Published online Jul 15, 2023. doi: 10.4251/wjgo.v15.i7.1311
Peer-review started: April 15, 2023
First decision: May 4, 2023
Revised: May 14, 2023
Accepted: May 26, 2023
Article in press: May 26, 2023
Published online: July 15, 2023
Processing time: 88 Days and 4.5 Hours
Liver interventional surgery is a relatively safe and minimally invasive surgery. However, for patients who have undergone Whipple surgery, the probability of developing a liver abscess after liver interventional surgery is very high. Fungal liver abscess has a high mortality rate, especially when complicated with mali
A 54-year-old woman with pancreatic head cancer received albumin-bound paclitaxel in combination with gemcitabine chemotherapy after laparoscopic pancreaticoduodenectomy. Liver metastasis was found 1 mo after completion of 8 cycles of chemotherapy, followed by ablation of the liver metastasis. After half a month of liver metastasis ablation, the patient experienced fever after chemo
Effective treatment of Candida albicans liver abscess requires early detection, percutaneous catheter drainage, and 5 wk of antifungal therapy. Meanwhile, complications such as COVID-19 should be actively managed and nutritional support should be provided.
Core Tip: Fungal liver abscess is rare and has a high mortality rate, especially when combined with malignant tumor, diabetes, coronavirus disease 2019 (COVID-19), and other complications, which increase the difficulty of treatment. However, there are no guidelines or expert consensus on the course of antifungal drugs. We present a rare case of Candida albicans liver abscess complicated with COVID-19 after ablation of liver metastasis from pancreatic head cancer. The patient was successfully cured after percutaneous catheter drainage, antifungal therapy, therapeutic management of comorbidities and nutritional support.
- Citation: Hu W, Lin X, Qian M, Du TM, Lan X. Treatment of Candida albicans liver abscess complicated with COVID-19 after liver metastasis ablation: A case report. World J Gastrointest Oncol 2023; 15(7): 1311-1316
- URL: https://www.wjgnet.com/1948-5204/full/v15/i7/1311.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v15.i7.1311
The incidence of liver abscess after liver intervention is very high in patients who have undergone Whipple surgery. Despite aggressive and appropriate treatment, the mortality rate for liver abscess remains high, particularly when combined with coronavirus disease 2019 (COVID-19). Fungal liver abscess is rare, and there are no guidelines or expert consensus on the timing of antifungal drug use for this condition. In this report, we present a rare case of Candida albicans liver abscess complicated by COVID-19 after liver metastasis ablation for pancreatic head cancer. The patient was treated with percutaneous catheter drainage, antifungal therapy, therapeutic management of comorbidities and nutritional support.
A 54-year-old woman was diagnosed with pancreatic head cancer for 8 mo and had liver metastasis ablation for 2 wk.
Eight months ago, the patient was hospitalized for sprained right wrist. It was unexpected to discover that she had pancreatic head cancer and diabetes. She subsequently underwent laparoscopic pancreaticoduodenectomy, and histopathologic results revealed pancreatic adenocarcinoma with mucinous adenomas (about 5%-10% of which were sig-ring cell carcinomas), G3/poorly differentiated, and invasion of nerves and lymphatic vessels. Following surgery, she completed 8 cycles of chemotherapy with albumin-bound paclitaxel and gemcitabine. One month after completing chemotherapy, contrast-enhanced abdominal computed tomography (CT) revealed liver metastasis in the right lobe, with a maximum cross-section of approximately 2.0 cm × 1.9 cm. Two weeks ago, the patient underwent CT-guided ablation of liver metastasis and was discharged after receiving treatment for infection prevention and liver protection. The patient had no discomfort and was admitted to the hospital for chemotherapy.
The patient sprained her right wrist more than 8 mo ago, and she had no other known medical conditions.
Her father died of an unknown type of cancer at the age 49.
The patient’s vital signs were stable, and her skin and sclera showed no signs of yellowing. The abdomen was flat and soft, and the right lower abdomen was tender and percussive.
Blood routine, renal function, coagulation, carcinoembryonic antigen, and carbohydrate antigen (CA) 19-9 results were all within the normal range. However, some laboratory results were abnormal, including C-reactive protein, 4.62 mg/L (normal range: < 4 mg/L); alanine aminotransferase, 50 IU/L (normal range: 7-40 IU/L); aspartate aminotransferase, 45 IU/L (normal range: 13-35 IU/L); CA125, 62.8 U/mL (normal range: ≤ 25 ng/mL) (Table 1). Real-time polymerase linked reaction (RT-PCR) indicated positive nucleic acid of novel coronavirus, and pus culture revealed Candida albicans, which was sensitive to fluconazole.
| Date | White blood cell count, × 109/L | Neutrophil percentage, % | Hemoglobin, g/L | Platelet count, × 109/L | hs-CRP, mg/L | PCT, ng/mL | ALT, IU/L | AST, IU/L | GGT, IU/L |
| 2022.12.14 | 6.35 | 66.9 | 123 | 410 | 4.62 | 0.13 | 50 | 45 | 35 |
| 2022.12.17 | 16.97 | 96.5 | 138 | 235 | 73.08 | 3.10 | 96 | 80 | 68 |
| 2022.12.19 | 8.22 | 93.2 | 112 | 122 | 169.78 | - | - | - | - |
| 2022.12.22 | 1.24 | 72.0 | 95 | 49 | 76.13 | 0.89 | 24 | 27 | 60 |
| 2022.12.28 | 18.81 | 88.8 | 98 | 212 | 74.18 | 0.19 | 35 | 47 | 41 |
| 2023.01.14 | 8.85 | 68.4 | 126 | 323 | 32.94 | 0.46 | 258 | 316 | 167 |
| 2023.01.20 | 3.86 | 56.2 | 110 | 224 | - | - | 47 | 39 | 78 |
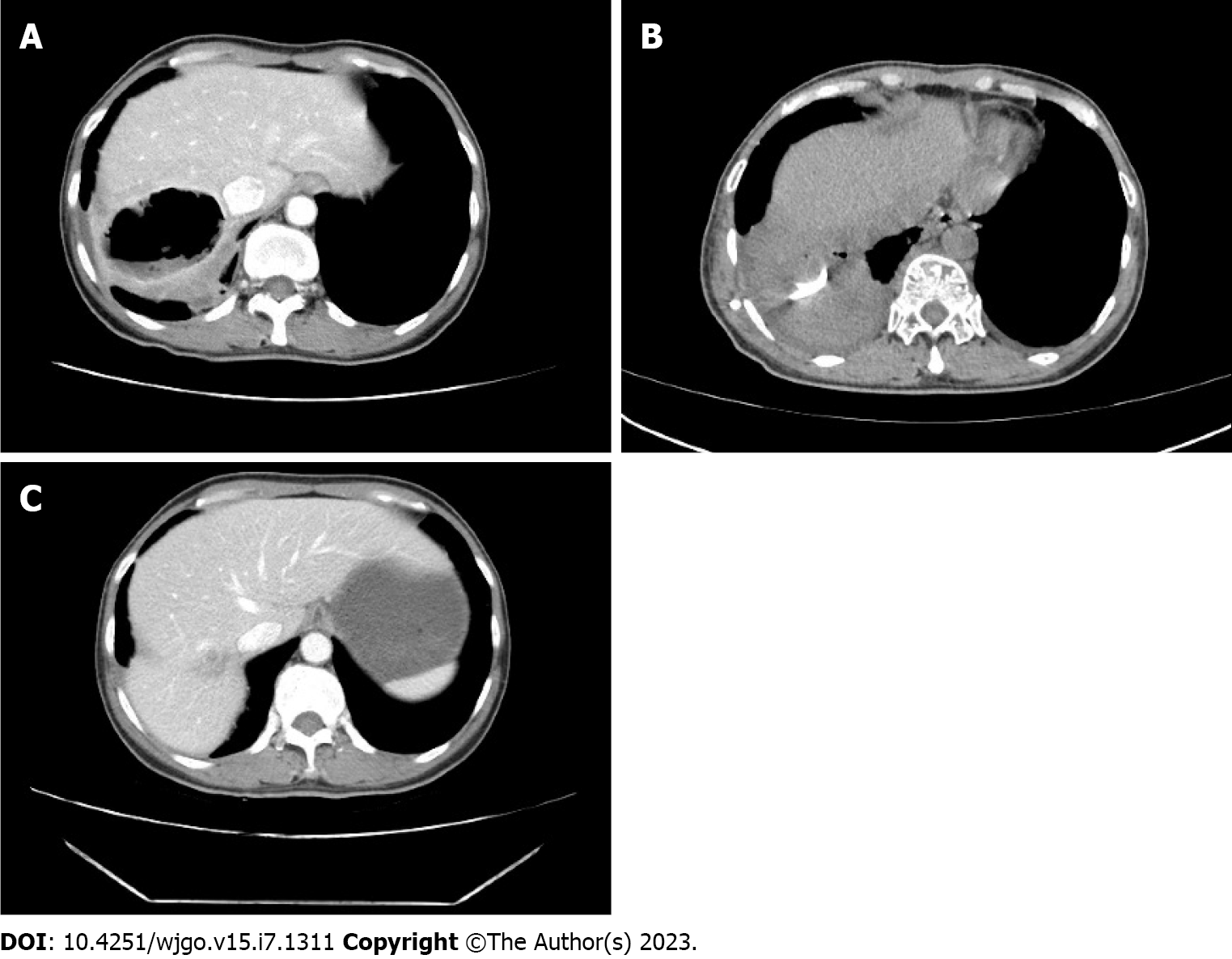
Chest CT examination indicated viral pneumonia, and contrast-enhanced abdominal CT revealed a liver abscess with a maximum cross-section of 6.9 cm × 6.0 cm, accompanied by fluid and gas (Figure 1A).
The patient was diagnosed as Candida albicans liver abscess, COVID-19, and Stage IV pancreatic head cancer.
The patient was admitted to the hospital on December 14, 2022, for chemotherapy with fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) regimen. On December 17, 2022, the patient developed a fever with a body temperature as high as 39.6 °C. Blood tests showed an increased white blood cell count, neutrophil percentage, C-reactive protein (CRP) and procalcitonin (PCT). Liver function indicated that the aminotransferase value was doubled (Table 1). Chest CT showed no abnormalities. Acute bronchitis was considered in combination with the patient’s cough. Given that the patient was a chemotherapy patient with advanced malignant tumor complicated with diabetes mellitus and a weakened immune system, she was given cefoperazone sulbactam sodium (3 g i.v. q12h), continued liver protection, immune enhancement, nutritional support, and other treatments. After 3 d of antibiotic use, the patient’s temperature still peaked at 39.6 °C, and her RT-PCR indicated COVID-19, while chest CT examination indicated viral pneumonia. She was treated with azvudine tablets (5 mg po qd). In addition, the patient experienced vomiting, poor appetite, and right upper abdominal pain. Contrast-enhanced abdominal CT showed a liver abscess with a maximum cross-section of 6.9 cm × 6.0 cm, accompanied by fluid and gas (Figure 1A). On January 20, 2022, the patient underwent CT-guided percutaneous catheter drainage for hepatic abscess. The pus was brown and turbid with flocculent substance and it was sent for microbial culture. The antibiotic was upgraded to Meropenem (1 g i.v. q8h). On December 22, 2022, the patient’s blood routine showed a very low white blood cell count of 1.24 × 109/L, a platelet count of 49 × 109/L, and CRP and PCT were still significantly elevated, while liver function was basically normal (Table 1). To improve both the white blood cell and platelet counts, the patient was injected with recombinant human granulocyte stimulating factor plus recombinant human thrombopoietin. On December 25, 2022, pus culture revealed Candida albicans, which was sensitive to fluconazole. Then the patient was treated with fluconazole injection (0.4 g i.v. qd, double the first dose). With the use of fluconazole, the patient’s symptoms and signs gradually improved. On December 29, 2022, contrast-enhanced abdominal CT showed no gas or fluid in the abscess space (Figure 1B). The patient had no pus coming out of the drain, and the drain was removed. On January 14, 2023, the patient’s laboratory results showed normal blood routine, slightly elevated CRP and PCT, and significantly elevated aminotransferase (Table 1). The significant elevated aminotransferases were considered a side effect of fluconazole, but fluconazole had to be continued, so liver protection therapy was strengthened. On January 20, 2023, the patient had no discomfort such as fever or abdominal pain, and her routine blood, CRP, PCT, and liver function were basically normal (Table 1). At this time, the patient received intravenous fluconazole for 4 wk and continued to take oral fluconazole (0.45 g po qd) and hepatoprotective drugs for 1 wk after discharge. In total, the antifungal course lasted for 5 wk.
The patient recovered well and received 4 cycles of FOLFOXIRI chemotherapy after 2 mo of antifungal therapy. The patient’s routine blood, liver function, kidney function, and coagulation were normal, tumor markers decreased, and contrast-enhanced abdominal CT did not indicate liver tissue absence, cavity, or gas any longer (Figure 1C).
The pancreas is made up of acinar cells that secrete digestive enzymes, ductal cells that secrete bicarbonate, central acinar cells that act as a transition zone between acinar and ductal cells, endocrine islets that secrete hormones, and relatively inactive stellate cells. Cancer occurs when abnormal DNA mutations in the pancreas cause pancreatic cells to grow and divide uncontrollably[1]. Risk factors for early hepatic metastasis of pancreatic cancer include age over 70 years, lymph node metastasis, adenocarcinoma or neuroendocrine carcinoma, large tumor size, poor differentiation, no surgery, no chemotherapy. Pancreatic cancer is one of the most aggressive and fatal malignancies[2].
The treatment of hepatic metastasis of pancreatic cancer includes chemotherapy, radiotherapy, and surgery. Ablation is one of the most effective and minimally invasive techniques for the treatment of liver tumors, with a low complication rate. Compared with chemotherapy alone, ablation combined with chemotherapy can further prolong the survival period of patients. However, in some rare cases, complications such as liver abscess, bronchobiliary fistula, hollow visceral perforation, diaphragmatic perforation, and hernia may occur[3,4]. The clinical symptoms of hepatic abscess are nons
Fungal liver abscess cases are rare, especially for patients with pancreatic head cancer, diabetes, bone marrow transplantation after chemotherapy, or COVID-19. There are no guidelines or expert consensus on the course of antifungal therapy to guide clinical treatment. For patients with Candida albicans, liver abscess complicated with various underlying diseases such as malignant tumor and diabetes, continuous antifungal therapy for 5 wk is effective. In the early stage, the efficacy can be judged according to the patient having no fever, abdominal pain has disappeared and leukocyte, CRP, PCT has decreased. It can also be combined with ultrasound, CT, or MRI to judge the treatment effect. However, the use of antifungal drugs for a long course should make the physician wary of liver function damage and other side effects while liver function and kidney function should be monitored.
The incidence of liver abscess after liver intervention is very high in patients who have undergone Whipple surgery. Effective treatment of Candida albicans liver abscess requires early detection, percutaneous catheter drainage, and antifungal therapy for 5 wk. Meanwhile, complications such as COVID-19 should be actively dealt with, and nutritional support should be provided.
Grammar consulting and writing assistance were kindly provided by Ying Liu and Tao Qin.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sudhamshu KC, Nepal; Meena DS, India S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Hu JX, Zhao CF, Chen WB, Liu QC, Li QW, Lin YY, Gao F. Pancreatic cancer: A review of epidemiology, trend, and risk factors. World J Gastroenterol. 2021;27:4298-4321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 349] [Cited by in RCA: 314] [Article Influence: 78.5] [Reference Citation Analysis (16)] |
| 2. | Cao BY, Tong F, Zhang LT, Kang YX, Wu CC, Wang QQ, Yang W, Wang J. Risk factors, prognostic predictors, and nomograms for pancreatic cancer patients with initially diagnosed synchronous liver metastasis. World J Gastrointest Oncol. 2023;15:128-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Yan X, Ning ZY, Wang P, Zhuang LP, Xu LT, Zhu ZF, Sheng J, Shen YH, Hua YQ, Meng ZQ. Combined ablation-chemotherapy versus chemotherapy alone for pancreatic cancer with liver metastasis: a propensity score matching study. Expert Rev Gastroenterol Hepatol. 2021;15:1047-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Dai H, Cui D, Li D, Zhai BO, Zhang J. Hepatic abscess with hepatobronchial fistula following percutaneous radiofrequency ablation for hepatocellular carcinoma: A case report. Oncol Lett. 2015;9:2289-2292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Lardière-Deguelte S, Ragot E, Amroun K, Piardi T, Dokmak S, Bruno O, Appere F, Sibert A, Hoeffel C, Sommacale D, Kianmanesh R. Hepatic abscess: Diagnosis and management. J Visc Surg. 2015;152:231-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 168] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 6. | Oh JG, Choi SY, Lee MH, Lee JE, Yi BH, Kim SS, Min JH, Lee B. Differentiation of hepatic abscess from metastasis on contrast-enhanced dynamic computed tomography in patients with a history of extrahepatic malignancy: emphasis on dynamic change of arterial rim enhancement. Abdom Radiol (NY). 2019;44:529-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Lee CM, Kang BK, Kim M. Differentiation of Small Hepatic Abscess From Hepatic Metastasis With a Combination of Imaging Parameters. J Comput Assist Tomogr. 2022;46:514-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Mavilia MG, Molina M, Wu GY. The Evolving Nature of Hepatic Abscess: A Review. J Clin Transl Hepatol. 2016;4:158-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Thomas KT, Bream PR Jr, Berlin J, Meranze SG, Wright JK, Chari RS. Use of percutaneous drainage to treat hepatic abscess after radiofrequency ablation of metastatic pancreatic adenocarcinoma. Am Surg. 2004;70:496-499. [PubMed] |
| 10. | Elliott R, Ohene Baah N, Grossman VA, Sharma AK. COVID-19 Related Mortality During Management of a Hepatic Abscess. J Radiol Nurs. 2020;39:271-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Deif MA, Mounir AM, Abo-Hedibah SA, Abdel Khalek AM, Elmokadem AH. Outcome of percutaneous drainage for septic complications coexisted with COVID-19. World J Radiol. 2022;14:91-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Shenoy S. Coronavirus (Covid-19) sepsis: revisiting mitochondrial dysfunction in pathogenesis, aging, inflammation, and mortality. Inflamm Res. 2020;69:1077-1085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 119] [Article Influence: 23.8] [Reference Citation Analysis (0)] |