Published online Jul 15, 2025. doi: 10.4251/wjgo.v17.i7.107460
Revised: April 19, 2025
Accepted: May 22, 2025
Published online: July 15, 2025
Processing time: 112 Days and 19.6 Hours
In this article, we comment on the work put forth by Wu et al regarding the investigation of oesophageal cancer-specific mortality for a cohort of patients from Chongqing University Cancer Hospital. We specifically focused on the implications of public health plans such as Urban Employee Basic Medical Insurance (UEBMI) and Urban Resident Basic Medical Insurance as well as out-of-pocket ratios on patient treatment plans regarding whether they pursue surgical interventions or therapeutic treatments such as chemotherapy. While Wu et al put forth potential explanations for why patients with the UEBMI plan surprisingly had a 23.30% increased risk of oesophageal cancer-specific death, more analysis is needed to alleviate cancer burden within this group. Although it is likely that patients covered by Urban Resident Basic Medical Insurance and higher out-of-pocket ratios have stronger self-recovery awareness, more work must be done to improve outcomes for people with the UEBMI plan while simultaneously imple
Core Tip: Despite comprising a fifth of the global population, China carries approximately half of oesophageal cancer burden. With nearly the entire Chinese population covered by public health insurance plans, investigating the impact of insurance type, demographic features, and clinical aspects of treatment on patient mortality is critical to enacting measures to alleviate the economic burden and mortality rate of oesophageal cancer. Recent findings highlight the need for unifying and addressing inequities among these insurance plans while promoting oesophageal cancer prevention and detection. Future directions include analyzing the efficacy of insurance plans for rural Chinese communities which carry a disproportionate cancer burden.
- Citation: Huilgol DK, Lucke-Wold B. Beyond numbers: Public health insurance and oesophageal cancer mortality risk. World J Gastrointest Oncol 2025; 17(7): 107460
- URL: https://www.wjgnet.com/1948-5204/full/v17/i7/107460.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i7.107460
Ranking seventh in global incidence and sixth in mortality worldwide, reducing oesophageal cancer is one of the biggest health challenges for the Chinese government, with Chinese cases comprising more than half of the global burden[1,2]. With the median age of diagnosis at 68 years of age, the oesophageal cancer burden in China coincides with the country’s rapidly aging population which is projected to become the world’s most aged society by 2050[3,4]. The country faces unique challenges in optimizing health insurance policies to advocate for prevention and earlier detection to reduce the economic burden and mortality risk caused by this disease, as the fragmentation of public health insurance along with greater burden in rural communities with less health coverage exacerbates the healthcare inequities that may be responsible for this disproportionate caner burden.
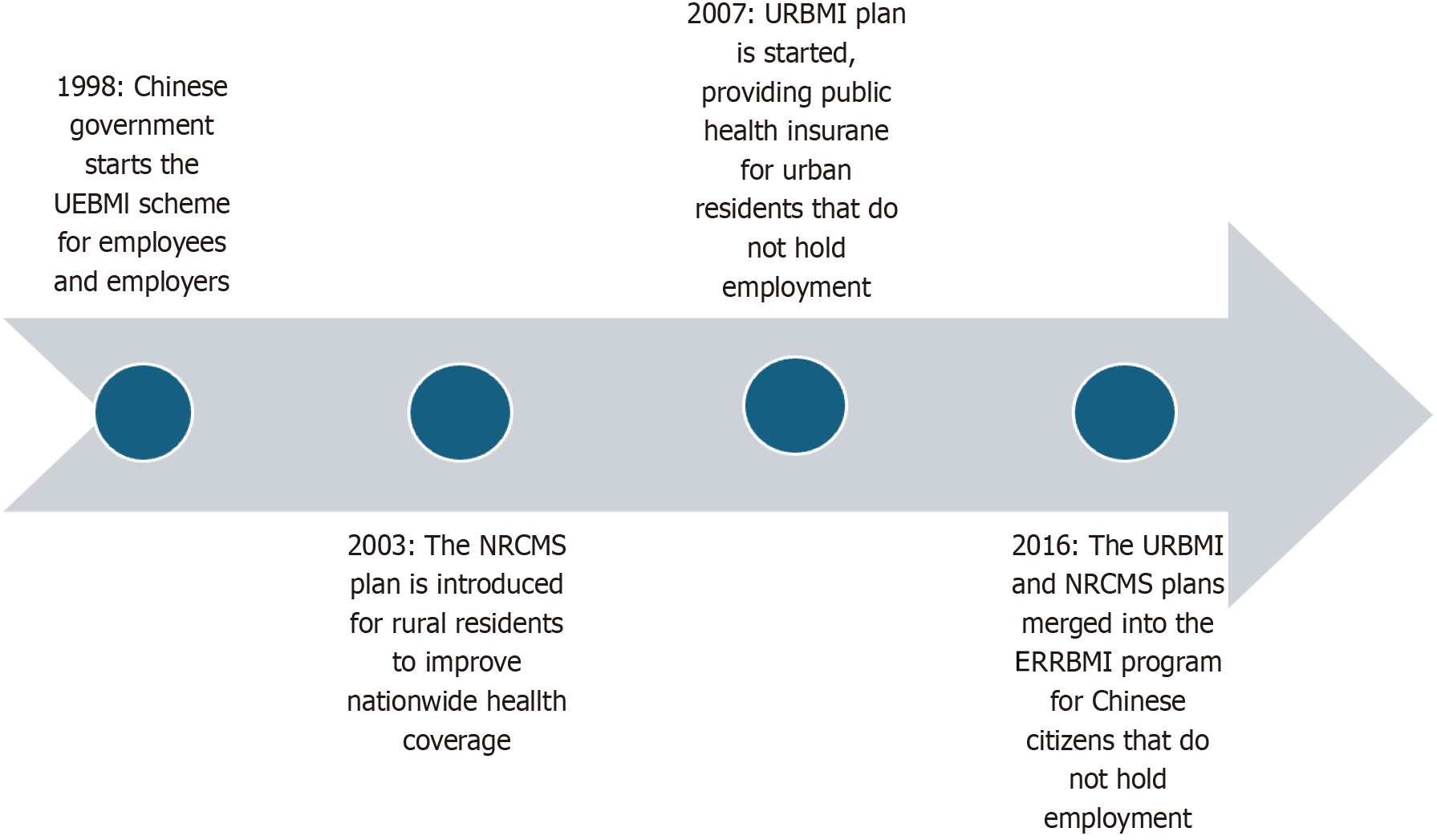
To combat this, China has made considerable changes in the last two decades by introducing distinct public health insurance plans covering up to 95% of the population to promote access to healthcare, with majority of people being covered by one of two major health insurance plans-Urban Employee Basic Medical Insurance (UEBMI) and Urban and Rural Resident Basic Medical Insurance[5]. The UEBMI plan was enacted in 1998 and covers urban employees living in public and private sectors, while the Urban and Rural Resident Basic Medical Insurance plan covers urban and rural residents that do not hold employment and is comprised of the Urban Resident Basic Medical Insurance (URBMI) plan and the New Rural Cooperative Medical System (NRCMS) (Figure 1)[5].
In this article, we delve into data from a cohort study by Wu et al[6] to investigate future directions for studies involving the impact the difference in these various public health insurance plans and out-of-pocket (OOP) ratios to assess their impact on oesophaeal cancer treatment modalities and mortality risk. We also emphasize the importance of future studies emphasizing unification of these health plans and specifically analyzing the impact of health insurance on rural Chinese communities, which often suffer higher oesophageal cancer-related mortality and incidence while having less medical insurance coverage[7].
To investigate the relationship between medical insurance and patient prognosis, Wu et al[6] collected data from a prospective cohort study in Chongqing, China from 2018-2020. With Chongqing being considered a large metropolis, the patients (n = 2543) that were diagnosed and primarily treated for oesophageal cancer at Chongqing University Cancer hospital primarily fell under the UEBMI and URBMI plans[6]. The cohort study encompassed the following: Demographic characteristics (age at diagnosis, gender, marriage, nation, insurance type, medical expenses), clinical features (underlying diseases, pathological types, cancer staging), treatment modalities (surgery, targeted therapy, immunotherapy, radiotherapy, chemotherapy), key biochemical indicators (body mass index, Karnofsky performance status, etc.), and follow-up information[6]. Upon recording these factors for each patient, Wu et al[6] utilized the χ2 and multivariate logistic regression tests as well as Cox proportional and competitive risk models to assess a potential difference among the patients’ demographic and clinical characteristics and calculate hazard ratios for all-cause death and oesophageal cancer-specific death for the different types of insurance and OOP ratios[6].
Results showed that patients with higher OOP ratios and patients under the URBMI plan had lower oesophageal cancer-specific mortality risk as well as lower all-cause mortality risk[6]. UEBMI funding primarily stems from employee and employer contributions while URBMI depends on government funding, with the latter often comprising of lower reimbursement rates that often place higher economic burden on the patient. Contrary to expectation, Wu et al[6] found that risk for oesophageal cancer-specific mortality increased by 23.30% for patients under UEBMI despite this group having higher reimbursement rates and that patients with higher OOP ratios. This may be due URBMI covering younger patients such as students and children that may not be affected by lifestyle factors that increase risk of having oesophageal cancer such as smoking or alcohol use. Although patients enrolled in UEBMI having higher reimbursement rates, they may have a higher risk of developing oesophageal cancer due to their age and lifestyle, which may account for the higher oesophageal cancer-specific mortality despite the higher insurance coverage.
The data provided by Wu and colleagues serves as reference for future studies that aim to measure the efficacy of initiatives that intends to bridge the inequities among these two plans. A significant value of this study was its ability to measure the effect of major health insurance plans on the affordability of available therapies for patients, which affected their prognoses. The cohort study was also valuable in that it assessed the joint effect of insurance type and OOP ratio on mortality risk for the patients with oesophageal cancer at Chongqing University Hospital[6]. While the Chinese government has been proactive in increasing accessibility to novel and effective therapies by introducing 111 new drugs as part of medications that are covered within these plans, research shows the need for the health insurance model to shift from emphasizing pay-for-service treatments to reinforcing the importance of covering outpatient procedures that emphasize prevention and treatment[6].
While these strengths of the cohort study do provide an analytical view into the Chinese healthcare system, the lack of detail or nuance regarding the factors surrounding the medical decisions made for patient treatments is a drawback that makes highlighting any specific consequences of the health insurance plan on patient prognosis difficult, while also preventing insights into potential regional differences in treatment plans. The use of Chongqing University Cancer Hospital - a metropolitan hospital that receives patient referrals from all over the Chongqing municipalities does allow researchers to base the study on a diverse patient population, with patients from rural and urban provinces alike.
However, a lack of emphasis on the rural Chinese population and omission of patients under NRCMS is also a significant limitation of this study, with rates of oesophageal cancer in rural areas being two to ten times higher than that of urban areas[8]. Because low-income and rural communities are often insured by NRCMS, the effects of this health insurance plan should be strongly considered when analyzing rural patient prognosis, as this health plan has significantly less funding and coverage for patients but has been shown to be instrumental in improving quality of life and medical care for rural communities[8,9]. Although the current infrastructure does offer some mode of economic relief for rural communities, NRCMS offers less generous benefits packages than the urban employee-based basic medical insurance scheme (UEBMI), especially for outpatient services. This disparity has led to difficulties in financial protection, particularly for patients with noncommunicable diseases[10]. Exploring inequities between urban and rural health insurance plans would be valuable in finding effective solutions to alleviate oesophageal cancer burden. Thus, the omission of NRCMS and its impacts on rural patient outcomes can potentially outweigh the health benefits observed with a reduction of mortality risk for patients under URBMI and patients with higher OOP ratios, as the former insures a larger percentage of the Chinese population with the most oesophageal-cancer burden as rural areas have a 2.01-fold oesophageal-cancer burden than urban areas[11]. Previous studies have also shown that NRCMS patients have higher hospitalization expenses, lower reimbursement ratios, and less coverage for high-value consumables, drugs, and surgical treatments for malignant cancer tumors[12]. Lastly, patients living in rural areas also have less opportunities for preventative screenings due to decreased access to medical centers making treatments and long-term care for chronic illnesses more difficult, which may also be contributing factors to worse health outcomes. Nevertheless, the work presented by Wu et al[6] serves as a valuable reference for future prospective cohort studies that aim to promote prevention and early detection and screening for rural communities to combat this inequity regarding oesophageal cancer in China.
Wu et al[6] proposed that patients covered by URBMI and those with a higher OOP ratio had better nutritional support, and participated in more rehabilitation exercises after their operations, which consequently resulted in a better surgical prognosis and lower mortality risk. This may be due to better standardized nutritional education and support initiatives for the retired elderly and for the younger individuals that are primarily covered by this plan or other governmental efforts across China. UEBMI also does not fully cover nutritional support services comprehensively as it is seen as supplementary to the primary treatment. The impact of health insurance plans on the importance of nutrition when undergoing treatment for oesophageal cancer treatment is an important angle for researchers to consider, as 40%-60% of patients are diagnosed with malnutrition upon diagnosis of oesophageal cancer[13]. Evidence-based research about how nutrition can vary among patients with under different medical insurance plans and among patients from rural vs urban areas could be beneficial in understanding the importance of preventative measures in alleviating oesophageal cancer burden in China.
The lack of coverage for high value consumables and drugs as well as surgical interventions under health plans negatively affects the prognoses of patients that cannot afford to pay high OOP ratios[6]. UEBMI can be said to incentivize treatments that have higher reimbursement rates, with typically prescribed drugs, surgeries, and treatments already covered by the government, prompting fee-for-service treatments over what is personalized and optimal for the patient. Patients under URBMI and higher OOP ratios opted for surgical interventions and had lower risk of oesophageal cancer-related mortality. This could be partly due to patients in that group being able to afford personalized care alongside surgical interventions that were covered with their plan. Patients with higher OOP costs can often afford the one-time cost of a surgery that has a higher chance of being covered within their health plan, with the surgical intervention itself outweighing the long-term costs of chemotherapies and drugs that may not be insured if recently introduced to market. Wu and colleagues also noted that patients who undergo surgical interventions first have lower mortality rates, which may also be due in part due to surgical candidates being deemed to be fit to survive the procedure, potentially denoting earlier-stage intervention. China’s health insurance plans have billing systems that have patients pay for procedures and drug treatments, with average medical expenditure per patient for esophageal cancer was 72.9% of the average family annual income for urban households[14]. This poses negative consequences for clinical outcomes, as it increases economic burden on patients and families while disincentivizing the need for oesophageal cancer prevention and early screening. Future research must investigate the value of shifting Chinese public health insurance plans to focus on outpatient procedures that seek to screen or prevent late-stage diagnosis of oesophageal cancer, particularly in rural communities that have higher incidence and mortality rates.
All in all, Wu et al[6] have put forth data that critically analyzes the impact of fragmented public health insurance plans on oesophageal cancer-specific economic burden and patient prognosis. By offering an opportunity for medical providers to analyze the values, limitations, and impact of domestic health insurance plans on outcomes for patients with oesophageal cancer, this study aims to explore the efficacy of national health expenditure and infrastructure. Such analysis should be performed to understand the limitations of health insurance systems across the globe - especially for countries that provide insurance-dependent care without universal coverage such as the United States, for which cancer is a leading cause of death. Broader implications of this study on the American healthcare model would comprise of understanding the impact of OOP ratio on cancer survival rates, with lack of affordability coinciding with lower survival rates in the United States for chronic illnesses such as cancer that require multiple treatments and medications. Understanding the benefit of insurance policies that offer universal coverage without disparity between income groups in countries such as Finland would also aid in implementation of more equitable insurance policies across employee status and urban-rural divides.
These results call for domestic and international cooperation in effectively reducing the economic burdens and alleviating mortality risk in oesophageal cancer patients in China by shifting healthcare policies to emphasize prevention and early detection instead of only covering specific treatments and procedures. While the Chinese government’s recent efforts to incorporate high-end drugs and surgeries into their health coverage do alleviate costs, patients would highly benefit from health insurance plans that comprehensively cover outpatient procedures and preventative care as well as treatment procedures. Along with exploring the values of such a shift in health insurance policy, future studies should also aim to further reduce healthcare inequities in rural China, as NRCMS does not provide rural patients with comparable coverage for treatment as the urban health insurance plans, despite rural communities facing higher mortality from oesophageal cancer.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64684] [Article Influence: 16171.0] [Reference Citation Analysis (177)] |
| 2. | Zhu H, Ma X, Ye T, Wang H, Wang Z, Liu Q, Zhao K. Esophageal cancer in China: Practice and research in the new era. Int J Cancer. 2023;152:1741-1751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 99] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 3. | Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4235] [Cited by in RCA: 11437] [Article Influence: 3812.3] [Reference Citation Analysis (4)] |
| 4. | Lopreite M, Zhu Z. The effects of ageing population on health expenditure and economic growth in China: A Bayesian-VAR approach. Soc Sci Med. 2020;265:113513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Zhang J, Zhao D, Zhang X. China's universal medical insurance scheme: progress and perspectives. BMC Glob Public Health. 2024;2:62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 6. | Wu XL, Li XS, Cheng JH, Deng LX, Hu ZH, Qi J, Lei HK. Oesophageal cancer-specific mortality risk and public health insurance: Prospective cohort study from China. World J Gastrointest Oncol. 2025;17:103629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Chen R, Zheng R, Zhang S, Wang S, Sun K, Zeng H, Li L, Wei W, He J. Patterns and trends in esophageal cancer incidence and mortality in China: An analysis based on cancer registry data. J Natl Cancer Cent. 2023;3:21-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 46] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 8. | Lin Y, Totsuka Y, Shan B, Wang C, Wei W, Qiao Y, Kikuchi S, Inoue M, Tanaka H, He Y. Esophageal cancer in high-risk areas of China: research progress and challenges. Ann Epidemiol. 2017;27:215-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 155] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 9. | Zeng H, Ran X, An L, Zheng R, Zhang S, Ji JS, Zhang Y, Chen W, Wei W, He J; HBCR Working Group. Disparities in stage at diagnosis for five common cancers in China: a multicentre, hospital-based, observational study. Lancet Public Health. 2021;6:e877-e887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 115] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 10. | Meng Q, Fang H, Liu X, Yuan B, Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. 2015;386:1484-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 349] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 11. | Liao Y, Li C, Xia C, Zheng R, Xu B, Zeng H, Zhang S, Wang J, Chen W. Spatial distribution of esophageal cancer mortality in China: a machine learning approach. Int Health. 2021;13:70-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Fu R, Lin Z, He F, Jiang Y, Zheng Z, Hu Z. Trend of disparity between coastland and inland in medical expenditure burden for rural inpatients with malignant tumor in southeast of China from 2007 to 2016. BMC Cancer. 2020;20:295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 13. | Cao J, Xu H, Li W, Guo Z, Lin Y, Shi Y, Hu W, Ba Y, Li S, Li Z, Wang K, Wu J, He Y, Yang J, Xie C, Zhou F, Song X, Chen G, Ma W, Luo S, Chen Z, Cong M, Ma H, Zhou C, Wang W, Qi Luo, Shi Y, Qi Y, Jiang H, Guan W, Chen J, Chen J, Fang Y, Zhou L, Feng Y, Tan R, Ou J, Zhao Q, Wu J, Xin Lin, Yang L, Fu Z, Wang C, Deng L, Li T, Song C, Shi H; Investigation on Nutrition Status and Clinical Outcome of Common Cancers (INSCOC) Group, Chinese Society of Nutritional Oncology. Nutritional assessment and risk factors associated to malnutrition in patients with esophageal cancer. Curr Probl Cancer. 2021;45:100638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 14. | Guo LW, Huang HY, Shi JF, Lv LH, Bai YN, Mao AY, Liao XZ, Liu GX, Ren JS, Sun XJ, Zhu XY, Zhou JY, Gong JY, Zhou Q, Zhu L, Liu YQ, Song BB, Du LB, Xing XJ, Lou PA, Sun XH, Qi X, Wu SL, Cao R, Lan L, Ren Y, Zhang K, He J, Zhang JG, Dai M; Health Economic Evaluation Working Group, Cancer Screening Program in Urban China (CanSPUC). Medical expenditure for esophageal cancer in China: a 10-year multicenter retrospective survey (2002-2011). Chin J Cancer. 2017;36:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |