Published online Oct 15, 2024. doi: 10.4251/wjgo.v16.i10.4166
Revised: August 23, 2024
Accepted: September 6, 2024
Published online: October 15, 2024
Processing time: 121 Days and 16.3 Hours
Pediatric pancreatic tumors are rare and account for < 0.1% of all childhood cancers. The primary treatment for pancreatic tumors is surgical resection. However, because of the lack of knowledge regarding pediatric pancreatic tumors, no comprehensive treatment plans for pediatric pancreatic tumors have been developed.
To compared the clinical features, treatment methods, and prognosis of pediatric pancreatic tumors in Japan with those in other countries.
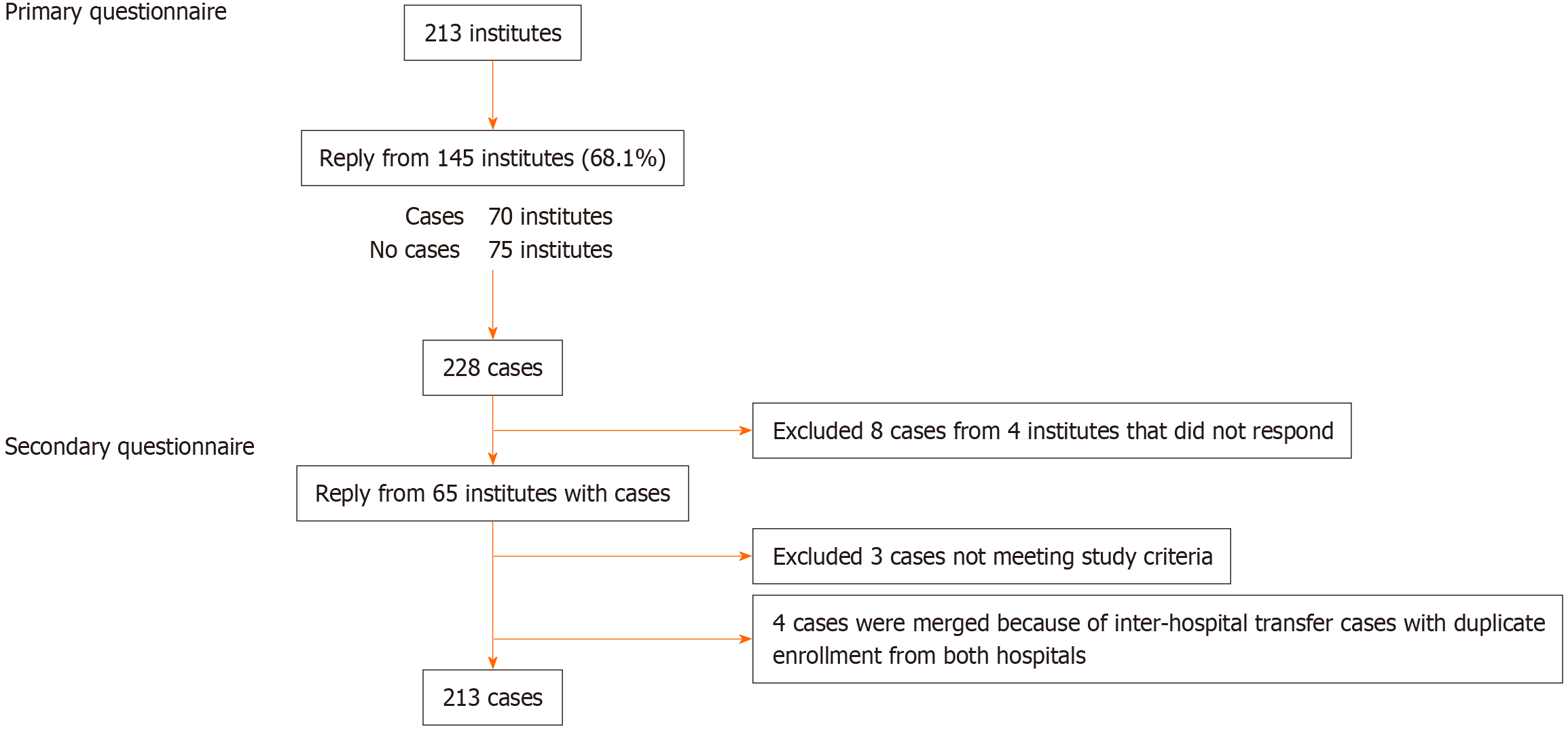
Questionnaires were sent to 213 pediatric surgical units in Japan. Pancreatic tumors that were not surgically treated were excluded from the survey. The primary survey investigated the number of patients aged 0-18 years who underwent pancreatic tumor surgery and the type of tumors managed during the 22-year study period (from January 1, 2000 to December 31, 2021) by post card. The secondary survey assessed the clinical images, treatment methods, and tumor outcomes via email.
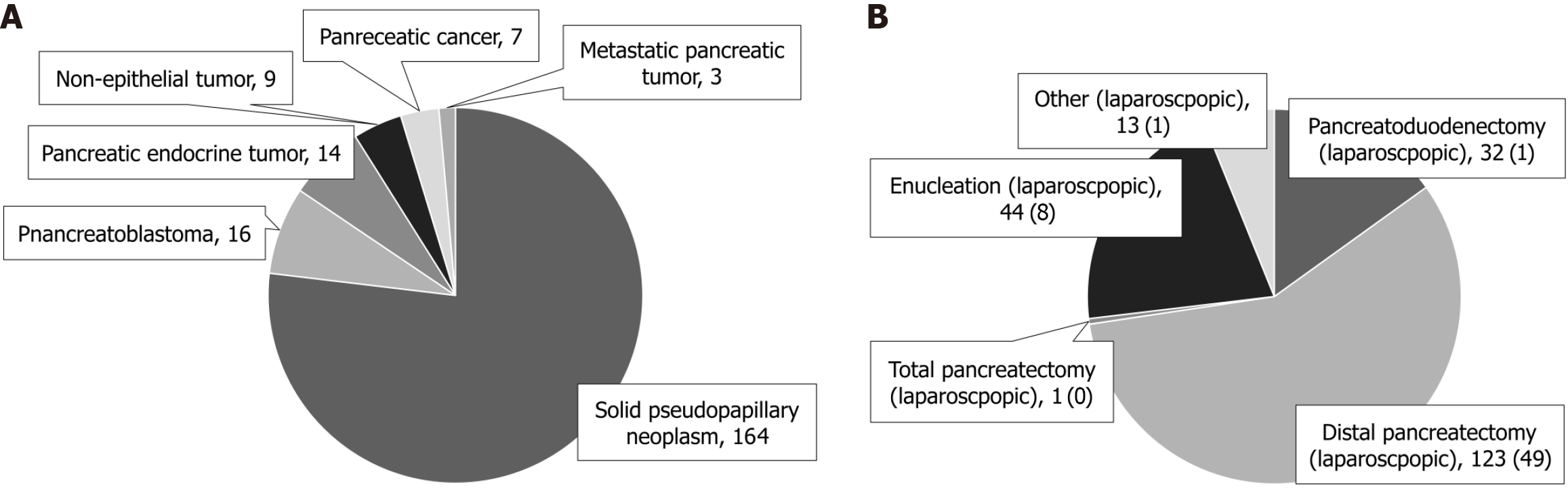
The primary survey enrolled 228 patients. In the secondary survey, 213 patients were eventually enrolled. The most common type of pancreatic tumor was solid pseudopapillary neoplasm (SPN) [n = 164 (77.0%)], followed by pancreatoblastoma [n = 16 (7.5%)], pancreatic endocrine tumor [n = 14 (6.6%)], non-epithelial tumor [n = 9 (4.2%)], pancreatic tumor [n = 7 (3.3%)], and metastatic pancreatic tumor [n = 3 (1.4%)]. Overall, 123 (57.7%) patients underwent distal pancreatectomy, of whom 49 underwent laparoscopic surgery. Forty-four (20.7%) patients underwent enucleation, of whom eight underwent laparoscopic surgery. Thirty-two (15.0%) patients underwent pancreaticoduodenectomy, of whom one underwent laparoscopic surgery. All patients with SPN, including those with distant metastases and recurrent disease, survived.
SPN was more common in Japan than in other countries. Regardless of the histological type, resection is the most effective treatment for pediatric pancreatic tumors.
Core Tip: Pediatric pancreatic tumors are rare. This study compared the clinical images, treatment methods, and prognosis of pediatric pancreatic tumors in Japan with those in other countries. The primary survey investigated the number of patients aged 0-18 years who underwent pancreatic tumor surgery and the types of tumors managed during the 22-year study period (from January 1, 2000 to December 31, 2021). The secondary survey assessed the clinical images, treatment methods, and tumor outcomes. In the secondary survey, 213 patients were eventually enrolled. Surgical resection is the main treatment for all histological types of pediatric pancreatic tumors.
- Citation: Makita S, Uchida H, Kano M, Kawakubo N, Miyake H, Yoneda A, Tajiri T, Fukumoto K. Nationwide questionnaire survey on pediatric pancreatic tumors in Japan. World J Gastrointest Oncol 2024; 16(10): 4166-4176
- URL: https://www.wjgnet.com/1948-5204/full/v16/i10/4166.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i10.4166
Pediatric pancreatic tumors are extremely rare with unvalidated clinicopathological features. Moreover, the number of reports on clinical images of pediatric pancreatic tumors in Japan is extremely low. Pancreatic neoplasms account for < 0.1% of all childhood cancers[1,2]. Solid pseudopapillary neoplasms (SPNs) is common in late childhood, and pancreatoblastomas are observed in early childhood. Pancreatic cancer is extremely rare. The incidence of SPNs increased seven-fold after 2000. The Asian population had a delayed peak incidence in women aged 30-39 years and men aged 50-59 years compared with the White population[3]. However, cross-racial data on pediatric SPNs are lacking. Other types of pediatric pancreatic tumors are rare, and differences in their frequency among different races are not well documented. Knowledge about racial differences in etiology is essential in clinical settings and can affect differential diagnosis. The primary treatment for pancreatic tumors is surgical resection[4,5]. However, because of the lack of knowledge regarding pediatric pancreatic tumors, no comprehensive treatment plans for pediatric pancreatic tumors have been developed. This study compared the clinical images, treatment methods, and prognosis of pediatric pancreatic tumors in Japan with those in other countries.
Considering that pediatric surgeons are the most common surgeons who surgically treat pediatric pancreatic tumors, we developed a questionnaire targeting pediatric surgeons. Pancreatic tumors that were not surgically treated were excluded from the study. Since November 2022, questionnaires were sent to 213 facilities accredited by the Japanese Society of Pediatric Surgeons (Supplementary material) via post cards. The primary survey investigated the number of patients aged 0-18 years who underwent pancreatic tumor surgery and the types of tumors during the 22-year study period (from January 1, 2000 to December 31, 2021). Since March 2023, the secondary survey forms were sent to facilities that had applicable cases in the primary survey via e-mail. Based on their responses, they were eligible to participate in the secondary survey. The secondary survey assessed histopathological diagnosis, age at diagnosis, sex, opportunity for detection, tumor size and site, tumor marker levels, surgical technique, occurrence of grade IIIa or higher complications based on the Clavien-Dindo classification, chemotherapy and radiotherapy status, and treatment outcomes. The respondents obtained these data by retrospectively searching medical records, completed a questionnaire for each case, and returned them via e-mail. The respondents filled in their age and size, while the remaining items were answered in a checkbox format. The secondary survey respondents were approved by the Ethics Committee of each institution to respond to the survey; therefore, their data are reliable. We were able to obtain all the data in January 2024. This study was approved by the Ethics Committee of Nagoya University (2022-0048) and the Academic Survey and Advanced Medical Science Committee of the Japanese Society of Pediatric Surgeons.
All statistical analyses were performed using EZR (v.3.0.3; Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Formulation for Statistical Computing)[6]. To examine the associations between variables, we used Fisher‘s exact test as appropriate. P values < 0.05 were used to denote statistical significance.
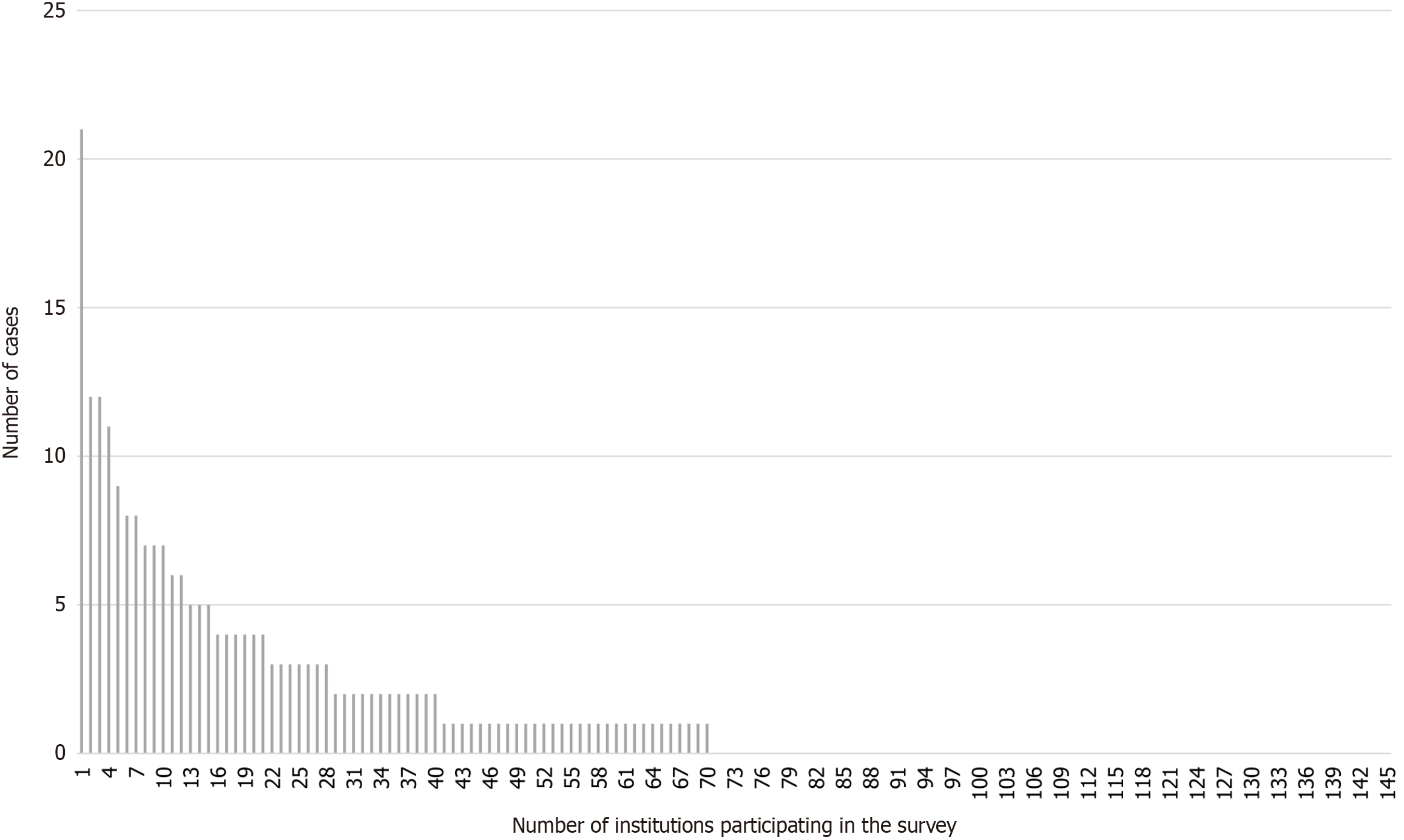
In total, 145 (68.1%) of the 213 facilities responded to the primary survey, and 228 cases were included in this analysis. Furthermore, 75 (51.7%) of the 145 facilities did not surgically treat patients with pancreatic tumors within 22 years. In total, 55 (37.9%) facilities managed 1-4 patients; 11 (7.6%) facilities treated 5-9 patients; and four (2.8%) facilities managed > 10 patients. Only one of the 145 facilities had managed > 20 patients (Figure 1). In total, 66 of the 70 facilities with applicable cases provided consent to participate in the secondary survey. Finally, 66 facilities responded to the secondary survey. The primary survey enrolled 228 patients. However, as shown in Figure 2, only 213 patients were ultimately enrolled.
Figure 3A presents a breakdown of the 213 patients with pancreatic tumors included in the study. The most common type of pancreatic tumor was SPN [n = 164 (77.0%)], followed by pancreatoblastoma [n = 16 (7.5%)], pancreatic endocrine tumor [n = 14 (6.6%)], non-epithelial tumor [n = 9 (4.2%)], pancreatic cancer [n = 7 (3.3%)], and metastatic pancreatic tumor [n = 3 (1.4%)]. Tables 1, 2, and 3 present data on patient demographic characteristics, opportunity for detection, surgical procedure, and outcomes for each illness. Overall, 123 (57.7%) patients underwent distal pancreatectomy. In 49 patients, laparoscopic surgery was performed. Furthermore, 44 (20.7%) patients underwent enucleation. In eight patients, laparoscopic surgery was performed. In total, 32 (15.0%) patients underwent pancreaticoduodenectomy. In one case, laparoscopic surgery was performed. Moreover, one patient underwent total pancreatectomy, and the remaining 13 patients underwent other procedures. Of them, one patient underwent laparoscopic surgery (Figure 3B). The involvement of adult gastrointestinal surgeons was also investigated. Results revealed that 84 (39.4%) of the 213 facilities surgically managed their patients. In total, 84 surgeons were the primary and assistant surgeons for 40 and 44 cases, respectively (Table 3). Based on the Clavien-Dindo classification, pancreatic fistula was the most common grade IIIa or higher complication. This condition was observed in 35 (16.4%) of the 213 patients.
| SPN | Pancreatoblastoma | Pancreatic endocrine tumor | Non-epithelial tumor | Pancreatic cancer | Metastatic pancreatic tumor | |
| Number | 164 | 16 | 14 | 9 | 7 | 3 |
| Age (month) | 146 (75-191) | 58 (0-156) | 76.5 (0-206) | 107 (18-187) | 102 (12-155) | 36 (33-129) |
| Male:female | 36:128 | 9:7 | 6:8 | 4:5 | 5:2 | 2:1 |
| Year of diagnosis | ||||||
| 2000-2010 | 48 | 6 | 2 | 3 | 3 | 2 |
| 2011-2021 | 116 | 10 | 12 | 6 | 4 | 1 |
| Stage | ||||||
| Localized | 160 | 8 | 14 | 8 | 5 | 2 |
| Distant | 4 | 8 | 0 | 1 | 2 | 1 |
| Location | ||||||
| Head | 41 | 6 | 5 | 6 | 3 | 2 |
| Body | 23 | 2 | 3 | 1 | 1 | 1 |
| Tail | 72 | 1 | 2 | 0 | 2 | 0 |
| Head + body | 4 | 2 | 1 | 0 | 1 | 0 |
| Body + tail | 24 | 4 | 3 | 1 | 0 | 0 |
| Other | 0 | 1 | 0 | 1 | 0 | 0 |
| Tumor size (mm) | 50 (10-110) | 90 (25-170) | 16.5 (6-25) | 60 (30-127) | 110 (58.4-122) | 30 (12-60) |
| 6 cases unknown size |
| SPN | Pancreatoblastoma | Pancreatic endocrine tumor | Non-epithelial tumor | Pancreatic cancer | Metastatic pancreatic tumor | |
| Number | 164 | 16 | 14 | 9 | 7 | 3 |
| Fever | 5 (3.0) | 0 (0) | 1 (7.1) | 1 (11.1) | 0 (0) | 1 (33.3) |
| Nausea/vomiting | 60 (36.6) | 2 (12.5) | 0 (0) | 4 (44.4) | 2 (28.6) | 0 (0) |
| Abdominal pain | 108 (65.9) | 7 (43.8) | 2 (14.3) | 6 (66.6) | 2 (28.6) | 0 (0) |
| Abdominal mass | 11 (6.7) | 8 (50.0) | 0 (0) | 2 (22.2) | 4 (57.1) | 1 (33.3) |
| Trauma | 31 (18.9) | 0 (0) | 0 (0) | 1 (11.1) | 0 (0) | 0 (0) |
| Jaundice | 1 (0.6) | 2 (12.5) | 0 (0) | 1 (11.1) | 0 (0) | 0 (0) |
| Image abnormality | 37 (22.6) | 0 (0) | 3 (21.4) | 0 (0) | 1 (14.3) | 1 (33.3) |
| Abnormal blood examination | 1 (0.6) | 1 (6.3) | 8 (57.1) | 0 (0) | 0 (0) | 1 (33.3) |
| Others | 8 (4.9) | 5 (31.3) | 1 (7.1) | 2 (22.2) | 0 (0) | 0 (0) |
| SPN | Pancreatoblastoma | Pancreatic endocrine tumor | Non-epithelial tumor | Pancreatic cancer | Metastatic pancreatic tumor | |
| Number | 164 | 16 | 14 | 9 | 7 | 3 |
| Type of resection | ||||||
| Pancreatoduodenectomy | 17 (1) | 8 (0) | 2 (0) | 2 (0) | 2 (0) | 1 (0) |
| Distal pancreatectomy | 105 (48) | 7 (0) | 7 (1) | 1 (0) | 2 (0) | 1 (0) |
| Total pancreatectomy | 0 (0) | 1 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Enucleation (laparoscopic) | 35 (6) | 0 (0) | 4 (1) | 4 (1) | 1 (0) | 0 (0) |
| Other (laparoscopic) | 7 (0) | 0 (0) | 1 (0) | 2 (0) | 2 (0) | 1 (0) |
| Involvement of adult gastrointestinal surgeons | ||||||
| Operator | 29 | 4 | 5 | 0 | 2 | 0 |
| Assistant | 39 | 4 | 1 | 0 | 1 | 0 |
| None | 96 | 8 | 8 | 9 | 4 | 3 |
| Complication | 33 | 3 | 2 | 1 | 4 | 0 |
| Pancreatic fistula | 28 | 1 | 2 | 0 | 4 | 0 |
| Others | 5 | 2 | 0 | 1 | 0 | 0 |
| Outcome | ||||||
| Alive without recurrence | 155 | 10 | 14 | 7 | 2 | 1 |
| With recurrence | 8 | 2 | 0 | 1 | 1 | 0 |
| Death | 0 | 4 | 0 | 1 | 4 | 2 |
SPN [n = 164 (77.0%)] was the most common pancreatic tumor. The median age at presentation was 146 months (range, 75-191 months), and it was more common in the latter half of childhood. Of 164 patients, 108 (65.9%) experienced abdominal pain. Thirty-one (18.9%) patients were diagnosed during close examination after trauma. Furthermore, 37 (22.6%) patients were diagnosed incidentally based on imaging of other diseases (Table 2). In total, 44 of 164 patients had elevated tumor marker levels. In particular, 33, 11, and 3 patients presented with high neuron-specific enolase, cancer antigen 19-9 (CA19-9), and CA125 levels. Furthermore, three patients presented with elevated levels of other tumor markers. Distal pancreatic lesions were the most common type of tumor. In total, 105 distal pancreatectomy procedures were performed, of which 48 were laparoscopic. Enucleation was the second most frequently used method (n = 35), and six surgeries were laparoscopic (Tables 1 and 3). Two patients who underwent enucleation did not undergo R0 resection and had residual tumors. However, both patients had long-term survival. Four (2.5%) patients presented with distant metastasis during the initial surgery (two in the liver and one in the greater omentum), and one patient presented with peritoneal dissemination. The four patients underwent total resection including metastatic lesions and achieved long-term survival without recurrence. Eight (4.9%) patients experienced recurrence after pancreatectomy (four local, two liver, and two peritoneal seeding). All patients underwent resection of recurrent lesions and achieved long-term survival. Five of the eight patients required multiple surgeries due to multiple recurrence. All patients survived, with a median follow-up of 60 months (range, 6-188 months) after pancreatectomy. Tumor markers [e.g., carcinoembryonic antigen, CA19-9, alpha-fetoprotein (AFP), and neuron-specific enolase] of 54 (33.1%) patients were monitored during outpatient follow-up. None of the patients received chemotherapy or radiotherapy.
Pancreatoblastoma accounted for 7.5% (n = 16) of all pancreatic tumors. The median age at presentation was 58 months (range, 0-156 months), and most patients presented with the condition in the first half of childhood. In total, eight (50.0%) of the 16 patients had an abdominal mass, and seven (43.8%) experienced abdominal pain (Table 2). In total, nine of the 16 patients had elevated AFP levels. Eight (50.0%) patients presented with metastatic lesions. Metastatic lesions were resected in five of the eight patients. All patients with tumors in the pancreatic head underwent pancreaticoduodenectomy [pancreaticoduodenectomy in three patients, pylorus-preserving pancreatoduodenectomy (PPPD) in three patients, and subtotal stomach-preserving pancreaticoduodenectomy in two patients]. One patient with a tumor involving the entire pancreas underwent total pancreatectomy (Tables 1 and 3). In total, six (37.5%) of the 16 patients underwent tumor resection with concomitant resection and reconstruction of major abdominal vessels. Moreover, 15 (93.8%) of the 16 patients received chemotherapy preoperatively or postoperatively. One patient was surgically treated in the neonatal period and was followed up as an outpatient without chemotherapy. Moreover, three (18.8%) of the 16 patients received radiotherapy. There were 10 (62.5%) recurrence-free survivors after treatment, one recurrence-free survivor after recurrence treatment, and one recurrence survivor (who was under follow-up). Moreover, four tumor-related deaths were recorded. The median follow-up time after pancreatectomy was 67 months (range, 12-171 months).
Pancreatic endocrine tumors accounted for 6.6% (n = 14) of all pancreatic tumors. Moreover, they included insulinomas (n = 6), congenital hyperinsulinemia (n = 4, nesidioblastosis; n = 2, islet cell adenomatosis), and pancreatic neuroendocrine tumors (n = 2). In total, eight (57.1%) of the 14 patients were diagnosed based on abnormal blood sampling (Table 2). Distal pancreatectomy (n = 7, laparoscopic surgery in one patient) was the most commonly performed procedure, followed by enucleation (n = 4, laparoscopic surgery in one patient). The median follow-up time after pancreatectomy was 80.5 months (range, 8-185 months), without recurrence.
Non-epithelial tumors (n = 9) included mature teratomas (n = 2), lymphatic malformations (n = 2), rhabdomyosarcoma (n = 1), neuroblastoma (n = 1), Ewing sarcoma (n = 1), malignant lymphoma (n = 1), and hamartoma (n = 1). Six (66.6%) of the nine patients were diagnosed because of abdominal pain (Table 2). Enucleation was performed in four of the nine patients. One patient underwent laparoscopic surgery (Table 3). Seven of the nine patients survived without recurrence after pancreatectomy. One patient with neuroblastoma presented with residual tumor after R2 resection. However, the patient survived 114 months after completing chemotherapy and radiotherapy. In one patient, rhabdomyosarcoma recurred 4 months after pancreatectomy due to peritoneal dissemination, and the patient died. The median follow-up time after pancreatectomy was 65 months (range, 15-180 months).
Histological classification of the seven pancreatic cancer cases included acinar cell carcinoma (n = 6) and adenocarcinoma (n = 7). The median age at presentation was 102 months (range, 12-155 months), mainly among school-aged children or later. However, in two patients, the condition occurred in children (Table 1). Four (57.1%) of the seven patients were diagnosed with abdominal masses. Six patients had elevated tumor markers. In particular, four and three patients had elevated AFP and CA125 levels, respectively, and two patients presented with elevated levels of other tumor markers. Two patients presented with distant metastasis. The procedures performed were PPPD (n = 2), distal pancreatomy (n = 2), enucleation (n = 1), partial pancreatectomy (n = 1), and biopsy only (n = 1). There were two recurrence-free survivors (177 and 181 months after pancreatectomy, respectively) and one recurrence case (on treatment), and four tumor-related deaths were recorded. All patients received chemotherapy. The median follow-up time after pancreatectomy was 23 months (range, 9-181 months).
Metastatic pancreatic tumors included neuroblastoma (n = 1), Ewing sarcoma (n = 1), and hepatoblastoma (n = 1). The neuroblastoma, Ewing sarcoma, and metastatic hepatoblastoma were resected via distal resection, PPPD, and partial pancreatectomy, respectively. Only patients with hepatoblastoma metastatic lesions survived for 145 months without recurrence after pancreatectomy. Meanwhile, the remaining two patients died of their tumors at 5 and 13 months after pancreatectomy, respectively.
In this study, questionnaires were sent to 213 pediatric surgical units in Japan, and 145 responses were obtained. The main findings of this study are as follows. First, the number of facilities with experience in pancreatic tumor surgery was low. As shown in Figure 1, 75 facilities had no applicable cases. Only four facilities managed > 10 cases in 22 years. In this study, the primary survey response rate was 68.1% (n = 145). However, the responses from larger pediatric surgical facilities were approximately similar. We believe that the results of this survey reflect the current situation in Japan. Therefore, Japanese pediatric surgeons have significantly low experience with pancreatic tumor surgery. Pancreatectomy is associated with the development of pancreatic fistula, which is a potentially dangerous complication[7]. In 84 (39.4%) of the 213 patients, a gastroenterology surgeon with experience in pancreatic resection was involved in the surgery. A pediatric surgeon with minimal experience in pancreatic resection did not perform the surgery alone, but was assisted by an adult gastroenterology surgeon. Some pediatric surgeons may encounter pediatric pancreatic tumors only once every few years to once every 10 years. Moreover, adult gastroenterology surgeons should provide support for pancreatic surgery from to ensure safe surgery.
Second, the clinical image of pancreatic tumors in children in Japan was validated. SPN is significantly common in Japan. As shown in Figure 3A, 164 (77.0%) patients presented with SPN, 16 (7.5%) patients presented with pancreatoblastoma, 14 (6.6%) patients presented with endocrine tumor, nine (4.2%) patients presented with non-epithelial tumor, seven (3.3%) patients presented with pancreatic cancer, and three (1.4%) patients presented with metastatic pancreatic tumor. Table 4 presents a comparison of disease frequencies between our study and the Surveillance, Epidemiology, and End Results (SEER), National Cancer Database, United Kingdom National Registry of Childhood Tumors, and TREP database. A previous report evaluated 195 cases of pancreatic tumors in patients aged ≤ 19 years using the SEER database of the National Cancer Institute in the United States between 1975 and 2018. Results revealed that 33.8% of the patients presented with endocrine pancreatic tumors, 32.3% presented with solid pseudopapillary tumors, 11.3% presented with pancreatoblastoma, and 22.6% presented with other tumor types[8]. These results differed from those reported in Japan. Similar results were also found in the National Cancer Database, which contains more patients registered than SEER[9]. From 2004 to 2014, 109 cases were reported, and the incidence can be estimated to be approximately 10 cases per year. This frequency is the same as that in Japan. Multicenter case summaries of pediatric pancreatic tumors have been reported in the United Kingdom and Italy. However, the numbers are low (2-3 cases per year), indicating that pediatric pancreatic tumors are rare in all countries[10].
| Our study | SEER | National Cancer Database | United Kingdom National Registry of Childhood Tumors | TREP database | |
| Age, year | ≤ 18 | ≤ 19 | ≤ 19 | ≤ 18 | ≤ 18 |
| Country | Japan | United States | United States | United Kingdom | Italy |
| Time | 2000-2021 | 1975-2018 | 2004-2014 | 1971-2000 | 2000-2009 |
| Number | 213 | 195 | 109 | 25 | 21 |
| Solid pseudopapillary neoplasm | 164 (77.0) | 63 (32.3) | 33 (30.3) | 8 (32) | 12 (57.1) |
| Pancreatoblastoma | 16 (7.5) | 22 (11.3) | 17 (15.6) | 11 (44) | 4 (19.0) |
| Pancreatic endocrine tumor | 14 (6.6) | 66 (33.8) | 30 (27.5) | 0 | 3 (14.3) |
| Sarcoma | 2 (0.9) | 44 (22.6) | 7 (6.4) | 0 | 0 |
| Pancreatic adenocarcinoma | 1 (0.5) | 17 (15.6) | 6 (24) | 2 (9.5) | |
| Acinar cell carcinoma | 6 (2.8) | 0 | 0 | 0 | |
| Metastatic pancreatic tumor | 3 (1.4) | 0 | 0 | 0 | 0 |
| Others | 7 (3.3) | 0 | 5 (4.6) | 0 | 0 |
Our data on SPN were compared with the SEER data reported by Qi et al[8] (Table 5). Age at onset was more likely to be lower in Japan than in other countries. Lin et al[3] evaluated 281 cases of SPN (n = 150, White; n = 88, Asian; and n = 43, Black) between 1988 and 2020. Results revealed that 22 of the 286 (n = 14, White; n = 7, Asian; and n = 1, Black) were aged 19 years. Most Asians in these data are Taiwanese, thereby showing regional differences in age at onset between Japan and Taiwan, even among the same Asian populations[3]. Racial differences between cohorts may include not only physical differences resulting from genetic factors but also differences due to social constructs, economic conditions, nutrition, and environmental exposure.
| Our study (2000-2021) | SEER (1975-2018) | P value | |
| n = 164 | n = 63 | ||
| Age at diagnosis | < 0.05 | ||
| < 14 years | 153 | 21 | |
| > 14 years | 11 | 42 | |
| Sex | < 0.05 | ||
| Male | 36 | 6 | |
| Female | 128 | 57 | |
| Race | < 0.05 | ||
| White | 0 | 47 | |
| Others | 164 | 16 | |
| All Asian | |||
| Primary site | |||
| Head | 41 | 21 | 0.246 |
| Body | 23 | 7 | 0.665 |
| Tail | 72 | 21 | 0.176 |
| Other | 28 | 0 | < 0.05 |
| Unknown | 0 | 14 | - |
| Localized | 160 | 45 | < 0.05 |
| Regional and distant | 4 | 18 | < 0.05 |
| Surgery | < 0.05 | ||
| Yes | 164 | 59 | |
| No | 0 | 4 | |
| 5-year overall survival | 100% | 100% |
All 164 patients with SPN in our study survived. All 63 patients with SPNs aged > 19 years also survived, as reported by Qi et al[8] (Table 5). Results revealed that aggressive resection of distant metastases from presentation and in cases of recurrence had good outcomes. In our study, nucleation was performed in 35 of 164 patients, and the outcomes were good. Results revealed that enucleation could be considered for SPN. However, pancreaticoduodenectomy, which is usually more invasive, should be considered for pancreatic head lesions.
Pancreatoblastoma is an extremely rare tumor type, with an incidence of 0.004 per 100000 individuals reported in the United States. Furthermore, it was more common among Asians than among Caucasians[3,5,11]. In total, 16 patients with pancreatoblastoma were included in this study. Six cases were reported from 2000 to 2010, and 10 cases were reported from 2011 to 2021. Eight patients presented with distal illnesses. However, six of the eight patients survived after aggressive resection of the distant lesion and chemotherapy. Aggressive surgery with revascularization was performed in 8 of the 16 patients. The preoperative and postoperative chemotherapy regimens varied from case to case. However, aiming for complete surgical resection, including the distant lesion, while controlling the illness with chemotherapy, was considered reasonable.
Treatment of pancreatic tumors requires surgical resection, regardless of histological type. Enucleation has a good prognosis for SPN, and aggressive resection is recommended for recurrent and distant lesions. Laparoscopic and robotic surgeries are increasingly used in the adult and pediatric surgical fields. Furthermore, open surgery was more likely to be selected over laparoscopic surgery because pediatric surgeons have less experience in pancreatectomy. In this study, 153 and 59 patients underwent laparotomy and laparoscopic surgery, respectively, accounting for 27.7% of all cases. The laparoscopic procedures included distal pancreatectomy (n = 49), enucleation (n = 8), and pancreaticoduodenectomy (n = 1). In Japan, the institutional standards for laparoscopic pancreatectomy are strictly enforced, and laparoscopic pancreatectomy is not widely performed in the pediatric surgical field in which the number of cases is small.
In this study, the number of patients who were treated solely by adult gastrointestinal surgeons was not reflected. In Japan, in institutions with a pediatric surgery department, pediatric surgeons are often involved in the procedures. However, in facilities without a pediatric surgery department, the surgeries for pancreatic tumors are typically performed solely by adult surgeons. In Japan, 2000-2500 new cases of childhood cancer are recorded annually. Therefore, 20-25 cases of pancreatic tumors, which account for < 0.1% of childhood cancers, are recorded annually. Cumulatively, in over a 20-year period, approximately 400-500 cases may have occurred in Japan, a discrepancy from the 213 cases obtained from the questionnaire survey. This may be because the survey was administered only to pediatric surgical units in Japan. In particular, SPN often occurs during teenage years. Considering that the body size is in close proximity to that of the adult body size, such cases are unlikely to be purposely referred to pediatric surgeons who have minimal experience in pancreatectomy. Preoperative or postoperative chemotherapy was not required. Moreover, treatment at a specialized facility was not required. In contrast, pancreatoblastoma, pancreatic cancer, and metastatic tumors require specialized chemotherapy, and pancreatic endocrine tumors require endocrinological management. Thus, these patients are likely to be treated at specialized facilities with pediatric surgeons.
In Japan, the National Clinical Database (NCD) was established as a database of surgical cases to support the medical specialist system, and the registration of cases began in January 2011[12]. As of April 2024, the number of registered facilities could have reached 5679, and > 95% of surgeries in Japan were registered. Although the statistics of cases before 2010 rely on questionnaires, data from the NCD can be used for the statistics of cases after 2011, and the NCD can extract cases in which pediatric surgeons are not involved. Therefore, the use of the NCD is essential for further understanding the clinical characteristics of pancreatic tumors.
Pediatric pancreatic tumors are rare, and their clinical characteristics vary among countries. SPN is more common in Japan than in other countries. In Japan, the experience of pediatric surgeons with pancreatic tumors varies widely by institution. Surgical resection is the main treatment for all histological types.
The authors wish to thank all doctors in the 145 facilities accredited by the Japanese Society of Pediatric Surgeons for replying to the questionnaires (Supplementary material).
| 1. | Mylonas KS, Nasioudis D, Tsilimigras DI, Doulamis IP, Masiakos PT, Kelleher CM. A population-based analysis of a rare oncologic entity: Malignant pancreatic tumors in children. J Pediatr Surg. 2018;53:647-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Ferrari A, Brecht IB, Gatta G, Schneider DT, Orbach D, Cecchetto G, Godzinski J, Reguerre Y, Bien E, Stachowicz-Stencel T, Ost M, Magni C, Kearns P, Vassal G, Massimino M, Biondi A, Bisogno G, Trama A. Defining and listing very rare cancers of paediatric age: consensus of the Joint Action on Rare Cancers in cooperation with the European Cooperative Study Group for Pediatric Rare Tumors. Eur J Cancer. 2019;110:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Lin YJ, Burkhart R, Lu TP, Wolfgang C, Wright M, Zheng L, Wu HY, Chen CH, Lee SY, Wu CH, He J, Tien YW. Solid Pseudopapillary Neoplasms of the Pancreas Across Races Demonstrate Disparities with Comparably Good Prognosis. World J Surg. 2022;46:3072-3080. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 4. | Cheng H, Yang S, Ren Q, Yang W, Han W, Chang X, Zhu Z, Qin H, Wang H. Pancreatectomies for pediatric pancreatic tumors: A single institute experience from 2007 to 2018. J Pediatr Surg. 2020;55:1722-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Perez EA, Gutierrez JC, Koniaris LG, Neville HL, Thompson WR, Sola JE. Malignant pancreatic tumors: incidence and outcome in 58 pediatric patients. J Pediatr Surg. 2009;44:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 13191] [Article Influence: 1099.3] [Reference Citation Analysis (0)] |
| 7. | Pranger BK, van Dam JL, Groen JV, van Eijck CH, Koerkamp BG, Bonsing BA, Mieog JSD, Besselink MG, Busch OR, Kazemier G, de Jong KP, de Kleine RHJ, Molenaar IQ, Stommel MWJ, Gerhards MF, Coolsen MME, van Santvoort HC, van der Harst E, Klaase JM, de Meijer VE; Dutch Pancreatic Cancer Group. Pancreatic resection in the pediatric, adolescent and young adult population: nationwide analysis on complications. HPB (Oxford). 2021;23:1175-1184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Qi X, Zhou B, Liang F, Wang X. Prognostic factors of pancreatic tumors in children and adolescents: a population study based on the surveillance, epidemiology, and end results database. BMC Gastroenterol. 2024;24:108. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 9. | Picado O, Ferrantella A, Zabalo C, Rao K, Thorson CM, Sola JE, Perez EA. Treatment patterns and outcomes for pancreatic tumors in children: an analysis of the National Cancer Database. Pediatr Surg Int. 2020;36:357-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 10. | Dall'igna P, Cecchetto G, Bisogno G, Conte M, Chiesa PL, D'Angelo P, De Leonardis F, De Salvo G, Favini F, Ferrari A; TREP Group. Pancreatic tumors in children and adolescents: the Italian TREP project experience. Pediatr Blood Cancer. 2010;54:675-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 11. | Huang Y, Yang W, Hu J, Zhu Z, Qin H, Han W, Wang H. Diagnosis and treatment of pancreatoblastoma in children: a retrospective study in a single pediatric center. Pediatr Surg Int. 2019;35:1231-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Miyata H, Gotoh M, Hashimoto H, Motomura N, Murakami A, Tomotaki A, Hirahara N, Ono M, Ko C, Iwanaka T. Challenges and prospects of a clinical database linked to the board certification system. Surg Today. 2014;44:1991-1999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |