Published online Jan 15, 2024. doi: 10.4251/wjgo.v16.i1.182
Peer-review started: October 1, 2023
First decision: October 18, 2023
Revised: October 20, 2023
Accepted: December 11, 2023
Article in press: December 11, 2023
Published online: January 15, 2024
Processing time: 101 Days and 11.1 Hours
Colorectal cancer (CRC) plays a significant role in morbidity, mortality, and economic cost in the Belt and Road Initiative (“B and R”) countries. In addition, these countries have a substantial consumption of processed meat. However, the burden and trend of CRC in relation to the consumption of a diet high in processed meat (DHPM-CRC) in these “B and R” countries remain unknown.
To analyze the burden and trend of DHPM-CRC in the “B and R” countries from 1990 to 2019.
We used the 2019 Global Burden of Disease Study to collate information regarding the burden of DHPM-CRC. Numbers and age-standardized rates (ASRs) of deaths along with the disability-adjusted life years (DALYs) were determined among the “B and R” countries in 1990 and 2019. Using joinpoint regression analysis, the average annual percent change (AAPC) was used to analyze the temporal trends of age-standardized DALYs rate (ASDALR) from 1990 to 2019 and in the final decade (2010–2019).
We found geographical differences in the burden of DHPM-CRC among “B and R” countries, with the three highest-ranking countries being the Russian Federation, China, and Ukraine in 1990, and China, the Russian Federation, and Poland in 2019. The burden of DHPM-CRC generally increased in most member countries from 1990 to 2019 (all P < 0.05). The absolute number of deaths and DALYs in DHPM-CRC were 3151.15 [95% uncertainty interval (UI) 665.74-5696.64] and 83249.31 (95%UI 15628.64-151956.31) in China in 2019. However, the number of deaths (2627.57-2528.51) and DALYs (65867.39-55378.65) for DHPM-CRC in the Russian Federation has declined. The fastest increase in ASDALR for DHPM-CRC was observed in Vietnam, Southeast Asia, with an AAPC value of 3.90% [95% confidence interval (CI): 3.63%-4.16%], whereas the fastest decline was observed in Kyrgyzstan, Central Asia, with an AAPC value of -2.05% (95% CI: -2.37% to -1.73%). A substantial upward trend in ASR of mortality, years lived with disability, years of life lost, and DALYs from DHPM-CRC changes in 1990-2019 and the final decade (2010-2019) for most Maritime Silk Route members in East Asia, South Asia, Southeast Asia, North Africa, and the Middle East, as well as Central Europe, while those of the most Land Silk Route members in Central Asia and Eastern Europe have decreased markedly (all P < 0.05). The ASDALR for DHPM-CRC increased more in males than in females (all P < 0.05). For those aged 50-74 years, the ASDALR for DHPM-CRC in 40 members exhibited an increasing trend, except for 20 members, including 7 members in Central Asia, Maldives, and 12 high or high-middle social development index (SDI) members in other regions (all P < 0.05).
The burden of DHPM-CRC varies substantially across “B and R” countries and threatens public health. Relevant evidence-based policies and interventions tailored to the different trends of countries in SDIs or Silk Routes should be adopted to reduce the future burden of CRC in “B and R” countries via extensive collaboration.
Core Tip: This article analyzes the burden diet high in processed colorectal cancer attributable to a diet high in processed meat (DHPM-CRC) from the perspective of the organization of “B and R” countries with long-term political and economic ties. It focuses on the burden of DHPM-CRC through the strong horizontal link of trade and analyzes the differences between countries and their respective social development indexs (SDIs) via the vertical sharing of experience between countries with different SDI levels. The study explores the potential benefits of controlling the quantity and quality of DHPM with regard to deepening regional cooperation and high-quality trade development, thus advancing the initiative of a community of shared destiny in the field of health.
- Citation: Liu G, Li CM, Xie F, Li QL, Liao LY, Jiang WJ, Li XP, Lu GM. Colorectal cancer’s burden attributable to a diet high in processed meat in the Belt and Road Initiative countries. World J Gastrointest Oncol 2024; 16(1): 182-196
- URL: https://www.wjgnet.com/1948-5204/full/v16/i1/182.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v16.i1.182
Chronic non-communicable diseases, including malignant tumors such as colorectal cancer (CRC), have emerged as predominant health concerns in most countries across the globe[1]. According to GLOBOCAN 2020, CRC ranks third in terms of new cases, with over 1.92 million occurrences annually, and fifth in terms of mortality, causing approximately 0.94 million deaths[2]. The Belt and Road Initiative (“B and R”) includes a diverse set of countries across Asia, North Africa, the Middle East, and Europe, each at varying stages of economic development. These countries account for a substantial 79.36% of new CRC cases and a staggering 83.39% of global CRC-related deaths[3,4]. Disability-adjusted life years (DALYs) are among the most advanced indicators for assessing disease burden[5,6]. Current research on CRC burden has primarily focused on trends in incidence and mortality rates, with a limited in-depth exploration of the DALYs attributed to risk factors. This gap in understanding becomes even more pronounced in the context of global aging and the absence of collaborative efforts toward a shared future[7-10]. It is crucial to elucidate the role of risk factors in the CRC burden within rapidly aging developing countries, facilitating regional cooperation, reinforcing risk factor control, and developing effective interventions for cancer screening[11]. Many “B and R” countries fall within the low- to low-middle range of social development indexes (SDIs). The increase in CRC incidence in these countries may be largely attributed to their economic growth over the past three decades and the westernization of lifestyles, particularly evident in dietary patterns. This shift is marked by increased meat consumption[9,12]. Processed meat is often used as an important supplement for meat-poor countries[13]. The trade of processed meat between meat-rich and meat-poor countries among the “B and R” countries has formed a significant component of their economic exchanges[14]. For instance, China has established the Suifenhe area within the Heilongjiang Free Trade Zone, specializing in the processing of horse meat and beef sourced from Mongolia, Belarus, and Russia[15]. A diet high in processed meat (DHPM) is a recognized risk factor for CRC, with processed meat consumption linked to an 18% increase in CRC risk[16]. Therefore, in this study, we used DALYs from the Global Burden of Disease 2019 (GBD 2019) to evaluate the scope and disparities in the burden of CRC attributable to a DHPM-CRC across gender and age groups within “B and R” countries. The study aims to provide valuable insights into precision-coordinated prevention and control of CRC by exploring evidence-based policies and interventions.
This study included 66 member countries within the “B and R” initiative, with detailed classification published elsewhere[3]. The GBD 2019, which is an international collaborative surveillance system, conducted estimates for 369 diseases, 87 risk factors, and combinations of risk factors across 204 countries and territories spanning from 1990 to 2019. GBD generates estimates for disease burden indices, including incidence, prevalence, mortality, years lived with disability (YLDs), years of life lost (YLLs), and DALYs at regional, national, and global levels. A comprehensive methodology for GBD has been previously published[17,18]. DALYs are a composite measure used to assess the burden of disease, considering both disability and premature death. DALYs are calculated by combining YLLs and YLDs[5]. For this study, data pertaining to annual deaths attributed to DHPM-CRC, DALYs, and the respective age-standardized rates (ASRs) for gender and age groups from 1990 to 2019 in “B and R” countries were obtained from the institute for health metrics and evaluation website (https://vizhub.healthdata.org/gbd-results/). To ensure the reproducibility and transparency of results, our study adheres to the guidelines for accurate and transparent health estimates reporting[19].
We calculated the absolute numbers, age-standardized mortality rates (ASMRs), and age-standardized DALYs (ASDALR) for DHPM-CRC. The estimated metrics with 95% uncertainty intervals (UI) were reported. The UI is determined by resampling each number 1000 times from the posterior distributions and selecting the 2.5th and 97.5th order of the uncertainty distribution[17]. ASMR and ASDALR were estimated using a global age structure from 2019, categorized into five age groups: < 15 years, 15-49 years, 50-74 years, and ≥ 75 years. Regional data was stratified by SDI (high-, high-middle, middle-, low-middle, low-), which is a composite indicator reflecting a country’s income per capita, educational attainment, and total fertility rate in females aged under 25 years. Detailed methods of SDI development and computation are available elsewhere[20]. The trends in DHPM-CRC burden from 1990 to 2019 were assessed using the joinpoint regression software (version 4.9.0.0. March 2021)[3], with trend segments identified and reported with 95% confidence intervals (CIs). Average annual percent change (AAPC) for ASDALR in DHPM-CRC was evaluated by gender and age. Additionally, changes in AAPC for DHPM-CRC burden from 1990 to 2019 and from 2010 to 2019 were compared. Detailed descriptions of the relationship between AAPC and increasing/decreasing trends, as well as map visualizations, can be found elsewhere[3]. A significance level of P < 0.05 was considered statistically significant.
The mortality and DALYs associated with DHPM-CRC in “B and R” countries for 1990 and 2019 are presented in Table 1. Notably, there were significant geographical variations in both mortality and DALYs for DHPM-CRC among “B and R” countries. In 1990, the countries with the highest burden were the Russian Federation, China, and Ukraine. By 2019, the countries with the highest DHPM-CRC burden had shifted to China, the Russian Federation, and Poland. In 2019, China had a mortality of 3151.15 (95%UI 665.74-5696.64) and DALYs of 83249.31 (95%UI 15628.64-151956.31), whereas the Maldives in Southeast Asia had the lowest mortality and DALY, with values of 0.15 (95%UI: 0.08-0.24) and 3.78 (95%UI: 1.77-6.13), respectively. Among the “B and R” countries, the largest decreases in DHPM-CRC DALYs from 1990 to 2019 were observed in the Russian Federation (-15.92%, from 65867.39 to 55378.65) and Kyrgyzstan (-9.11%, from 382.85 to 347.99), whereas the countries with the most substantial increases were Qatar (703.33%, from 4.50 to 36.15) and Saudi Arabia (563.05%, from 94.58 to 627.11)
| Countries/regions | 1990 | 2019 | ||||||
| Mortality | DALYs | Mortality | DALYs | |||||
| Number | 95%UI | Number | 95%UI | Number | 95%UI | Number | 95%UI | |
| Global | 20185.18 | 7514.54 to 30917.34 | 462267.80 | 176029.61 to 707331.78 | 33927.57 | 11645.16 to 52095.67 | 735043.63 | 262813.06 to 1127202.7 |
| SDI regions | ||||||||
| High SDI | 12344.14 | 4087.4 to 18742.78 | 265997.94 | 92053.79 to 404795.34 | 17957.26 | 6062.65 to 27711.02 | 358289.23 | 126856.86 to 554318.85 |
| High-middle SDI | 6473.44 | 2283.01 to 10458.60 | 156995.36 | 58186.43 to 253727.23 | 10455.98 | 2857.06 to 16318.91 | 228839.61 | 62892.39 to 356760.51 |
| Middle SDI | 725.38 | 307.21 to 1102.05 | 20856.61 | 8535.2 to 31828.59 | 3293.44 | 1028.10 to 5402.14 | 87334.95 | 25247.15 to 143831.02 |
| Low-middle SDI | 425.88 | 172.40 to 660.88 | 12195.33 | 4977.73 to 18857.48 | 1620.04 | 653.61 to 2474.76 | 43433.53 | 16891.93 to 66781.46 |
| Low SDI | 208.16 | 46.97 to 364.09 | 6047.54 | 1354.61 to 10554.61 | 586.76 | 138.50 to 986.79 | 16859.65 | 3948.37 to 28481.72 |
| East Asia | ||||||||
| China | 573.31 | 264.38 to 905.72 | 16516.96 | 7250.01 to 26427.44 | 3151.15 | 665.74 to 5696.64 | 83249.31 | 15628.64 to 151956.31 |
| Central Asia | ||||||||
| Armenia | 8.56 | 0.99 to 15.10 | 254.23 | 29.36 to 442.90 | 14.27 | 1.58 to 25.73 | 341.48 | 38.58 to 614.85 |
| Azerbaijan | 18.81 | 2.99 to 31.37 | 608.86 | 96.76 to 1006.24 | 42.14 | 8.21 to 72.82 | 1266.76 | 267.40 to 2171.53 |
| Georgia | 24.15 | 4.03 to 40.47 | 700.62 | 118.11 to 1167.46 | 27.68 | 4.84 to 48.69 | 687.70 | 129.06 to 1191.91 |
| Kazakhstan | 78.79 | 14.76 to 128.11 | 2233.94 | 419.17 to 3575.49 | 91.43 | 15.34 to 151.9 | 2405.55 | 428.72 to 4030.59 |
| Kyrgyzstan | 13.09 | 2.31 to 21.74 | 382.85 | 73.43 to 628.18 | 12.87 | 2.05 to 22.15 | 347.99 | 63.93 to 598.29 |
| Mongolia | 3.18 | 0.49 to 5.57 | 92.58 | 16.59 to 161.63 | 7.15 | 1.34 to 12.67 | 221.58 | 43.87 to 392.11 |
| Tajikistan | 7.56 | 1.05 to 12.97 | 248.24 | 36.06 to 427.30 | 12.14 | 1.53 to 22.00 | 378.79 | 51.19 to 674.71 |
| Turkmenistan | 5.76 | 1.08 to 9.37 | 186.18 | 36.74 to 299.83 | 10.85 | 2.51 to 18.54 | 311.04 | 75.24 to 525.98 |
| Uzbekistan | 30.58 | 5.28 to 50.65 | 969.16 | 195.31 to 1589.62 | 61.56 | 11.66 to 107.04 | 1918.05 | 376.88 to 3309.55 |
| South Asia | ||||||||
| Bangladesh | 50.04 | 5.75 to 94.41 | 1434.83 | 169.4 to 2699.75 | 167.43 | 21.36 to 344.14 | 4280.95 | 566.55 to 8593.91 |
| Bhutan | 0.28 | 0.04 to 0.58 | 8.57 | 1.05 to 17.66 | 1.13 | 0.18 to 2.16 | 28.18 | 4.41 to 53.58 |
| India | 196.15 | 134.6 to 303.76 | 5667.35 | 3897.39 to 8874.42 | 956.93 | 635.07 to 1398.40 | 24428.69 | 16067.44 to 36082.08 |
| Nepal | 8.46 | 1.02 to 16.63 | 256.88 | 31.46 to 508.80 | 33.49 | 4.56 to 63.08 | 866.55 | 121.35 to 1638.59 |
| Pakistan | 84.11 | 12.69 to 147.02 | 2338.58 | 357.43 to 4004.62 | 262.35 | 41.49 to 482.79 | 7972.21 | 1317.46 to 14492.48 |
| Southeast Asia | ||||||||
| Cambodia | 2.16 | 1.19 to 3.45 | 65.00 | 33.16 to 107.42 | 10.01 | 4.75 to 16.32 | 276.67 | 121.07 to 464.88 |
| Indonesia | 34.39 | 24.4 to 44.10 | 1007.54 | 701.85 to 1310.91 | 156.04 | 87.49 to 237.82 | 4224.25 | 2335.66 to 6607.83 |
| Lao People's Democratic Republic | 1.15 | 0.57 to 1.94 | 34.67 | 16.14 to 60.07 | 3.57 | 1.59 to 6.12 | 103.41 | 43.05 to 183.42 |
| Malaysia | 14.66 | 2.93 to 26.72 | 392.23 | 74.28 to 703.87 | 70.05 | 10.22 to 135.78 | 1785.41 | 238.9 to 3483.87 |
| Maldives | 0.04 | 0.02 to 0.07 | 1.24 | 0.55 to 2.14 | 0.15 | 0.08 to 0.24 | 3.78 | 1.77 to 6.13 |
| Myanmar | 10.67 | 6.01 to 16.85 | 320.50 | 167.86 to 524.74 | 36.30 | 16.26 to 63.27 | 993.97 | 412.40 to 1812.61 |
| Philippines | 42.13 | 9.14 to 75.28 | 1307.32 | 259.26 to 2321.77 | 170.83 | 25.55 to 318.69 | 5150.70 | 713.11 to 9650.54 |
| Sri Lanka | 2.98 | 1.50 to 4.57 | 81.46 | 37.52 to 127.66 | 10.60 | 4.35 to 18.5 | 252.70 | 94.84 to 454.85 |
| Thailand | 17.02 | 11.26 to 23.09 | 481.34 | 309.77 to 666.1 | 66.39 | 29.64 to 114.00 | 1627.20 | 622.98 to 2935.75 |
| Viet Nam | 10.70 | 8.42 to 13.39 | 267.82 | 207.01 to 337.34 | 65.44 | 44.87 to 89.53 | 1734.20 | 1157.67 to 2486 |
| High-income Asia pacific | ||||||||
| Brunei Darussalam | 0.69 | 0.10 to 1.24 | 21.10 | 3.19 to 37.20 | 2.07 | 0.29 to 3.70 | 60.38 | 8.77 to 106.55 |
| Singapore | 7.96 | 1.08 to 14.03 | 211.42 | 27.54 to 372.52 | 24.84 | 2.71 to 43.91 | 583.27 | 62.65 to 1022.00 |
| North Africa and Middle East | ||||||||
| Afghanistan | 4.30 | 1.12 to 9.11 | 124.86 | 27.92 to 274.08 | 8.37 | 2.32 to 16.49 | 274.28 | 65.28 to 564.90 |
| Bahrain | 0.20 | 0.04 to 0.37 | 6.17 | 1.26 to 11.19 | 0.94 | 0.18 to 1.83 | 28.96 | 5.24 to 57.39 |
| Egypt | 15.04 | 3.33 to 26.15 | 461.56 | 95.34 to 812.9 | 64.31 | 9.15 to 133.63 | 1958.79 | 260.95 to 4054.83 |
| Iran (Islamic Republic of) | 16.16 | 4.54 to 29.76 | 476.35 | 123.59 to 887.22 | 64.86 | 18.49 to 111.79 | 1702.88 | 435.74 to 2968.75 |
| Iraq | 4.86 | 1.19 to 9.77 | 136.16 | 30.31 to 282.97 | 15.84 | 4.31 to 29.49 | 467.04 | 112.77 to 900.12 |
| Jordan | 1.41 | 0.34 to 2.69 | 42.35 | 9.40 to 81.53 | 7.55 | 1.68 to 14.05 | 214.03 | 43.98 to 400.30 |
| Kuwait | 0.40 | 0.09 to 0.72 | 12.43 | 2.62 to 22.66 | 2.47 | 0.52 to 4.74 | 67.41 | 13.27 to 128.85 |
| Lebanon | 2.60 | 0.6 to 5.01 | 67.45 | 14.42 to 131.45 | 8.53 | 2.08 to 16.26 | 194.00 | 43.10 to 372.37 |
| Oman | 0.38 | 0.11 to 0.74 | 11.09 | 2.86 to 22.21 | 1.30 | 0.30 to 2.49 | 38.63 | 8.09 to 76.72 |
| Palestine | 0.93 | 0.30 to 1.74 | 25.27 | 7.30 to 48.80 | 3.24 | 1.10 to 5.66 | 89.65 | 27.01 to 157.63 |
| Qatar | 0.14 | 0.03 to 0.27 | 4.50 | 0.77 to 8.98 | 1.09 | 0.19 to 2.17 | 36.15 | 5.90 to 72.22 |
| Saudi Arabia | 3.20 | 0.73 to 6.49 | 94.58 | 19.27 to 197.13 | 18.09 | 3.38 to 34.99 | 627.11 | 107.33 to 1227.35 |
| Syrian Arab Republic | 2.65 | 0.61 to 5.08 | 80.06 | 16.73 to 155.76 | 6.46 | 1.51 to 12.86 | 174.91 | 37.41 to 356.62 |
| Turkey | 40.12 | 9.69 to 74.42 | 1132.02 | 254.66 to 2143.91 | 118.79 | 23.06 to 227.55 | 2948.39 | 522.58 to 5711.33 |
| United Arab Emirates | 1.14 | 0.13 to 2.35 | 38.87 | 4.29 to 80.21 | 6.85 | 0.92 to 14.06 | 249.27 | 32.46 to 506.35 |
| Yemen | 1.90 | 0.58 to 3.78 | 56.39 | 15.85 to 114.49 | 6.41 | 2.06 to 12.16 | 189.19 | 55.64 to 368.67 |
| Central Europe | ||||||||
| Albania | 11.31 | 3.89 to 17.85 | 296.84 | 108.54 to 473.91 | 26.85 | 9.32 to 45.59 | 585.56 | 207.45 to 1031.68 |
| Bosnia and Herzegovina | 19.96 | 3.23 to 32.82 | 553.12 | 98.29 to 900.96 | 52.35 | 9.81 to 92.41 | 1186.04 | 234.7 to 2100.25 |
| Bulgaria | 98.01 | 17.25 to 159.39 | 2563.41 | 484.79 to 4131.57 | 181.34 | 42.79 to 300.82 | 4102.99 | 1034.14 to 6749.72 |
| Croatia | 15.36 | 2.99 to 27.54 | 361.08 | 67.40 to 648.47 | 26.31 | 4.78 to 50.31 | 517.68 | 91.80 to 996.80 |
| Czechia | 181.12 | 32.03 to 297.59 | 4194.79 | 811.51 to 6815.73 | 188.73 | 37.03 to 322.86 | 3895.53 | 825.87 to 6666.43 |
| Hungary | 166.23 | 26.01 to 268.12 | 3800.34 | 649.76 to 6118.43 | 261.40 | 56.38 to 434.87 | 5673.18 | 1347.95 to 9311.48 |
| Montenegro | 4.54 | 1.20 to 7.34 | 113.33 | 30.58 to 180.99 | 8.96 | 2.33 to 14.66 | 203.95 | 55.29 to 331.89 |
| North Macedonia | 10.27 | 1.86 to 16.96 | 276.41 | 53.18 to 451.64 | 28.16 | 5.61 to 49.59 | 679.70 | 145.98 to 1185.22 |
| Poland | 216.91 | 28.20 to 372.26 | 5095.47 | 666.31 to 8742.38 | 546.23 | 83.82 to 950.33 | 11527.70 | 1787.76 to 20046.17 |
| Romania | 116.09 | 16.42 to 194.90 | 3123.81 | 461.46 to 5221.26 | 383.92 | 95.92 to 627.87 | 8784.83 | 2367.61 to 14251.47 |
| Serbia | 76.24 | 11.38 to 131.83 | 1995.00 | 319.37 to 3414.82 | 124.69 | 16.97 to 220.02 | 2806.62 | 406.27 to 4997.03 |
| Slovakia | 52.43 | 8.54 to 86.69 | 1303.37 | 227.37 to 2134.07 | 119.49 | 28.18 to 201.82 | 2723.27 | 656.21 to 4579.18 |
| Slovenia | 33.41 | 11.09 to 54.36 | 751.17 | 258.76 to 1223.39 | 58.85 | 19.44 to 96.54 | 1121.96 | 389.15 to 1857.04 |
| Eastern Europe | ||||||||
| Belarus | 133.54 | 41.33 to 201.62 | 3412.26 | 1074.16 to 5114.01 | 146.30 | 41.63 to 241.15 | 3346.68 | 1023.98 to 5524.75 |
| Estonia | 30.37 | 11.47 to 51.31 | 720.88 | 274.29 to 1231.3 | 40.06 | 15.01 to 68.04 | 756.67 | 282.30 to 1336.20 |
| Latvia | 53.07 | 19.49 to 94.90 | 1269.38 | 444.72 to 2324.08 | 59.61 | 23.08 to 105.42 | 1169.57 | 431.45 to 2122.06 |
| Lithuania | 61.93 | 22.74 to 112.36 | 1499.31 | 535.39 to 2766.02 | 84.13 | 29.44 to 150.31 | 1673.06 | 557.78 to 3034.96 |
| Republic of Moldova | 45.84 | 13.45 to 69.43 | 1264.54 | 373.2 to 1911.48 | 53.78 | 13.70 to 87.43 | 1347.21 | 343.81 to 2182.01 |
| Russian Federation | 2627.57 | 911.55 to 4926.12 | 65867.39 | 22350.47 to 126827.42 | 2528.51 | 789.43 to 3916.69 | 55378.65 | 17294.58 to 86288.18 |
| Ukraine | 360.39 | 42.08 to 626.01 | 9531.71 | 1122.4 to 16437.15 | 434.32 | 52.43 to 754.61 | 11131.07 | 1400.72 to 19218.94 |
| Western Europe | ||||||||
| Cyprus | 4.25 | 0.86 to 6.88 | 96.47 | 20.83 to 152.9 | 10.95 | 2.08 to 18.34 | 227.23 | 45.61 to 375.83 |
| Greece | 82.10 | 13.14 to 135.31 | 1725.60 | 302.24 to 2801.49 | 159.07 | 28.01 to 264.30 | 2892.14 | 572.77 to 4645.95 |
| Israel | 32.40 | 4.18 to 55.21 | 698.17 | 99.64 to 1162 | 72.97 | 10.38 to 119.95 | 1438.25 | 230.44 to 2339.16 |
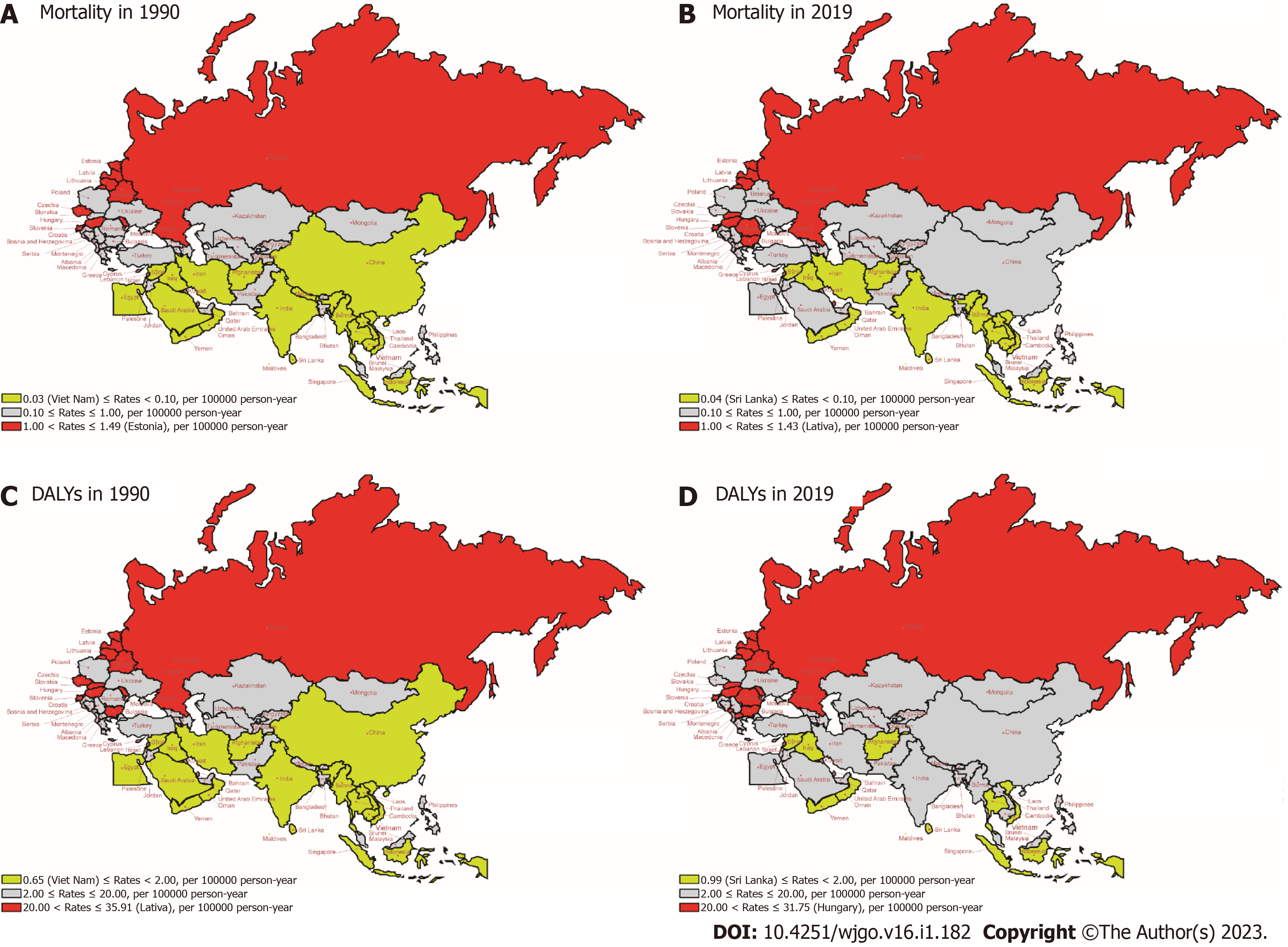
Figure 1 illustrates the ASMR and ASDALR of DHPM-CRC in 1990 and 2019 among “B and R” countries. Regions with higher ASMR and ASDALR were primarily concentrated in Eastern Europe and Central Europe, with Estonia having the highest rates in 1990 (1.49 per 100000 for ASMR and 35.41 per 100000 for ASDALR). In contrast, Sri Lanka exhibited the lowest ASMR and ASDALR in 1990 (0.03 per 100000 and 0.69 per 100000, respectively). In 2019, Sri Lanka continued to maintain the lowest ASMR and ASDALR (0.04 per 100000 and 0.99 per 100000, respectively), whereas Latvia exhibited the highest rates (1.43 per 100000 for ASMR and 31.61 per 100000, for ASDALR).
Of the 66 “B and R” countries, 65.15% (43/66) witnessed an increase in ASDALR for DHPM-CRC from 1990 to 2019, whereas 28.79% (19/66) observed a decrease. However, Romania experienced a substantial increase of 14.85 per 100000 in ASDALR, whereas the Russian Federation exhibited a decrease of 11.87 per 100000. Additional details are provided in Supplementary Table 1.
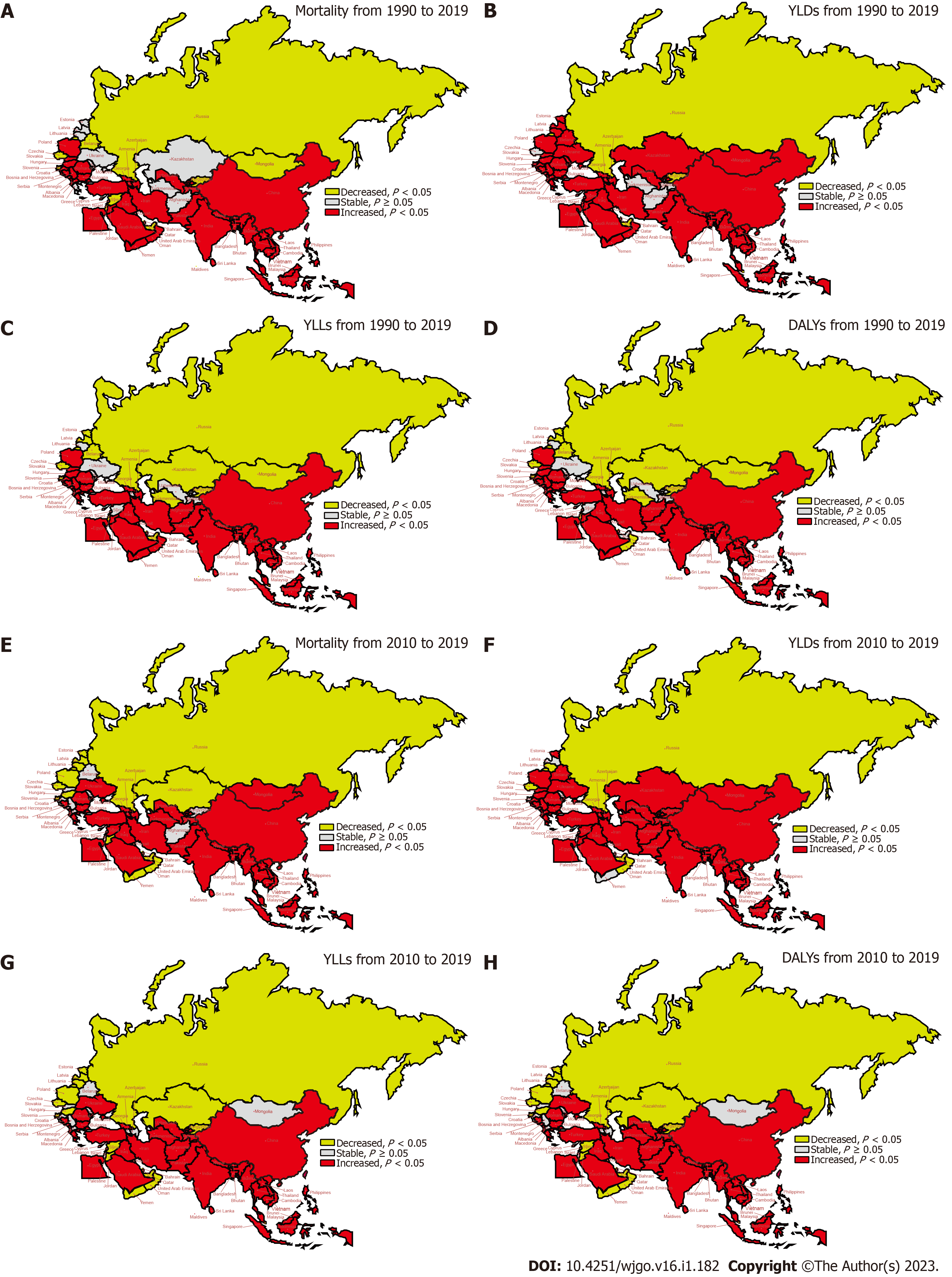
The trends in ASMR and ASDALR for DHPM-CRC from 1990 to 2019 and from 2010 to 2019 in “B and R” countries are illustrated in Figure 2. The most rapid decline in ASR for both mortality and DALYs was observed in the Russian Federation, Eastern Europe, with AAPC values of -1.58% (95%CI: -1.97% to -1.20%) and -1.99% (95%CI: -2.42% to -1.56%), respectively. Conversely, the fastest increase in ASR for mortality and DALYs occurred in Vietnam and Southeast Asia (mortality: AAPC = 3.70%; DALYs: AAPC = 3.90%; P < 0.001, respectively) from 1990 to 2019. Furthermore, the ASR for mortality, YLDs, YLLs, and DALYs in most Maritime Silk Route member countries of “B and R” in Southeast Asia, East Asia, South Asia, North Africa, and the Middle East, and Central Europe exhibited a significant increase from 1990 to 2019 and the final decade (2010-2019) (all P < 0.01). In contrast, the ASR for these measures in most Land Silk Route member countries of “B and R” in Central Asia and Eastern Europe experienced a substantial decrease (all P < 0.01). The ASDALR for global, high SDI and high-middle SDI countries decreased significantly, whereas those of middle SDI, low-middle SDI, and low SDI countries increased significantly (all P < 0.01). Further details are available in Supple
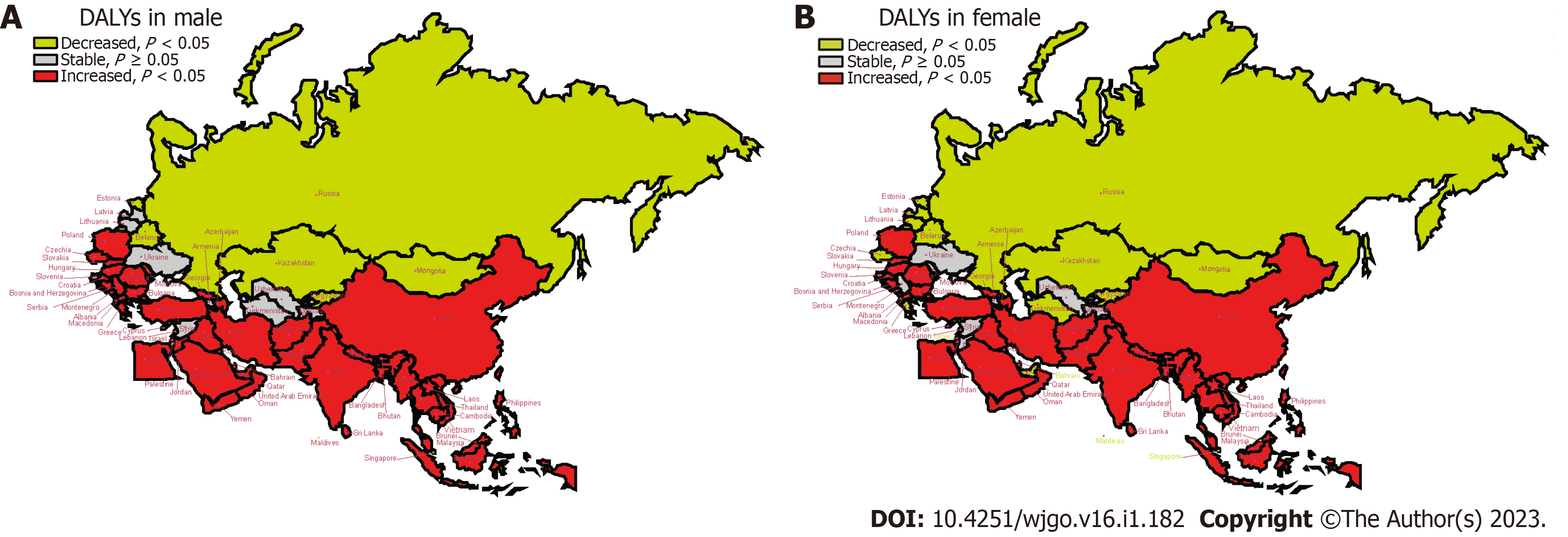
Figure 3 displays the AAPC values of ASDALR for DHPM-CRC in each member country of the “B and R” for males and females from 1990 to 2019.
For males, there was a marked increase in the ASDALR in most member countries of the “B and R” in East Asia (1/1), Southeast Asia (9/10), South Asia (5/5), North Africa and the Middle East (14/16), Central Europe (11/13), and Western Europe (2/3), whereas only individual member countries in Central Asia (2/9) and Eastern Europe (1/7) showed a significant increase (all P < 0.01).
For females, a significant increase in ASDALR was observed in the majority of member countries in East Asia (1/1), South Asia (5/5), Southeast Asia (9/10), North Africa and the Middle East (10/16), and Central Europe (9/13). However, individual member countries in Central Asia (2/9), Eastern Europe (0/7), and Western Europe (0/3) also displayed an increase (all P < 0.01).
The ASDALR for both males and females in global, high SDI and high-middle SDI countries decreased significantly, whereas those of middle SDI, low-middle SDI, and low SDI countries increased significantly (all P < 0.01) (Supplementary Table 3).
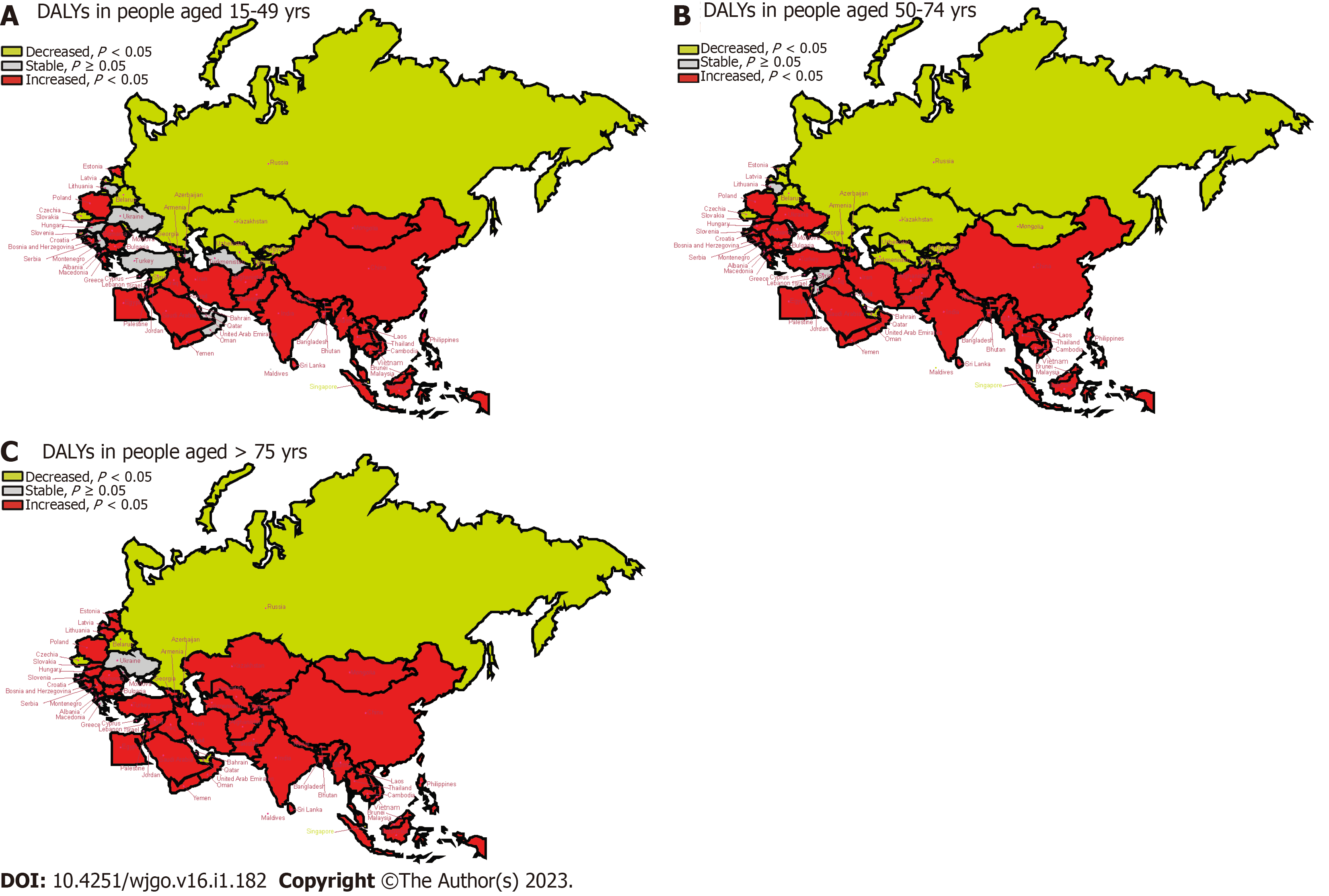
Figure 4 illustrates the trends of DALYs rates attributable to DHPM-CRC in various age groups from 1990 to 2019 among “B and R” countries. The results revealed that the DALYs rate experienced a decreasing trend in all age groups in the Russian Federation, Belarus, Czechia, Singapore, and the United Arab Emirates. In contrast, among member countries in East Asia (1/1), Southeast Asia (9/10), South Asia (5/5), North Africa and the Middle East (8/16), and Central Europe (7/13), the DALYs rate showed an increasing trend in all age groups (all P < 0.01). For individuals aged 15-49 years and 50-74 years, the DALYs rate displayed a decreasing trend in Central Asian countries such as Armenia, Kazakhstan, Kyrgyzstan, Tajikistan, Turkmenistan, Uzbekistan, as well as in Maldives in Southeast Asia, Slovenia in Central Europe, and Eastern European countries including Estonia, Latvia, and Lithuania (all P < 0.01). However, for people aged 15-49 years in global and high SDI countries, the DALYs rate showed no significant trend (all P > 0.05). For individuals aged 75 years or older, the AAPC values of the DALYs rate indicated an increasing trend in most member countries of the “B and R”. Nonetheless, the AAPC values in Bahrain, Slovenia, Moldova, Ukraine, and Greece exhibited considerable variation with no statistical significance. Refer to Supplementary Table 4 for more details.
Processed meat is a rich source of saturated fats and heme iron for humans. Countries with low meat production often rely on international trade to meet domestic meat demand, and processed meat is an essential component of this meat product trade owing to its easy preservation and transportation[14]. However, with increasing globalization and growing economies, residents with improved purchasing power are meeting their meat demand satisfactorily. Driven by the concept of an omnivorous diet, higher meat consumption has been observed in such residents with improved purchasing power compared with that has been observed in their peers, larger families, and people driven by the thought of a positive moral cognition towards meat consumption; the former often tend to overconsume meat, exceeding amounts recommended by the World Health Organization (WHO)[21]. DHPM, including bacon, hot dogs, salami, sausages, or processed turkey, may increase the risk of cancers, including CRC[22]. The European Prospective Investigation into Cancer and Nutrition has shown a correlation between DHPM and CRC risk[23]. Additionally, a meta-analysis has shown that DHPM increases cancer risk by 57%, and for every 50 g/d increase in processed meat consumption, cancer risk increases by 72%[24]. Moreover, multiple studies have shown that DHPM is positively correlated with breast cancer, colon cancer, CRC, rectal cancer, and lung cancer risk[15,25,26]. Processed meat products are the major dietary sodium source for populations in developed countries, accounting for approximately 20% of the total sodium intake for the general population[27]. Excessive sodium intake markedly increases blood pressure as well as increases the risk of cardiovascular diseases and tumors[28]. Additionally, some of the byproducts produced during meat processing are toxic and harmful to humans. These byproducts affect the living environment, and if not treated properly, they can cause pollution, ultimately entering human food and damaging human health. Carcinogenic studies on processed meat have shown that processed meat, including cured and smoked products, can produce carcinogens such as N-nitroso compounds (NOCs) and polycyclic aromatic hydrocarbons (PAHs)[29]. NOCs and animal-derived products containing antibiotics can affect the gut microbiota by affecting the adhesion of microorganisms to colonic cells, inhibiting tumor suppressor genes, activating oncogenes and genetic toxicity, and activating downstream targets of angiogenesis[29,30]. PAHs may cause cancer by forming DNA adducts and interfering with cell apoptosis[31]. Heme iron in processed meat induces cytotoxicity, promotes epithelial cell apoptosis and proliferation, induces lipid peroxidation, generates free radicals and DNA adducts, and catalyzes NOC formation, thereby promoting carcinogenesis[32]. Persistent organic pollutants accumulated in animal fat cells may adversely affect the endocrine pathway and increase the risk of various chronic diseases, including CRC[33]. Increased DHPM is correlated to increased plasma concentrations of biomarkers related to oxidative stress and inflammation, including C-reactive protein[34]. Additionally, many times livestock raised for consumption is treated with carcinogenic estrogen hormones such as estradiol-17β to promote growth, and some estrogen metabolites may result in free radical formation, epigenetic and inflammatory changes, immune and genetic toxicity, and hyperprolactinemia. Thus, consuming the meat of such hormone-treated animals may induce or promote carcinogenesis[15].
Recent studies have suggested that the “B and R” countries, which account for most new cases and deaths from CRC worldwide, may see a continued increase in the disease burden in the near future. Therefore, quantifying the DHPM-CRC burden and monitoring its trends are imperative[2,35]. Along with controlling recommended DHPM amounts, the “B and R” countries should cooperate to improve processed meat quality and reduce carcinogen levels by improving meat processing techniques, sharing efficient ecological solutions for processing processed meat by-products, developing new biodegradable plastics to avoid environmental pollution and secondary contamination, and rationally using inedible fats[28]. A Polish study showed that compared with similar European products, their unique cold cuts, sausages, and ham produced using special techniques contained higher levels of essential amino acids and micronutrients, tasted better, and were an important dietary source of balanced monounsaturated fatty acids for their residents[36]. Additionally, factors affecting nutrition quality, animal welfare, beliefs, chemical and biological hazards, and fraud may affect consumer perception regarding meat product safety[36]. An Italian study indicated that reducing meat consumption, especially in industrialized countries, is crucial for reducing health issues, and they found that two health framework prompts, namely societal impact and the individual impact of overconsumption, were more readily accepted by women, respondents with children at home, and individuals with lower perceived health status than others[21].
Most findings on the relationship between processed meat and CRC have been reported by studies conducted in developed countries, which have taken early measures to address the issue. For instance, the World Cancer Research Fund and the American Institute for Cancer Research have proposed dietary guidelines to restrict or avoid the consumption of red and processed meat in order to reduce cancer risk, and the American Cancer Society has issued dietary guidelines for the same, which has helped to reduce the burden of CRC over the years[37]. In Europe, the ASMR for CRC decreased by 16.9% (1990, 22.4/100000; 2019, 18.6/100000), and the ASDALR decreased by 18.6% (1990, 472.9/100000; 2019, 385.1/100000) from 1990 to 2019[38]. In Japan, the ASDALR showed a downward trend for CRC from 1990 to 2019, whereas CRC incidence and mortality rates in the United States have been decreasing slowly since 1985[39,40]. The present results indicated that the ASR mortality rate and DALYs of patients with CRC in the global, high SDI, and medium-high SDI countries have been decreasing at an annual rate of more than 1% from 1990 to 2019, which supports the previous results. Therefore, leveraging the experience of countries with a higher SDI on a global scale regarding CRC prevention and control and the internal coordination and cooperation among international organizations can help curb the increasing DHPM-CRC burden in most “B and R” countries, and this can serve as a model of cooperation for CRC prevention and control in low, medium-low, and medium SDI countries worldwide[41].
The results indicated that the DHPM-CRC burden on the “B and R” countries in 2019 was positively correlated with their population size. However, compared with DHPM-CRC DALYs in 1990, those in 2019 have decreased by 15.92% in Russia, whereas have increased by 6-7 times in Saudi Arabia and Qatar, which is consistent with the trend of the CRC burden in these countries[7,42]. The reasons behind these observations may be that the healthcare system in Russia, which was previously supported by Soviet tax subsidies, has adopted mandatory health insurance since 1990, providing more funding for national health projects, and Russia has implemented measures for the early diagnosis of CRC during this period, including population screening, adenoma removal, treatment, and the widespread use of aspirin[43]. Lifestyle choices such as red meat consumption, sedentary lifestyles, and increased calorie intake contribute to the CRC incidence increase in Saudi Arabia[44]. Despite the significant investments in healthcare, sufficient attention has not been paid to predictive diagnosis and targeted prevention. Despite the availability of sufficient finances, Qatar has low awareness regarding CRC prevention and treatment among residents, and reluctance towards screening and a lack of reminders from healthcare providers are some other screening barriers[45].
The present results showed that “B and R” countries in Central Europe had high DALYs for DHPM-CRC and showed highly increased incidence and mortality rates. The reason may be that these countries are both major meat-producing and high meat-consuming countries, with daily per capita intake exceeding the recommended amount by the WHO[46]. Conversely, the increased CRC incidence in Central European countries (such as the Czech Republic and Croatia) may be attributed to the Westernized lifestyle characterized by obesity and lack of exercise[47]. However, Poland proposed and vigorously implemented a national cancer control program around 2005, including free screening colonoscopy for early CRC detection, through which Polish residents could undergo CRC screening and receive effective treatment (including radiotherapy)[48]. Croatia launched a national cancer screening program in 2007 to actively address the challenges of the increasing burden of CRC[49]. The decrease in CRC incidence of some developed countries has been attribute to screening, which can detect polyps that can be removed before they become cancerous. Therefore, future attention should be focused on the many regions with a growing and aging population and an increasingly westernized lifestyle[2]. For example, a CRC screening program using the fecal immunochemical test was recently piloted in Thailand and China Shanghai, proved that CRC screening is also effective in controlling the rising CRC incidence rate in the “B and R” countries[50,51].
The present results showed that, unlike the global trend of decline, the ASDALR of DHPM-CRC in most “B and R” countries in Asia, North Africa, and the Middle East increased, which could be attributed to economic development in the countries. CRC occurrence is strongly correlated with economic levels, and these countries experienced economic transformation from 1990 to 2019[52]. During this period, significant changes were observed in the living environment and lifestyle of the residents, with a tendency towards Westernization and decreasing physical activity[3,53].
Additionally, the results showed gender differences in the ASR mortality and DALYs for DHPM-CRC in the “B and R” countries. Differences were observed in the overall burden of CRC between men and women[7,54]. In China in 2020, the ratio of newly diagnosed cases of CRC between men and women was 1.35:1, and the ratio of deaths between men and women was 1.36:1[14]. Moreover, differences were observed in dietary habits between men and women. Women were more likely to take health education and pay attention to the effect of several factors on meat quality and reduce processed meat intake as needed[36,42]. Additionally, in Greece, Cyprus, and Lithuania, the ASDALR for men increased, whereas that for women decreased, which may be attributed to the higher coverage rate of CRC screening and colonoscopy response rate among women in these high or high-middle SDI countries[55,56].
Age differences were observed for the ASDALR of DHPM-CRC in the “B and R” countries. Inconsistencies were observed in the disease burden on people aged 50 and above in high and high-middle SDI countries, where the burden decreased, whereas in the middle, low-middle, and low-SDI countries, the burden increased across all age groups. However, in three high SDI Eastern European countries, namely Estonia, Latvia, and Lithuania, the DALY rate of DHPM-CRC among residents aged 75 and above increased significantly. In seven Central Asian countries, namely Armenia, Kazakhstan, Kyrgyzstan, Mongolia, Tajikistan, Turkmenistan, Uzbekistan, Afghanistan, and Syria, the DALY rates decreased among residents aged 50-74 years. Similarly, in five Central Asian countries namely Armenia, Kazakhstan, Kyrgyzstan, Tajikistan, Uzbekistan, and the Maldives, the DALY rates decreased among residents aged 15-49 years. These differences were observed because of the varying degrees of dietary changes among residents of different ages in different countries and different CRC screening strategies. In Kazakhstan, after implementing the CRC screening program, the incidence rate in residents over 70 years old increased by 16.0 per 100000, whereas that in the 65-69 age group increased by 23.3 per 100000[30].
The present visual analysis results showed differences in the trend of DHPM-CRC burden between the Maritime Silk Route and the Land Silk Route along the “B and R” countries. Significant differences were observed even after adjusting for year ranges (1990-2019 vs. 2010-2019), gender (male vs. female), and age groups. The ASR mortality rate, YLLs, YLDs, and DALYs in most Maritime Silk Route countries increased, whereas those in most inland countries associated with the Land Silk Road decreased. These changes may be attributed to economic globalization, where coastal countries have exhibited higher economic growth rates and the dietary patterns of their residents have shifted towards high meat intake, similar to residents in high and high-middle SDI countries. This has increased the CRC burden caused by processed meat consumption. Inland countries are generally high meat producers and consumers, and through trade, they have expanded their diverse diets. Additionally, these countries have benefited from increased CRC screening, which has effectively reduced the CRC burden caused by processed meat consumption[7,40,56,57].
The strength of this study is that it analyzed the DHPM-CRC burden from the perspective of the organization of the “B and R” countries with long-term political and economic ties. It focused on the DHPM-CRC burden from the perspective of the horizontal strong link of trade and analyzed the differences between countries and their respective SDI levels through the vertical sinking of experience. Additionally, the study investigated the potential benefits of controlling DHPM quantity and quality in the context of regional cooperation and high-quality trade development, thus taking an initiative to establish cooperation and coordination between countries with similarities in health-related aspects.
Nevertheless, the study has some limitations. First, it is based on the secondary analysis of the GBD2019 data; therefore, we could not avoid the inherent limitations of all GBD studies. Second, the analysis of the trends of DHPM-CRC mortality, YLDs, YLLs, and DALYs in 66 Belt and Road countries during 1990-2019 according to the actual join points generated redundant information; thus, we referred to the literature on cancer statistics to analyze the trends observed in the entire period and the last decade[2].
In conclusion, unlike general global studies, a quantitative and in-depth analysis focusing on the DHPM-CRC burden helped clarify the effect of a single factor (processed meat consumption) on the CRC burden. Additionally, international organizations that have strong links in the context of meat trade and consumption are excellent samples for investigating the reduction of the disease burden. We found differences in socioeconomic levels, genders, and ages regarding the DHPM-CRC burden in the “B and R” countries. Additionally, targeted cooperation among the “B and R” countries was possible with respect to CRC prevention and control, especially regarding the different development trends of the disease burden among countries within the same organization. The study provides new perspectives on CRC prevention and control.
Currently, the research on the burden of colorectal cancer (CRC) mainly focuses on the trend analysis of incidence and mortality rates, with only a few in-depth studies on the disability-adjusted life years (DALYs) caused by risk factors, especially in the context of global aging and the lack of cooperation to achieve a community of shared future.
It is crucial to clarify the contribution of risk factors to the burden of CRC in developing countries with rapid aging rates toward enhancing regional cooperation, strengthening control of risk factors, and developing effective intervention measures for cancer screenings.
In this study, we employed DALYs in the Global Buden of Disease 2019 (GBD 2019) study to analyze the magnitude and variations of diet high in processed meat-induced CRC (DHPM-CRC) burden in different gender and age groups, as well as to explore the relevant evidence-based policies and interventions in the Belt and Road Initiative (“B and R”) countries so as to provide a reference for precision-coordinated prevention and control of CRC.
The absolute numbers and age-standardized mortality rates (ASMR) and age-standardized DALYs (ASDALR) for DHPM-CRC were calculated. For the estimated metrics, the 95% uncertainty interval was reported, which was calculated by extracting each number 1000 times from the posterior distributions by using the 2.5th and 97.5th order of the uncertainty distribution. ASMR and ASDALR were estimated using a global age structure in 2019 and divided by age into 5 groups: < 15 years, 15-49 years, 50-74 years, and ≥ 75 years. The regional data were stratified by social development index (SDI) (as high-, high-middle, middle-, low-middle, and low-), which is a composite indicator of a country’s lag-distributed income per capita, educational attainment, and the total fertility rate in women aged < 25 years. The methods of SDI development and computation are detailed elsewhere. The trends of DHPM-CRC’s burden from 1990 to 2019 were assessed by the join point regression software (version 4.9.0.0. March 2021) by using the 95% confidence intervals for the identified trend segment. In addition, we evaluated the average annual percent change (AAPC) of ASDALR for DHPM-CRC in gender and age. Meanwhile, we compared the changes in AAPC of burden in DHPM-CRC from 1990 to 2019 or from 2010 to 2019. The relationship between AAPC and increasing/decreasing trend or stability and the map visualization are detailed elsewhere. P < 0.05 was considered to indicate statistical significance.
The results indicated that: (1) The burden of DHPM-CRC in “B and R” countries in 2019 was positively correlated with the population size; (2) the “B and R” member countries in Central Europe not only exhibit high DALYs of DHPM-CRC but also a large increase in these rates; (3) there are gender differences in the ASR mortality and DALYs of DHPM-CRC in “B and R” countries; (4) there are age differences in the ASDALR of DHPM-CRC in countries along the “B and R” countries; and (5) differences were detected in the trend of DHPM-CRC burden between the Maritime Silk Route and the Land Silk Route along the “B and R” countries.
Unlike the general global studies, a quantitative and in-depth analysis focusing on the burden of DHPM-CRC helped clarify the impact of a single factor on the burden of CRC, and international organizations with strong links based on this factor are excellent samples for exploring the reduction of disease burden. We noted socioeconomic level, gender, and age differences in the burden of DHPM-CRC in “B and R” countries, thus making targeted cooperation in CRC prevention and control among “B and R” countries possible, especially considering the different development trends of disease burden among countries within the same organization to provide fresh perspectives on CRC prevention and control research.
In this study, we employed DALYs in the GBD 2019 to analyze the magnitude and variations of DHPM-CRC burden in the gender and age groups and explore the relevant evidence-based policies and interventions in the “B and R” countries so as to provide a reference for precision coordinated prevention and control of CRC.
We thank Medjaden Inc. for its assistance in the preparation of this manuscript.
Provenance and peer review: Invited article; Externally peer-reviewed.
Peer-review model: Single-blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ahmed M, United States; Batyrbekov K, Kazakhstan; Mohamed SY, Egypt S-Editor: Qu XL L-Editor: A P-Editor: Yu HG
| 1. | NCD Countdown 2030 collaborators. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392:1072-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 540] [Cited by in RCA: 736] [Article Influence: 105.1] [Reference Citation Analysis (1)] |
| 2. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 63668] [Article Influence: 15917.0] [Reference Citation Analysis (174)] |
| 3. | Zhang Y, Luo Z, Yi J, Zhu J, Qiu Y, Xu X, Xie W, Wu J, Lv H, Mou C, Zhang W, Li X. Burden and trends of stroke attributable to dietary risk factors from 1990 to 2019 in the Belt and Road Initiative countries: an analysis from the global burden of disease study 2019. Front Nutr. 2023;10:1235271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Morgan E, Arnold M, Gini A, Lorenzoni V, Cabasag CJ, Laversanne M, Vignat J, Ferlay J, Murphy N, Bray F. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Gut. 2023;72:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 848] [Article Influence: 424.0] [Reference Citation Analysis (1)] |
| 5. | Murray CJL, Lopez AD. Measuring global health: motivation and evolution of the Global Burden of Disease Study. Lancet. 2017;390:1460-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 126] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 6. | Devleesschauwer B, Havelaar AH, Maertens de Noordhout C, Haagsma JA, Praet N, Dorny P, Duchateau L, Torgerson PR, Van Oyen H, Speybroeck N. Calculating disability-adjusted life years to quantify burden of disease. Int J Public Health. 2014;59:565-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 165] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 7. | GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7:627-647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 327] [Cited by in RCA: 350] [Article Influence: 116.7] [Reference Citation Analysis (0)] |
| 8. | Sharma R, Rakshit B. Spatial and temporal patterns of colorectal cancer in Asia, 1990-2019. Int J Clin Oncol. 2023;28:255-267. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Muzi CD, Banegas MP, Guimarães RM. Colorectal cancer disparities in Latin America: Mortality trends 1990-2019 and a paradox association with human development. PLoS One. 2023;18:e0289675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Zhang SZ, Zhang L, Xie L. Cancer Burden in China during 1990-2019: Analysis of the Global Burden of Disease. Biomed Res Int. 2022;2022:3918045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Yang B, Lv Y, Shi O, Yan M, Li X, Kang W, Yang Y, Wang W, Wang Q. The global burden of colorectal cancer attributable to high plasma glucose in 204 countries and territories, 1990-2019: an analysis of the Global Burden of Disease Study. Public Health. 2023;217:46-53. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Yu D, Ou Z, Zhang W, He H, Li Y, He W, Zhang M, Gao Y, Wu F, Chen Q. Global and national trends in years of life lost and years lived with disability caused by three common gastrointestinal cancers from 1990 to 2019. BMC Gastroenterol. 2022;22:493. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Huang Y, Cao D, Chen Z, Chen B, Li J, Guo J, Dong Q, Liu L, Wei Q. Red and processed meat consumption and cancer outcomes: Umbrella review. Food Chem. 2021;356:129697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 14. | Zhou G, Zhang W, Xu X. China's meat industry revolution: challenges and opportunities for the future. Meat Sci. 2012;92:188-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Chen W, Zhang H. Characterizing the Structural Evolution of Cereal Trade Networks in the Belt and Road Regions: A Network Analysis Approach. Foods. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 16. | Farvid MS, Sidahmed E, Spence ND, Mante Angua K, Rosner BA, Barnett JB. Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2021;36:937-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 195] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 17. | GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11327] [Cited by in RCA: 9637] [Article Influence: 1927.4] [Reference Citation Analysis (35)] |
| 18. | GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223-1249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5702] [Cited by in RCA: 4911] [Article Influence: 982.2] [Reference Citation Analysis (1)] |
| 19. | Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, Grove JT, Hogan DR, Hogan MC, Horton R, Lawn JE, Marušić A, Mathers CD, Murray CJ, Rudan I, Salomon JA, Simpson PJ, Vos T, Welch V; (The GATHER Working Group). Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016;388:e19-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 890] [Article Influence: 98.9] [Reference Citation Analysis (1)] |
| 20. | GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160-1203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1253] [Cited by in RCA: 1083] [Article Influence: 216.6] [Reference Citation Analysis (1)] |
| 21. | Caso G, Rizzo G, Migliore G, Vecchio R. Loss framing effect on reducing excessive red and processed meat consumption: Evidence from Italy. Meat Sci. 2023;199:109135. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC monographs on the evaluation of carcinogenic risks to humans. Ingested nitrate and nitrite, and cyanobacterial peptide toxins. IARC Monogr Eval Carcinog Risks Hum. 2010;94:v-vii, 1. [PubMed] |
| 23. | Ubago-Guisado E, Rodríguez-Barranco M, Ching-López A, Petrova D, Molina-Montes E, Amiano P, Barricarte-Gurrea A, Chirlaque MD, Agudo A, Sánchez MJ. Evidence Update on the Relationship between Diet and the Most Common Cancers from the European Prospective Investigation into Cancer and Nutrition (EPIC) Study: A Systematic Review. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 84] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 24. | Han MA, Zeraatkar D, Guyatt GH, Vernooij RWM, El Dib R, Zhang Y, Algarni A, Leung G, Storman D, Valli C, Rabassa M, Rehman N, Parvizian MK, Zworth M, Bartoszko JJ, Lopes LC, Sit D, Bala MM, Alonso-Coello P, Johnston BC. Reduction of Red and Processed Meat Intake and Cancer Mortality and Incidence: A Systematic Review and Meta-analysis of Cohort Studies. Ann Intern Med. 2019;171:711-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 25. | Kim SR, Kim K, Lee SA, Kwon SO, Lee JK, Keum N, Park SM. Effect of Red, Processed, and White Meat Consumption on the Risk of Gastric Cancer: An Overall and Dose⁻Response Meta-Analysis. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 26. | Zhang S, Wang Q, He J. Intake of red and processed meat and risk of renal cell carcinoma: a meta-analysis of observational studies. Oncotarget. 2017;8:77942-77956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Delgado J, Ansorena D, Van Hecke T, Astiasarán I, De Smet S, Estévez M. Meat lipids, NaCl and carnitine: Do they unveil the conundrum of the association between red and processed meat intake and cardiovascular diseases?_Invited Review. Meat Sci. 2021;171:108278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Toldrá F, Reig M, Mora L. Management of meat by- and co-products for an improved meat processing sustainability. Meat Sci. 2021;181:108608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 29. | Abu-Ghazaleh N, Chua WJ, Gopalan V. Intestinal microbiota and its association with colon cancer and red/processed meat consumption. J Gastroenterol Hepatol. 2021;36:75-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 30. | Zhylkaidarova A, Kaidarova D, Batyrbekov K, Shatkovskaya O, Begimbetova D. Trends of Colorectal Cancer Prevalence in Kazakhstan Related to Screening. Clin Endosc. 2021;54:32-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (2)] |
| 31. | Pratt MM, John K, MacLean AB, Afework S, Phillips DH, Poirier MC. Polycyclic aromatic hydrocarbon (PAH) exposure and DNA adduct semi-quantitation in archived human tissues. Int J Environ Res Public Health. 2011;8:2675-2691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 32. | Gamage SMK, Dissabandara L, Lam AK, Gopalan V. The role of heme iron molecules derived from red and processed meat in the pathogenesis of colorectal carcinoma. Crit Rev Oncol Hematol. 2018;126:121-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 33. | Guo W, Pan B, Sakkiah S, Yavas G, Ge W, Zou W, Tong W, Hong H. Persistent Organic Pollutants in Food: Contamination Sources, Health Effects and Detection Methods. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 193] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 34. | Azadbakht L, Esmaillzadeh A. Red meat intake is associated with metabolic syndrome and the plasma C-reactive protein concentration in women. J Nutr. 2009;139:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 189] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 35. | Chen Y, Chen T, Fang JY. Burden of gastrointestinal cancers in China from 1990 to 2019 and projection through 2029. Cancer Lett. 2023;560:216127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 36. | de Araújo PD, Araújo WMC, Patarata L, Fraqueza MJ. Understanding the main factors that influence consumer quality perception and attitude towards meat and processed meat products. Meat Sci. 2022;193:108952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 37. | Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV, Gapstur S, Patel AV, Andrews K, Gansler T; American Cancer Society 2010 Nutrition and Physical Activity Guidelines Advisory Committee. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62:30-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 956] [Cited by in RCA: 897] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 38. | Sharma R. A comparative examination of colorectal cancer burden in European Union, 1990-2019: Estimates from Global Burden of Disease 2019 Study. Int J Clin Oncol. 2022;27:1309-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Shiratori Y, Hutfless S, Rateb G, Fukuda K. The burden of gastrointestinal diseases in Japan, 1990-2019, and projections for 2035. JGH Open. 2023;7:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70:145-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2268] [Cited by in RCA: 3239] [Article Influence: 647.8] [Reference Citation Analysis (2)] |
| 41. | Song M. Global epidemiology and prevention of colorectal cancer. Lancet Gastroenterol Hepatol. 2022;7:588-590. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 42. | GBD 2019 Australia Collaborators. The burden and trend of diseases and their risk factors in Australia, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2023;8:e585-e599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 36] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 43. | Avksentyeva M. Colorectal cancer in Russia. Eur J Health Econ. 2010;10 Suppl 1:S91-S98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 44. | Alyabsi M, Alhumaid A, Allah-Bakhsh H, Alkelya M, Aziz MA. Colorectal cancer in Saudi Arabia as the proof-of-principle model for implementing strategies of predictive, preventive, and personalized medicine in healthcare. EPMA J. 2020;11:119-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 45. | Al-Dahshan A, Abushaikha S, Chehab M, Bala M, Kehyayan V, Omer M, AlMohamed O, Al-Kubaisi N, Selim N. Perceived Barriers to Colorectal Cancer Screening among Eligible Adults in Qatar and the Associated Factors: A Cross- Sectional Study. Asian Pac J Cancer Prev. 2021;22:45-51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 46. | Waraczewski R, Bartoń M, Stasiak DM, Sołowiej BG. Long-matured cured meats from Poland and Europe compared - An overview. Meat Sci. 2023;206:109336. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 47. | Zatoński W, Didkowska J. Closing the gap: cancer in Central and Eastern Europe (CEE). Eur J Cancer. 2008;44:1425-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 48. | Ruszkowski J. Colorectal cancer management in Poland: current improvements and future challenges. Eur J Health Econ. 2010;10 Suppl 1:S57-S63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Kirac I, Sekerija M, Simunović I, Zgaga L, Velimir Vrdoljak D, Kovacević D, Kulis T, Znaor A. Incidence and mortality trends of gastric and colorectal cancers in Croatia, 1988-2008. Croat Med J. 2012;53:124-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 50. | Khuhaprema T, Sangrajrang S, Lalitwongsa S, Chokvanitphong V, Raunroadroong T, Ratanachu-Ek T, Muwonge R, Lucas E, Wild C, Sankaranarayanan R. Organised colorectal cancer screening in Lampang Province, Thailand: preliminary results from a pilot implementation programme. BMJ Open. 2014;4:e003671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 51. | Li X, Qian M, Zhao G, Yang C, Bao P, Chen Y, Zhou X, Yan B, Wang Y, Zhang J, Sun Q. The performance of a community-based colorectal cancer screening program: Evidence from Shanghai Pudong New Area, China. Prev Med. 2019;118:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 52. | Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14:1165-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 549] [Cited by in RCA: 641] [Article Influence: 53.4] [Reference Citation Analysis (0)] |
| 53. | Nejadghaderi SA, Roshani S, Mohammadi E, Yoosefi M, Rezaei N, Esfahani Z, Azadnajafabad S, Ahmadi N, Shahin S, Kazemi A, Namazi Shabestari A, Khosravi A, Mokdad AH, Larijani B, Farzadfar F. The global, regional, and national burden and quality of care index (QCI) of colorectal cancer; a global burden of disease systematic analysis 1990-2019. PLoS One. 2022;17:e0263403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 54. | Roy HK, Bianchi LK. Differences in colon adenomas and carcinomas among women and men: potential clinical implications. JAMA. 2009;302:1696-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 55. | Kliemann N, Rauber F, Bertazzi Levy R, Viallon V, Vamos EP, Cordova R, Freisling H, Casagrande C, Nicolas G, Aune D, Tsilidis KK, Heath A, Schulze MB, Jannasch F, Srour B, Kaaks R, Rodriguez-Barranco M, Tagliabue G, Agudo A, Panico S, Ardanaz E, Chirlaque MD, Vineis P, Tumino R, Perez-Cornago A, Andersen JLM, Tjønneland A, Skeie G, Weiderpass E, Monteiro CA, Gunter MJ, Millett C, Huybrechts I. Food processing and cancer risk in Europe: results from the prospective EPIC cohort study. Lancet Planet Health. 2023;7:e219-e232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 52] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 56. | Dutta A, Pratiti R, Kalantary A, Aboulian A, Shekherdimian S. Colorectal Cancer: A Systematic Review of the Current Situation and Screening in North and Central Asian Countries. Cureus. 2023;15:e33424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 57. | Lavingia V, Gore AA. Time for colorectal cancer screening in India! Indian J Cancer. 2021;58:315-316. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |