Published online Mar 15, 2016. doi: 10.4251/wjgo.v8.i3.326
Peer-review started: August 6, 2015
First decision: November 6, 2015
Revised: November 19, 2015
Accepted: December 29, 2015
Article in press: January 4, 2016
Published online: March 15, 2016
Processing time: 219 Days and 15.5 Hours
Primary cardiac liposarcoma is exceedingly rare and its metastatic potential varies based on the actual tumor subclass. Intestinal intussusception is also an uncommon cause of abdominal pain and bowel obstruction in adults and it usually generates at a malignant lead point in this age group. We report a case of a primary cardiac dedifferentiated liposarcoma in a pregnant woman causing small bowel seeding leading to bowel intussusception.
Core tip: Primary cardiac liposarcoma is exceedingly rare and its metastatic potential varies based on the actual tumor subclass. Intestinal intussusception is also an uncommon cause of abdominal pain and bowel obstruction in adults and it usually generates at a malignant lead point in this age group. We report a case of a primary cardiac dedifferentiated liposarcoma in a pregnant woman causing small bowel seeding leading to bowel intussusception.
- Citation: Gomez G, Bilal M, Klepchick P, Clarke K. Rare case of entero-enteric intussusception caused by small bowel metastasis from a cardiac liposarcoma. World J Gastrointest Oncol 2016; 8(3): 326-329
- URL: https://www.wjgnet.com/1948-5204/full/v8/i3/326.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v8.i3.326
Primary cardiac liposarcoma is exceedingly rare and its metastatic potential varies based on the actual tumor subclass. Intestinal intussusception is also an uncommon cause of abdominal pain and bowel obstruction in adults and it usually generates at a malignant lead point in this age group. We report a case of a primary cardiac dedifferentiated liposarcoma in a pregnant woman causing small bowel seeding leading to bowel intussusception.
A 29-year-old female with recent history of surgically resected intra-cardiac liposarcoma presents to the hospital at 27 wk of gestational age with complains of sudden onset of abdominal pain associated with intractable nausea and vomiting.
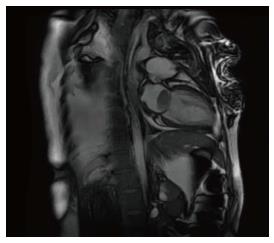
Three months prior to this presentation, the patient was admitted with severe shortness of breath and dyspnea on exertion. She was found to have a left intra-atrial mass on a transthoracic echocardiogram involving a large portion of the left atrium, anterior leaflet of the mitral valve and pulmonary venous system causing complete occlusion of the right inferior pulmonary vein. Cardiac magnetic resonance imaging confirmed the lesion (Figure 1). The patient underwent resection of the mass and porcine mitral valve replacement. In addition, she also had pulmonary venous endarterectomy. Due to the size of the mass with significant extension into the pulmonary venous vasculature, a complete en-block resection could not be performed. Postoperative course was complicated by a transient 3rd degree atrio-ventricular block. She was discharged on post-operative day 14. Outpatient tumor staging included non-contrast MRIs of the brain, abdomen and pelvis that were negative for any metastatic disease.
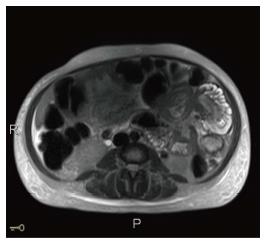
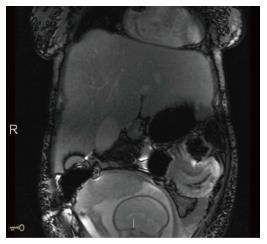
On this presentation to the hospital, an magnetic resonance imaging (MRI) of the abdomen and pelvis was performed for severe abdominal pain, which revealed an entero-enteric left upper quadrant intestinal intussusception with proximal small bowel dilation suggestive of a mechanical small bowel obstruction (Figures 2 and 3). After an unsuccessful trial of conservative management with nil per os and naso-gastric tube decompression, she developed acute cardiopulmonary decline associated with significant fetal cardiac distress. A multi-disciplinary meeting was held and she had an emergency caesarian section, exploratory laparotomy and placement of a transcutaneous cardiac pacemaker prior to the surgical interventions. A healthy, viable 950 g female infant was delivered. At exploratory laparotomy, a 10 cm long intussuscepted small bowel segment without evidence of ischemia, beginning at 50 cm form the ligament of Treitz was identified. After several and unsuccessful manual attempts at reducing this bowel segment, partial small bowel resection of the affected area with end-to-end anastomosis was performed.
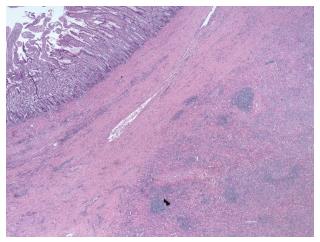
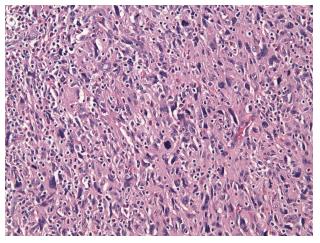
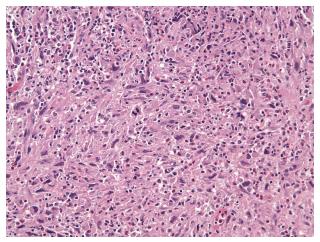
The surgically resected specimen showed two polypoid lesions, which were 5 cm and 1 cm in their greatest dimension. Pathology was consistent with pleomorphic neoplasm with spindle cells, giant cells, vesicular nuclei with macro nuclei and occasional intra nuclear inclusions (Figures 4 and 5). Immunohistochemical staining was positive for Murine Double Minute (MDM) 2 and CDK 4. The histological features were identical to the original neoplasm seen in the heart 3 mo earlier (Figure 6). Post operatively the patient developed respiratory failure and was not able to be weaned off the ventilator. On post-operative day 8, the family decided to withdraw care. Unfortunately, the patient passed away the same day.
Primary cardiac neoplasms are exceedingly rare. Secondary (metastatic) cardiac lesions are 20-40 times more common than primary tumors[1,2]. Malignant cardiac neoplasms constitute between 15%-25% of these primary lesions and sarcomas are found to be the most common malignancy[3,4]. Liposarcoma accounts for about 13% of primary malignant tumors of the heart[5]. There are five histological subtypes of these adipocyte precursor tumors including well differentiated, dedifferentiated, myxoid or round cell type, pleopmorphic and mixed variant. Dedifferentiated liposarcoma commonly rises from the retroperitoneum and extremities and carries a lower incidence of distal seeding compared to the pleomorphic variant[6-8]. Most common sites of metastasis include the lung, liver, bone, brain and soft tissues. Metastasis to the small bowel is rare with only few previously reported cases in the medical literature.
Surgical management is the preferred approach for cardiac liposarcoma, given its metastatic potential and the significant associated cardiorespiratory morbidity.
Intestinal intussusception is a rare cause of intestinal obstruction in adults accounting for 1%-5% of the cases[9]. It is defined as telescoping or prolapsing of a proximal intestinal segment into the adjacent more distal bowel segment secondary to peristaltic movements. Depending on the location of intestinal segment involved, intussusceptions are classified as enteroenteric, ileocolic, ileocecal or colocolonic. Majority of cases in adults are related to pathologic conditions that serve as a lead point for initiation of the prolapsing process. Intestinal diverticulum, luminal strictures and benign or malignant neoplasm are some of the more common causes[9,10]. Enteroenteric intussusceptions due to malignant conditions accounts for up to 30% of all cases[11]. Metastatic disease, adenocarcinoma and small bowel lymphomas are some of the leading metastatic causes[12].
Clinical presentation varies depending of the degree of obstruction and ranges from chronic abdominal pain to intractable nausea, vomit and frank hematochezia in cases of complete obstruction associated with intestinal ischemia. Computer tomography scan of the abdomen and pelvis is the preferred imaging modality, with reported accuracy rates form 30%-100%[12]. Abdominal Ultrasound and abdominal MRI are two other alternatives and can be used in pregnancy to minimize radiation exposure to the fetus.
Surgical resection of the intussuscepted area is the treatment of choice in the adult population[9]. Although surgical resection was performed in our patient, with appropriate treatment of intestinal obstruction, her simultaneous pregnancy, heart block and respiratory condition increased her overall risks for mortality.
There have been few reported cases of liposarcoma causing metastasis to the small bowel. To the best of our knowledge, this is the first reported case of a primary cardiac dedifferentiated liposarcoma causing metastasis to the small bowel with associated intussusception.
Primary cardiac liposarcoma is exceedingly rare and its metastatic potential varies based on the actual tumor subclass.
Intestinal intussusception is also an uncommon cause of abdominal pain and bowel obstruction in adults and it usually generates at a malignant lead point in this age group.
The authors report a case of a primary cardiac dedifferentiated liposarcoma in a pregnant woman causing small bowel seeding leading to bowel intussusception.
On this presentation to the hospital, a magnetic resonance imaging of the abdomen and pelvis was performed for severe abdominal pain, which revealed an entero-enteric left upper quadrant intestinal intussusception with proximal small bowel dilation suggestive of a mechanical small bowel obstruction.
The case is interesting, well written and easy to read. References are new and adequate.
P- Reviewer: Ramia J S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Harvey WP. Clinical aspects of cardiac tumors. Am J Cardiol. 1968;21:328-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 159] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Pino PG, Zampi G, Pergolini A, Pero G, Polizzi V, Sbaraglia F, Minardi G, Musumeci F. Metastatic liposarcoma of the heart. Case series and brief literature review. Herz. 2013;38:938-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Agaimy A, Rösch J, Weyand M, Strecker T. Primary and metastatic cardiac sarcomas: a 12-year experience at a German heart center. Int J Clin Exp Pathol. 2012;5:928-938. [PubMed] |
| 4. | Barreiro M, Renilla A, Jimenez JM, Martin M, Al Musa T, Garcia L, Barriales V. Primary cardiac tumors: 32 years of experience from a Spanish tertiary surgical center. Cardiovasc Pathol. 2013;22:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Steger CM. Primary liposarcoma of the heart. BMJ Case Rep. 2011;2011:pii: bcr0320114013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Dei Tos AP. Liposarcoma: new entities and evolving concepts. Ann Diagn Pathol. 2000;4:252-266. [PubMed] |
| 7. | Henricks WH, Chu YC, Goldblum JR, Weiss SW. Dedifferentiated liposarcoma: a clinicopathological analysis of 155 cases with a proposal for an expanded definition of dedifferentiation. Am J Surg Pathol. 1997;21:271-281. [PubMed] |
| 8. | Shibata Y, Sato K, Kodama M, Nanjyo H. Metastatic liposarcoma in the jejunum causing intussusception: report of a case. Surg Today. 2008;38:1129-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 428] [Cited by in RCA: 507] [Article Influence: 31.7] [Reference Citation Analysis (2)] |
| 10. | Weilbaecher D, Bolin JA, Hearn D, Ogden W. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 213] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 384] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 12. | Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics. 2006;26:733-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |