.2 units/milliliter and cancer antigen -125 of 682.8 units/ milliliter.
Computed tomography revealed lung lesion with mediastinal adenopathy and metastasis to liver.
Histopathology from gastric ulcer and rectal mass revealed adenocarcinoma of lung.
Chemotherapy.
Prior reports of gastrointestinal metastasis from lung cancer included mostly autopsy series with small bowel being the most common site. There have been no reports of synchronous metastasis of lung cancer to stomach and rectum as in the case.
Adenocarcinoma of the lung is one the types of lung cancer with malignant potential.
This is a unique presentation of lung cancer metastasis.
The case is well drafted and references are adequate.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Garfield D, Sugawara I, Yu XC S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Yoshimoto A, Kasahara K, Kawashima A. Gastrointestinal metastases from primary lung cancer. Eur J Cancer. 2006;42:3157-3160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 2. | Yang CJ, Hwang JJ, Kang WY, Chong IW, Wang TH, Sheu CC, Tsai JR, Huang MS. Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcome. Lung Cancer. 2006;54:319-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 151] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 3. | Mao Y, Yang D, He J, Krasna MJ. Epidemiology of Lung Cancer. Surg Oncol Clin N Am. 2016;25:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 304] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 4. | Del Rosario M, Tsai H. Not all gastric masses are gastric cancer. BMJ Case Rep. 2016;2016:pii: bcr2015213535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Kim MS, Kook EH, Ahn SH, Jeon SY, Yoon JH, Han MS, Kim CH, Lee JC. Gastrointestinal metastasis of lung cancer with special emphasis on a long-term survivor after operation. J Cancer Res Clin Oncol. 2009;135:297-301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 93] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Al-Tarakji M, Feilchenfeldt J, Haidar A, Szabados L, Abdelaziem S, Sayed A, Toro A, Di Carlo I. Rare occurrence of metastasis from lung cancer to the anus: case report and review of the literature. World J Surg Oncol. 2016;14:157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Sileri P, D’Ugo S, Del Vecchio Blanco G, Lolli E, Franceschilli L, Formica V, Anemona L, De Luca C, Gaspari AL. Solitary metachronous gastric metastasis from pulmonary adenocarcinoma: Report of a case. Int J Surg Case Rep. 2012;3:385-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Akahoshi K, Chijiiwa Y, Hirota I, Ohogushi O, Motomatsu T, Nawata H, Sasaki I. Metastatic large-cell lung carcinoma presenting as gastrointestinal hemorrhage. Acta Gastroenterol Belg. 1996;59:217-219. [PubMed] |
| 9. | Park JY, Hong SW, Lee JY, Kim JH, Kang JW, Lee HW, Im JP. Simultaneous Esophageal and Gastric Metastases from Lung Cancer. Clin Endosc. 2015;48:332-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Aoyama K, Hiyama J, Horita N, Shiota Y, Ono T, Yamakido M. [Bowel perforation due to metastatic lung cancer: a case report]. Nihon Kokyuki Gakkai Zasshi. 2003;41:537-540. [PubMed] |
| 11. | Berger A, Cellier C, Daniel C, Kron C, Riquet M, Barbier JP, Cugnenc PH, Landi B. Small bowel metastases from primary carcinoma of the lung: clinical findings and outcome. Am J Gastroenterol. 1999;94:1884-1887. [PubMed] [DOI] [Full Text] |
| 12. | Rossi G, Marchioni A, Romagnani E, Bertolini F, Longo L, Cavazza A, Barbieri F. Primary lung cancer presenting with gastrointestinal tract involvement: clinicopathologic and immunohistochemical features in a series of 18 consecutive cases. J Thorac Oncol. 2007;2:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Jevremovic V, Abboud A, Krauss S. Colonic Metastasis with Anemia Leading to a Diagnosis of Primary Lung Adenocarcinoma. Case Rep Oncol Med. 2016;2016:5275043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Kaswala DH, Patel NR, Shah SS, Razack RM, Fitzhugh VA, Brelvi ZS. Metastatic lung adenocarcinoma mimicking a colonic polyp. N Am J Med Sci. 2013;5:306-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Miyazaki J, Hirota S, Abe T. Metastasis of lung cancer to the gastrointestinal tract, presenting with a volcano-like ulcerated mass. Dig Endosc. 2015;27:397-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Sakai H, Egi H, Hinoi T, Tokunaga M, Kawaguchi Y, Shinomura M, Adachi T, Arihiro K, Ohdan H. Primary lung cancer presenting with metastasis to the colon: a case report. World J Surg Oncol. 2012;10:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Hirasaki S, Suzuki S, Umemura S, Kamei H, Okuda M, Kudo K. Asymptomatic colonic metastases from primary squamous cell carcinoma of the lung with a positive fecal occult blood test. World J Gastroenterol. 2008;14:5481-5483. [PubMed] |
| 18. | Stinchcombe TE, Socinski MA, Gangarosa LM, Khandani AH. Lung cancer presenting with a solitary colon metastasis detected on positron emission tomography scan. J Clin Oncol. 2006;24:4939-4940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Habeşoğlu MA, Oğuzülgen KI, Oztürk C, Akyürek N, Memiş L. A case of bronchogenic carcinoma presenting with acute abdomen. Tuberk Toraks. 2005;53:280-283. [PubMed] |
| 20. | Carroll D, Rajesh PB. Colonic metastases from primary squamous cell carcinoma of the lung. Eur J Cardiothorac Surg. 2001;19:719-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Bastos I, Gomes D, Gouveia H, de Freitas D. Colonic metastasis of a lung carcinoma with ileocolic fistula. J Clin Gastroenterol. 1998;26:348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Gitt SM, Flint P, Fredell CH, Schmitz GL. Bowel perforation due to metastatic lung cancer. J Surg Oncol. 1992;51:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Gateley CA, Lewis WG, Sturdy DE. Massive lower gastrointestinal haemorrhage secondary to metastatic squamous cell carcinoma of the lung. Br J Clin Pract. 1993;47:276-277. [PubMed] |
| 24. | Brown KL, Beg RA, Demany MA, Lacerna MA. Rare metastasis of primary bronchogenic carcinoma to sigmoid colon: report of a case. Dis Colon Rectum. 1980;23:343-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Smith HJ, Vlasak MG. Metastasis to the colon from bronchogenic carcinoma. Gastrointest Radiol. 1978;2:393-396. [PubMed] |
| 26. | Lin HC, Yu CP, Lin HA, Lee HS. A case of lung cancer metastasized to the gastrointestinal anastomosis site where the primary gastric cancer was resected 17 years ago. Lung Cancer. 2011;72:255-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | El Hag M, Schmidt L, Roh M, Michael CW. Utility of TTF-1 and Napsin-A in the work-up of malignant effusions. Diagn Cytopathol. 2016;44:299-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |