Published online Dec 15, 2016. doi: 10.4251/wjgo.v8.i12.835
Peer-review started: May 3, 2016
First decision: July 5, 2016
Revised: August 25, 2016
Accepted: October 22, 2016
Article in press: October 24, 2016
Published online: December 15, 2016
Processing time: 217 Days and 7.3 Hours
Rhabdomyomatous well-differentiated esophageal liposarcomas are extremely rare. As of August 2016, only one other such case has been reported in the English-language medical literature. Liposarcomas in general are one of the most common soft tissue neoplasms in adults, but the incidence of primary esophageal liposarcomas is exceptionally low. There have been only 42 reported cases of primary liposarcoma of the esophagus worldwide thus far. These malignancies are harbored within giant fibrovascular polyps, which slowly grow within the esophageal lumen causing obstructing symptoms. We hereby present the case of a 68-year-old male patient who came in with a 2-mo history of worsening intermittent dysphagia, persistent cough, and postprandial retrosternal pain. After an esophagogastroduodenoscopy, a computed tomographic scan, and a diagnostic endoscopy, complete endoscopic resection was performed of the 13 cm × 6 cm × 2.6 cm fibrovascular polyp. A literature review was done and results are presented herein.
Core tip: This is only the second case of a rhabdomyomatous well-differentiated esophageal liposarcoma to be reported in the literature. Both cases clinically presented as standard esophageal liposarcomas housed in a giant fibrovascular polyp until histological examination by pathology. Given the rarity of the disease, there are only a few studies outlining its optimal management, nevertheless, diagnosis and treatment of this pathology can be approached by customary means, bearing extremely favorable prognosis.
- Citation: Valiuddin HM, Barbetta A, Mungo B, Montgomery EA, Molena D. Esophageal liposarcoma: Well-differentiated rhabdomyomatous type. World J Gastrointest Oncol 2016; 8(12): 835-839
- URL: https://www.wjgnet.com/1948-5204/full/v8/i12/835.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v8.i12.835
Primary esophageal liposarcomas are rare, with only 42 cases being reported in English-language literature as of August 2016[1]. Histologically, liposarcomas can be further classified into 4 subtypes based on their degree of differentiation: Dedifferentiated, well-differentiated, myxoid, or pleomorphic[2]. We present the case of a patient who had an esophageal well-differentiated liposarcoma containing rhabdomyomatous cells, of which, only one other case - to the best of our knowledge - has ever been reported[3].
A 68-year-old Caucasian male presented with a 2-mo history of worsening intermittent dysphagia, persistent cough, and postprandial retrosternal pain. He also complained of persistent dull pain on the left side of his neck, radiating to his left ear, which was not related to meals.
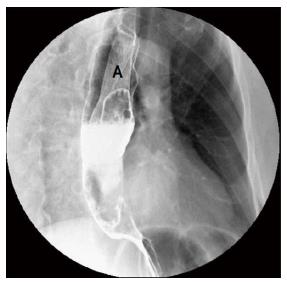
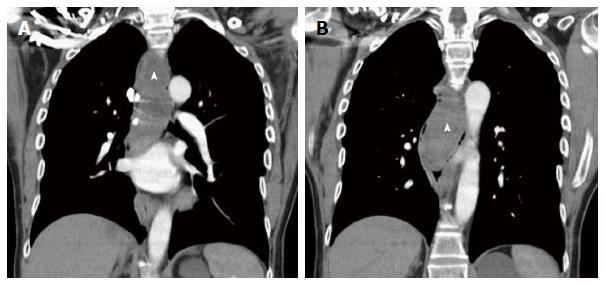
Suspecting gastroesophageal reflux disease, the patient was started on proton pump inhibitor pharmacotherapy. Upon no relief of symptoms, the patient was referred to an otolaryngologist to evaluate the pharynx with a laryngoscopy; no abnormalities were seen, and therefore the patient was referred to a gastroenterologist. An esophagram was first performed, which showed a voluminous intraluminal lesion within the thoracic esophagus, possibly being a neoplastic process such as a leiomyoma (Figure 1). An esophagogastroduodenoscopy was then performed, identifying a polypoid mass, which started at the level of the upper esophageal sphincter with a single stalk and extended all the way down to the esophagogastric junction. The polyp occupied about a third of the esophageal lumen, was heterogeneous in surface appearance, and consistent with a giant fibrovascular polyp; concurrently a small hiatal hernia was also seen. Biopsies from the head of the polyp exhibited benign squamous mucosa with mild acute and chronic inflammation. A computed tomographic (CT) scan of the chest showed a large mass along the entire course of the esophagus (Figure 2). After an endoscopic ultrasound excluded the presence of major vessels within the main stalk, endoscopic resection was pursued. While using a flexible esophagoscope to visualize the mass, a snare was passed around the distal end of the polyp on retroflexion and then pulled up around the stalk, which was located on the left side of the esophagus just at the level of the upper esophageal sphincter. The proximal stalk was cauterized and divided with the snare, causing the polyp to drop into the distal esophagus. The polyp was then retrieved transorally using the endoscope and the snare to bring the mass to the level of the upper esophageal sphincter, followed by a laryngoscope and a clamp to extract it from the hypopharynx.
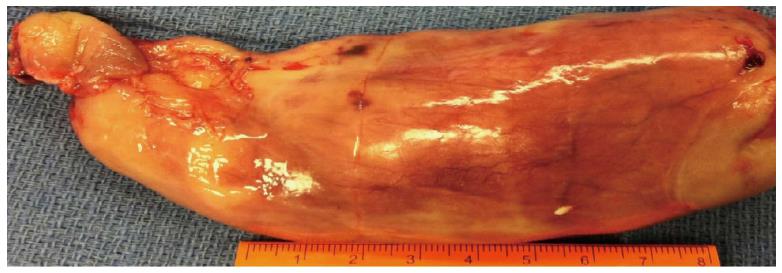
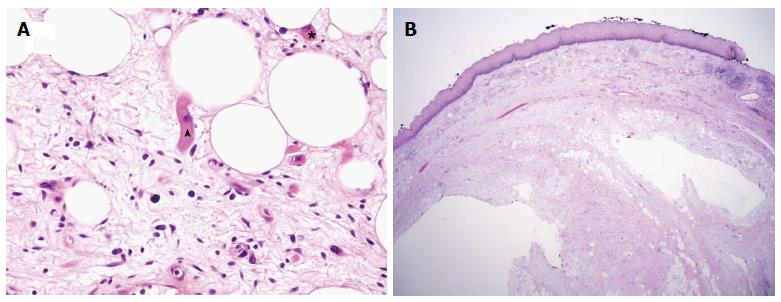
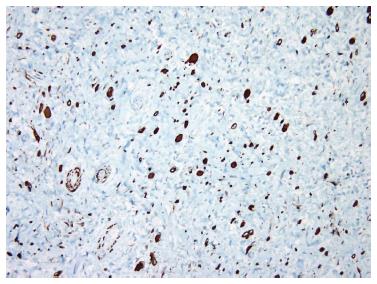
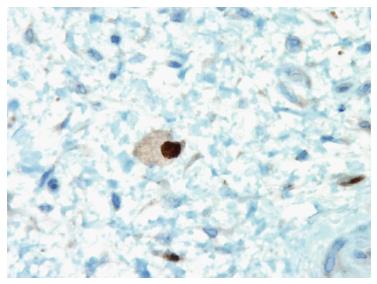
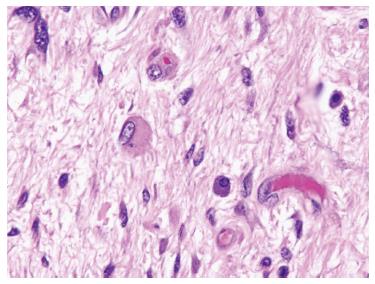
Pathology identified the 13.0 cm × 6.0 cm × 2.6 cm specimen as a well-differentiated liposarcoma arising in a giant fibrovascular polyp. Grossly the polyp had tan uniform surface without stigma of hemorrhage or necrosis (Figure 3). Histologically the polyp showed a central core of adipose and fibrovascular tissue surrounded by overlying squamous mucosa (Figure 4). An immunohistochemical stain for MDM-2 supported the diagnosis of liposarcoma (Figure 5). Focal areas of ossification were noted. In addition, there were scattered atypical cells with abundant eosinophilic cytoplasm, positive for desmin and also focally myogenin positive (Figure 6). The rhabdomyomatous differentiation is considered a low grade lesion (Figure 7).The final resection margin was uninvolved by the tumor. Patient recovered uneventfully and was discharged from the hospital on postoperative day 1. On follow up visit at 4 years, patient still has complete resolution of dysphagia, cough, neck and chest pain. He has been eating well and gained 15 pounds to date. Annual endoscopies and CT scans confirm no reoccurrence thus far.
Esophageal liposarcomas reside in giant fibrovascular polyps and are rare, consisting of 0.5% of all esophageal neoplasms[4]. Of the histologic sub classifications, well-differentiated type are the most common, with a prevalence of approximately 68%; myxoid being 20%; dedifferentiated and pleomorphic at 6% each[5]. The pathophysiology of esophageal giant fibrovascular polyps is unknown. The only theory with consensus is that an erroneous out-pouching of loose submucosal tissue undergoes traction and peristaltic forces causing it to insidiously grow and elongate into the lumen[3]. The average size of a giant fibrovascular polyp is approximately 13 cm in length, and 3.5 cm in width[3,5]. Liposarcomas are believed to originate from primitive mesenchymal cells rather than mature adipocytes[2]. The average age of onset of symptoms is 58.4 years, ranged from 38 to 73 years[4,5]. There has been a 72% male predominance of reported cases[5]. Almost all lesions were polypoid, except for a couple that were transmural[5,6]. Eighty percent of the liposarcomas described have been from the cervical portion of the esophagus, with the rest originating more distally[5].
Clinically, patients can present with dysphagia for solids and/or liquids, weight loss, intermittent odynophagia, nausea, globus sensation, cough, emesis and retrosternal pain[2]. If proper diagnosis and treatment is not administered, there can be drastic complications such as anemia, vomiting of tumor fragments, oral regurgitation of polyp upon emesis, respiratory compromise and fatal asphyxiation[2,3]. Objective diagnosis can be conducted with barium swallow, esophagogastroduodenoscopy, CT scans, and magnetic resonance imaging (MRI). However, making the diagnosis can require some scrutiny. More specifically, Jakowski and Wakely[3] described a particular case in which the imaging investigations lead to a differential of achalasia initially, later corrected to a giant pedunculated mass. At best, an accurate esophagram can only identify the presence of a mass; often, other examinations must be used in combination to differentiate, evaluate, and grade the tumor. MRI and CT scans are of great help, not only in recognizing the tumor, but also by calculating the fat component of the tumor, hence providing better characterization of the mass: A 100% fat content is in fact consistent with a lipoma, whereas < 75% signifies atypical lipomas or low grade sarcoma[2,7].
The standard of care for giant esophageal polyps is surgical resection, which can be directed by different techniques; including an aggressive open cervical approach, radical three-hole esophagectomy, or local endoscopic resection[8,9]. Since in our case the endoscopic ultrasound identified a single proximal stalk without a significant feeding vessel, trans oral endoscopic resection was pursued; making sure completeness was achieved by examining margins of specimen to be uninvolved, as cases of reoccurrence after inadequate resection have been reported[2,5]. Alternatively, resection can also be done through a cervical incision with excision of the polyp from the esophageal lumen, which is in fact the traditional approach, and would have been pursued in presence of a large feeding vessel. Lastly, if the polyps were to have had multiple stalks throughout the entire esophagus, making complete removal through cervical approach unfeasible, an esophagectomy would then be indicated.
In conclusion, given the rarity of the disease, there are only a few studies outlining its optimal management, nevertheless, diagnosis and treatment of this pathology can be approached by customary means, bearing extremely favorable prognosis.
A 68-year-old Caucasian male presented with a 2-mo history of worsening intermitted dysphagia, persistent cough, post-prandial retrosternal pain and dull pain on the left side of his neck radiating to his left hear.
Polypoid mass starting at the level of the upper esophageal sphincter and extending down to the esophagogastric junction, occupying a third of the esophageal lumen.
Neoplastic lesion such as a leiomyoma.
Esophagogram and computed tomography scan showed a large mass along the entire course of the thoracic esophagus and an esophagogastroduodenoscopy identified a polypoid mass.
A 13.0 cm × 6.0 cm × 2.6 cm specimen is identified as a well-differentiated liposarcoma with rhabdomyomatous differentiation arising in a giant fibrovascular polyp and an immunohistochemical stain for MDM-2 supported the diagnosis of liposarcoma.
Complete endoscopic resection of the polyp.
Esophageal liposarcomas reside in giant fibrovascular polyps and are rare consisting of 0.5% of all esophageal neoplasms. The pathophysiology of esophageal giant fibrovascular polyps is unknown. The only theory with consensus is that an erroneous out-pouching of loose submucosal tissue undergoes traction and peristaltic forces causing it to insidiously grow and elongate into the lumen.
Liposarcoma is a soft tissue neoplasm and is believed to originate from primitive mesenchymal cells rather than mature adipocytes.
The standard of care for giant esophageal polyps is surgical resection, which can be directed by different techniques, including a transoral endoscopic resection. A complete resection should be achieved to avoid reoccurrence.
This is only the second case of a rhabdomyomatous well-differentiated esophageal liposarcoma to be reported in literature.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Abdou AG, Ding XW, Lee CL, Shimoyama S S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Dowli A, Mattar A, Mashimo H, Huang Q, Cohen D, Fisichella PM, Lebenthal A. A pedunculated giant esophageal liposarcoma: a case report and literature review. J Gastrointest Surg. 2014;18:2208-2213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 2. | Beaudoin A, Journet C, Watier A, Mongeau CJ, Chagnon M, Beaudry R. Giant liposarcoma of the esophagus. Can J Gastroenterol. 2002;16:377-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Jakowski JD, Wakely PE. Rhabdomyomatous well-differentiated liposarcoma arising in giant fibrovascular polyp of the esophagus. Ann Diagn Pathol. 2009;13:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Smith MA, Kluck E, Jagannath S, Yang SC. Giant multi-polypoid liposarcoma of the esophagus: an atypical presentation. Ann Thorac Surg. 2010;89:610-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Sui X, Li Y, Zhao H, Wang J. Giant liposarcoma of the esophagus with Li-Fraumeni-like syndrome. Eur J Cardiothorac Surg. 2011;40:1253-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Garcia M, Buitrago E, Bejarano PA, Casillas J. Large esophageal liposarcoma: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:922-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Yang B, Shi PZ, Li X, Xu RJ. Well-differentiated liposarcoma of esophagus. Chin Med J (Engl). 2006;119:438-440. [PubMed] |
| 8. | Lin ZC, Chang XZ, Huang XF, Zhang CL, Yu GS, Wu SY, Ye M, He JX. Giant liposarcoma of the esophagus: A case report. World J Gastroenterol. 2015;21:9827-9832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Caceres M, Steeb G, Wilks SM, Garrett HE. Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg. 2006;81:393-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |