Published online Sep 15, 2022. doi: 10.4251/wjgo.v14.i9.1739
Peer-review started: December 2, 2021
First decision: March 11, 2022
Revised: April 24, 2022
Accepted: July 26, 2022
Article in press: July 26, 2022
Published online: September 15, 2022
Processing time: 281 Days and 11.6 Hours
Primary malignant melanoma of the esophagus (PMME) is a rare malignant disease and has not been well characterized in terms of clinicopathology and survival.
To investigate the clinical features and survival factors in Chinese patients with PMME.
The clinicopathological findings of ten cases with PMME treated at Henan Provincial People’s Hospital were summarized. Moreover, the English- and Chinese-language literature that focused on Chinese patients with PMME from 1980 to September 2021 was reviewed and analyzed. Univariate and multivariate analyses were employed to investigate the clinicopathologic factors that might be associated with survival.
A total of 290 Chinese patients with PMME, including ten from our hospital and 280 from the literature were enrolled in the present study. Only about half of the patients (55.8%) were accurately diagnosed before surgery. Additionally, 91.1% of the patients received esophagectomy, and 88 patients (36.5%) received adjuvant therapy after surgery. The frequency of lymph node metastasis (LNM) was 51.2% (107/209), and LNM had a positive rate of 45.3% even when the tumor was confined to the submucosal layer. The risk of LNM increased significantly with the pT stage [P < 0.001, odds ratio (OR): 2.47, 95% confidence interval (CI): 1.72-3.56] and larger tumor size (P = 0.006, OR: 1.21, 95%CI: 1.05-1.38). The median overall survival (OS) was 11.0 mo (range: 1-204 mo). The multivariate Cox analysis showed both the pT stage [P = 0.005, hazard ratio (HR): 1.70, 95%CI: 1.17-2.47] and LNM (P = 0.009, HR: 1.78, 95%CI: 1.15-2.74) were independent prognostic factors for OS. The median disease-free survival (DFS) was 5.3 mo (range: 0.8-114.1 mo). The multivariate analysis indicated that only the advanced pT stage (P = 0.02, HR: 1.93, 95%CI: 1.09-3.42) was a significant independent indicator of poor RFS in patients with PMME.
The correct diagnosis of PMME before surgery is low, and physicians should pay more attention to avoid a misdiagnosis or missed diagnosis. Extended lymph node dissection should be emphasized in surgery for PMME even though the tumor is confined to the submucosal layer. Both the LNM and pT stage are independent prognosis factors for OS, and the pT stage is the prognosis factor for DFS in patients with PMME.
Core Tip: Primary malignant melanoma of esophagus (PMME) is a rare malignant disease. We comprehensively analyzed the clinicopathological characteristics of 290 Chinese patients with PMME. Only about half of the patients were accurately diagnosed before surgery. The positive rate of lymph node metastasis (LNM) was 45.3% even the tumor confined to the submucosal layer. The median overall survival (OS) and disease-free survival were 11.0 mo and 5.3 mo, respectively. Cox analysis showed that both pT stage and LNM were the independent prognostic factors for OS, while only advanced pTNM stage was a significant independent indicator of poor RFS in patients with PMME.
- Citation: Zhou SL, Zhang LQ, Zhao XK, Wu Y, Liu QY, Li B, Wang JJ, Zhao RJ, Wang XJ, Chen Y, Wang LD, Kong LF. Clinicopathological characterization of ten patients with primary malignant melanoma of the esophagus and literature review. World J Gastrointest Oncol 2022; 14(9): 1739-1757
- URL: https://www.wjgnet.com/1948-5204/full/v14/i9/1739.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i9.1739
Primary malignant melanoma of the esophagus (PMME) is the most common non-epithelial malignancy in the esophagus[1], which comprises approximately 0.2% of all tumors of the esophagus[2]. Until now, only several hundred cases of PMME have been reported in the literature, most as case reports[3]. The limited sample size restricted research on the malignancy. Reports on Chinese PMME are limited, although some areas of China have a high incidence of esophageal cancer. Large studies on Chinese PMME were reported by Wang et al[4] (n = 76), Dai et al[5] (n = 70), Sun et al[6] (n = 21), and Chen et al[7] (n = 20). PMME has the following characteristics: Difficult to diagnosis, rapid progression, high rate of recurrence and metastasis, and poor prognosis. The median survival of PMME in China is 13.5 mo[5]. To date, the diagnosis, treatment, and pathological staging of PMME follow the guidelines for esophageal cancer[5]. Systematically analyzing the clinicopathologic features and the possible prognostic factors of PMME will improve the effectiveness of its diagnosis and treatment.
In this retrospective study, we presented ten cases of PMME encountered at Henan Provincial People’s Hospital, together with a systematic analysis of 280 Chinese patients with PMME collected from both the English- and Chinese-language literature, with the aim of analyzing the clinicopathological and prognostic characteristics of Chinese patients with PMME.
The records of 12 patients with PMME were retrieved at Henan Provincial People’s Hospital from January 1990 to September 2021. Two patients were excluded because of a history of cutaneous melanoma. The clinical data of the remaining ten patients, including gender, age, symptoms, endoscopic and radiographic examination, tumor location, tumor size, operative time, tumor node metastasis (TNM) stage, and others were collected. All of the ten patients were confirmed by endoscopic biopsy and four of them received surgical treatment. None of them had a history of melanoma in the skin or other malignancy history.
The tumor diagnostic evaluation was reviewed and confirmed by two independent pathologists. In order to be consistent with the published literature, the clinical and pathological stages were reassessed according to the 7th edition of the Union for International Cancer Control (UICC) TNM classification system. Follow-ups were performed by telephone and the outpatient medical record system, and the complete follow-up data should include survival status, cause of death, and time of death.
The present study was approved by the Institutional Review Board of Henan Provincial People’s Hospital, and it conformed to the provisions of the Declaration of Helsinki. Written informed consent was obtained from all individuals before biopsy or surgery.
A systematic literature review was performed in databases of China BioMedical Literature on Disc (CBMdisc), and Medical Literature Analysis and Retrieval System online (MEDLINE). Relevant publications were identified using the following terms and keywords: “Malignant melanoma of the esophagus” or “Malignant melanoma” and “Esophagus”. The last search was updated on September 1, 2021. References of the retrieved articles were further reviewed to find other potential eligible studies. The title and abstract were first screened, followed by full text assessing for eligibility. Each step was independently conducted by two researchers, results were compared, and differences were resolved by consensus.
To be eligible for inclusion in this meta-analysis, the article must meet the following criteria: (1) Describing studies on PMME in Chinese population; (2) Providing detailed information of each patients, including gender and age; and (3) Providing pathology diagnosis. Articles were excluded due to the following reasons: (1) Studies were not focused on Chinese population; (2) Meta-analysis or reviews; (3) There was no detailed information of each patients; (4) Content repeats in different articles; and (5) Accompanied with other malignancies, including melanoma in other body parts simultaneously or heterogeneously.
Data from retrieved articles were independently collected by two reviewers. The following information was extracted from each study: First author, year of publication, and detailed information of each patients. In event of inconsistent evaluations, a third investigator was consulted to resolve the dispute and made the final decision.
Descriptive or frequency analysis was used for basic information analysis. Numerical variables are expressed as the mean ± SD. Statistical differences were evaluated by χ2 test or t test. The effects of the clinicopathologic factors on lymph node metastasis (LNM) was evaluated using univariate and multivariate logistic-regression models. The Kaplan- Meier method was used to assess associations between clinicopathological characteristics and survival outcome. Univariate and multivariate analyses were performed using Cox regression. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. The log-rank test was used to compare survival curves. All statistical tests were two-sided. P values less than 0.05 were considered statistically significant. All statistical analyses were conducted using SPSS 21 (IBM Corporation, Waltham, NY, United States).
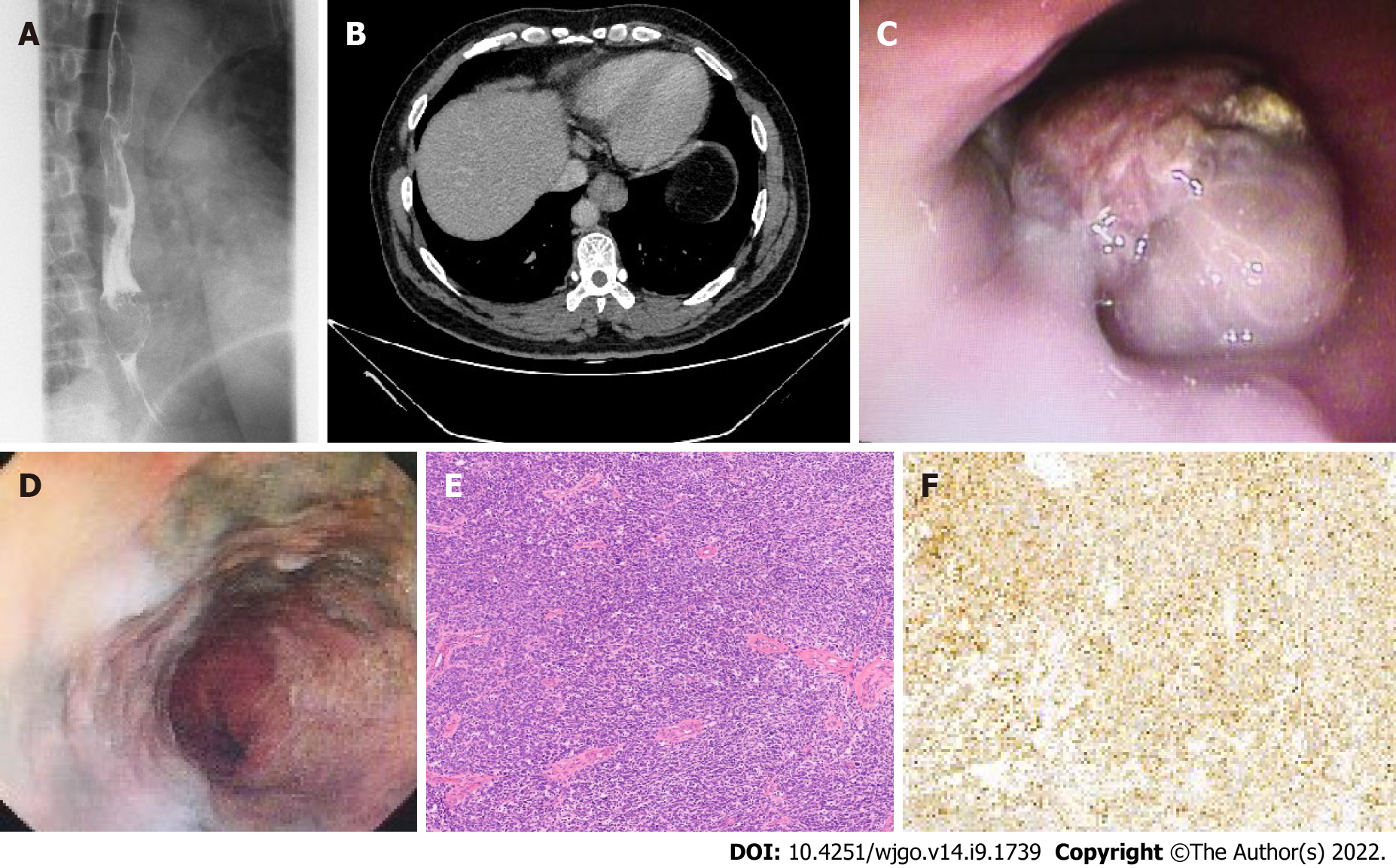
The clinicopathological characteristics of ten PMME patients are summarized in Table 1. There were six men and four women. The ages ranged from 47 years to 80 years with a mean age of 62.2 ± 9.9 years. Although the mean age of female patients (68.3 ± 10.4 years) was much older than that of the male patients (58.0 ± 7.8 years), there was no statistical difference (P = 0.111). Eight of them presented with dysphagia as the main symptom (80%, 8/10), and the other two had retrosternal pain or bellyache. Six of them also had an esophagography and computerized tomography (CT) scan. The esophagography revealed mucosa destruction and an irregular filling defect of the esophageal lumen (Figure 1A). The CT scan showed polypoid masses in the esophagus (Figure 1B). There were one, six, and three patients having the masses located at the upper, middle, and lower portion of the esophagus, respectively.
| Case No. | Gender | Age (yr) | Chief complaint | Location | Gross classification | Tumor number | Preoperative diagnosis | Tumor length | Deep in depth | LNM | Treatment | Survival (mo) |
| 1 | Male | 61 | Dysphagia | Middle | NA | 1 | PMME | NA | NA | NA | NA | FU loss |
| 2 | Female | 59 | Dysphagia | Middle | NA | 1 | PMME | NA | NA | NA | NA | FU loss |
| 3 | Male | 47 | Dysphagia | Lower | NA | 1 | PMME | NA | NA | NA | NA | FU loss |
| 4 | Female | 60 | Dysphagia | Lower | NA | 1 | PMME | NA | NA | NA | NA | FU loss |
| 5 | Female | 80 | Dysphagia | Middle | NA | 1 | PMME | NA | NA | NA | R + C | 31 |
| 6 | Male | 69 | Dysphagia | Middle | NA | 1 | PMME | NA | NA | NA | C | 51 |
| 7 | Male | 57 | Dysphagia | Upper | Ulcering | 1 | Poor differentiated carcinoma | 5 | DP | No | S | 18 |
| 8 | Female | 74 | Retrosternal pain | Lower | Polypoid | 2 | PMME | 5 | SM | No | S | FU loss |
| 9 | Male | 62 | bellyache | Middle | Polypoid | 1 | PMME | 2.5 | DP | No | S | 3 |
| 10 | Male | 52 | Dysphagia and retrosternal pain | Middle | Polypoid | 1 | PMME | 4 | SM | No | S | 22 alive |
All of the ten patients had a preoperative esophagoscopy and biopsy pathology. The endoscopy manifestations were polypoid or a protuberant mass (n = 7), ulcerative mass (n = 1), and superficial lesion (n = 2). About half of the patients had pigment deposition on the surface of the tumors (Figure 1C and D). Nine patients had an accurate preoperative diagnosis of PMME, but the remaining one who was initially diagnosed with poor differentiated carcinoma by biopsy pathology, was eventually diagnosed with PMME by postoperative pathology (Figure 1E and F). There were four patients who received surgery and two who received chemoradiotherapy only. A postoperative pathological examination of the four patients showed that the lesions of two cases were confined to the submucous layer (T1b), and two had lesions extended to the muscularis propria (T2). The mean number of lymph nodes dissected in surgery was 14.5 ± 6.1 (range: 6-19). Notably, none of the four patients had LNM.
Five of the six patients who received treatments at our hospital were successfully followed up. One was still alive until the last follow up, but the remaining four died because of recurrence or metastasis. The median survival time was 24.5 mo (range: 3-31.9 mo).
The literature flowchart (Supplementary Figure 1) exhibits the entire selection process from the eligible studies. The search can be traced using the publication date from 1980 to September 2021. A total of 122 studies were collected using the inclusion and exclusion criteria, including 98 articles in Chinese and 24 in English. Finally, a total of 280 patients diagnosed with PMME were enrolled in the study. The main characteristics of the included studies[4,6-126] as well as the corresponding clinicopathological features are summarized in the Supplementary Table 1. Finally, a total of 290 patients, including the ten cases recruited from our hospital and the 280 cases collected from the literature, were subjected to subsequent analysis. The clinicopathological characteristics are shown in Table 2.
| Characteristic | n | % |
| Gender | ||
| Male | 200 | 69.0 |
| Female | 90 | 31.0 |
| Age | 58.4 ± 9.7 yr | |
| Symptoms | ||
| Dysphagia | 219 | 79.1 |
| Restrosternal pain | 13 | 4.7 |
| Dysphagia and restrosternal pain | 18 | 6.5 |
| Bellyache | 11 | 4.0 |
| No symptom found by physical examination | 8 | 2.9 |
| Loss of appetite | 6 | 2.2 |
| Hoematemesis or melena | 2 | 0.7 |
| Censored | 13 | |
| Location | ||
| Upper | 16 | 5.4 |
| Middle | 137 | 47.3 |
| Lower | 137 | 47.3 |
| Pigmentation | ||
| Yes | 141 | 71.9 |
| No | 55 | 28.1 |
| Censored | 94 | |
| Pathological diagnosis of biopsy | ||
| PMME | 115 | 55.8 |
| ESCC | 32 | 15.5 |
| Poorly differentiated carcinoma | 39 | 18.9 |
| Esophageal adenocarcinoma | 10 | 4.9 |
| High-grade dysplasia or non-neoplastic lesions | 10 | 4.9 |
| Censored | 84 | |
| Treatment | ||
| Surgery | 153 | 58.8 |
| Surgery and adjuvant treatment | 88 | 35.1 |
| Adjuvant treatment | 16 | 6.1 |
| Censored | 33 | |
| Tumor size (censored: n = 77) | 5.2 ± 2.9 cm | |
| Tumor number | ||
| Single | 74 | 61.7 |
| Multiple | 46 | 38.3 |
| Censored | 170 | |
| Gross classification | ||
| Superficial elevated | 14 | 5.7 |
| Polypoid | 194 | 77.9 |
| Ulcerative and others | 36 | 14.4 |
| Censored | 46 | |
| Depth of invasion | ||
| T1 | 97 | 45.6 |
| T2 | 67 | 31.4 |
| T3 and T4 | 49 | 23.0 |
| Censored | 77 | |
| Lymph node metastasis | ||
| Yes | 107 | 51.2 |
| No | 102 | 48.8 |
| Censored | 81 | |
Each case of the 290 cases had gender, age, tumor location, and pathology documents. There were 200 males and 90 females with a male-to-female ratio of 2.2:1. Their ages ranged from 26 to 84 years, with a mean age of 58.5 ± 9.7 years. No significant difference was found in age between male and female patients (male: 58.6 ± 9.1 years; female: 58.3 ± 11.1 years).
Most of the tumors (274/290, 94.6%) were located in the middle (n = 138) or lower (n = 136) of the esophagus, and only 16 cases (5.4%) had the tumors located in the upper esophagus. Interestingly, the tumors in female patients were prone to being located in the upper esophagus (62.5%, 10/16), and conversely, tumors in male patients were more often located in the both middle and lower esophagus (72.3%, 198/274, P = 0.003).
There were 277 patients who had their main symptoms documented. The most common symptom was dysphagia (219, 79.1%), followed by retrosternal pain (31, 11.2%), bellyache (11, 4.0%), poor food intake with no obvious incentive (6, 2.2%), and hematemesis or melena (2, 0.7%), respectively. Eight (2.9%) patients were asymptomatic and had the tumors detected in the physical examination. The interval between the diagnosis of the disease and the onset of symptom occurrence was documented in 188 patients. The symptom duration ranged from 0.2-36 mo, with a median of 2.0 mo.
Notably, there were 147 patients who had detailed information of upper gastrointestinal barium esophagogram and CT. For most of them, the esophagography revealed mucosa destruction, irregular filling defect, and narrowness of the esophageal lumen. The CT examination mainly showed bulky or polypoid and intraluminal obstructive masses in the esophagus.
About 181 patients had preoperative endoscopy documents. The most common manifestation of the endoscopy was an irregular segmented, lobular, polypoid, or segmented intraluminal tumor mass. Half of the tumors had a rough, eroded, and friable and easily bleeding surface (87/181, 48.1%). Six patients failed to have the mucosa biopsy taken because it bled readily.
The detailed pathological results of the preoperative biopsy were described in 206 patients. Only 115 (55.8%) of the 206 patients were accurately diagnosed as having PMME. Biopsy pathology of the remaining cases were as follows: Poorly differentiated carcinoma (39/206, 18.9%), squamous cell carcinoma (15.5%, 32/206), adenocarcinoma (4.9%, 10/206), and high-grade dysplasia or nonneoplastic lesions (4.9%, 10/206).
Treatment was documented in 257 of the 290 patients (88.6%). The majority of the cases (234/257, 91.1%) accepted esophagogastrostomy or subtotal esophagectomy, and seven (2.7%) patients accepted endoscopic submucosal dissection (ESD). Besides surgery or ESD, 88 (88/241, 36.5%) patients also received adjuvant therapy, including radiotherapy, chemotherapy, and immunotherapy. There were 16 (6.2%) cases that only received adjuvant therapy without surgery.
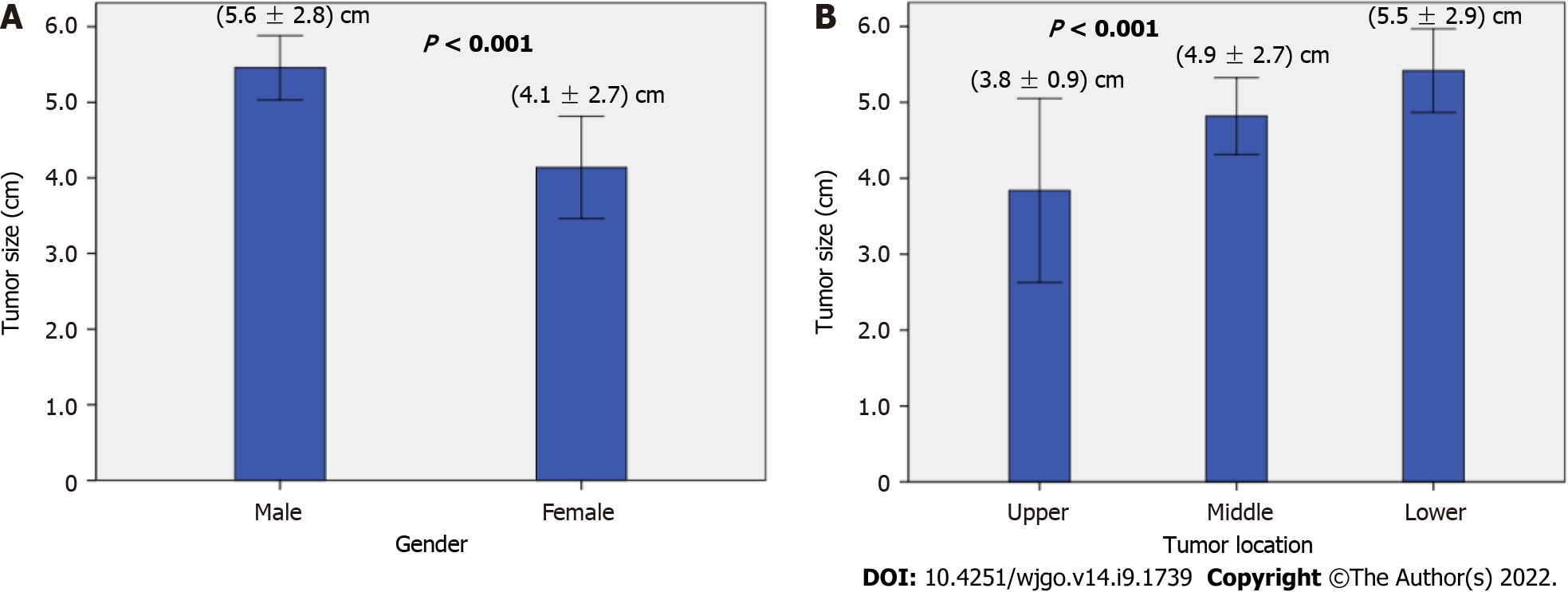
Multiple tumors were defined as there was at least one satellite nodule or it was scattered with a black pigmented spot near the primary tumor. The tumor size of multiple tumors was calculated as the size of the primary tumor instead of the sum of multiple tumors. There were 71.9% of PMME masses that had a pigmented surface. Seventy-four (61.8%) cases had single tumors, and 46 (38.2%) had multiple tumors. The mean size was 5.2 ± 2.9 cm (range: 0.3-17.0 cm). The mean tumor size in males was significantly longer than that in female patients (P < 0.001, Figure 2A). Additionally, the tumor size was significantly correlated with tumor location (P < 0.001), and the mean tumor size was much shorter when the tumor was located in the upper thoracic esophagus (Figure 2B). No difference was found in tumor size between single and multiple tumors (single: 5.2 ± 2.8 cm; multiple: 5.3 ± 3.1 cm; P = 0.895).
There were 244 patients who had gross classification documents. The most common subtype was polypoid (194/244, 79.5%), followed by ulcerative (n = 29, 11.9%), superficial (n = 14, 5.7%), medullary (n = 6, 2.5%), and constrictive subtypes (n = 1, 0.4%).
There were 213 patients who had depth of tumor invasion documents. Pathological examination revealed that the tumors in 45.6% of the PMME patients were limited to submucosal layer, including 14 (6.6%) cases restricted to the mucosa (T1a) and 83 (39.0%) restricted to the submucosal layer (T1b). The number of patients with tumor extension to the muscularis propria (T2), fibrous membrane (T3), and outer membrane (T4) was 67 (31.4%), 40 (18.8%), and 9 (4.2%), respectively. No correlation was found between the tumor infiltration depth and clinical characteristics (P > 0.05; data not shown).
Totally, 209 patients had LNM documents. The mean number of lymph nodes dissected in surgery was 11.7 ± 8.9 (range: 1 to 43). The positive rate of LNM was 51.2% (102/209). The correlation between LNM and clinicopathological features is shown in Table 3. Significantly, no LNM was found when the tumor was confined to the mucous layer (T1a). The risk of LNM was significantly increased with the progression of the pT stage [P < 0.001, odds ratio (OR): 2.47, 95%CI: 1.72-3.56]. The size for the tumors with LNM was significantly larger than that of tumors without (P < 0.001, OR: 1.24, 95%CI: 1.09-1.42). A regression analysis found that the risk of LNM was associated with both the pT stage and tumor size (pT stage: P < 0.001, OR: 2.22, 95%CI: 1.47-3.33; tumor size: P = 0.006, OR: 1.21, 95%CI: 1.05-1.38).
| Feature | LNM- | LNM+ | P valve | Logistic regression analysis | |||
| n | % | n | % | P valve | OR (95%CI) | ||
| Gender | |||||||
| Male | 77 | 51.0 | 74 | 49.0 | 0.307 | ||
| Female | 25 | 43.1 | 33 | 56.9 | |||
| Age (yr) | 59.4 ± 8.9 | 57.2 ± 10.3 | 0.109 | ||||
| Location | |||||||
| Upper | 3 | 75.0 | 1 | 25.0 | 0.202 | ||
| Middle | 52 | 53.6 | 45 | 46.4 | |||
| Lower | 47 | 43.5 | 61 | 56.5 | |||
| Tumor size (cm) | 4.6 ± 2.4 | 6.0 ± 3.0 | < 0.001 | 0.006 | 1.21 (1.05-1.38) | ||
| Tumor number | |||||||
| Single | 23 | 41.1 | 33 | 58.9 | 0.919 | ||
| Multiple | 14 | 40.0 | 21 | 60.0 | |||
| Censored | 67 | 54.5 | 56 | 46.5 | |||
| Gross classification | |||||||
| Superficial elevated | 11 | 91.7 | 1 | 8.3 | 0.01 | 0.261 | |
| Polypoid | 68 | 46.6 | 78 | 53.4 | |||
| Ulcerative and others | 14 | 45.2 | 17 | 54.8 | |||
| Censored | 9 | 45 | 11 | 55 | |||
| Infiltration depth | |||||||
| T1a | 14 | 100 | 0 | 0 | < 0.001 | < 0.001 | 2.22 (1.47-3.33) |
| T1b | 40 | 54.8 | 33 | 45.2 | |||
| T2 | 30 | 48.4 | 32 | 51.6 | |||
| T3 + T4 | 9 | 20.0 | 36 | 80.0 | |||
| Censored | 9 | 60 | 6 | 40 | |||
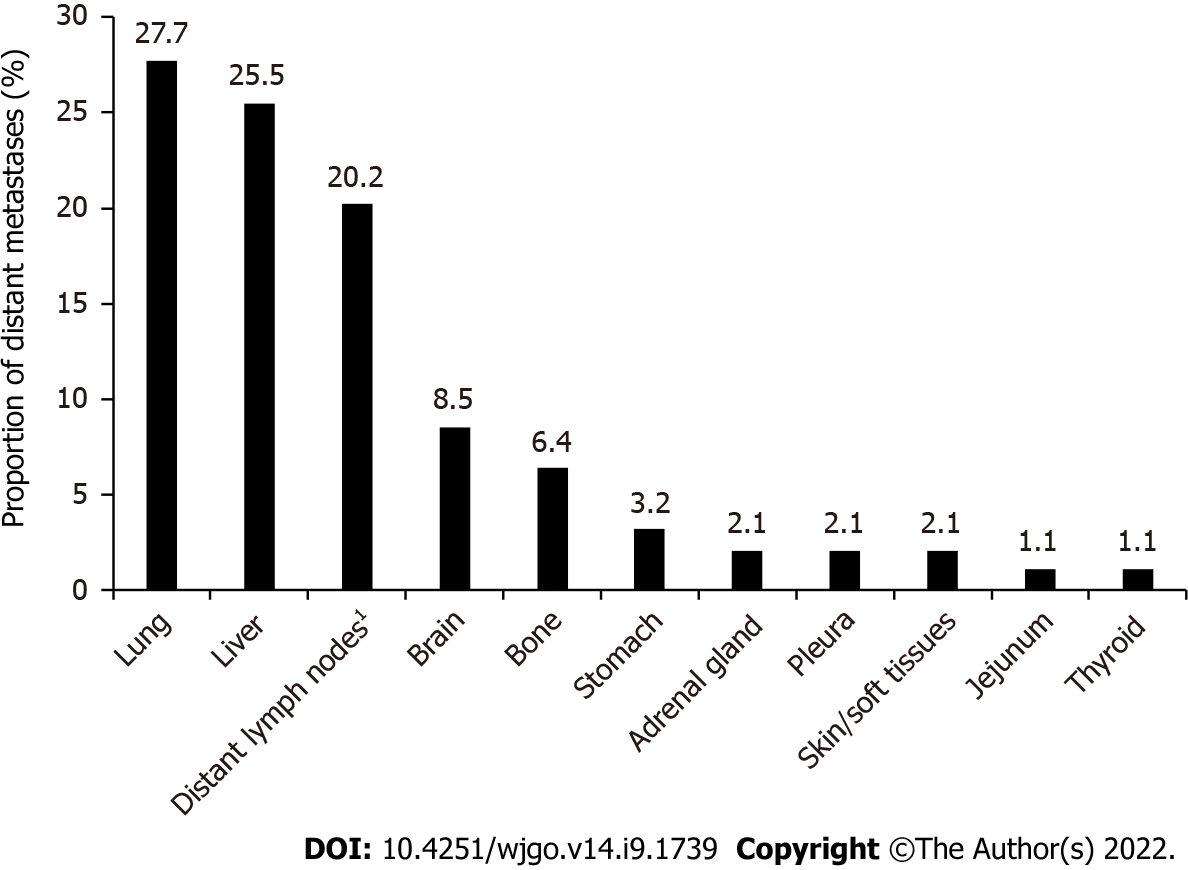
Eighty-four patients had records for local recurrence and distant metastasis, and 16 cases were combined with distant metastasis in addition to local recurrence. The precise sites of the distant metastasis were well documented in 74 cases. A total of 94 PMME metastatic sites were affected in the 74 patients; 19 cases had two sites involved, and 5 had three sites involved synchronously or metachronously. Both the lung (n = 26, 27.7%) and liver (n = 24, 25.5%) were the sites most frequently involved, followed by the lymph nodes (including those of the enterocoelia, neck, mediastinum, and axilla, n = 19, 20.2%), brain (n = 8, 8.5%), bone (n = 6, 6.4%), and other locations. The detailed distant metastasis locations are shown in Figure 3.
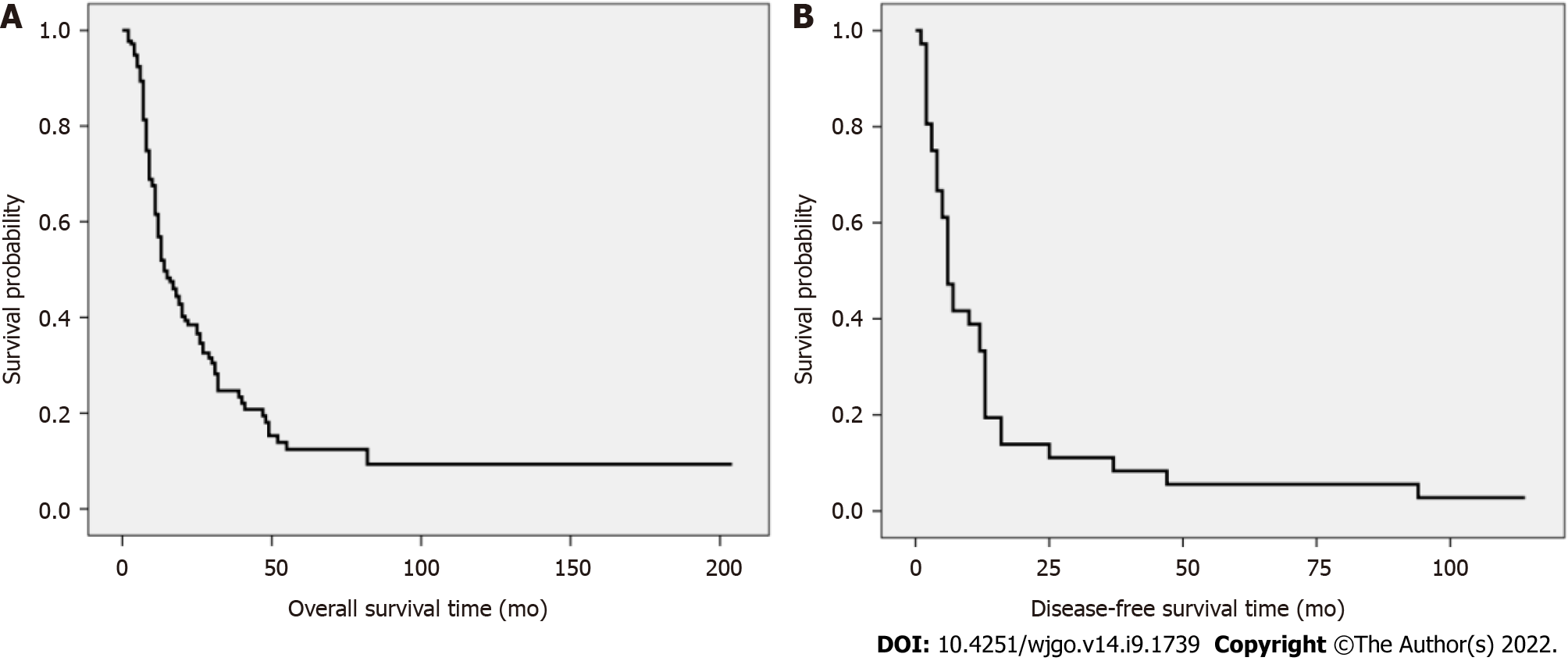
The follow-up data were documented in 179 patients. Three patients died of serious complications during the preoperative period. Two cases were lost after surgery at 12 and 33 mo, respectively. After excluding the five patients, the survival analysis was performed on the remaining 174 patients. There were 116 cases (65.9%) with cancer-specific deaths and 58 (32.9%) were still alive at the time that the articles were published. The median overall survival (OS) of 174 patients was 11.0 mo (range: 1-204 mo), and the 1-, 3-, and 5-year survival rates were 57%, 25%, and 12%, respectively (Figure 4A).
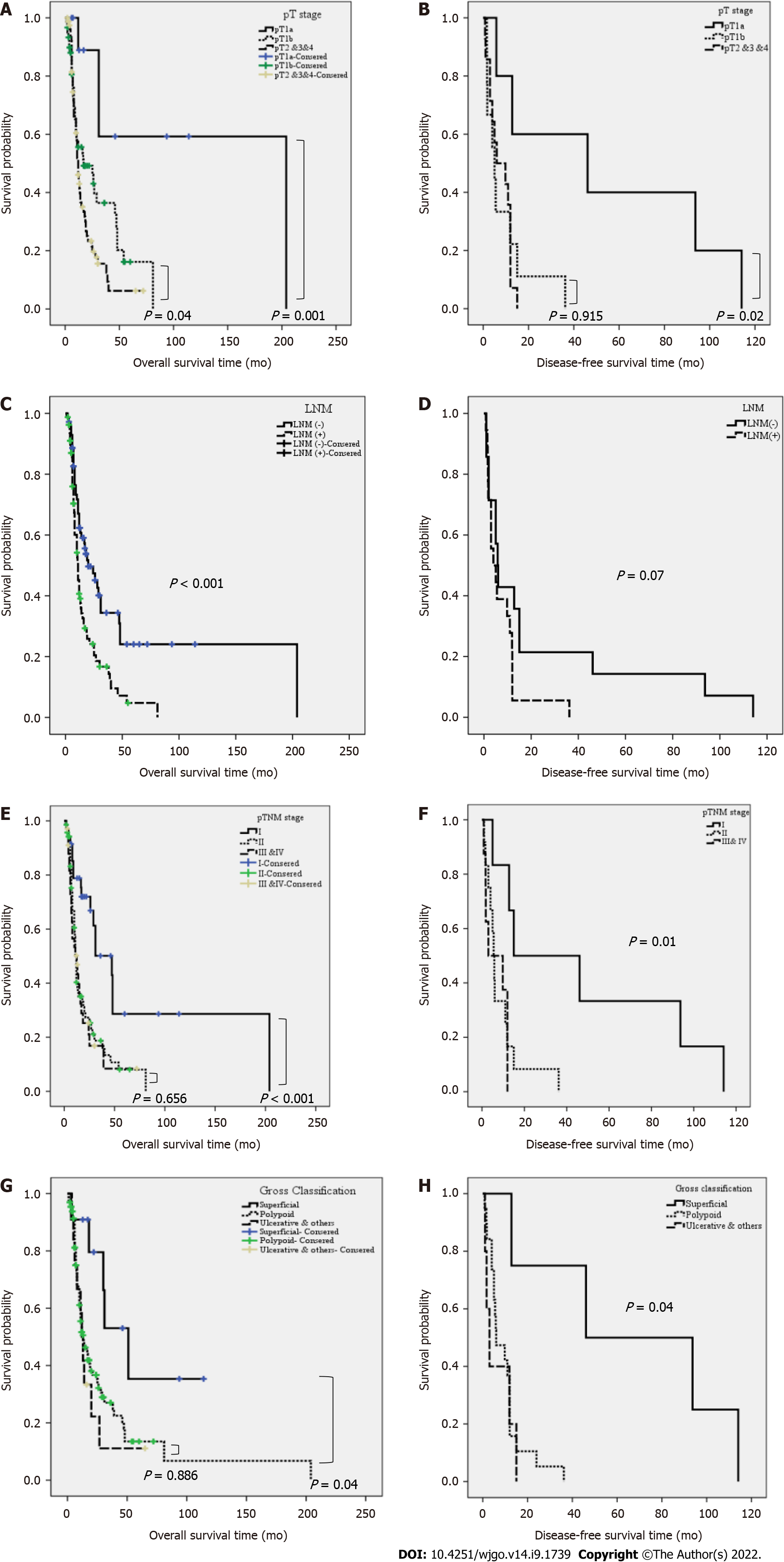
We compared the OS rate between the different clinicopathological characteristics of the PMME patients (Table 4). As shown in Figure 5A, patients at pT1b (n = 60) or advanced pT stages (n = 79) had a significantly worse prognosis than patients at T1a stage (n = 12, P = 0.01 and P = 0.001, respectively). Moreover, the prognosis of patients at the pT1b stage was much better compared with patients at advanced pT stage (P = 0.03, Figure 5A). In addition, the LNM-positive group had a significantly poorer prognosis compared with the LNM-negative group (P < 0.001, Figure 5C). As for the pathological tumor node metastasis (pTNM) stages, both the stage II and stage III/IV groups had a worse prognosis than the stage I group (P < 0.001, Figure 5E). Furthermore, patients with a superficial subtype had a significantly longer OS time than patients with other gross classifications (P = 0.02, Figure 5G). Male patients tended to have a worse prognosis compared with female patients (P = 0.08). A multivariate analysis demonstrated that both pT and LNM were independent prognostic factors for PMME patients (pT stage: P = 0.005, HR: 1.70, 95%CI: 1.17-2.47; LNM: P = 0.009, HR: 1.78, 95%CI: 1.15-2.74).
| Variable | Overall survival | Disease-free survival | ||||||
| Uni-P | Multi-P | HR | 95%CI | Uni-P | Multi-P | HR | 95%CI | |
| Gender | ||||||||
| Male vs female | 0.08 | 0.450 | ||||||
| Age (yr) | ||||||||
| < 55 vs ≥ 55 | 0.348 | 0.353 | ||||||
| Tumor location | ||||||||
| Upper vs middle vs lower | 0.647 | 0.385 | ||||||
| Tumor number | ||||||||
| Single vs multiple | 0.200 | 0.227 | ||||||
| Tumor size (cm) | ||||||||
| < 5.5 vs ≥ 5 | 0.282 | 0.124 | ||||||
| Gross classification | ||||||||
| Superficial vs polypoid vs ulcerative and others | 0.04 | 0.249 | 0.007 | 0.893 | ||||
| Depth of invasion | ||||||||
| T1a vs T1b vs T2 and T3 and T4 | 0.001 | 0.005 | 1.70 | 1.17-2.47 | 0.02 | 0.02 | 1.93 | 1.09-3.42 |
| LNM | ||||||||
| No vs yes | < 0.001 | 0.009 | 1.78 | 1.15-2.74 | 0.07 | |||
| pTNM stage | ||||||||
| I vs II vs III and IV | < 0.001 | 0.349 | 0.02 | 0.540 | ||||
| Treatment | ||||||||
| Surgery vs surgery plus adjuvant therapy | 0.433 | 0.02 | 0.698 | |||||
For disease-free survival (DFS), only 36 cases had detailed documents. The median DFS was 5.3 mo (range: 0.8-114.1 mo), and the 1-, 3-, and 5-year survival rates were 33%, 11%, and 6%, respectively (Figure 4B). Similar to the OS, the DFS of the patients at T1a was significantly better than that of patients at advanced pT stages (P = 0.01, Figure 5B). Patients at pTNM I had a better RFS compared with patients at pTNM II-IV (P = 0.02, Figure 5F). Furthermore, the DFS of patients with superficial subtype was significantly longer than patients with other gross classifications (P = 0.007, Figure 5H). Moreover, LNM-positive patients also tended to had a worse DFS than LNM-negative patients (P = 0.07; Figure 5D). Multivariate analysis demonstrated that only pT stage was the independent DFS prognostic factor for patients with PMME (P = 0.02, HR: 1.93, 95%CI: 1.09-3.42) (Table 4).
Primary mucosal melanomas can be found in the mucosal membranes of the respiratory, gastroin
The male-to-female ratio of PMME was 2.2:1, and the mean age was 58.5 ± 9.7 years. The most common site was the middle and lower thoracic esophagus, which accounted for 94.5%. All of the features resembled those of esophageal squamous cell carcinoma (ESCC), a major form of esophageal malignancies in China. The male-to-female ratio of Japanese patients with PMME was 3.5:1, and the median age was 64.5 years[130], which was much higher than that of Chinese patients. In Western populations, male patients were only a little more than female ones with a male-to-female ratio of 1:3.1, and the mean age was 71.8 ± 13.6 years[131]. This distinction suggested that there might be different tumorigeneses between the Asian and Western populations with PMME. Both the middle and lower esophagus were the most common location of PMME for the Asian and Western populations[130,131]. Additionally, our results showed that the tumor masses of female patients were prone to being located in the upper esophagus compared with males, which prompted that an endoscopist should pay more attention to the upper thoracic esophagus of female patients to avoid missing an early lesion even though PMME is rare in the upper of the esophagus.
Polypoid lesions (79.5%) were the predominant gross classification of PMME, many of which are relatively soft, friable, and easily bleed. Sometimes, it was mistaken for phlebangioma under endoscopy[36,86,105]. There were only 5% of patients with PMME who had superficial lesions. The physician and endoscopist might be unfamiliar with the manifestations of PMME at early stage. In one patient from Kunming City, China, who presented with retrosternal pain after eating for 7 d, the first endoscopy showed several black lesions scattered throughout the middle esophagus. He was misdiagnosed because the doctor was unfamiliar with PMME. After 8 mo, the second endoscopy showed a polypoid lesion. The patient died 3 mo after surgery because of systemic metastasis[48].
The pathognomonic endoscopic finding of PMME is pigmentation. Our results showed that about 71.9% of PMME masses had a pigmented surface, which was similar to a previous study[131] showing that 26.9% of the lesions were amelanotic. These results suggested that the absence of pigmentation does not necessarily exclude PMME[3,132]. PMME is always surrounded by satellite lesions. Our results showed that one third of patients had multiple lesions, which was a little higher than that in Japanese patients[3], perhaps because one third of Japanese patients had superficial lesions. Physicians and endoscopists should enhance their awareness of rare diseases of the esophagus, paying particular attention to early lesion, to avoid missed diagnosis and misdiagnosis.
In our study, only 55.8% of patients were clearly diagnosed by biopsy before surgery, which was similar to previous studies[5-7]. The possible reasons for PMME misdiagnosis were as follows[5,6]: (1) Limited biopsy tissue without enough immunohistochemical analysis; (2) Lacking experience in the diagnosis of PMME in clinical practice; (3) Some tumors had no pigmented surface or no melanin granules in the cytoplasm; and (4) The lesion tissue was not biopsied by endoscopy because it bled readily. An accurate diagnosis could be obtained by immunohistochemical analysis. Human melanoma black antibody 45 (HMB45), melanoma antigen protein (Melan-A), and S100 are the specific diagnostic indicators for melanoma.
Melanoma might be associated with cancer predisposition syndromes[133]. In addition, a history of melanoma approximately increase the risk of subsequent melanoma[134]. Thus, multiple imaging diagnostics were employed in PMME and other mucosal melanoma to evaluate primary tumor, metastasis, and treatment responses[127]. Ultrasonography, endoscopic ultrasound, CT, magnetic resonance imaging, and positron emission tomography (PET) contribute to the information for diagnosis and management[127]. PET/CT improves the diagnosis, staging, treatment evaluation, and surveillance of tumors. It is currently considered to be the most sensitive method for the identification of metastatic lesions of solid tumors and has a huge impact on patient management[127].
The tumor size of PMME had a wide range, and the mean value was 5.2 ± 2.7 cm, which was similar to Japanese patients[130]. Previous studies[3,135,136] considered that PMME is prone to spread longitudinally, and local recurrence is frequently found soon after surgery. Thus, PMME should be resected with adequate margins. Masses in male patients had a significantly larger tumor size than that in female patients. Men might endure symptoms longer than women before seeking medical care[137].
The overall LNM-positive rate in our study was 51.2%. Our results showed that nearly half of PMME were at early pT stage, which was different from ESCC - mainly at the advanced pT stage. There were 52.2% of Japanese patients with PMME limited to the submucosal layer[130]. No LNM was found in patients at the pT1a stage in the present study and a previous study[50]. Interestingly, the frequency of LNM increased sharply to 45.3% in our study when the primary tumor was at the pT1b stage. Dai et al[5] found that the rate of LNM was as high as 54.2% among patients with pT1 tumors. The risk of LNM increased about 2.5 times along with the deeper depth of the tumor invasion. Previous studies[5,130] also indicated that with a deeper tumor invasion, the probability of LNM was higher. PMME might metastasize through blood or lymph vessels at early stage. Extended lymph node dissection combined with radical esophagectomy should be emphasized even when the tumor is at the pT1b stage.
The median OS of patients with PMME was 11 mo and the 5-year OS was 12%, which were similar to those of the previous studies[5,7]. Japanese patients with PMME have a relatively better survival with a 5-year OS of 25.3%[130]. For the Western population with PMME, the 3-year OS was only 7.3%[131]. It seems the Western population with PMME has a worse survival rate compared with the Asian population, which might be related to elder age of the diagnosed Western patients. Furthermore, PMME patients had poorer outcomes compared with common malignancies of the esophagus (ESCC, adenocarcinoma, and small cell carcinoma)[131]. It is necessary to employ a multidisciplinary team to improve treatments and outcomes for patients with PMME[5].
Multivariate analysis showed that pT (depth of tumor invasion) is an independent prognostic factor for both OS and DFS in patients with PMME. Patients at pT1 had better OS, which was also found in previous studies focused on the Chinese[5] and Japanese[130] populations. As mentioned previously, LNM was extremely rare for the tumor at pT1a, and it increased rapidly for tumors at pT1b or the advanced pT stage.
LNM was also an independent prognostic factor for OS. Previous studies on Chinese[5,7,50] and Japanese[130] patients also suggested that LNM was strongly associated with a poor prognosis. However, no influence of LNM on prognosis was found in the Western population[131]. Furthermore, Dai et al[5] showed that ≥ 12 lymph nodes dissected was an independent factor for OS and DFS. A thorough lymph node dissection should be emphasized in the surgical treatment of PMME.
Patients at an advanced pTNM stage, including II-IV, had a significantly worse OS and DFS compared with patients at pTNM I. Similar results were also found in previous studies[4,5]. Our results and others[4,5] suggested that TNM stage of PMME according to the AJCC classification for esophageal cancer might discriminate the prognosis of patients with PMME. Although the TNM stage in accordance with the mucosal melanoma classification could also separate the survival curves, the difference was not statistically significant[6]. Further study is needed to confirm the standard staging system of PMME[6].
Until now, treatment consensus on PMME had not been established because of its low prevalence. Surgery is still the primary option for resectable tumors. The median OS for patients who received immunotherapy besides surgery and chemoradiotherapy tended to be longer than patients who received surgery plus chemoradiotherapy or patients who only received surgery. However, there was no apparent difference in DFS between patients who received adjuvant therapy in addition to surgery and those who only received surgery. A comparison of the prognosis between surgery and adjuvant therapy was not conducted because there were only four patients successfully followed who only received adjuvant treatments. Many studies tried to seek optional treatments for patients with PMME. Dai et al[5] indicated that adjuvant therapy could improve both DFS and OS of patients with PMME. Wang et al[4] also suggested that postoperative chemotherapy could improve DFS. Additionally, PD-1 inhibitors might be a viable option for patients with PMME because the tumor has a dramatically high response rate to PD-1 checkpoint inhibitor monotherapy[4]. Systemic treatment of PMME, including surgery, chemoradiotherapy, and immunotherapy, should be used to improve multidisciplinary treatments and outcomes for patients with PMME.
Male patients tend to have a worse prognosis compared with female patients. Previous studies indicated that male gender was an independent prognostic predictor of PMME[5,6,128]. Our results also found that male patients had a larger tumor size compared with female patients. The serum estradiol significantly decreased in both male and female patients with ESCC or precancerous lesions[138]; moreover, the expression of estrogen receptor in precursor lesions of the esophagus changed during the multistage process of esophageal carcinogenesis[139]. All those phenomena suggested that estrogen might play an important role in esophageal malignancy.
PMME is a rare esophageal malignancy with a poor prognosis. Because of the low rate of correct diagnosis before surgery, physicians and endoscopists should develop their awareness of rare diseases of the esophagus, paying particular attention to early lesions. Extended lymph node dissection combined with radical esophagectomy should be stressed because of multifocality and high frequency of LNM — even the depth of the tumor invasion is limited to within the submucosal layer. Both the LNM and pT stage are independent prognostic factors for the OS, while only pT stage was identified to be an independent prognostic factor for the DFS of patients with PMME. Adjuvant treatment, particularly immunotherapy, might be used in clinical practice to improve multidisciplinary treatments and the prognosis of patients with PMME.
Primary malignant melanoma of the esophagus (PMME) is a rare malignant disease. It has not been well characterized in terms of clinicopathology and survival.
The clinical features, survival, and prognostic factors of Chinese patients with PMME are not comprehensively analyzed until now.
This study aimed to investigate the clinical features, survival, and prognostic factors of Chinese patients with PMME.
The clinicopathological findings of ten cases with PMME treated at our hospital and 280 cases from both the English- and Chinese-language literature which focused on Chinese patients with PMME were analyzed.
Only about half of the patients (55.8%) were accurately diagnosed before surgery. Lymph node metastasis (LNM) was easy to be found with a positive rate of 45.3% even when the tumor was confined in the submucosal layer. The risk of LNM was significantly raised along with the increase of pT stage (P < 0.001) and larger tumor size (P = 0.006). The median overall survival (OS) and disease-free survival (DFS) were 11 mo and 5.3 mo, respectively. Multivariate Cox analysis showed that both pT stage (P = 0.005) and LNM (P = 0.009) were independent prognostic factors for OS, but only advanced pT stage (P = 0.02) was identified to be a significant independent indicator of poor RFS in patients with PMME.
Correct diagnosis of PMME before surgery is low. Both LNM and pT stage are the independent prognosis factors for OS, but only pT stage was identified to be an independent indicator for DFS of patients with PMME.
Physicians and endoscopists should develop their awareness of rare diseases of the esophagus, paying particular attention to early lesions. Extended lymph node dissection combined with a radical esophagectomy should be stressed because of multifocality and a high frequency of LNM. Adjuvant treatment, particularly immunotherapy, might be used in clinical practice to improve multidisciplinary treatments and the prognosis of patients with PMME.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Corvino A, Italy; Dambrauskas Z, Lithuania; Gupta R, India S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Yuan YY
| 1. | Lam AK. Updates on World Health Organization classification and staging of esophageal tumors: implications for future clinical practice. Hum Pathol. 2021;108:100-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Lam KY, Law S, Wong J. Malignant melanoma of the oesophagus: clinicopathological features, lack of p53 expression and steroid receptors and a review of the literature. Eur J Surg Oncol. 1999;25:168-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Schizas D, Mylonas KS, Bagias G, Mastoraki A, Ioannidi M, Kanavidis P, Hasemaki N, Karavokyros I, Theodorou D, Liakakos T. Esophageal melanoma: a systematic review and exploratory recurrence and survival analysis. Dis Esophagus. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Wang X, Kong Y, Chi Z, Sheng X, Cui C, Mao L, Lian B, Tang B, Yan X, Si L, Guo J. Primary malignant melanoma of the esophagus: A retrospective analysis of clinical features, management, and survival of 76 patients. Thorac Cancer. 2019;10:950-956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Dai L, Wang ZM, Xue ZQ, He M, Yuan Y, Shang XQ, Chen KN; Chinese Cooperative Primary Malignant Melanoma of the Esophagus Group (CCPMMEG). Results of surgical treatment for primary malignant melanoma of the esophagus: A multicenter retrospective study. J Thorac Cardiovasc Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Sun H, Gong L, Zhao G, Zhan H, Meng B, Yu Z, Pan Z. Clinicopathological characteristics, staging classification, and survival outcomes of primary malignant melanoma of the esophagus. J Surg Oncol. 2018;117:588-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Chen H, Fu Q, Sun K. Characteristics and prognosis of primary malignant melanoma of the esophagus. Medicine (Baltimore). 2020;99:e20957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Ai L, Chen HX, Lu H. Primary malignant melanoma of esophagus: case report. Zhongguo Yixue Yingxiang Jishu. 2021;37:511. [DOI] [Full Text] |
| 9. | Liu ZJ, Geng TT, Gao SM. Primary melanoma of lower esophagus: report of one case. Zhongguo Linchuang Yixue Yingxiang Zazhi. 2020;31:70-71. |
| 10. | Li J, Li X, Song QY, Ge QY, Zhang ZH. Primary malignant melanoma of esophagus: a clinicopathological analysis of 6 cases. Zhonghua Bingli Xue Zazhi. 2020;49:1317-1319. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Lou J, Niu TT, Wang Y, Hou GQ. Primary malignant melanoma of esophagus with gastric metastasis: A case report. Guoji Yiyao Weisheng Daobao. 2020;26:1122-1123. |
| 12. | Sun XJ, Zhang W, Hua HY, Li P, Zhang PT. Clinical analysis of primary malignant melanoma of esophagus. Linchuang He Shiyan Yixue Zazhi. 2019;18:480-483. |
| 13. | Zhang RX, Li YY, Liu CJ, Wang WN, Cao Y, Bai YH, Zhang TJ. Advanced primary amelanotic malignant melanoma of the esophagus: A case report. World J Clin Cases. 2019;7:3160-3167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Li J. Primary esophageal malignant melanoma: a case report and literature review. Zhongguo Minkang Yixue. 2019;31:129-130. [DOI] [Full Text] |
| 15. | Song YY, Zhu Y, Ding C. Three cases of primary malignant melanoma of the esophagus. Zhongguo Xiong Xinxueguan Waike Linchuang Zazhi. 2019;26:192-194. [DOI] [Full Text] |
| 16. | Chen LX, Liu P, Gan MF. One case of primary malignant melanoma of the esophagus. Shiyong Zhongliu Zazhi. 2019;34:265-267. [DOI] [Full Text] |
| 17. | Li HJ, Yang JQ. One case of primary malignant melanoma of the esophagus. Yunnan Yiyao. 2019;40:190-191. |
| 18. | Liu QH, Long ZQ, Huang WM, Shang XQ, Li J. Clinical analysis of 6 cases of malignant melanoma of the esophagus. Zhongguo Yiyao Daobao. 2018;15:109-112. |
| 19. | Ling C, Feng J, Li J, Liu Q. Primary malignant melanoma of the esophagus. Turk J Gastroenterol. 2018;29:711-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Wei XJ, Zhang YN, Liu WH, Zheng XD, Zhang SH, Zhou XG. Primary malignant melanoma of esophagus. Zhonghua Bingli Xue Zazhi. 2018;47:548-550. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Liu YL, Zhou ZG, Yan HC. Two cases of primary malignant melanoma of the esophagus. Fangshe Xue Shijian. 2017;32:302-304. [DOI] [Full Text] |
| 22. | Wang FQ, Tan GM. Clinicopathological analysis of 5 cases of primary malignant melanoma of the esophagus. Linchuang Yu Bingli Xue Zazhi. 2017;37:245-251. [DOI] [Full Text] |
| 23. | Zhao T, Kong FW, Wang H, Liu D, Wang CY, Luo JH, Zhang M, Wu WB. A long-term survivor with esophageal melanoma and pulmonary metastasis after single-stage esophagectomy and lobectomy: Case report and literature review. Medicine (Baltimore). 2017;96:e7003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Zheng ZG, Sun WY. Clinicopathological analysis of primary malignant melanoma of esophagus. Zhejiang Shiyong Yixue. 2016;21:366-369. [DOI] [Full Text] |
| 25. | Gao S, Li J, Feng X, Shi S, He J. Characteristics and Surgical Outcomes for Primary Malignant Melanoma of the Esophagus. Sci Rep. 2016;6:23804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Liu H, Yan Y, Jiang CM. Primary Malignant Melanoma of the Esophagus With Unusual Endoscopic Findings: A Case Report and Literature Review. Medicine (Baltimore). 2016;95:e3479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Qiu X, Zhai SH. One case of primary malignant melanoma of the esophagus. Fangshe Xue Shijian. 2016;31:673-674. [DOI] [Full Text] |
| 28. | Wang M, Chen J, Sun K, Zhuang Y, Xu F, Xu B, Zhang H, Li Q, Zhang D. Primary malignant melanoma of the esophagus treated by endoscopic submucosal dissection: A case report. Exp Ther Med. 2016;12:1319-1322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Li HM, Yu JX, Yang HJ. Clinicopathological analysis of 5 cases of primary malignant melanoma of the esophagus. Zhongliu Jichu Yu Linchuang. 2016;29:361-362. [DOI] [Full Text] |
| 30. | Zhu HM, Zhang M, Cai L, Zhao QC, Chen L. Primary malignant melanoma of the esophagus: one case report. Weichangbing Xue He Ganbing Xue Zazhi. 2016;25:302-303. |
| 31. | Zhang Y, Zhang M. The diagnosis of primary esophageal malignant melanoma. Zhongliu Xue Zazhi. 2016;22:864-866. [DOI] [Full Text] |
| 32. | Sun C, Chai HN, Zhu Y, Xu XL, Chen F. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Bing Yu Yingxiang Zazhi. 2017;7:87-88. [DOI] [Full Text] |
| 33. | Yu Q, Yuan S. Primary malignant melanoma of the esophagus with subtotal esophagectomy: a case report. Int J Clin Exp Med. 2014;7:4519-4522. [PubMed] |
| 34. | Liu GJ, Wang B, Yu Z, Xia D, Xie SN, Liu F, Liu QY. Analysis of clinical characteristics and prognostic factors of 17 cases of primary malignant melanoma of the esophagus. Zhongguo Quanke Yixue. 2015;18:3561-3565. |
| 35. | Song X, Song H, Li HW. Analysis of clinical characteristics of 6 cases of primary malignant melanoma of the esophagus. Zhongliu Jichu Yu Linchuang. 2015;28:539-540. [DOI] [Full Text] |
| 36. | Zhang YP, Wang YJ, Zhang ST, Li P. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Neijing Zazhi. 2015;32:637-638. |
| 37. | Zhao XJ, Xie H, Li AQ, Sheng JQ. Primary malignant melanoma of the esophagus: one case report. Weichangbing Xue He Ganbing Xue Zazhi. 2015;24:666. |
| 38. | Yang DY. One case of primary malignant melanoma of the esophagus. Zhongliu Yufang Yu Zhiliao. 2014;27:159-160. [DOI] [Full Text] |
| 39. | Fan YY, Liu ZJ, Ye ZS, Zhou F, Yang XN, Hu YQ. Two cases of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Zazhi. 2014;34:414-415. [DOI] [Full Text] |
| 40. | Zheng J, Mo H, Ma S, Wang Z. Clinicopathological findings of primary esophageal malignant melanoma: report of six cases and review of literature. Int J Clin Exp Pathol. 2014;7:7230-7235. [PubMed] |
| 41. | Jiang W, Zou Z, Liu B. Primary malignant melanoma of the esophagus: A case report and review of the literature. Oncol Lett. 2015;9:2036-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Hu YM, Yan JD, Gao Y, Xia QA, Wu Y, Zhang ZY. Primary malignant melanoma of esophagus: a case report and review of literature. Int J Clin Exp Pathol. 2014;7:8176-8180. [PubMed] |
| 43. | Cheng DL, Liu P, Zhang J, Lin CY, Zeng M. One case of primary malignant melanoma of the esophagus. Zhongguo Xiong Xinxueguan Waike Linchuang Zazhi. 2011;27:357-360. [DOI] [Full Text] |
| 44. | Xue JR, Sheng Y, Yan JD, Xin H, Gao N, Jiao J. One case of primary malignant melanoma of the esophagus. Zhongguo Shiyan Zhenduan Xue. 2014;18:1897-1898. |
| 45. | Zhang JF, Mo HY, Ma SF, Wei Zhi. Primary malignant melanoma of the esophagus: A clinicopathological study of 5 cases. Linchuang Yu Shiyan Bingli Xue Zazhi. 2014;30:1090-1093. [DOI] [Full Text] |
| 46. | Wu IC, Lee JY, Wu CC. A rare but unique tumor in the esophagus. Primary esophageal melanoma. Gastroenterology. 2013;144:695, 856-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 47. | Li YH, Li X, Zou XP. Primary malignant melanoma of the esophagus: a case report. World J Gastroenterol. 2014;20:2731-2734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 48. | Lu ML, Huang H, Chang J, Li WH, Zhao GF, He HY, Tang P, Zheng MY, Niu YC, Fu W. Primary malignant melanoma of the esophagus: misdiagnosis and review of literature. Rev Esp Enferm Dig. 2013;105:488-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Yang L, Sun X, Meng X. A case of primary malignant melanoma of the esophagus. Dig Dis Sci. 2013;58:3634-3636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 50. | Wang S, Tachimori Y, Hokamura N, Igaki H, Kishino T, Kushima R. Diagnosis and surgical outcomes for primary malignant melanoma of the esophagus: a single-center experience. Ann Thorac Surg. 2013;96:1002-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 51. | Zhang L, Ma W, Li Y. Huge primary malignant melanoma of the esophagus: A case report and literature review. Thorac Cancer. 2013;4:479-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 52. | Liu Y, Chu XY, Xue ZQ, Ma KF. Malignant melanoma in esophagus: A clinical analysis of 9 cases. Jiefangjun Yixueyuan Xuebao. 2013;34:142-144. |
| 53. | Tang XB, Xu YG, Tang MX, Zhang J, Liu T. One case of primary malignant melanoma of the esophagus. Zhenduan Bingli Xue Zazhi. 2013;20:156. [DOI] [Full Text] |
| 54. | Niu XW, He SL, Chen D, Yan D, Ma MJ, Han B, Zhang Y. One case of primary malignant melanoma of the esophagus. Zhongguo Zhongliu Linchuang. 2012;39:614. [DOI] [Full Text] |
| 55. | Yang JY, Chen XL, Ji F. One case of primary malignant melanoma of the esophagus by endoscopic resection and literature review. Zhonghua Xiaohua Neijing Zazhi. 2012;29:172-173. [DOI] [Full Text] |
| 56. | Wang ZY, Yang WJ, Wu JL, Sun lW, Guo Y, Fu JL. One case of primary malignant melanoma of the esophagus. Zhonghua Linchuang Yishi Zazhi. 2012;6:6620-6621. |
| 57. | Lv S, Wang XL. One case of primary malignant melanoma of the esophagus. Xibei Guofang Yixue Zazhi. 2013;34:318. |
| 58. | Liu WP, Zhuang HX, Lai YD, Xu XN. Clinical characteristics primary malignant melanoma of digestive tract (Reports of 10cases). Zhongguo Neijing Zazhi. 2011;17:543-547. |
| 59. | Yu H, Huang XY, Li Y, Xie X, Zhou JL, Zhang LJ, Fu JH, Wang X. Primary malignant melanoma of the esophagus: a study of clinical features, pathology, management and prognosis. Dis Esophagus. 2011;24:109-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 60. | Li B, Hu CJ. Li JR, Tang XB, Li HH. One case of primary malignant melanoma of the esophagus and literature review. Zhongguo Zhongliu Waike Zazhi. 2012;4:123-125. [DOI] [Full Text] |
| 61. | Zhu J, Bai RZ, Weng Y, Cai M, Chang JH, Geng JQ. Two cases report of primary esophageal malignant melanoma and literature review. Zhonghua Linchuang Yishi Zazhi. 2011;5:3371-3373. |
| 62. | Tang Y, Jiang M, Hu X, Chen C, Huang Q. Difficulties encountered in the diagnosis of primary esophageal malignant melanoma by 18F-fluorodeoxyglucose positron emission tomography/computed tomography: a case report. Ann Palliat Med. 2021;10:4975-4981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Tao JY, Liu HZ, Wang YX. One case of primary malignant melanoma of the esophagus. Zhongguo Yiliao Qianyan. 2010;5:66. |
| 64. | Hu J, Chang D, Gong M, Tian F. Clinicopathological characteristics and treatment of primary malignant melanoma of esophagus. Zhonghua Yixue Zazhi. 2010;90:1785-1787. |
| 65. | Ma K, Ye B, Liu XY, Sun KL, He J. 10 cases of primary malignant melanoma of the esophagus. Zhongguo Yikan. 2010;45:53-55. [DOI] [Full Text] |
| 66. | Li GR, Dai JH, Chen GH, Miao FL, Zhang JZ. 3 cases of primary malignant melanoma of the esophagus. Shiyong Aizheng Zazhi. 2010;25:81-82. |
| 67. | Yang X, Qu J, Wang S. Primary malignant melanoma of the esophagus. Melanoma Res. 2010;20:59-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 68. | Cai ZX, Hong SF, Ye BN, Huang ZZ, Li DM. One case of primary malignant melanoma of the esophagus. Zhongguo Xiandai Yisheng. 2009;47:132. |
| 69. | Zhang H, Zhang SM, Xin DH, Cai ZG, Xu XP. A case of primary malignant melanoma of the esophagus report and literature review. Shiyong Aizheng Zazhi. 2009;124:407-410. |
| 70. | Zhuang YZ, Zhang ZY, Liao YQ. One case of primary malignant melanoma of the esophagus. Zhonghua Bingli Xue Zazhi. 2009;38:60-61. [DOI] [Full Text] |
| 71. | Yin ZW, Zhao J, Xin XD, Qin W, Han XD, Zhang YX. One case of primary malignant melanoma of the esophagus. Linchuang Fangshe Xue Zazhi. 2009;28:434. |
| 72. | Li L, Tian H, Wang SZ. Analysis of clinical characteristics of three cases of primary malignant melanoma of the esophagus. Zhongguo Laonian Xue Zazhi. 2009;29:1703-1704. |
| 73. | Lian JH, Han F, Hu F, Hu CG, Niu JJ. Three One cases of primary malignant melanoma of the esophagus and literature review. Zhongliu Yanjiu Yu Linchuang. 2009;21:409-411. [DOI] [Full Text] |
| 74. | Zhao SC, Xiong SJ, Zhuang WX, Gao F. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Neijing Zazhi. 2009;26:302. |
| 75. | Gong L, Zhao JY, Chen HC, Sun RL, Zhu SJ, Lan M, Zhang W. The clinicopathological observation of primary malignant melanoma of the esophagus. Xiandai Zhongliu Yixue. 2008;16:1496-1499. |
| 76. | Zhang BH, Wang JS, He JJ. A case of primary malignant melanoma of the esophagus report and literature review. Xiandai Zhongliu Yixue. 2008;16:1524-1525. |
| 77. | Shen C, Zhang LH, Zhang SL. One case of primary malignant melanoma of the esophagus. Fangshe Xue Shijian. 2008;23:32. |
| 78. | Tzung-Ju L, Tsai-Wang H, Shih-Chun L. Primary malignant melanoma of the esophagus. Ann Saudi Med. 2008;28:458-460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 79. | Wang S, Thamboo TP, Nga ME, Zin T, Cheng A, Tan KB. C-kit positive amelanotic melanoma of the oesophagus: a potential diagnostic pitfall. Pathology. 2008;40:527-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 80. | Zhang AB. Analysis of clinical characteristics of primary malignant melanoma of the esophagus. Shiyong Linchuang Yiyao Zazhi. 2008;12:118-120. |
| 81. | Li J, Zhang YX, Li QJ. One case of primary malignant melanoma of the esophagus and literature review. Linchuang Yixue. 2008;28:56-57. |
| 82. | Liang WM, Wen BQ, Zhu J, Li P, Wang L, Xu JZ, Zhang XJ. One case of primary malignant melanoma of the esophagus by endoscopic resection. Xiandai Yiyao Weisheng. 2008;24:1384. |
| 83. | Jia H, Liang B, Feng CW. One case of primary malignant melanoma of the esophagus and cardia. Zhonghua Zhongliu Zazhi. 2008;30:468. |
| 84. | Chen GM, Cen XB, Liu H. One case of primary malignant melanoma of the esophagus. Xinan Yike Daxue Xuebao. 2008;03:311. |
| 85. | Gan YL, He XL, Shao GF. Clinicopathological analysis of primary malignant melanoma of esophagus. Xiandai Shiyong Yixue. 2007;19:278-279. |
| 86. | Liu F. One case of primary malignant melanoma of the esophagus. Zhongguo Wuzhen Xue Zazhi. 2008;8:5285. |
| 87. | Han XH, Chen M. One case of primary malignant melanoma of the esophagus. Linchuang Yu Shiyan Bingli Xue Zazhi. 2006;22:124. |
| 88. | Lan YZ, Li SH, Wang S, Zhou AH. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Neijing Zazhi. 2006;23:149-150. |
| 89. | Wang GJ, Li CQ, Li CP, Hou YG, Li F. Analysis of two cases of primary malignant melanoma of the esophagus. Shanxi Yiyao Zazhi. 2006;35:456-457. |
| 90. | Xia Y, Feng CN, Gao Q, Yao J, Wang Y, Zheng Q. One case of primary malignant melanoma of the esophagus. Waike Lilun Yu Shijian. 2006;11:461. |
| 91. | Ma XP, Wang Y, Li JJ. Primary esophageal malignant melanoma: A case report and literature review. Ningxia Yixue Zazhi. 2005;27:684-685. |
| 92. | Bao SL, Gao P. One case of primary malignant melanoma of the esophagus. Ningxia Yixue Zazhi. 2004;26:325. |
| 93. | Ding BG, Sun Y’E, Zhou NK, Yan M. Clinicopathological characteristics and treatment of primary malignant melanoma of esophagus- two cases report and literature review. Zhongguo Xiong Xinxueguan Waike Linchuang Zazhi. 2003;10:226-228. |
| 94. | Gao XJ, Zhang QG, Wang YJ, Liu HJ, Li W, Chen MH, Zhang LG, Tian D. Diagnosis and treatment of primary malignant melanoma of the esophagus. Binzhou Yixueyuan Xuebao. 2003;26:374-375. |
| 95. | Shi LQ, Lu QM, Zhang YL. Two cases of primary malignant melanoma of the esophagus. Shijie Huaren Xiaohua Zazhi. 2003;12:2052. |
| 96. | Lin CY, Cheng YL, Huang WH, Lee SC. Primary malignant melanoma of the oesophagus presenting with massive melena and hypovolemic shock. ANZ J Surg. 2002;72:62-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 97. | Xu G, Chen DZ, Yang H. Clinicopathologic characteristics and histogenesis of primary malignant melanoma of the esophagus. Zhongguo Zhongliu Linchuang Yu Kangfu. 2002;9:88-90. [DOI] [Full Text] |
| 98. | Kong P, Liu HL. One case of primary malignant melanoma of the esophagus. Shiyong Fangshe Xue Zazhi. 2002;18:252-253. |
| 99. | Ren YC. One case of primary malignant melanoma of the esophagus. Henan Daxue Xuebao (Yixueban). 2002;21:76. |
| 100. | Li Y, Liu GY, Wang FH, Ye LX, Zhang H, Liu HG. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Neijing Zazhi. 2002;19:97. |
| 101. | Piao XX, Zhang Y, Piao DM, Jin YR. One case of primary malignant melanoma of the esophagus by endoscopic resection. Zhonghua Xiaohua Neijing Zazhi. 2001;18:380. |
| 102. | Zhong HC, Wang XP, Mei LY. Primary esophageal malignant melanoma: A case report and literature review. Huanan Guofang Yixue Zazhi. 2000;14:65-67. |
| 103. | Xu YH, Liu P, Zou WZ. One case of primary malignant melanoma of the esophagus. Zhenduan Bingli Xue Zahi. 2001;8:165. |
| 104. | Zhao XX, Shao L, Bei ZQ, Chen J, Shi CH, Zhang Q. Clinicopathological characteristics of two cases of primary malignant melanoma of the esophagus. Zhongliu Jichu Yu Linchuang. 2001;1:76. |
| 105. | Ren JJ, Ma S’E. The X-ray and pathological features of primary malignant melanoma of the esophagus. Yixue Yingxiang Xue Zazhi. 1998;3:49-50. |
| 106. | Li YZ, Tang YL, Li GP, Yan F. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Neijing Zazhi. 1998;4:12. |
| 107. | Zhao WZ, Xu J, Yang D. One case of primary malignant melanoma of the esophagus. Zhonghua Xiong Xinxueguan Waike Zazhi. 1998;14:147. |
| 108. | Chen JS, Shi LS, Zhan M, Wang H, Xu J. One case of primary malignant melanoma of the esophagus. Zhonghua Zhongliu Zazhi. 1998;20:73. |
| 109. | Shao ZQ, Yan MH, Li ZY. Two cases of primary malignant melanoma of the esophagus. Zhonghua Zhongliu Zazhi. 1997;19:426. |
| 110. | Wang R, Wang ZL, Chen Y, He M, Ping YM, Wang XL. Primary malignant melanoma of the esophagus (Reports of 3 cases). Hebei Yixue. 1997;19:67-68. |
| 111. | Duan XF, Gao XX, Tian D, Wang CY. One case of primary malignant melanoma of the esophagus. Zhonghua Zhongliu Zazhi. 1997;19:266. |
| 112. | Chen CZ, Wang CY, Wang ZH. One case of primary malignant melanoma of the esophagus and literature review. Shangdong Yixue Gaodeng Zhuanke Xuexiao Xuebao. 1999;21:15-16. |
| 113. | Cai KC, Zhang LX. One case of primary malignant melanoma of the esophagus. Jiefangjun Yixue Zazhi. 1997;22:433. |
| 114. | Liu AD, Shi YJ. One case of primary malignant melanoma of the esophagus. Zhonghua Xiaohua Neijing Zazhi. 1997;14:4. |
| 115. | Jiang B, Zheng B. One case of primary malignant melanoma of the esophagus. Shiyong Aizheng Zazhi. 1999;14:5-6. |
| 116. | Zhang LH, Pan YM, Tang YX, Zhang BG, Chen QF. Two cases of primary malignant melanoma of the esophagus. Tongji Yike Daxue Xuebao. 1996;25:170. |
| 117. | Guo KJ. One case of primary malignant melanoma of the esophagus. Shiyong Aizheng Zazhi. 1997;12:104. |
| 118. | Tong GW, Chen YR. One case of primary malignant melanoma of the esophagus. Aizheng. 1997;01:70. |
| 119. | Fu GZ, Chen G, Song SH, Yang CJ. Two cases of primary malignant melanoma of the esophagus. Tianjin Yiyao. 1995;23:55-56. |
| 120. | Zhang JJ, Hu L. One case of primary malignant melanoma of the esophagus. Zhonghua Bingli Xue Zazhi. 1987;16:287. |
| 121. | Gao ZX, Liu Y, Lv CY. Primary malignant melanoma of the esophagus (reports of one case). Tianjin Yiyao. 1985;06:374. |
| 122. | Wang JZ, Zhang YJ, Mao YQ, Zhang JQ, Tan YB. Analysis of clinical characteristics of one case of primary malignant melanoma of the esophagus and literature review. Tianjin Yiyao. 1986;11:689-690. |
| 123. | Li CL, Qian H. One case of primary malignant melanoma of the esophagus. Zhonghua Zhongliu Zazhi. 1983;01:80. |
| 124. | Wang GW. One case of primary malignant melanoma of the esophagus. Zhonghua Zhongliu Zazhi. 1984;03:222. |
| 125. | Zhu ZX, Wang GM. One case of primary malignant melanoma of the esophagus. Zhonghua Waike Zazhi. 1984;05:294. |
| 126. | Bao YH, Song ST, Yu SC, Li GM. One case of primary malignant melanoma of the esophagus. Beijing Yiyao. 1981;05:320. |
| 127. | Yde SS, Sjoegren P, Heje M, Stolle LB. Mucosal Melanoma: a Literature Review. Curr Oncol Rep. 2018;20:28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 128. | Malaguarnera G, Madeddu R, Catania VE, Bertino G, Morelli L, Perrotta RE, Drago F, Malaguarnera M, Latteri S. Anorectal mucosal melanoma. Oncotarget. 2018;9:8785-8800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 129. | Corvino A, Catalano O, Corvino F, Petrillo A. Rectal melanoma presenting as a solitary complex cystic liver lesion: role of contrast-specific low-MI real-time ultrasound imaging. J Ultrasound. 2016;19:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 130. | Makuuchi H, Takubo K, Yanagisawa A, Yamamoto S. Esophageal malignant melanoma: analysis of 134 cases collected by the Japan Esophageal Society. Esophagus. 2015;12:158-169. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 131. | Chen J, Wen J, Xu X, Liu D, Huang L, Fan M. Primary malignant melanoma of the esophagus: a population-based study. Transl Cancer Res. 2018;7:1253-1262. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 132. | Taniyama K, Suzuki H, Sakuramachi S, Toyoda T, Matsuda M, Tahara E. Amelanotic malignant melanoma of the esophagus: case report and review of the literature. Jpn J Clin Oncol. 1990;20:286-295. [PubMed] |
| 133. | Vogt A, Schmid S, Heinimann K, Frick H, Herrmann C, Cerny T, Omlin A. Multiple primary tumours: challenges and approaches, a review. ESMO Open. 2017;2:e000172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 369] [Article Influence: 46.1] [Reference Citation Analysis (1)] |
| 134. | Bradford PT, Freedman DM, Goldstein AM, Tucker MA. Increased risk of second primary cancers after a diagnosis of melanoma. Arch Dermatol. 2010;146:265-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 178] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 135. | Bisceglia M, Perri F, Tucci A, Tardio M, Panniello G, Vita G, Pasquinelli G. Primary malignant melanoma of the esophagus: a clinicopathologic study of a case with comprehensive literature review. Adv Anat Pathol. 2011;18:235-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 136. | Volpin E, Sauvanet A, Couvelard A, Belghiti J. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus. 2002;15:244-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 86] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 137. | Wang Y, Hunt K, Nazareth I, Freemantle N, Petersen I. Do men consult less than women? BMJ Open. 2013;3:e003320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 292] [Cited by in RCA: 377] [Article Influence: 31.4] [Reference Citation Analysis (1)] |
| 138. | Wang QM, Yuan L, Qi YJ, Ma ZY, Wang LD. Estrogen analogues: promising target for prevention and treatment of esophageal squamous cell carcinoma in high risk areas. Med Sci Monit. 2010;16:HY19-HY22. [PubMed] |
| 139. | Wang QM, Qi YJ, Jiang Q, Ma YF, Wang LD. Relevance of serum estradiol and estrogen receptor beta expression from a high-incidence area for esophageal squamous cell carcinoma in China. Med Oncol. 2011;28:188-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |