Published online Apr 15, 2012. doi: 10.4251/wjgo.v4.i4.89
Revised: January 14, 2012
Accepted: January 25, 2012
Published online: April 15, 2012
Simultaneous development of adenocarcinoma and primary B cell lymphoma of mucosa-associated lymphoid tissue (MALT) lymphoma of the colon is rare; only one case has so far been reported out of 13 cases with the coexistence of colonic adenocarcinoma with involvement of the colon by lymphoma. We hereby present three more cases, two females (aged 75 and 71 years) and a male (aged 72 years). All three underwent colectomy based on a preoperative biopsy revealing colonic carcinoma. Histological examination of the resection specimens disclosed a colonic adenocarcinoma in two cases, whereas a tubulovillous adenoma with superficial foci of intraepithelial adenocarcinoma was seen in the third case. Moreover, in all three cases, a coexisting MALT lymphoma was diagnosed in the colon (1 case), in both colon and adjacent lymph nodes (1 case) or in colonic lymph nodes and omentum (1 case). In the last case, a post-operative bone marrow biopsy revealed extensive infiltration of the bone marrow, due to which the patient received postoperative chemotherapy. Diagnostic and treatment issues are briefly discussed.
- Citation: Argyropoulos T, Foukas P, Kefala M, Xylardistos P, Papageorgiou S, Machairas N, Boltetsou E, Machairas A, Panayiotides IG. Simultaneous occurrence of colonic adenocarcinoma and MALT lymphoma: A series of three cases. World J Gastrointest Oncol 2012; 4(4): 89-93
- URL: https://www.wjgnet.com/1948-5204/full/v4/i4/89.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v4.i4.89
Colonic adenocarcinoma is the third most commonly diagnosed cancer worldwide[1]. In contrast, extranodal marginal zone B-cell lymphoma [lymphoma of the mucosa-associated lymphoid tissue (MALT) type] is rare, constituting 6%-8% of non Hodgkin lymphomas. The colon is a rare location for the aforementioned lymphoma[2]. Only one case of simultaneous occurrence of adenocarcinoma and MALT lymphoma of the colon has so far been reported[3] out of 13 cases with the coexistence of colonic adenocarcinoma and involvement of the colon by lymphoma[3-13]. We hereby report three more cases.
A 75-year-old female was referred due to anemia, weakness, fatigue and presence of blood in the stools (positive Mayer test). Lower gastrointestinal endoscopy revealed a polypoid mass located about 4 cm proximal to the anal verge. An abdominoperineal resection was performed which showed a 7-cm polypoid tumor. Adjacent to the aforementioned tumor, a 1.5-cm large solid, whitish area was detected. A postsurgical work-up of upper endoscopy, abdominal computed tomography and bone marrow examination was negative for lymphoma involvement. The patient received no further treatment. Although she missed scheduled follow ups, she has since been readmitted due to intermittent incomplete intestinal obstruction. She is alive, 20 mo post-operatively.
A 71-year-old female was admitted due to a fainting episode. She mentioned a loss of 20 kg over the past year and had anemia. Colonoscopy revealed a tumor of the ascending colon; a biopsy diagnosed it as adenocarcinoma. The patient underwent a right hemicolectomy which revealed an 8.5 cm large, constricting ulcerated tumor 12 cm from the ileocaecal valve. The patient received no adjuvant therapy. She has since been regularly followed up and is alive and well 4 years post-operatively.
Colonoscopy of a 72-year-old male with anemia showed the presence of a polyp at the ascending colon, histologically shown to be a tubulovillous adenoma with superficial foci of intraepithelial adenocarcinoma. A subsequent right hemicolectomy specimen revealed a-4.5 cm large, fungating tumor at a distance of 7.6 cm from the ileocecal valve upon incision. He had no history of fever, loss of weight or night sweats. Clinical examination showed no peripheral lympadenopathy or hepatosplenomegaly. However, a post-operative bone marrow biopsy revealed infiltration (almost 80% of the total marrow area) by a CD20 (+), CD5 (-), CD10 (-), CD23 (-), CD43 (-), cyclin D1 (-) B cell lymphoid population, consistent with the MALT lymphoma previously diagnosed. Consequently, the patient was staged as IV A (Longano Staging system)[14] and was treated with six cycles of FCR [Fludarabine, Cyclophosphamide and Rituximab (monoclonal anti-CD20 antibody)]. He is alive and well 18 mo post-operatively.
Surgical specimens were fixed in a 10% buffered formol solution and processed according to standard protocols. 4 μm thick, deparaffinised sections were stained with Haematoxylin-Eosin[15]. Moreover, immunostains with primary antibodies (Table 1) were performed.
| P/M (clone) | Company | Dilution | Treatment | |
| CD3 | M mouse (LN10) | Novocastra | 1:200 | PT |
| CD5 | M rabbit (SP19) | DakoCytomation | 1:50 | PT |
| CD10 | M mouse (56C6) | Novocastra | 1:25 | PT |
| CD20 | M mouse (L26) | Novocastra | 1:50 | PT |
| CD21 | M mouse (1F8) | DakoCytomation | r. t. u. | S1700 |
| CD23 | M rabbit (SP23) | DakoCytomation | 1:50 | PT |
| CD34 | M mouse (QBEnd/10) | DakoCytomation | 1:50 | PT |
| CD35 | M mouse (Ber-MAC-DRC) | DakoCytomation | 1:30 | S1700 |
| CD43 | M mouse (MT1) | Novocastra | 1:50 | PT |
| CD61 | M mouse (Y2/51) | DakoCytomation | 1:40 | S1700 |
| CD138 | M mouse (MI15) | DakoCytomation | r. t. u. | ER1 |
| cyclin D1 | M rabbit (SP4) | DakoCytomation | r. t. u. | PT |
| Glycophorin A | M mouse (JC159) | DakoCytomation | 1:100 | PT |
| MPO | P rabbit | DakoCytomation | 1:2500 | PT |
| IgA | M mouse (6E2C1) | DakoCytomation | 1:70 | TR |
| IgG | M mouse (A57H) | DakoCytomation | 1:70 | TR |
| IgM | M mouse (R1/69) | DakoCytomation | 1:100 | TR |
| κ light chains | P rabbit | DakoCytomation | 1:60.000 | PT |
| λ light chains | P rabbit | DakoCytomation | 1:60.000 | PT |
| Bcl-2 | M mouse (124) | DakoCytomation | 1:40 | PT |
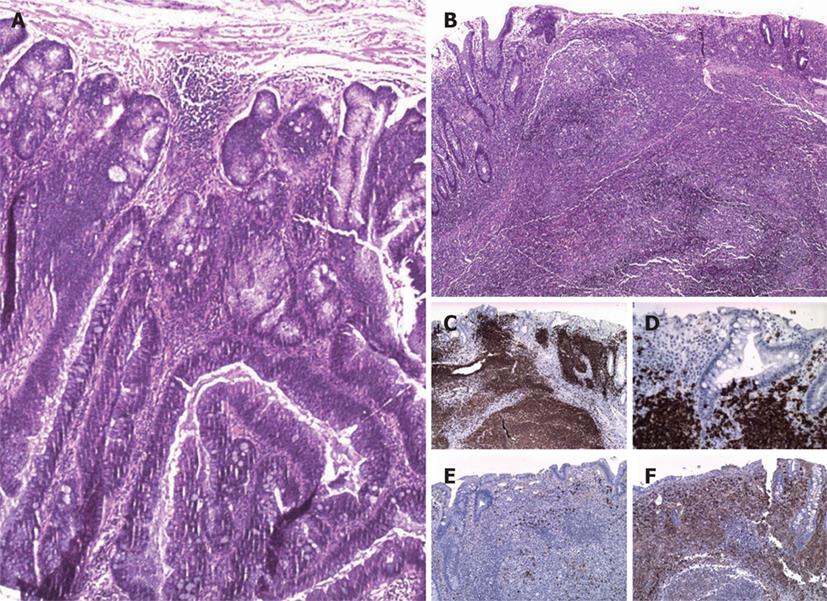
Case 1: Histology showed the polypoid tumor to be a tubulovillous adenoma with superficial foci of high grade intraepithelial neoplasia (i.e., in situ adenocarcinoma), without invasion of muscularis mucosae or submucosa (Figure 1A). The whitish area had histological and immunohistochemical features of an extranodal marginal zone B-cell lymphoma (of MALT type) with prominent plasmacytic differentiation and cIgλ clonality (Figure 1B-F). Two out of twenty two colonic lymph nodes retrieved were involved by lymphoma. A postsurgical bone marrow biopsy revealed no involvement of the bone marrow.
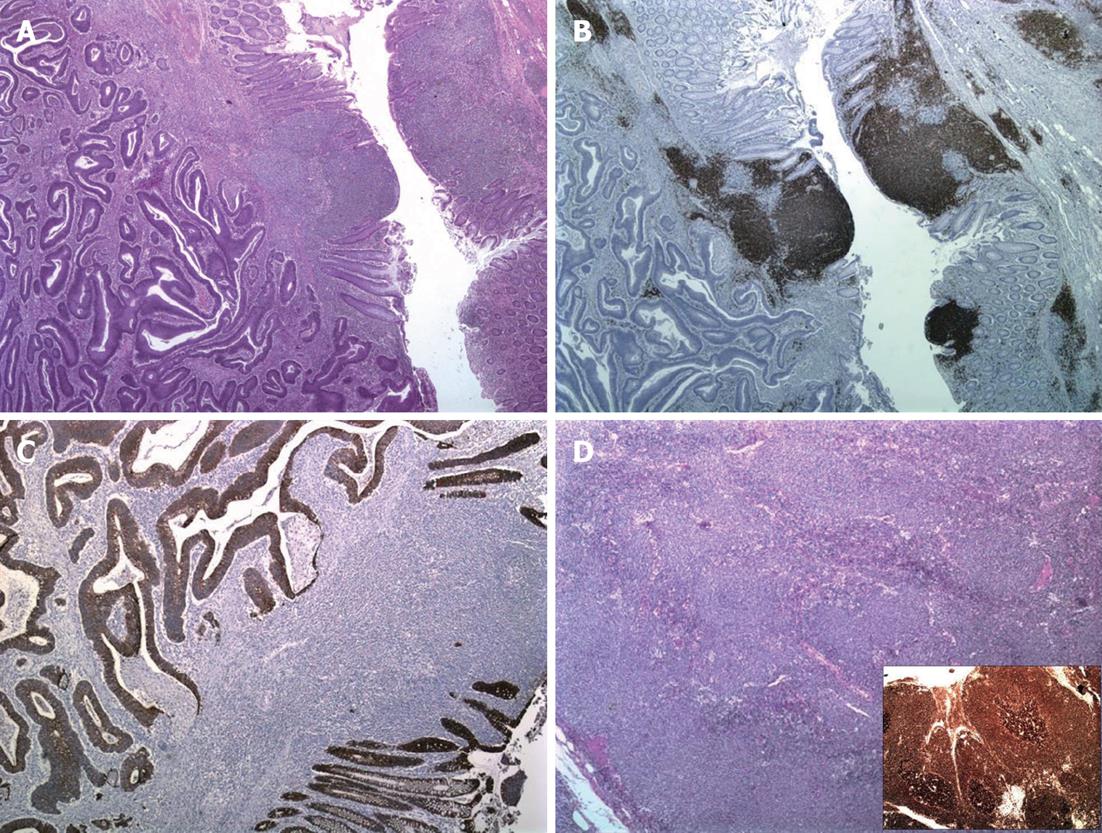
Case 2: Histology showed the colonic tumor to be a moderately differentiated adenocarcinoma infiltrating the colonic wall and the surrounding adipose tissue, but not extending to or beyond the serosa. Adjacent to the carcinoma, areas of extranodal marginal zone B-cell lymphoma (of MALT type) were identified (Figure 2A-C), involving 22 out of 34 totally excised colonic lymph nodes as well (Figure 2D). No bone marrow involvement was detected.
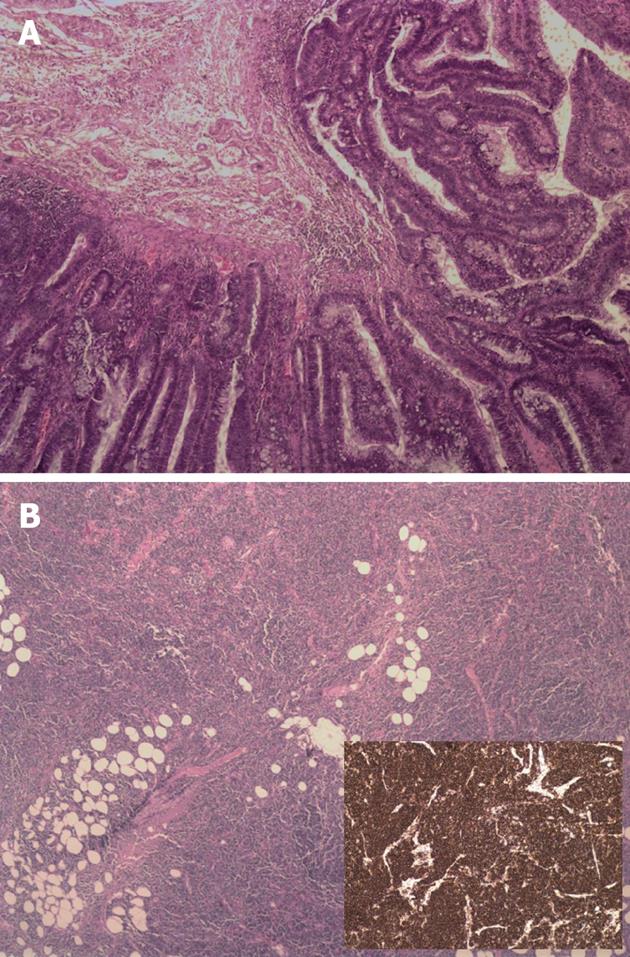
Case 3: Histological examination revealed a tubulovillous adenoma containing superficial foci of well differentiated colonic adenocarcinoma infiltrating the submucosa (Figure 3A). No secondaries were found in the 12 colonic lymph nodes retrieved; nevertheless, both these lymph nodes and a 5-cm large fragment of omentum were involved by an extranodal marginal zone B-cell lymphoma (of MALT type) (Figure 3B).
Our cases are, to the best of our knowledge, the second ever reported concerning simultaneous occurrence of adenocarcinoma and MALT lymphoma of the colon. Out of 13 cases of coexisting adenocarcinoma and lymphoma of the colon[3-13], only one is a MALT type lymphoma[3]; the rest usually deal either with another type of primary colonic lymphoma, mostly mantle cell lymphoma[5,9,11], or with involvement of the colon by an extracolonic lymphoma.
Two issues are to be noted: (1) whereas the presence of lymphocytes in the vicinity of colonic carcinomas is common, these cells are not always reactive. The presence of a dense lymphocytic infiltrate should therefore alert the pathologist to carefully assess its morphology, immunophenotype and clonality in order to rule out a coexisting MALT lymphoma; and (2) in a case when such a lymphoma is diagnosed, it is important to closely scrutinize colonic lymph nodes for their eventual involvement.
In all three cases, MALT lymphoma was only diagnosed in the excision specimen, with no previous clinical symptoms attributable to it. The simultaneous diagnosis of a lymphoma in a colectomy specimen led to a different post-operative work-up, including a bone marrow biopsy, in order to exclude extracolonic extension of the lymphoma.
Since no etiological factor for primary colonic lymphomas has been determined until now, its coexistence with colonic adenocarcinoma might rather be attributed to the advanced age of the patient in all cases.
Treatment of colon MALT lymphoma is not standard. However, there is a general agreement that surgical treatment alone is effective for localized disease, while combined chemotherapy is the mainstay for disseminated disease[16]. The role of inclusion of Rituximab (monoclonal anti-CD20 antibody) to the chemotherapy has not yet been commented on in this rare entity. In our case series, surgical resection was the only treatment for two patients with local disease, whereas the third patient, due to disseminated disease with bone marrow involvement, also received post-operative combined chemo-immunotherapy.
Peer reviewer: Satoru Takayama, MD, Department of Gastroenterological Surgery, Nagoya City University, 1 Kawasumi, Mizuho-cho, Mizuho-ku, Nagoya 467-8601, Japan
S- Editor Wang JL L- Editor Roemmele A E- Editor Zheng XM
| 1. | Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-2917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11128] [Cited by in RCA: 11831] [Article Influence: 845.1] [Reference Citation Analysis (4)] |
| 2. | Doolabh N, Anthony T, Simmang C, Bieligk S, Lee E, Huber P, Hughes R, Turnage R. Primary colonic lymphoma. J Surg Oncol. 2000;74:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Sahasrabudhe N, Khirwadkar N, Prescott R. Synchronous adenocarcinoma and marginal zone B-cell lymphoma of the colon: a case report. Diagn Histopath. 2009;15:318-322. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Mir-Madjlessi SH, Vafai M, Khademi J, Kamalian N. Coexisting primary malignant lymphoma and adenocarcinoma of the large intestine in an IgA-deficient boy. Dis Colon Rectum. 1984;27:822-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Padmanabhan V, Trainer TD. Synchronous adenocarcinoma and mantle cell lymphoma of the colon. Arch Pathol Lab Med. 2003;127:E64-E66. [PubMed] |
| 6. | Foltyn W, Kos-Kudła B, Siemińska L, Zemczak A, Strzelczyk J, Marek B, Kajdaniuk D, Nowak M, Borowska M, Jurecka-Lubienicka B. [Unique case of caecum plasmablastic lymphoma CD138(+) in patient with late diagnosed colon neuroendocrine carcinoma]. Endokrynol Pol. 2006;57:160-165. [PubMed] |
| 7. | Moriya Y, Koyama Y, Minato K, Shimoyama M, Hirota T, Itabashi M. [Coexisting malignant lymphoma and advanced adenocarcinoma of the colon--a case report]. Gan No Rinsho. 1985;31:894-899. [PubMed] |
| 8. | Quilon JM, Day S, Lasker JC. Synchronous tumors: Hodgkin disease presenting in mesenteric lymph nodes from a right hemicolectomy for colon carcinoma. South Med J. 2004;97:1133-1135. [PubMed] |
| 9. | Hopster D, Smith PA, Nash JR, Elders K, Poston GJ. Synchronous multiple lymphomatous polyposis and adenocarcinomata in the large bowel. Postgrad Med J. 1995;71:443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Mannweiler S, Dinges HP, Beham-Schmid C, Hauser H, Starlinger M, Regauer S. Colliding / concomitant tumors of the intestine: report of 3 cases. Pathol Oncol Res. 2003;9:188-192. [PubMed] |
| 11. | Kanehira K, Braylan RC, Lauwers GY. Early phase of intestinal mantle cell lymphoma: a report of two cases associated with advanced colonic adenocarcinoma. Mod Pathol. 2001;14:811-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Wagle SD, Mohandas KM, Vazifdar KF, Dhir V, Swaroop VS, Jagannath P, Desouza LJ. Synchronous adenocarcinoma and lymphoma of the colon. Indian J Gastroenterol. 1997;16:28-29. [PubMed] |
| 13. | Jaworski RC, Dowton B, Grant A, Gibson M, Chapuis PH, Pheils MT. Colorectal carcinoma and lymphoma. Aust N Z J Surg. 1982;52:37-38. [PubMed] |
| 14. | Rohatiner A, d'Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, Lister TA, Norton A, Salem P, Shipp M. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994;5:397-400. [PubMed] |
| 15. | Bancroft JD, Gamble M. Theory and Practice of Histological Techniques. Philadelphia: Churchill Livingstone Elsevier 2008; . |