Published online Feb 15, 2025. doi: 10.4251/wjgo.v17.i2.101211
Revised: November 6, 2024
Accepted: December 9, 2024
Published online: February 15, 2025
Processing time: 132 Days and 19.2 Hours
Recently, there has been a significant increase in the consumption of ultra-processed foods worldwide. However, the association between the consumption of ultra-processed food, obesity, and the prevalence of colon cancer remains controversial.
To find out the association between the consumption of ultra-processed food, obesity, and the prevalence of colon cancer.
A comprehensive systematic literature search of PubMed, Scopus, Web of Science, and Google Scholar for grey literature was done for articles published before 8th March 2023. The search was done to retrieve potential peer-reviewed articles that explored the association between the consumption of ultra-processed food, obesity, and the prevalence of colon cancer.
Of the 246 potential articles assessed, 17 met the inclusion criteria. Meta-analysis results demonstrated that high consumption of ultra-processed food is associated with an increased risk of obesity [odds ratio (OR): 1.65; 95%CI: 1.07-2.45; P < 0.05]. Consequently, there is a positive association between obesity and an increased risk of colon cancer (OR 1.48; 95%CI: 0.77-2.87; P > 0.05).
Consuming ultra-processed foods increases the risk of obesity and colon cancer.
Core Tip: High consumption of ultra-processed foods is significantly associated with an increased risk of obesity and colon cancer. Our systematic review and meta-analysis, which included 17 peer-reviewed studies, found that individuals with a high intake of ultra-processed foods had a 65% higher likelihood of developing obesity. Reducing the intake of these foods and promoting a diet rich in fruits, vegetables, and whole grains are essential strategies to mitigate obesity and cancer risk. Public health initiatives may further support these efforts.
- Citation: Tin J, Lee H, Trejo AG, Tin K. Ultra-processed food, obesity, and colon cancer: A systematic review and meta-analysis. World J Gastrointest Oncol 2025; 17(2): 101211
- URL: https://www.wjgnet.com/1948-5204/full/v17/i2/101211.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i2.101211
The global consumption of ultra-processed foods (UPFs) has surged in recent years, leading to widespread concerns about their health implications. UPFs are food products heavily processed from industrial formulations of substances derived from foods, often enhanced with additives, preservatives, and flavorings. Examples of UPFs include soda, candy, chips, and frozen dinners[1]. These foods are typically high in calories, added sugars, and unhealthy fats and low in essential nutrients such as fiber, vitamins, and minerals[1]. The high caloric content of UPFs can contribute to weight gain and obesity, increasing the risk of colon cancer.
Studies have shown that consumption is associated with an increased risk of obesity, type 2 diabetes, and other chronic diseases, including colon cancer[2]. Obesity is a major risk factor for colon cancer, and the prevalence of both obesity and colon cancer has increased globally. According to the World Health Organization, over 650 million adults are obese worldwide, a number projected to exceed 1.1 billion by 2030[3]. Concurrently, colon cancer incidence has risen by 2%-3% annually in countries such as the United States, Canada, and Australia[4]. These trends suggest a potential link between UPF consumption, obesity, and colon cancer.
Several studies reinforce this association. Fiolet et al[4] found that a 10% increase in UPFs in the diet was associated with a 12% increased risk of obesity, while Mendonça et al[5] reported a 33% higher risk of obesity for individuals consuming the highest levels of UPFs compared to the lowest. Regarding colon cancer, Srour et al[6] observed that a 10% increase in UPF consumption was linked to a 10% increased risk of colon cancer, while Schnabel et al[7] found a 30% higher risk for individuals consuming the highest UPFs. Animal studies, such as Zong et al[8], support these findings, showing that diets high in UPFs increase colon tumor incidence in experimental models.
Despite the evidence, uncertainties remain. The specific mechanisms linking UPFs to colon cancer, as well as their differential impacts across diverse populations, remain underexplored. Moreover, many studies rely on cross-sectional designs, limiting their ability to establish causality or assess long-term effects. Most existing research also focuses on Western populations, leaving gaps in understanding how UPFs influence health in other regions with differing dietary patterns and genetic predispositions.
Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines[9] were used to identify published studies on the association between the consumption of UPF, obesity, and the prevalence of colon cancer. Articles fulfilling the modified population, intervention, comparison, primary outcomes, study design (PICOS) criteria were chosen[10]. The PICOS criteria for eligible studies were defined as follows: (1) Population (P): All patients involved in the assessment of the association between consumption of UPF, obesity, and the prevalence of colon cancer; (2) Intervention (I): Reduced or low consumption of UPF; (3) Comparison (C): High vs low consumption of UPF and its association with obesity and prevalence of colon cancer; (4) Primary outcomes (O): Overweight, obesity, and prevalence of colon cancer; and (5) Study design (S): Most included studies were cross-sectional or prospective. However, there were no restrictions to study design.
A comprehensive systematic literature search of PubMed, Scopus, Web of Science, and Google Scholar for grey literature was done for articles published before 8th March 2023. The search was done to identify potential peer-reviewed articles that explored the association between the consumption of UPF, obesity, and the prevalence of colon cancer. The following keywords and medical sub-headings were used simultaneously in each set: ("Colon cancer" OR "Colorectal cancer" OR "Rectum cancer" OR "Rectal cancer”) AND (obesity OR Overweight OR fatness) OR ("Colon cancer" OR "Colorectal cancer" OR "Rectum cancer" OR "Rectal cancer”) AND (“Processed food" OR "Ultra-processed food" OR "Junk food" OR "Canned food") OR (obesity OR Overweight OR fatness) AND (“Processed food" OR "Ultra-processed food" OR "Junk food" OR "Canned food"). Synonyms and alternative spellings were considered. The keywords were used exhaustively in different combinations in different electronic databases.
Eligible studies included in this review met the following inclusion criteria: They were scholarly articles; they were published in the English language or could be translated into the English language; they explored the association between consumption of UPF, obesity, and the prevalence of colon cancer; they were conducted on humans. Ineligible studies were excluded due to the following reasons: They were duplicates or continued work of previous publications; they were reviews, meta-analyses, protocols, bibliometric analyses, opinion pieces abstracts, or editorial articles; they had no methods and results; they explored the association between consumption of UPF, obesity, and other types of cancers other than colon cancer; they were conducted in non-humans or animals such as mice.
Upon finalizing the initial search strategy, a study selection was carried out following a step-by-step process. Duplicated references were deleted using the Zotero reference manager, and the remaining studies for review were included in the screening stages. All potential scholarly articles were reviewed. Titles and abstracts were first screened to remove inappropriate studies. Full texts of the remaining studies were additionally assessed based on the current inclusion and exclusion criteria. Data were extracted using a carefully designed form with crucial search terms. Relevant studies were evaluated for accuracy.
Eligible studies that met the inclusion were critically checked for quality. The Joanna Briggs Institute (JBI) Critical Appraisal Checklist for the analytical cross-sectional study was used to independently assess and confirm the included studies' accuracy[11]. The JBI Critical Appraisal Checklist for analytical cross-sectional studies’ bias criteria revolves around inclusion and exclusion criteria, subject setting description, confounding factors, outcome measures, and statistical analysis methods employed. The judgment is either yes, no, unclear, or not applicable[11].
The characteristics (Author, publication year, the number of participants, age range, study design, study region, outcome, and significant findings) were extracted and summarized in the study descriptor table (Table 1)[5,7,12-26]. Homogeneous studies regarding statistical methods and outcome measures were pooled, and a meta-analysis was conducted using odds ratios (OR) and a 95%CI. Studies regarded as heterogeneous based on statistical approaches and outcome measures were excluded from the meta-analyses. Most studies categorized food according to the NOVA food classification system[1]. Body mass index (BMI) less than 18.5 kg/m3 was considered underweight, a BMI of 18.5 to < 25 kg/m3 - was a healthy weight, a BMI of 25 to 30 kg/m3 - was considered overweight, and a BMI > 30 kg/m3 - was considered obese.
| Ref. | Study design | No. of participants | Study region | Age range | Outcome | Major findings |
| Wang et al[12], 2022 | Three prospective cohorts | Men (n = 46341), women (n = 159907) | United States | 30-55, 25-42, 40-75 | Compared with those in the lowest fifth of ultra-processed food consumption, men in the highest fifth of consumption had a 29% higher risk of developing colorectal cancer | High consumption of whole ultra-processed foods in men and specific subgroups of ultra-processed foods in men and women was associated with an increased risk of colorectal cancer |
| Oxentenko et al[13], 2010 | Prospective study | 36941 women | Mayo Clinic Rochester and the University of Minnesota, United States | 55-69 | Baseline height, weight, BMI, hip circumference, waist circumference, and WHR were all positively associated with incident colorectal cancer | A strong association between body size and colorectal cancer risk among older women |
| Romaguera et al[14], 2021 | Case-control | 1852 | Spain | 20-85 | Consumption of ultra-processed foods and drinks was associated with a higher risk of colorectal cancer (OR for a 10% increase in consumption | Results suggest an association between the consumption of ultra-processed foods and drinks, and colorectal cancer |
| Terry et al[15], 2002 | Prospective cohort study | 89835 women | Canada | 40-59 | Obesity was associated with an increased risk of colorectal cancer among premenopausal women at baseline. There was no association among postmenopausal women | Obesity is associated with an increased risk of colorectal cancer in premenopausal women but is not associated with altered risk in postmenopausal women |
| Movahedi et al[16], 2015 | Prospective study | 937 | Unspecified | Median 44.9 | During follow-up, 55 of 937 participants developed CRC. For obese participants, CRC risk was 2.41 × (95%CI: 1.22-4.85) more significant than underweight and normal-weight participants | Obesity is associated with substantially increased CRC risk in patients with LS, but this risk is abrogated in those taking aspirin |
| Kitahara et al[17], 2013 | Prospective study | 966 | United States | 55-74 | Compared with normal-weight men (18.5-24.9 kg/m2), obese men (≥ 30 kg/m2) had a significantly higher risk of incident adenoma (OR, 1.32; 95%CI: 1.06-1.65) and colorectal cancer | Obesity is critical throughout the natural history of colorectal cancer, at least in men. Colorectal cancer prevention efforts should encourage achieving and maintaining a healthy body weight in addition to regular screenings |
| Anderson et al[18], 2014 | Multicentre, parallel-group, randomized controlled trial | 329 | Scotland | 50-74 | Differences between groups were significant for waist circumference, body mass index, blood pressure, blood glucose level, diet, and physical activity. No reported adverse events were related to trial participation | Significant weight loss can be achieved by a diet and physical activity intervention offering considerable potential for risk reduction of disease in older adults |
| Flaherty et al[19], 2018 | Prospective study | 70 | United States | Mean 66.1 | Patients with mismatch repair-deficient tumors (n = 11) had a lower mean BMI than those with mismatch repair-proficient tumors (n = 59) (22.16 vs 26.30 kg/m2, respectively; P = 0.029) | Tumor mismatch repair status and obesity are correlated in patients with colon cancer; increased |
| Hall et al[20], 2019 | RCT | 20 | Unspecified | Mean 31.2 | Weight changes were highly correlated with energy intake (r = 0.8, P < 0.0001), with participants gaining 0.9 ± 0.3 kg (P = 0.009) during the ultra-processed diet and losing 0.9 ± 0.3 kg (P = 0.007) during the unprocessed diet | Limiting the consumption of ultra-processed foods may be an effective strategy for obesity prevention and treatment |
| Canella et al[21], 2014 | Cross-sectional study | 55970 | Brazil | Unspecified | Compared with those in the lower quartile, people in the upper quartile of household consumption of ultra-processed products were 37% more likely to be obese | Greater household availability of ultra-processed food products in Brazil is positively and independently associated with a higher prevalence of excess weight and obesity |
| Silva et al[22], 2018 | Cross-sectional study | 45 | Brazil | 35-64 | Individuals in the fourth quartile of percentage energy contribution from ultra-processed foods presented a higher BMI and WC and higher chances of being overweight or obese and having significantly increased WC compared with those in the first quartile | Results indicate the existence of associations between more significant energy contributions from ultra-processed foods and higher BMI and WC, which are independent of total energy intake |
| Louzada et al[23], 2015 | Cross-sectional study | 30243 | Brazil | ≥ 10 | Ultra-processed foods represented 30% of the total energy intake. Those in the highest quintile of consumption of ultra-processed foods had significantly higher body-mass-index and higher odds of being obese and excess weight compared with those in the lowest quintile of consumption | Findings support the role of ultra-processed foods in the obesity epidemic in Brazil |
| Nardocci et al[24], 2019 | Cross-sectional study | 19363 | Canada | 18 or more | Individuals in the highest quintile of ultra-processed food consumption were 32% more likely to have obesity than those in the first quintile | Ultra-processed food consumption is positively associated with obesity |
| Juul et al[25], 2018 | Cross-sectional study | 15977 | United States | 20–64 | Individuals in the highest quintile of ultra-processed food consumption were 32% more likely to have obesity than those in the first quintile | Findings support that higher consumption of ultra-processed food is associated with excess weight and that the association is more pronounced among women |
| Rauber et al[26], 2020 | Cross-sectional study | 6143 | United Kingdom | 19-96 | The consumption of ultra-processed food was associated with increased BMI and obesity in both sexes | Higher consumption of ultra-processed food is associated with greater adiposity in the United Kingdom adult population. Policymakers should consider actions that promote the consumption of unprocessed or minimally processed foods and reduce the consumption of ultra-processed foods |
| Schnabel et al[7], 2019 | Prospective cohort study | 44551 | France | 45 or older | A 10% increase in the proportion of ultra-processed food consumption was statistically significantly associated with a 14% higher risk of all-cause mortality | An increase in ultra-processed food consumption is associated with higher mortality |
| Mendonça et al[5], 2016 | Prospective cohort study | 8451 | Spain | Unspecified | A total of 1939 incident cases of overweight and obesity were identified during follow-up. After adjustment for potential confounders, participants in the highest quartile of ultra-processed food consumption were at a higher risk of developing overweight or obesity | Ultra-processed food consumption was associated with a higher risk of being overweight and obese |
Table 1 provides an overview of the included studies. These studies were published between 2010 and 2022. Over 70% of the studies were published in the last six years. A total of 517941 patients were included across all the studies. Most patients were women with an average age of over 55 years. The included studies were conducted in Europe, North America, and South America. Eight of the 15 included studies were prospective, 6 were cross-sectional studies, two were Randomized Controlled Trials, and one was a case-control study.
The included studies shown in Table 2 demonstrated high methodological quality overall, with all meeting criteria for clear inclusion criteria, detailed study settings, valid exposure and outcome measurements, and appropriate statistical analysis. However, four studies did not adequately address confounding factors or report strategies to manage them, which may impact the validity of their findings. Limitations were observed in studies such as Movahedi et al[16] and Kitahara et al[17], which failed to address confounding factors despite strengths in other domains. Most studies were conducted in Western populations, limiting generalizability to other settings.
| Ref. | Q1: Inclusion criteria | Q2: Subject setting | Q3: Valid exposure measurement | Q4: Standard outcome criteria | Q5: Confounding factors identified | Q6: Strategies for confounding | Q7: Valid outcome measurement | Q8: Statistical analysis |
| Wang et al[12], 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Oxentenko et al[13], 2010 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Romaguera et al[14], 2021 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Terry et al[15], 2002 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Movahedi et al[16], 2015 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Kitahara et al[17], 2013 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Anderson et al[18], 2014 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Flaherty et al[19], 2018 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Hall et al[20], 2019 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Canella et al[21], 2014 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Silva et al[22], 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Louzada et al[23], 2015 | Yes | Yes | Yes | Yes | No | Not applicable | Yes | Yes |
| Nardocci et al[24], 2019 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Juul et al[25], 2018 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Rauber et al[26], 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Schnabel et al[7], 2019 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mendonça et al[5], 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
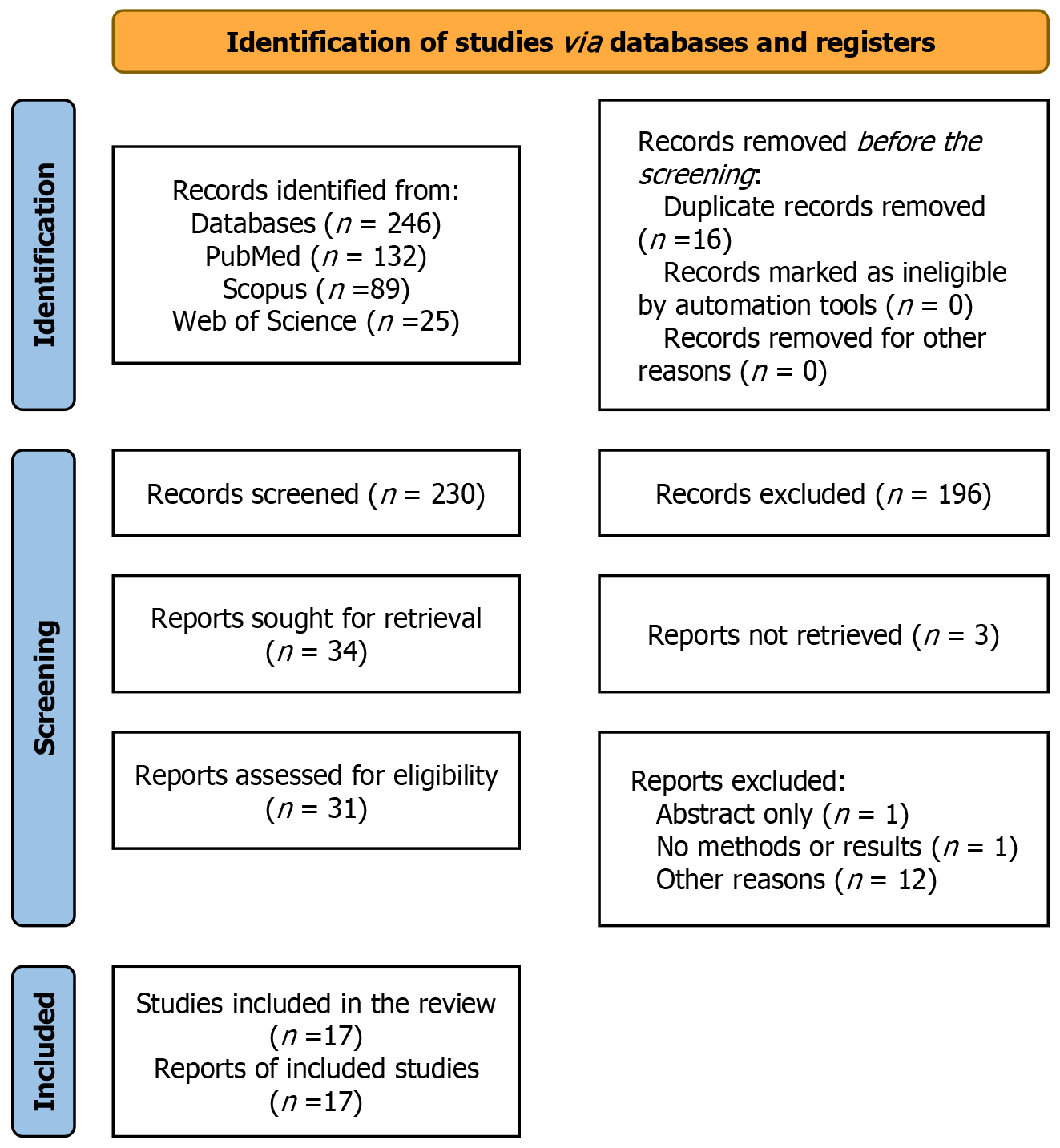
Database search yielded 246 articles, out of which 16 duplicates were eliminated. The title and abstract screening conducted removed 196 articles. Thirty-four articles were sought for retrieval. Three articles could not be retrieved. Thirty-one articles were assessed for eligibility. Fourteen articles were eliminated as they needed to meet the stipulated inclusion criteria. Seventeen articles were considered eligible for review after the screening, as indicated in Figure 1.
Event numbers of obesity, overweight, and colon cancer cases were pooled from the eligible studies. All data were statistically analyzed using Review Manager Version 5.4.1 for Windows, an open-source statistical analysis software (The Cochrane Collaboration, Oxford, United Kingdom). Heterogeneity between studies was assessed through χ2 analysis. A P value less than 0.05 was considered statistically significant.
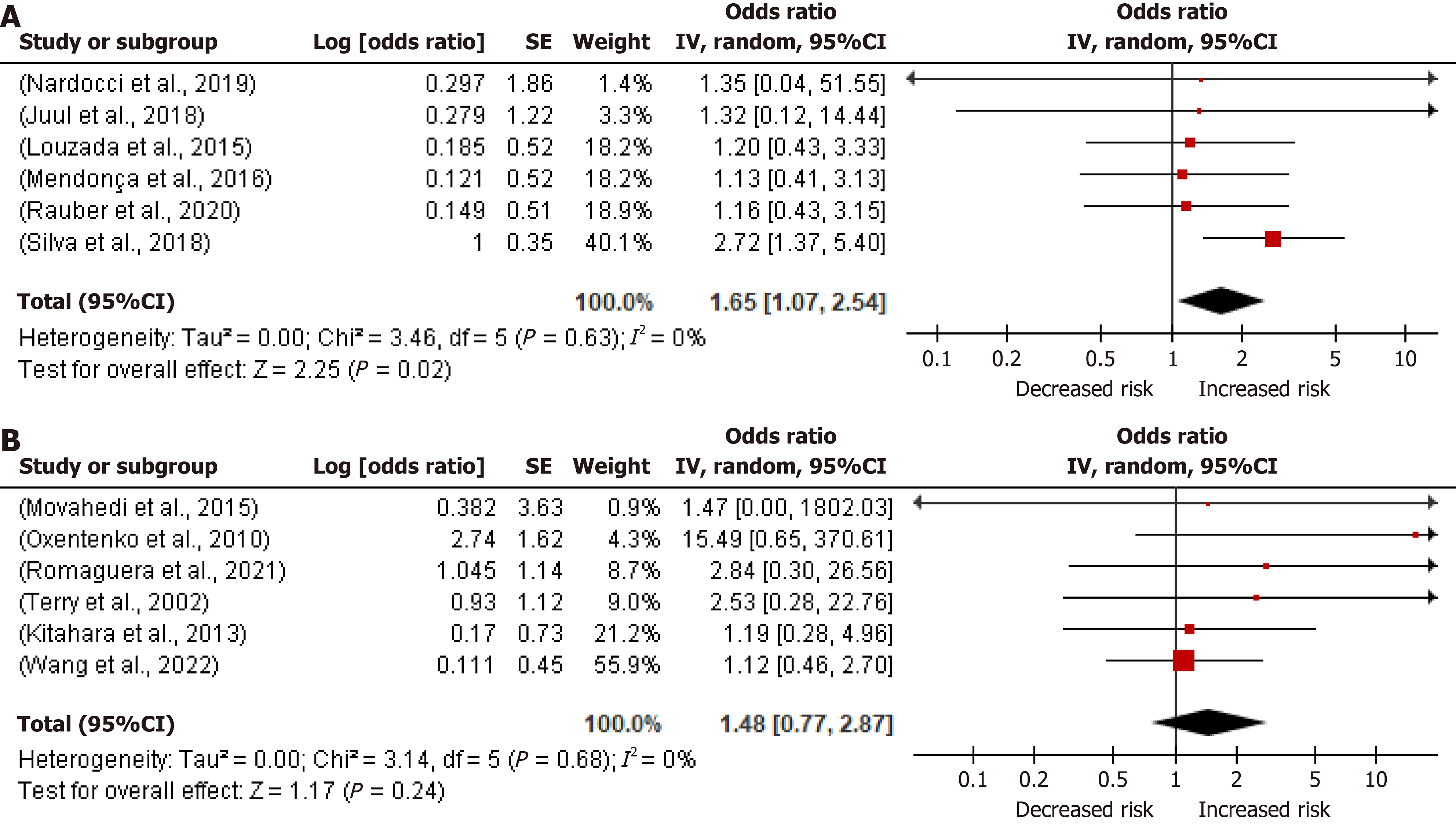
Six studies (Figure 2A) assessed the outcome of the association between higher vs lower consumption of UPF and obesity risk in adults. All the studies were individually significant (P < 0.05). Silva et al[22] had the highest precision (40.1%), while Nardocci et al[24] had the lowest precision (1.4%). A random effect model was used; the pooled summary effect was 1.65, and the 95%CI was 1.07 and 2.54. The included studies had low heterogeneity P = 0.63 and I2 = 0%. Overall effect Z = 2.25 (P = 0.02). The overall results show that high consumption of UPF is associated with an increased risk of obesity in adults (OR: 1.65; 95%CI: 1.07-2.45; P < 0.05).
Some studies assessed the outcome of the association between obesity vs healthy weight and colon cancer risk in adults (Figure 2B). Wang et al[12] had the highest precision (55.9%), while Movahedi et al[16] had the lowest precision (0.9%). A random effect model was used, the pooled summary effect was 1.48, and the 95%CI was 0.77 and 2.87. The included studies had low heterogeneity P = 0.68 and I2 = 0%. Overall effect Z = 1.17 (P = 0.24). The overall results demonstrate a positive association between obesity and an increased risk of colon cancer in adults (OR: 1.48; 95%CI: 0.77-2.87; P > 0.05). However, the results are insignificant.
This systematic review and meta-analysis provide a comprehensive synthesis of quantitative and qualitative data on the association between UPF consumption, obesity, and colon cancer risk in adults. Our findings indicate that high UPF intake is significantly associated with an increased risk of obesity (OR: 1.65; 95%CI: 1.07-2.45; P < 0.05). This suggests a direct positive relationship between elevated UPF consumption and the prevalence of overweight (BMI of 25 to 30 kg/m²) and obesity (BMI > 30 kg/m²). Furthermore, our analysis reveals a positive association between obesity and an increased risk of colon cancer in adults (OR: 1.48; 95%CI: 0.77-2.87; P > 0.05); however, this result is not statistically significant and should be interpreted with caution.
Our findings align with previous studies that have identified a link between UPF consumption and adverse health outcomes. For instance, Fiolet et al[4] reported that a 10% increase in the proportion of UPFs in the diet was associated with a 12% increase in the risk of obesity. Similarly, Mendonça et al[5] found that individuals with the highest UPF intake had a 33% higher risk of obesity compared to those with the lowest intake. In terms of cancer risk, Srour et al[6] demonstrated that a 10% increase in UPF consumption correlated with a similar increase in colon cancer risk. Schnabel et al[7] also observed that individuals with the highest UPF consumption had a 30% higher risk of colon cancer than those with the lowest consumption.
A systematic review and meta-analysis by Shu et al[27] highlighted that higher UPF consumption is linked to a significantly increased risk of colorectal cancer. This study also emphasized the role of food additives and processing methods in influencing cancer risk. Similarly, Lian et al[28] demonstrated a robust association between UPF consumption and cancer risk, particularly colorectal cancer, underscoring the importance of dietary interventions. In line with these findings, Pagliai et al[29] found that higher UPF consumption is associated with increased risks of obesity and related metabolic disorders. These results corroborate our analysis, which identifies obesity as a key intermediary in the relationship between UPF consumption and colon cancer risk.
Furthermore, Chang et al[30], using data from the United Kingdom Biobank, reported a strong link between UPF consumption, cancer risk, and cancer mortality, further validating the significance of dietary quality in disease prevention. Vitale et al[31] also highlighted the dose-response relationship between UPF intake and chronic disease risks, including obesity and colorectal cancer, while emphasizing the need for population-wide dietary shifts. These findings collectively reinforce the evidence base for reducing UPF intake as part of public health strategies.
The high caloric content, added sugars, and unhealthy fats prevalent in UPFs contribute to weight gain and obesity, which are significant risk factors for colon cancer. Moreover, the elevated levels of fat, sugar, and salt in these foods may promote inflammation, insulin resistance, and oxidative stress, all of which are known to facilitate carcinogenesis[32]. The presence of certain food additives in UPFs, such as titanium dioxide, has been implicated in disrupting gut microbiota and enhancing inflammatory processes, thereby increasing cancer risk.
Given the escalating prevalence of obesity and colon cancer, particularly in developed countries, there is an urgent need to mitigate these risks through dietary and lifestyle modifications. Individuals should be encouraged to consume diets rich in fruits, vegetables, whole grains, and lean proteins while limiting UPF intake[33]. Public health initiatives and policies are crucial in reducing UPF consumption and promoting healthier dietary choices. Addressing the association between UPF intake, obesity, and colon cancer is essential for reducing disease burden and fostering a healthier future for all.
This analysis has several limitations. Many included studies were cross-sectional, and the dietary patterns assessed may not accurately reflect habitual intake, underscoring the need for longitudinal studies with repeated dietary nutritional evaluations. Variations in the classification and analysis of UPFs across studies pose challenges in drawing definitive conclusions about the specific quantity of UPF consumption that leads to adverse health outcomes. Additionally, the observational nature of most studies limits the ability to establish causation. Language restrictions and relatively small sample sizes in some studies may also affect the generalizability of the findings.
Obesity, overweight, and the risk of colon cancer can be minimized by reducing the consumption of UPF and promoting a healthy diet and lifestyle. The diet should contain fruits, vegetables, whole grains, and lean proteins. Public health initiatives and government policies may also play a crucial role in reducing the consumption of UPF and drinks and encouraging healthier dietary choices. Consuming UPF increases the risk of obesity and colon cancer.
| 1. | Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. Freshly Prepared Meals and Not Ultra-Processed Foods. Cell Metab. 2019;30:5-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Lane MM, Davis JA, Beattie S, Gómez-Donoso C, Loughman A, O'Neil A, Jacka F, Berk M, Page R, Marx W, Rocks T. Ultraprocessed food and chronic noncommunicable diseases: A systematic review and meta-analysis of 43 observational studies. Obes Rev. 2021;22:e13146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 332] [Article Influence: 83.0] [Reference Citation Analysis (0)] |
| 3. | World Health Organization. Obesity and Overweight. Mar 1, 2024. [cited 3 December 2024]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. |
| 4. | Fiolet T, Srour B, Sellem L, Kesse-Guyot E, Allès B, Méjean C, Deschasaux M, Fassier P, Latino-Martel P, Beslay M, Hercberg S, Lavalette C, Monteiro CA, Julia C, Touvier M. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 466] [Cited by in RCA: 578] [Article Influence: 82.6] [Reference Citation Analysis (0)] |
| 5. | Mendonça RD, Pimenta AM, Gea A, de la Fuente-Arrillaga C, Martinez-Gonzalez MA, Lopes AC, Bes-Rastrollo M. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr. 2016;104:1433-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 402] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 6. | Srour B, Fezeu LK, Kesse-Guyot E, Allès B, Méjean C, Andrianasolo RM, Chazelas E, Deschasaux M, Hercberg S, Galan P, Monteiro CA, Julia C, Touvier M. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ. 2019;365:l1451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 362] [Cited by in RCA: 535] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 7. | Schnabel L, Kesse-Guyot E, Allès B, Touvier M, Srour B, Hercberg S, Buscail C, Julia C. Association Between Ultraprocessed Food Consumption and Risk of Mortality Among Middle-aged Adults in France. JAMA Intern Med. 2019;179:490-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 255] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 8. | Zong G, Li Y, Wanders AJ, Alssema M, Zock PL, Willett WC, Hu FB, Sun Q. Intake of individual saturated fatty acids and risk of coronary heart disease in US men and women: two prospective longitudinal cohort studies. BMJ. 2016;355:i5796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 157] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 9. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47144] [Article Influence: 2946.5] [Reference Citation Analysis (0)] |
| 10. | Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014;14:579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 640] [Cited by in RCA: 1307] [Article Influence: 118.8] [Reference Citation Analysis (0)] |
| 11. | Ma LL, Wang YY, Yang ZH, Huang D, Weng H, Zeng XT. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res. 2020;7:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 575] [Cited by in RCA: 710] [Article Influence: 142.0] [Reference Citation Analysis (0)] |
| 12. | Wang L, Du M, Wang K, Khandpur N, Rossato SL, Drouin-Chartier JP, Steele EM, Giovannucci E, Song M, Zhang FF. Association of ultra-processed food consumption with colorectal cancer risk among men and women: results from three prospective US cohort studies. BMJ. 2022;378:e068921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 13. | Oxentenko AS, Bardia A, Vierkant RA, Wang AH, Anderson KE, Campbell PT, Sellers TA, Folsom AR, Cerhan JR, Limburg PJ. Body size and incident colorectal cancer: a prospective study of older women. Cancer Prev Res (Phila). 2010;3:1608-1620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Romaguera D, Fernández-Barrés S, Gracia-Lavedán E, Vendrell E, Azpiri M, Ruiz-Moreno E, Martín V, Gómez-Acebo I, Obón M, Molinuevo A, Fresán U, Molina-Barceló A, Olmedo-Requena R, Tardón A, Alguacil J, Solans M, Huerta JM, Ruiz-Dominguez JM, Aragonés N, Fernández-Villa T, Dierssen-Sotos T, Moreno V, Guevara M, Vanaclocha-Espi M, Lozano-Lorca M, Fernández-Tardón G, Castaño-Vinyals G, Pérez-Gómez B, Molina AJ, Llorca J, Gil L, Castilla J, Pollán M, Kogevinas M, Amiano P. Consumption of ultra-processed foods and drinks and colorectal, breast, and prostate cancer. Clin Nutr. 2021;40:1537-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 15. | Terry PD, Miller AB, Rohan TE. Obesity and colorectal cancer risk in women. Gut. 2002;51:191-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 134] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Movahedi M, Bishop DT, Macrae F, Mecklin JP, Moeslein G, Olschwang S, Eccles D, Evans DG, Maher ER, Bertario L, Bisgaard ML, Dunlop MG, Ho JW, Hodgson SV, Lindblom A, Lubinski J, Morrison PJ, Murday V, Ramesar RS, Side L, Scott RJ, Thomas HJ, Vasen HF, Burn J, Mathers JC. Obesity, Aspirin, and Risk of Colorectal Cancer in Carriers of Hereditary Colorectal Cancer: A Prospective Investigation in the CAPP2 Study. J Clin Oncol. 2015;33:3591-3597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Kitahara CM, Berndt SI, de González AB, Coleman HG, Schoen RE, Hayes RB, Huang WY. Prospective investigation of body mass index, colorectal adenoma, and colorectal cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. J Clin Oncol. 2013;31:2450-2459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Anderson AS, Craigie AM, Caswell S, Treweek S, Stead M, Macleod M, Daly F, Belch J, Rodger J, Kirk A, Ludbrook A, Rauchhaus P, Norwood P, Thompson J, Wardle J, Steele RJ. The impact of a bodyweight and physical activity intervention (BeWEL) initiated through a national colorectal cancer screening programme: randomised controlled trial. BMJ. 2014;348:g1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 19. | Flaherty DC, Jalas JR, Sim MS, Stojadinovic A, Protic M, Lee DJ, Bilchik AJ. The Negative Impact of Body Mass Index on the Tumor Microenvironment in Colon Cancer: Results of a Prospective Trial. Ann Surg Oncol. 2018;25:1374-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, Chung ST, Costa E, Courville A, Darcey V, Fletcher LA, Forde CG, Gharib AM, Guo J, Howard R, Joseph PV, McGehee S, Ouwerkerk R, Raisinger K, Rozga I, Stagliano M, Walter M, Walter PJ, Yang S, Zhou M. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019;30:67-77.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 580] [Cited by in RCA: 922] [Article Influence: 153.7] [Reference Citation Analysis (0)] |
| 21. | Canella DS, Levy RB, Martins AP, Claro RM, Moubarac JC, Baraldi LG, Cannon G, Monteiro CA. Ultra-processed food products and obesity in Brazilian households (2008-2009). PLoS One. 2014;9:e92752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 268] [Cited by in RCA: 287] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 22. | Silva FM, Giatti L, de Figueiredo RC, Molina MDCB, de Oliveira Cardoso L, Duncan BB, Barreto SM. Consumption of ultra-processed food and obesity: cross sectional results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort (2008-2010). Public Health Nutr. 2018;21:2271-2279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 23. | Louzada ML, Baraldi LG, Steele EM, Martins AP, Canella DS, Moubarac JC, Levy RB, Cannon G, Afshin A, Imamura F, Mozaffarian D, Monteiro CA. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 377] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 24. | Nardocci M, Leclerc BS, Louzada ML, Monteiro CA, Batal M, Moubarac JC. Consumption of ultra-processed foods and obesity in Canada. Can J Public Health. 2019;110:4-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 175] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 25. | Juul F, Martinez-Steele E, Parekh N, Monteiro CA, Chang VW. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018;120:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 265] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 26. | Rauber F, Steele EM, Louzada MLDC, Millett C, Monteiro CA, Levy RB. Ultra-processed food consumption and indicators of obesity in the United Kingdom population (2008-2016). PLoS One. 2020;15:e0232676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 132] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 27. | Shu L, Huang Y, Si C, Zhu Q, Zheng P, Zhang X. Association between ultra-processed food intake and risk of colorectal cancer: a systematic review and meta-analysis. Front Nutr. 2023;10:1170992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 28. | Lian Y, Wang GP, Chen GQ, Chen HN, Zhang GY. Association between ultra-processed foods and risk of cancer: a systematic review and meta-analysis. Front Nutr. 2023;10:1175994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 29. | Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125:308-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 379] [Cited by in RCA: 561] [Article Influence: 140.3] [Reference Citation Analysis (0)] |
| 30. | Chang K, Gunter MJ, Rauber F, Levy RB, Huybrechts I, Kliemann N, Millett C, Vamos EP. Ultra-processed food consumption, cancer risk and cancer mortality: a large-scale prospective analysis within the UK Biobank. EClinicalMedicine. 2023;56:101840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 78] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 31. | Vitale M, Costabile G, Testa R, D'Abbronzo G, Nettore IC, Macchia PE, Giacco R. Ultra-Processed Foods and Human Health: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Adv Nutr. 2024;15:100121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 32. | Bruce WR, Giacca A, Medline A. Possible mechanisms relating diet and risk of colon cancer. Cancer Epidemiol Biomarkers Prev. 2000;9:1271-1279. [PubMed] |
| 33. | Song M, Garrett WS, Chan AT. Nutrients, foods, and colorectal cancer prevention. Gastroenterology. 2015;148:1244-60.e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 467] [Article Influence: 46.7] [Reference Citation Analysis (0)] |