Published online Feb 15, 2022. doi: 10.4251/wjgo.v14.i2.396
Peer-review started: September 7, 2021
First decision: November 8, 2021
Revised: November 8, 2021
Accepted: January 5, 2022
Article in press: January 5, 2022
Published online: February 15, 2022
Processing time: 156 Days and 5.6 Hours
The most common histological type of gastric cancer (GC) is gastric adenocarcinoma arising from the gastric epithelium. Less common variants include mesenchymal, lymphoproliferative and neuroendocrine neoplasms. The Lauren scheme classifies GC into intestinal type, diffuse type and mixed type. The WHO classification includes papillary, tubular, mucinous, poorly cohesive and mixed GC. Chronic atrophic gastritis (CAG) and intestinal metaplasia are recommended as common precancerous conditions. No definite precancerous condition of diffuse/poorly/undifferentiated type is recommended. Chronic superficial inflammation and hyperplasia of foveolar cells may be the focus. Presently, the management of early GC and precancerous conditions mainly relies on endoscopy including diagnosis, treatment and surveillance. Management of precancerous conditions promotes the early detection and treatment of early GC, and even prevent the occurrence of GC. In the review, precancerous conditions including CAG, metaplasia, foveolar hyperplasia and gastric hyperplastic polyps derived from the gastric epithelium have been concluded, based on the overview of gastric epithelial histological organization and its renewal.
Core Tip: We provided a detailed overview of gastric epithelial organization and its renewal and reviewed precancerous conditions including chronic atrophic gastritis, spasmolytic polypeptide-expressing metaplasia, intestinal metaplasia, foveolar hyperplasia and gastric hyperplastic polyps derived from gastric epithelium based on histological perspective, covering their epidemiology, clinical management and advances, histological structure, causes and potential origin and reversibility. The origins, processes and reversibility are the main controversial topics. More clinical and basic research on molecular alterations of these gastric lesions may shed light on the controversies.
- Citation: Yang H, Yang WJ, Hu B. Gastric epithelial histology and precancerous conditions. World J Gastrointest Oncol 2022; 14(2): 396-412
- URL: https://www.wjgnet.com/1948-5204/full/v14/i2/396.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i2.396
Gastric cancer (GC) is a major global problem, ranking fifth in incidence and third in cancer-related mortality worldwide, and it was responsible for over 1000000 new cases in 2018 and an estimated 783000 deaths[1]. The incidence of GC varies by sex and region. The incidence is twice as high in men as in women. Incidence rates are markedly elevated in Eastern Asia, whereas the rates in Northern America and Northern Europe are generally low and are equivalent to those seen across African regions[1]. Risk factors include Helicobacter pylori ( H. pylori) infection, family history (hereditary diffuse GC due to germline mutations in CDH1), dietary intake of foods preserved by salting and low fruit intake, Epstein–Barr virus infection, alcohol consumption, active tobacco smoking, consumption of foods contaminated with aflatoxin, nitrates and fungi, and pernicious anemia[2]. The GC incidence has decreased in a growing number of countries partly due to decreasing risk factors, improving standards of living and increasing use of screening programs in high-risk populations[3,4]. GC screening is recommended in regions of high prevalence and patients at risk. In Japan and South Korea, national population-based screening programs for early GC are performed most commonly using barium radiography or endoscopic screening aimed at patients over 40 or 50 years old. These strategies have achieved a 5-year survival rate of more than 50% in Japan (60.3%) and South Korea (55.7%), which is higher than that in China (35.9%) from 2010 to 2014[5], and endoscopy is with superiority over other screening techniques such as barium radiography and is more cost-effective[6-8]. In Asian guidelines, high-risk individuals, including male patients, Chinese patients, patients with first-degree relatives who have GC, patients with persistent H. pylori infection and patients with age 40–45 years or older, should be considered for targeted invasive screening in regions with moderate or low incidence of GC[9]. In contrast with Asian guidelines, European guidelines recommend that patients with advanced stages of atrophic gastritis (including severe atrophic changes or intestinal metaplasia (IM) in both the antrum and corpus, OLGA/OLGIM III/IV) should be followed up with high-quality endoscopy every 3 years. Patients with advanced stages of atrophic gastritis and with a family history of GC may benefit from a more intensive follow-up (every 1–2 years after diagnosis; every 3–5 years for those with autoimmune gastritis)[10]. Patients with IM specifically at higher risk of GC (those with incomplete IM or extensive IM and a family history) and/or who are at overall increased risk for GC (racial/ethnic minorities, immigrants from regions with high GC incidence, or individuals with a first-degree relative with GC) may reasonably elect to undergo repeat endoscopy within 1 year for risk stratification[11]. H. pylori gastritis accounts for more than 80% of gastritis, and persistent infection may eventually cause chronic atrophic gastritis (CAG) through the canonical process originating from acute-on-chronic inflammation. H. pylori eradication abolishes the inflammatory response[12]. A noninvasive test-and-treat strategy is appropriate for uninvestigated dyspepsia[13]. An endoscopy-based strategy combined with Sydney system biopsies is supposed to be considered in patients who have dyspeptic symptoms and/or alarm symptoms or older patients, particularly in low-prevalence H. pylori populations (< 10%)[14]. A screen-and-treat strategy is recommended in communities at high risk of GC[15]. GC still carries a poor prognosis, in part due to the late stage of diagnosis. Recognition of precancerous conditions is indispensable for the management of early GC. In this review, we have focused on precancerous gastric conditions, including CAG, metaplasia, foveolar hyperplasia and gastric hyperplastic polyps derived from gastric epithelium, and provide an overview of gastric epithelium organization and renewal.
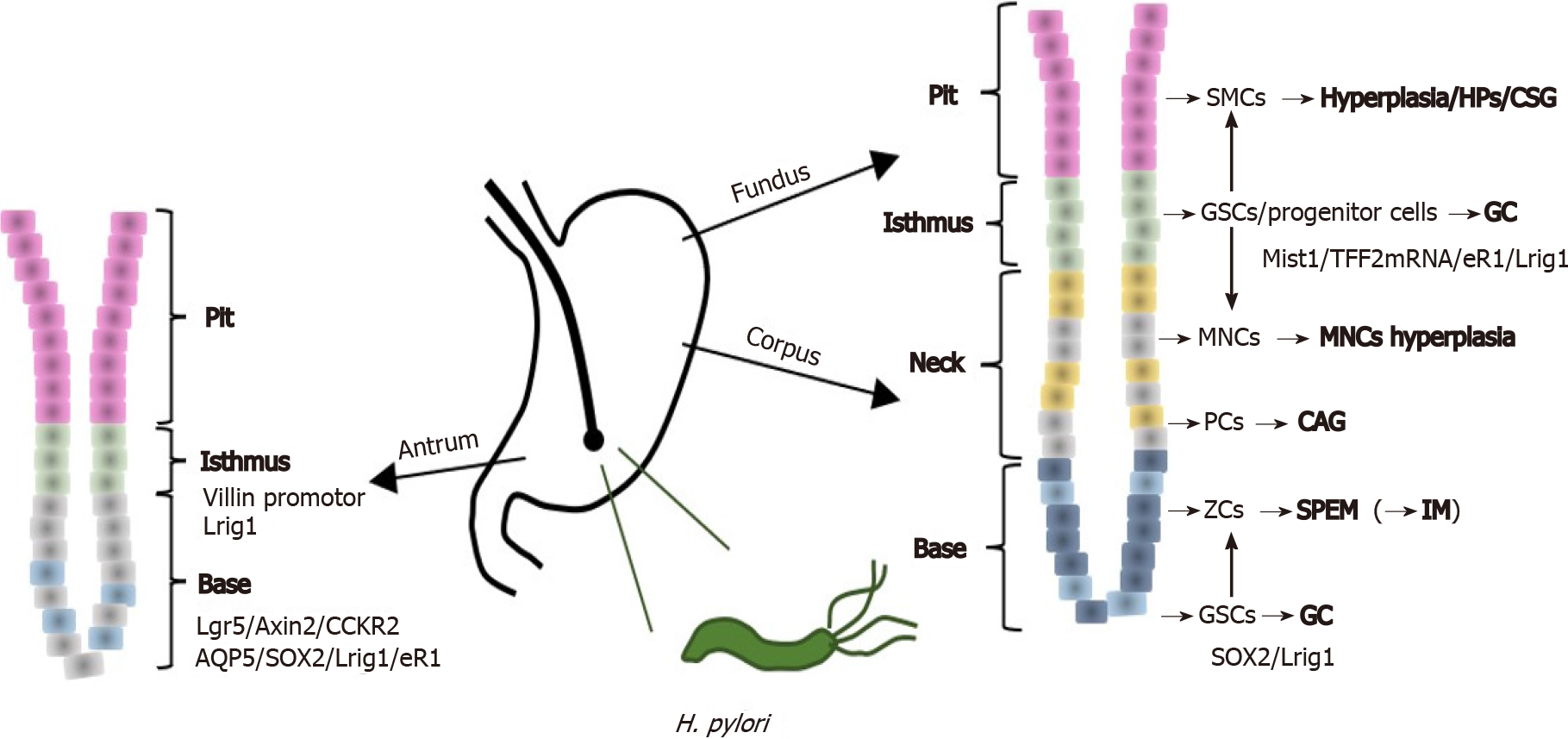
Histologically, the self-renewing gastric epithelium is covered by surface mucous cells (SMCs) which also line the approximately 3 million funnel-shaped gastric pits. Gastric glands in the isthmus, neck and base open into the bottom of these pits. The combination of a pit and a gland is called a gastric unit[16]. The gastric corpus and body are characterized by oxyntic glands with parietal cells (PCs) and chief cells/zymogenic cells (ZCs). The gastric units of the antrum consist predominantly of mucous cells and are largely devoid of PCs and ZCs[17]. The epithelium of fundic units contains mesenchymal stem cells (MSCs), PCs, mucous neck cells (MNCs), ZCs and several types of enteroendocrine cells[16]. The antral unit contains SMCs, antral gland cells (AGCs) and endocrine cells (gastrin-producing G cells, D and EC cells). The genes used to identify cell clusters include ATP4a (PCs)[18], trefoil factor family 2 (TFF2) and MUC6 (MNCs)[19], MUC5AC and TFF1 (SMCs)[20], and gastric intrinsic factor (GIF) (ZCs)[21]. Based on their expression patterns, mucinous AGCs resemble MNCs. The human antral mucosa (particularly the SMCs in it) is known to have a much higher turnover rate than the fundic mucosa[22]. The different proteins expressed by SMCs of the fundic and antral units, such as gastric lipase, TFF3, FCGBP and lysozyme, may be the basis of the different self-renewal rates and may further influence the spatial organization of the bacterial microbiota[23]. These cells originate by stepwise maturation from multipotent gastric stem cells (GSCs) and progenitor cells derived from GSCs such as pre-SMCs, pre-MNCs, pre-PCs and pre-AGCs residing in the isthmus of the gastric gland[16,24]. ZCs are generated by transdifferentiation of MNCs during their downward migration toward the base of the glands[25].
Subjected to countless daily injuries, the stomach still functions as a remarkably efficient digestive organ and microbial filter mainly because of its regeneration and repair. Rapid repair of superficial lesions occurs via a cell migration process called restitution, which starts within minutes. Continuous regeneration via differentiation and proliferation of stem cells and progenitor cells leads to self-renewal within days to months[22]. Pit cells are rapidly turned over after cell death, phagocytosed by a neighboring cell or extruded to the surface, and their half-life, which is regulated by Indian hedgehog and epidermal growth factor (EGF), is approximately 3 d[26,27]. The half-life of PCs and ZCs is several months. PCs are generated from GSC-derived pre-PCs, a process regulated by sonic hedgehog (SHH), gastrin and bone morphogenetic protein (BMP)[27]. In the past several years, strong evidence that ZCs differentiate from MNCs (a process that takes 14 d) has been reported, and the process is regulated by Mist1 and retinoic acid[16,28,29]. The degree of maturation correlates with the distance migrated from the GSCs. MNCs are located in the neck region, ZCs are located at the base, and intermediate pre-ZCs with characteristics of both MNCs and ZCs are located between the neck and the base region[25,30]. Transitional cells with coexpression of MUC6 and GIF are found in the normal gastric mucosa of mice[31]. Proper maturation of the MNC-zymogenic lineage is strictly dependent on PCs, perhaps via their functional secretion of SHH, BMP and amphiregulin[27]. Genetic ablation of PCs blocked the pattern of the entire zymogenic lineage: Progenitors showed premature expression of differentiated cell markers, and fully differentiated ZCs failed to develop, and these aberrancies may also correlate with a notable change in gastric unit architecture[32]. GSCs are characterized as undifferentiated granule-free and mitotic cells, and progenitor cells have a few granules or few microvilli[33]. The mesenchymal compartment surrounding the glands is less studied and poorly understood. It can be significantly affected by H. pylori infection and infiltrated by immune cells, including macrophages, neutrophils, regulatory T cells, natural killer cells and inflammatory mediators such as cytokines, chemokines and metalloproteinases, which may further contribute to epithelial–mesenchymal transition and carcinogenesis[34,35]. MSCs have multipotent potential to differentiate into various cell types and woundhealing ability, as well as tumorpromoting potential[36]. MSCs have immunoregulatory effects on macrophages and polarize them toward M2-like tumor-associated macrophages (TAMs). In turn, M2-TAMs modulate the transition of “naive” MSCs into tumor-derived MSCs, contributing to carcinogenesis by the induction of EMT process, metastasis, immune invasion and immunotherapy resistance of tumor cells[37,38].
GSCs can bidirectionally migrate and differentiate into various cell types after the apoptosis of mature cells[16]. The lateral expansion of GSC clones is impeded by the physical barrier of long-lived PCs. Only when PCs are lost can GSC clones expand laterally around the gland circumference, which may indicate the reversibility of atrophy in the appropriate setting[39,40]. GSCs or progenitor cells reside in the isthmus region within a “niche”, an area providing an optimal microenvironment to regulate physiological tissue renewal and injury repair. The ability of stromal niche cells to control and modify GSC dynamics constitutes a sophisticated mechanism that orchestrates epithelial regeneration and the maintenance of tissue integrity[41]. These cell populations include the villin+, Lgr5+, Axin2+ and CCKR2+ stem cells in the antrum, TFF2 mRNA+, Mist1+ cells and Troy+ or Lgr5+ mature ZCs in the corpus, and Sox2+, eR1+, Lrig1+, Bmi1+ cells in both the antrum and the corpus. These cells are the main suppliers of regenerated glands in response to injury and inflammation regulated by Wnt5a[42]. Villin promotor stem cells are normally quiescent, but multiply in response to IFN-γ, locate in the isthmus and can differentiate into all types of cells in the antral glands. Disruption of Klf4 in villin+ gastric progenitor cells promotes the formation and progression of GC[43]. Mouse gastric corpus gland epithelium is maintained by two stem cell populations: A rapidly cycling population in the isthmus region with a broad expression signature and a quiescent reserve population in the base, marked by expression of Troy or Lgr5[39]. Single adult Lgr5+ stem cells predominantly restricted to the base of mature pyloric glands build gastric organoids closely resembling pyloric gastric units in vitro. Neonate Lgr5+ stem cells located at the base of the prospective corpus and pyloric glands contribute to the development of mature gastric epithelium in both the pylorus and corpus regions[44]. Activation of Wnt signaling in these Lgr5+ cells can induce GC[44]. Lgr5 or Troy is also expressed at the gland base by mature ZCs, and these ZCs can be cultured to generate long-lived gastric organoids, displaying plasticity and an ability to replenish entire gastric units, essentially serving as quiescent “reserve” stem cells for gland regeneration after injury[45,46]. In this same zone, Axin2+/Lgr5− stem cells adjacent to Axin2+/Lgr5+ stem cells are highly proliferative and able to repopulate entire glands, including those of the base, upon the depletion of the Lgr5+ population, which can be regulated by stroma-derived R-spondin 3 produced by gastric myofibroblasts after H. pylori infection[41]. CCK2R+/Lgr5− stem cells in the antrum and are stimulated by gastrin through CCK2R to enhance antral gland fission and carcinogenesis[47]. The TFF2 mRNA-expressing cells above the neck region are the progenitors of the oxyntic mucosa but not of the pit or enterochromaffin-like (ECL) cell lineages in the corpus. SOX2-positive cells are found in the pylorus and corpus of the mice stomach and participate in normal regeneration[48]. Runx1 enhancer element (eR1) expression is present in the stomach corpus and pyloric gland, and eR1+ stem cells can generate organoids via Wnt signaling pathway-dependent WENR. Activation of eR1 induces foveolar hyperplasia and antralization. Lrig1+ cells give rise to gastric lineage epithelial cells in both the gastric corpus and antrum. The replacement of damaged gastric oxyntic glands occurs via the differentiation of Lrig1+ cells into normal gastric lineage cells after acute oxyntic atrophy in the gastric corpus rather than via transdifferentiation of chief cell lineages[49].
Different gastric lesions, such as chronic superficial/atrophic gastritis and gastric hyperplastic polyps, can be derived from their corresponding cells after injury caused by H. pylori infection, autoimmune gastritis, reactive or chemical stimulation, liver cirrhosis and portal hypertension[50,51]. Pathophysiologically, the stomach follows two patterns of adaptation after injury. The superficial response is a pattern whereby SMCs migrate and rapidly proliferate to repair erosions induced by acid or other irritants. Pit cells come from pre-pit cells arising in the isthmus region from undifferentiated granule-free cells through a pre-pit cell precursor stage and subsequently differentiate during their upward migration to the luminal surface, which takes approximately 3 days[52]. Metaplastic response [spasmolytic polypeptide-expressing metaplasia (SPEM) and IM] can follow gastric atrophy which is histologically characterized by the loss (atrophy) of acid-producing (oxyntic) PCs accompanied by invariable loss of mature ZCs when the portion of the gastric gland from the isthmus down to the base is damaged[53].
Chronic gastritis (CG) is an inflammatory condition of the gastric mucosa. H. pylori infection is the most common cause, especially of CAG[54], compared with other relatively common causes, including bile reflux, autoimmune disease, long-term use of nonsteroidal anti-inflammatory drugs and other drugs and ethanol intake. Globally, on average, more than half of people may have CG, with approximately 70%–90% having H. pylori infection[55,56]. According to the updated Sydney system classification of CG, CG can be divided into atrophic and non-atrophic gastritis (chronic superficial gastritis)[57]. H. pylori-induced chronic non-atrophic gastritis can progress to atrophic gastritis[58,59]. Atrophy of the gastric mucosa is defined as the decrease or disappearance of the original gastric glands, which may be replaced by SPEM/pseudopyloric metaplasia (PPM), pyloric metaplasia, IM or fibrosis[60]. Corpus gland atrophy is characterized by the loss of PCs leading to impaired gastric acid and intrinsic factor secretion (malabsorption of iron and vitamin B12 resulting in anemia)[61,62]. The diagnosis of corpus gland atrophy is mainly based on endoscopy findings, such as H. pylori gastritis and open- and closed-type gastritis, the findings of pathology assessment with histological staging systems (OLGA and OLGIM), and the findings of noninvasive methods, such as the combination of pepsinogens, gastrin-17 and anti-H. pylori antibody serum assays, serum ghrelin assays, volatile organic compound assays and gastric juice pH assays based on hypochlorhydric conditions)[63-65]. Under endoscopy, IM is the most reliable marker of atrophy. Patients with advanced stages of gastritis, that is, atrophy and/or IM affecting both the antral and corpus mucosa, should be considered at a high risk for GC[10]. High-definition endoscopy with chromoendoscopy (CE) and image-enhanced endoscopy (IEE) with ME, such as NBI with ME, are better than high-definition and conventional white-light endoscopy[10,66,67]. Artificial intelligence (AI) has also been applied to diagnose CAG based on different images. For example, convolutional neural network (CNN) models based on conventional white light images to diagnose CAG achieved more than 90% (93%-94.2%) higher accuracy than experts, as well as being able to distinguish H. pylori gastritis from autoimmune gastritis[68,69]. When differentiating CAG from GC, the accuracy, sensitivity and specificity of a CNN model based on ME-NBI images were 85.3%, 95.4% and 71.0%, respectively (0.02 s/image)[70]. CG can be found in the gastric antrum, predominantly in the gastric body, and the involvement of the entire stomach is seen on endoscopy. Mild, moderate or severe CAG can be diagnosed according to histopathological results. The OLGA system stages gastritis by combining the extent of atrophy scored histologically with the topography of atrophy identified through biopsy mapping. It is recommended that patients with advanced stages of CAG (including severe atrophic change, IM in both the antrum and corpus or OLGA/OLGIM III/IV disease) should be followed up with a high-quality endoscopy every 3 years, and those with autoimmune CAG should be followed up every three-five years[10,64,71]. For patients with mild to moderate atrophy restricted to the antrum, there is no evidence to recommend surveillance.
In patients with CAG, the annual incidence of GC is 0.1%. Within 1, 5 and 10 years of follow-up after initial diagnosis, GC is diagnosed in 0.3%, 0.6% and 0.8% of patients, respectively. The median interval between initial diagnosis and GC is 1.6 years[72]. In terms of reversibility, H. pylori eradication may contribute to the regression of CAG, although this is controversial[73]. In clinical research, significant differences in CAG between H. pylori-eradicated and H. pylori-negative groups disappeared at the 1-year follow-up[74]. In patients > 59 years old, atrophy was alleviated in both the 5th and 10th years, and patients ≤ 59 years old showed alleviation of atrophy in the 10th year[75]. Moreover, it has been reported that CAG can be improved after some drug treatments[76-78]. These results indicate the reversibility of CAG. Another clinical study showed that severe gastric atrophy persisted in the mucosa adjacent to the GC for a long time following H. pylori eradication, indicating the irreversibility of H. pylori-induced gastric atrophy[79]. CAG may continue for a long time and may even become severe, even after eradication[80]. In addition, the longer the follow-up, the greater the risk of developing diffuse-type GC became in patients who have mild-to-moderate gastric atrophy[80]. It is likely that slight atrophy is reversible after stimulus removal, whereas severe atrophy caused by long-term infection may not be readily reversed. Molecular alterations related to CAG are not common, especially mutations, and this is further evidence for reversibility. For instance, single-nucleotide polymorphisms (SNPs) have been studied, such as the C allele of TLR1 rs4833095 T/C and the IL10 gene promoter -819C/T (rs1800871) polymorphism related to the immune response, which might increase the risk of CAG and GC[81-83]. rs7521584 minor allele homozygosity and p53 gene mutation might be associated with the degree of gastric mucosal atrophy induced by H. pylori infection[84,85]. Gastric microbiota alteration is also a potential factor. Significant mucosal microbial dysbiosis was observed in gastric mucosal samples from patients with CAG, IM and dysplasia, including alterations of Fusobacterium, Neisseria, Prevotella, Veillonella, and Rothia, compared with the microbial environment in superficial gastritis, indicating the potential correlation of these alterations with disease progression[86].
Gland cells loss or dropout is followed by replacement with metaplastic cells coexpressing proteins, including TFF2 and MUC6 expressed by MNCs and pepsinogen expressed by mature ZCs, and is not affected by GSCs[87]. This metaplasia occurs because of dysregulated transdifferentiation of the mucous neck-ZC lineage and is termed as SPEM; it is inherent to the gastric corpus and has an unclear initiation mechanism (transdifferentiation is a process in which one differentiated cell type converts into a completely different cell type present in the tissue.)[88]. SPEM is often considered synonymous with PPM. PPM is a histological name, and SPEM is a molecular name[89]. However, pyloric and PPMs are not always coincident with SPEM in H. pylori gastritis and autoimmune gastritis, which may be because SPEM resembles MNC hyperplasia on histochemical staining and can occur with MNC hyperplasia[90,91]. SPEM can be identified in mice with chronic infection of H. pylori or autoimmune gastritis, and it also develops in mice immediately after acute epithelial injury, such as in response to drugs including DMP777, L-635 and high-dose tamoxifen. SPEM is characterized by abundant mucins in cells that are found below the isthmus region, which often expands to the gland base[92]. Tamoxifen/DMP777 can cause > 90% PCs loss, increased proliferation of stem/progenitor cells and reduced mutation and morphology change of ZCs, which is the characteristic of SPEM, without neoplastic transformation over 3–6 mo, and gastric histology returns to nearly normal status within 3 mo after withdrawing the drug[53,93]. Furthermore, in mice treated with PCs alone responding to apoptosis-inducing diphtheria toxin (DT)[94], > 90% of PCs were killed, and increased proliferation occurred in the isthmus and neck but not in the base, while ZCs maintained largely normal morphology with apical GIF granules[95]. In contrast with tamoxifen and DMP777, DT targeted at PCs has never caused substantial SPEM. SPEM develops in response to both acute injury and chronic inflammation. The emergence of SPEM can also be altered by endocrine or paracrine regulation. For example, mice with gastrin or histidine deficiency had accelerated development of SPEM after DMP777 administration compared with wild-type mice as well as attenuated EGF receptor signaling[96]. Thus, the emergence of SPEM is regulated by a complex coordinated mechanism including PC loss due to inflammation (not apoptosis), which may be accompanied by ZC loss, damage to other mucosal cell lineages and their cytokines and immune reactions. No factor has been found to be solely responsible for the emergence of SPEM.
SPEM is a regenerative lesion in gastric mucosa, and SPEM cells can redifferentiate into ZCs following recovery from injury. As a mucous-secreting reparative lineage, SPEM cells arise in the setting of acute injury or ulceration. SPEM around ulcers contributes to the healing of these lesions[89]. During chronic inflammation, such as that induced by H. pylori infection, SPEM glands can connect to allow deeper penetration of H. pylori and expansion of its intragastric niche[97]. Heterogeneity in mouse SPEM cell lineages has been identified, and chronic inflammation can lead to the further evolution of goblet-cell IM, which shows varying levels of intestinalization-related transcripts, including TFF3, MAL2, CFTR and MUC4[98]. In addition, inflammation is necessary for SPEM to progress directly to dysplasia induced by H. pylori infection without the development of phenotypic IM[99,100]. Inflammation is also considered a potential precursor to IM and GC in a chronic inflammatory setting[99]. Both SPEM and IM are associated with GC.
IM, an adaptive response to chronic injury, generates epithelium in the stomach that resembles small intestinal epithelium with or without a brush border characterized by the presence of intestinal goblet cells labeled by MUC2 and TFF3. The expression of MUC2 in IM was found to be higher in GC of earlier stages and was correlated with lower tumor depth of invasion and a lower rate of lymph node metastasis, and these features are considered reliable markers of IM[101-103]. Foveolar hyperplasia, SPEM and IM are histological changes observed in atrophic gastritis, and the lesions express TFF1, TFF2, and TFF3, respectively. TFF3 can easily form a disulfide-linked heterodimer with FCGBP (TFF3–FCGBP), as both TFF3 and FCGBP are secreted from intestinal goblet cells. TFF3 expression seems to be dependent on the STAT1/3 signaling induced by IL-6 during inflammation. The TFF3–FCGBP interaction is likely part of the innate immune defense of gastric mucous, defensing microorganisms and promoting mucosal wound healing in mice and humans[104-106]. Serum level of TFF3 was found to be a potential noninvasive marker of GC, and the use of TFF3 serum levels combined with pepsinogen could improve GC screening[107,108]. In addition, only the serum TFF3 Level was stable and not significantly affected by H. pylori eradication[109]. GC patients with negative TFF3 expression exhibited longer survival than the positive TFF3 expression group. TFF3 was also demonstrated to be an independent prognostic indicator of recurrence and overall survival in GC[110]. Caudal-related homeobox 1 (CDX1) and CDX2 are intestine-specific transcription factors strictly confined to the gut, expressed from the duodenum to the rectum. Expression of nuclear CDX1 and CDX2 has been noted in human IM and is involved in the progression to dysplasia and GC[111]. CDX1 is predominantly expressed in the undifferentiated cells of the intestinal crypts, whereas CDX2 is mostly present in the villi or differentiated cell compartment of the small intestine[112]. Differences in differentiation, structure, and proliferation between IM induced by CDX1 vs CDX2 have also been found. CDX1 may play a role in the transdifferentiation of the mucosa into an intestinal type. The maintenance of intestinal differentiation may depend on CDX2[113]. CDX1 expression can be transcriptionally activated by nuclear factor-kappaB (NF-κB) signaling after direct binding to the unmethylated promoter. In normal gastric mucosa, CDX1 is not expressed due to high levels of CDX1 promoter methylation and the absence of inflammation. The methylation level of the CDX1 promoter decreases during H. pylori infection and IM and reaches the lowest level in low-grade intraepithelial neoplasia[114]. In H. pylori infection, the contribution of CDX2 to IM is regulated by the NOD1-mediated innate immune response to bacterial infection. In vivo, prolonged infection of NOD1-deficient mice with H. pylori led to increased CDX2 expression and IM with increased nuclear expression of the NF-κB p65 subunit and decreased expression of TRAF3[115]. Eradication of H. pylori did not show beneficial effects on aberrant CDX1/CDX2 expression. Reversal of IM may be associated with a decrease in CDX2 mRNA expression[116]. CDX2 activation in IM can be driven by the reflux of bile acids via the FXR/NF-κB signaling pathway and can be increased by microRNA (microRNA-92a-1–5p) targeting FOXD1[117]. SOX2 is a member of the high-mobility group domain proteins and has been identified as an adult stem cell marker. SOX2 can negatively regulate the CDX2 promoter. It was associated with gastric differentiation in incomplete IM and lost in the progression to dysplasia, whereas CDX2 was acquired de novo in IM and maintained in dysplasia[118].
Factors affecting gene expression, including mutations, DNA methylation and SNPs, as well as epigenetic factors, including microRNAs, long noncoding RNAs and mRNAs, have been associated with IM and have a potential role in screening, treatment and prognostic purposes[119]. IM patients with shortened telomeres and chromosomal alterations were likely to develop subsequent dysplasia or GC, whereas patients exhibiting normal epigenetic patterns were likely to experience regression. IM in patients with intermediate levels of DNA methylation changes tended to regress, while IM in patients with high levels of DNA methylation changes tended to persist/progress, indicating that levels of aberrant DNA methylation might influence the “point of no return”[120]. Further heterogeneous levels of DNA methylation were found in isolated metaplastic gland samples and isolated nonmetaplastic gland samples from the same IM mucosa. DNA methylation of mir34-b/c was found to be common in isolated cancer and IM glands. The mir34-b/c gene methylation status among isolated samples of IMs and isolated non-IM glands had an impact on IM development[121]. SNP analysis showed a negative association between the minor allele C of TLR4 rs11536889 and the progression of IM[122].
IM may arise from SPEM, mentioned above, or perhaps directly from ZCs[123] or gastric isthmus GSCs[124]. Elucidating the origin of gastric IM is difficult because H. pylori infection in mice does not result in IM. It has been demonstrated that IM can be mostly surrounded by SPEM foci and developed subsequently to SPEM with the SPEM- and MUC2-positive goblet cells during the course of H. pylori infection in Mongolian gerbils[125]. Dual TFF2 and TFF3 positivity was seen in about 50% of the foci of IM and in about 33% of SPEM samples adjacent to GC. The expression patterns of TFFs and MUCs may indicate that IM evolves from SPEM[126]. SPEM was found to originate from ZCs in mice, and cells redifferentiated into ZCs upon injury resolution; in this process, activation of Ras may promote metaplasia and inhibition of Ras signaling may reverse metaplasia. The acquisition of genetic/epigenetic mutations in long-lived stem cells may leads to GC and precancerous lesions such as metaplasia and dysplasia[42]. For example, it was demonstrated that short-term SPEM might arise from neck progenitors rather than transdifferentiated mature ZCs, and long-term SPEM might originate from isthmus progenitors[127]. A downward migration of the stem cell zone toward the base to form SPEM was shown in one study, and depleting Lgr5+ ZCs did not impair metaplasia development, indicating that Mist1+ isthmus cells, rather than Mist1+ ZCs, were the origin[124,127]. Therefore, the origin of gastric IM is presently under debate.
Gastric IM can be classified into complete and incomplete types on H&E-stained sections. Types I, II and III are classified based on the type of secretory mucins identified by the special stains Alcian blue pH 2.5 (AB)/periodic acid-Schiff (PAS) and high iron diamine/AB. Type I corresponds to complete IM, and types II and III are subclassifications of incomplete IM[128,129]. The pooled prevalence of IM, a precancerous condition, was 4.8%; the pooled incidence rate for the progression of IM to GC in the absence of dysplasia was 12.4 per 10000 person-years; the median time to progression to GC from IM was estimated to be 6.1 years[130]; and the pooled global regression rate of IM to normal mucosa or non-atrophic gastritis at 1 year, 3 years, 5 years, and 10 years was 29.7%, 19.4%, 25.9% and 19.4%, respectively[129]. However, IM reversibility is still controversial. IM in the corpus was most likely to progress to more than one location[131]. Incomplete type, extensive IM and a first-degree relative with GC have been shown to be higher risk factors (carrying a more than 2-fold increased risk for GC) than complete type, limited IM and no family history. Therefore, the AGA recommends patients with IM specifically at higher risk of GC (those with incomplete IM, extensive IM or a family history) and/or who are at overall increased risk for GC (racial/ethnic minorities, immigrants from regions with high GC incidence, or individuals with a first-degree relative with GC) may reasonably choose repeat endoscopy within 1 year for the risk stratification[11]. European guidelines recommend that endoscopic surveillance with CE and guided biopsies within 3 years may be considered in patients with IM at a single location with a family history of GC, incomplete IM or persistent H. pylori gastritis[10]. British guidelines recommend that patients with IM should undergo endoscopy for no less than 7 min with photographic documentation of gastric regions, including location and extent and pathology, and recommend endoscopic surveillance every 3 years for patients with extensive IM, a strong family history or persistent H. pylori infection. IEE is recommended to accurately detect and risk-stratify IM. Endoscopic grading is documented as distal gastric (antrum or incisura—low risk) or proximal gastric (corpus—high risk). Biopsies are directed at mucosa within Sydney protocol areas where enhanced imaging discloses IM[132]. In addition, AI, especially the deep CNN system, has been introduced into research to aid real-time diagnosis of IM based on IEE images and has achieved acceptable results[133,134]. For example, the accuracy of an AI model for diagnosing IM was between 0.86 and 0.91, similar to expert's accuracy for detecting IM (0.89 vs 0.82), and was superior to that of nonexperts for detecting IM (0.74 vs 0.82)[133]. Although IM has been considered a point of no return, H. pylori eradication can achieve the most benefit before the development of precancerous lesions, including IM and CAG. There are also some studies indicating that IM may be reversible, and the most common treatment is eradication of H. pylori to reverse IM. For example, in one study, IM in the antrum and corpus improved significantly in the H. pylori-eradicated group. A significant difference in IM between the H. pylori-eradicated and H. pylori-negative groups disappeared at ≥ 5 years of follow-up in the antrum and at 3 years of follow-up in the corpus[74]. Chronic celecoxib users had a higher regression rate of IM after eradication of H. pylori[135]. Resveratrol can reduce bile acid-induced IM through the PI3K/AKT/p-FoxO4 signaling pathway and has a potential reversing effect on IM, especially that caused by bile acid reflux[136].
Both foveolar hyperplasia and gastric hyperplastic polyps are the expansion of normal foveolar/pit cells. A hyperproliferative response to tissue injury such as erosions and ulcers accompanied by increased cellular exfoliation results in the histopathological appearance of foveolar hyperplasia. They commonly arise from the background mucosa containing chronic active or reactive inflammation caused by H. pylori infection, liver cirrhosis and portal hypertension, autoimmune gastritis and reactive or chemical stimulation (e.g., bile reflux or NSAIDs and gastric stump), etc.[137]. The hyperplasia originated from pre-pit/progenitor cells in isthmus[138]. Hyperplastic polyps consist of elongated, grossly distorted, branching and dilated hyperplastic foveola lying in an edematous stroma rich in vasculature. Smooth muscle fibers may also be apparent in the lamina propria[139]. Although glands are usually not involved in the formation of polyps, they may contain pyloric glands, ZCs and PCs[140]. Both the epithelium and mesenchymal stromal cells can show marked regenerative changes and contain varying degrees of chronic and active inflammation[139]. Hyperplastic polyps represent 30%–93% of all gastric epithelial polyps and rarely undergo neoplastic progression, but are associated with an increased risk of synchronous cancer occurring elsewhere in gastric mucosa[141]. The rate of dysplasia arising in hyperplastic polyps was reported from 1.9% to 19% and the rate of GC was from 0.6% to 2.1%[142]. Molecular alterations have also been studied including expression of p53, K-ras, microsatellite instability, p21WAF1/CIP1 and cyclin D1 Levels, involving in the process of neoplastic transformation, which still remain controversial[143].
Endoscopically, they are found most frequently in the antrum and are often multiple between 0.5 and 1.5 cm in diameter. Size larger than 1 cm has been considered as a risk factor of malignant transformation. The larger a GHP is, the more likely it is to become cancerous, as its continuously increasing volume indicates the persistence of hyperplasia and inflammatory stimulating factors. One carcinogenesis process is intestinal type: Persistent inflammation can increase the damage of the proper gastric glands followed by atrophy, IM, dysplasia and adenocarcinoma. The other is gastric type: The metaplasia of foveal epithelium occurs and resists the repeated inflammatory stimulation. It is tall columnar cells resembling foveolar cells, further developing to dysplasia and gastric type adenocarcinoma[143]. On the management, hyperplastic polyps should be biopsied and an examination of the whole stomach should be made for mucosal abnormalities and biopsied abnormalities[144]. Test for H. pylori and eradicate it when present, as it is the most common cause. One meta-analysis showed that after eradicating H. pylori, most GHPs were eliminated, and the GHP elimination rate was increased by more than 20 times than that in the control group[145]. In view of the potential neoplastic transformation risk, hyperplastic polyps larger than 10 mm should be resected completely[144]. However, there is a controversial issue on the recurrence and neoplastic transformation after endoscopic resection, even R0 resection[137]. When it does not harbor foci of dysplasia and/or carcinoma, whether R0 resection has little impact on recurrence, as inflammatory hyperplasia foveolar cells are not able to divide and proliferate themselves[137]. Similarly, either ESD or EMR resection of a GHP may have little effect on recurrence. How about the residual inflammatory hyperplasia foveolar cells? As the resection deep is at least mucosa, it means proper gastric glands in the lamina propria will be removed together, further losing the regeneration of pit and gland epithelium and being followed by scar formation/fibrosis. The residual cells can initially derive from the removed glands or adjacent glands. If they are from the removed glands, there is no chance of recurrence. However, if they are from adjacent glands, endoscopic resection will increase the rate of recurrence when the background mucosa contains chronic active or reactive inflammation. If there is free of chronic active/reactive inflammation, the residual cells from adjacent glands will die from necrosis/apoptosis, or they continue the inflammatory hyperplasia and recover after the recession of the acute inflammation induced by resection. It can be explained by ESD removing early GC after eradication of H. pylori, in which rare GHP can be found during surveillance, as the background mucosa is commonly chronic atrophy instead of active inflammation and IM instead of foveolar cells[146,147]. However, if the background mucosa contains atrophy and IM with chronic active/reactive inflammation, the possibility of neoplastic transformation will increase derived from the residual cells. When a GHP harbors foci of dysplasia and/or carcinoma, R0 resection will be pivotal to prevent recurrence, as these cells have already contained the potential for malignant proliferation themselves, no matter whether there is a new origin of neoplasms. We can see the “recurrence” is actually from adjacent glands in the background mucosa with chronic active/reactive inflammation. The background mucosa where GHPs derive is one of determinants. Eliminating the common causes should be applied at the same time as resection when a GHP is more than 10 mm which will reduce the recurrence rate and bring benefits for patients to a large extent better than being in the dilemma (whether resection or not)[148,149] (Figure 1).
Reducing the rate of GC and increasing endoscopic eradication therapy have always been core goals of GC management. Timely and effective detection and surveillance of precancerous conditions can facilitate early detection and treatment of GC in the early stage and even prevent the occurrence of GC. We provided a detailed overview of gastric epithelium organization and its renewal and reviewed precancerous conditions, including CAG, SPEM, IM, foveolar hyperplasia and GHPs derived from gastric epithelium, based on a histological perspective, covering their epidemiology, clinical management and advances, histological structures, causes, and potential origins and reversibility. Regarding the origin, process and reversibility, they are the mainly controversial parts, such as whether CAG and IM are reversible and what the point of no return is, whether IM derives from SPEM or which cells are the origin of IM and what the association is between R0 resection and recurrence and neoplastic transformation of gastric hyperplastic polyps. We discussed these issues in detail based on a review of almost all related articles. More clinical and basic research on the molecular alterations of these gastric lesions may shed light on the controversies in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Batyrbekov K, Mohamed SY S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55774] [Article Influence: 7967.7] [Reference Citation Analysis (132)] |
| 2. | Poorolajal J, Moradi L, Mohammadi Y, Cheraghi Z, Gohari-Ensaf F. Risk factors for stomach cancer: a systematic review and meta-analysis. Epidemiol Health. 2020;42:e2020004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 180] [Cited by in RCA: 166] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 3. | Lagergren J, Andersson G, Talbäck M, Drefahl S, Bihagen E, Härkönen J, Feychting M, Ljung R. Marital status, education, and income in relation to the risk of esophageal and gastric cancer by histological type and site. Cancer. 2016;122:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Thrift AP, El-Serag HB. Burden of Gastric Cancer. Clin Gastroenterol Hepatol. 2020;18:534-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 977] [Article Influence: 195.4] [Reference Citation Analysis (1)] |
| 5. | Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, Bonaventure A, Valkov M, Johnson CJ, Estève J, Ogunbiyi OJ, Azevedo E Silva G, Chen WQ, Eser S, Engholm G, Stiller CA, Monnereau A, Woods RR, Visser O, Lim GH, Aitken J, Weir HK, Coleman MP; CONCORD Working Group. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2711] [Cited by in RCA: 3408] [Article Influence: 486.9] [Reference Citation Analysis (1)] |
| 6. | Suh YS, Lee J, Woo H, Shin D, Kong SH, Lee HJ, Shin A, Yang HK. National cancer screening program for gastric cancer in Korea: Nationwide treatment benefit and cost. Cancer. 2020;126:1929-1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 7. | Huang HL, Leung CY, Saito E, Katanoda K, Hur C, Kong CY, Nomura S, Shibuya K. Effect and cost-effectiveness of national gastric cancer screening in Japan: a microsimulation modeling study. BMC Med. 2020;18:257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 8. | Noh CK, Lee E, Lee GH, Kang JK, Lim SG, Park B, Park JB, Shin SJ, Cheong JY, Kim JH, Lee KM. Association of Intensive Endoscopic Screening Burden With Gastric Cancer Detection. JAMA Netw Open. 2021;4:e2032542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Shen L, Shan YS, Hu HM, Price TJ, Sirohi B, Yeh KH, Yang YH, Sano T, Yang HK, Zhang X, Park SR, Fujii M, Kang YK, Chen LT. Management of gastric cancer in Asia: resource-stratified guidelines. Lancet Oncol. 2013;14:e535-e547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 382] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 10. | Pimentel-Nunes P, Libânio D, Marcos-Pinto R, Areia M, Leja M, Esposito G, Garrido M, Kikuste I, Megraud F, Matysiak-Budnik T, Annibale B, Dumonceau JM, Barros R, Fléjou JF, Carneiro F, van Hooft JE, Kuipers EJ, Dinis-Ribeiro M. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy. 2019;51:365-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 712] [Cited by in RCA: 670] [Article Influence: 111.7] [Reference Citation Analysis (0)] |
| 11. | Gupta S, Li D, El Serag HB, Davitkov P, Altayar O, Sultan S, Falck-Ytter Y, Mustafa RA. AGA Clinical Practice Guidelines on Management of Gastric Intestinal Metaplasia. Gastroenterology. 2020;158:693-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 209] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 12. | Yang H, Hu B. Diagnosis of Helicobacter pylori Infection and Recent Advances. Diagnostics (Basel). 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Beresniak A, Malfertheiner P, Franceschi F, Liebaert F, Salhi H, Gisbert JP. Helicobacter pylori "Test-and-Treat" strategy with urea breath test: A cost-effective strategy for the management of dyspepsia and the prevention of ulcer and gastric cancer in Spain-Results of the Hp-Breath initiative. Helicobacter. 2020;25:e12693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Malfertheiner P, Megraud F, O'Morain CA, Gisbert JP, Kuipers EJ, Axon AT, Bazzoli F, Gasbarrini A, Atherton J, Graham DY, Hunt R, Moayyedi P, Rokkas T, Rugge M, Selgrad M, Suerbaum S, Sugano K, El-Omar EM; European Helicobacter and Microbiota Study Group and Consensus panel. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut. 2017;66:6-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2220] [Cited by in RCA: 1983] [Article Influence: 247.9] [Reference Citation Analysis (1)] |
| 15. | Walecka-Kapica E, Knopik-Dabrowicz A, Klupińska G, Chojnacki J. Ocena stezenia metabolitów tlenku azotu w soku zoładkowym u zakazonych Helicobacter pylori z uwzglednieniem stopnia zmian zapalnych w błonie sluzowej zoładka [The assessment of nitric oxide metabolites in gastric juice in Helicobacter pylori infected subjects in compliance with grade of inflammatory lesions in gastric mucosa]. Pol Merkur Lekarski. 2008;24:95-100. [PubMed] |
| 16. | Hoffmann W. Self-renewal of the gastric epithelium from stem and progenitor cells. Front Biosci (Schol Ed). 2013;5:720-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | McCracken KW, Catá EM, Crawford CM, Sinagoga KL, Schumacher M, Rockich BE, Tsai YH, Mayhew CN, Spence JR, Zavros Y, Wells JM. Modelling human development and disease in pluripotent stem-cell-derived gastric organoids. Nature. 2014;516:400-404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 649] [Cited by in RCA: 717] [Article Influence: 65.2] [Reference Citation Analysis (0)] |
| 18. | Spicer Z, Miller ML, Andringa A, Riddle TM, Duffy JJ, Doetschman T, Shull GE. Stomachs of mice lacking the gastric H,K-ATPase alpha -subunit have achlorhydria, abnormal parietal cells, and ciliated metaplasia. J Biol Chem. 2000;275:21555-21565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 132] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Hanisch FG, Ragge H, Kalinski T, Meyer F, Kalbacher H, Hoffmann W. Human gastric TFF2 peptide contains an N-linked fucosylated N,N'-diacetyllactosediamine (LacdiNAc) oligosaccharide. Glycobiology. 2013;23:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Ruchaud-Sparagano MH, Westley BR, May FE. The trefoil protein TFF1 is bound to MUC5AC in human gastric mucosa. Cell Mol Life Sci. 2004;61:1946-1954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Todisco A, Mao M, Keeley TM, Ye W, Samuelson LC, Eaton KA. Regulation of gastric epithelial cell homeostasis by gastrin and bone morphogenetic protein signaling. Physiol Rep. 2015;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Hoffmann W. Regeneration of the gastric mucosa and its glands from stem cells. Curr Med Chem. 2008;15:3133-3144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 23. | Kouznetsova I, Kalinski T, Meyer F, Hoffmann W. Self-renewal of the human gastric epithelium: new insights from expression profiling using laser microdissection. Mol Biosyst. 2011;7:1105-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Karam SM. Mouse models demonstrating the role of stem/progenitor cells in gastric carcinogenesis. Front Biosci (Landmark Ed). 2010;15:595-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Karam SM, Straiton T, Hassan WM, Leblond CP. Defining epithelial cell progenitors in the human oxyntic mucosa. Stem Cells. 2003;21:322-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 101] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 26. | Mimuro H, Suzuki T, Nagai S, Rieder G, Suzuki M, Nagai T, Fujita Y, Nagamatsu K, Ishijima N, Koyasu S, Haas R, Sasakawa C. Helicobacter pylori dampens gut epithelial self-renewal by inhibiting apoptosis, a bacterial strategy to enhance colonization of the stomach. Cell Host Microbe. 2007;2:250-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 170] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 27. | Han ME, Oh SO. Gastric stem cells and gastric cancer stem cells. Anat Cell Biol. 2013;46:8-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Tian X, Jin RU, Bredemeyer AJ, Oates EJ, Błazewska KM, McKenna CE, Mills JC. RAB26 and RAB3D are direct transcriptional targets of MIST1 that regulate exocrine granule maturation. Mol Cell Biol. 2010;30:1269-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | Karam SM, John R, Alpers DH, Ponery AS. Retinoic acid stimulates the dynamics of mouse gastric epithelial progenitors. Stem Cells. 2005;23:433-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Gómez-Santos L, Alonso E, Díaz-Flores L, Madrid JF, Sáez FJ. Transdifferentiation of mucous neck cells into chief cells in fundic gastric glands shown by GNA lectin histochemistry. Tissue Cell. 2017;49:746-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Goldenring JR, Nam KT, Mills JC. The origin of pre-neoplastic metaplasia in the stomach: chief cells emerge from the Mist. Exp Cell Res. 2011;317:2759-2764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 32. | Bredemeyer AJ, Geahlen JH, Weis VG, Huh WJ, Zinselmeyer BH, Srivatsan S, Miller MJ, Shaw AS, Mills JC. The gastric epithelial progenitor cell niche and differentiation of the zymogenic (chief) cell lineage. Dev Biol. 2009;325:211-224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 33. | Karam SM, Leblond CP. Dynamics of epithelial cells in the corpus of the mouse stomach. I. Identification of proliferative cell types and pinpointing of the stem cell. Anat Rec. 1993;236:259-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 284] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 34. | Baj J, Korona-Głowniak I, Forma A, Maani A, Sitarz E, Rahnama-Hezavah M, Radzikowska E, Portincasa P. Mechanisms of the Epithelial-Mesenchymal Transition and Tumor Microenvironment in Helicobacter pylori-Induced Gastric Cancer. Cells. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 35. | Suarez-Carmona M, Lesage J, Cataldo D, Gilles C. EMT and inflammation: inseparable actors of cancer progression. Mol Oncol. 2017;11:805-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 420] [Article Influence: 52.5] [Reference Citation Analysis (0)] |
| 36. | Liang W, Chen X, Zhang S, Fang J, Chen M, Xu Y. Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines. Cell Mol Biol Lett. 2021;26:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 119] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 37. | Zheng P, Li W. Crosstalk Between Mesenchymal Stromal Cells and Tumor-Associated Macrophages in Gastric Cancer. Front Oncol. 2020;10:571516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 38. | Li W, Zhang X, Wu F, Zhou Y, Bao Z, Li H, Zheng P, Zhao S. Gastric cancer-derived mesenchymal stromal cells trigger M2 macrophage polarization that promotes metastasis and EMT in gastric cancer. Cell Death Dis. 2019;10:918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 196] [Cited by in RCA: 239] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 39. | Han S, Fink J, Jörg DJ, Lee E, Yum MK, Chatzeli L, Merker SR, Josserand M, Trendafilova T, Andersson-Rolf A, Dabrowska C, Kim H, Naumann R, Lee JH, Sasaki N, Mort RL, Basak O, Clevers H, Stange DE, Philpott A, Kim JK, Simons BD, Koo BK. Defining the Identity and Dynamics of Adult Gastric Isthmus Stem Cells. Cell Stem Cell. 2019;25:342-356.e7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 40. | Nomura S, Esumi H, Job C, Tan SS. Lineage and clonal development of gastric glands. Dev Biol. 1998;204:124-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 41. | Sigal M, Logan CY, Kapalczynska M, Mollenkopf HJ, Berger H, Wiedenmann B, Nusse R, Amieva MR, Meyer TF. Stromal R-spondin orchestrates gastric epithelial stem cells and gland homeostasis. Nature. 2017;548:451-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 157] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 42. | Hayakawa Y, Ariyama H, Stancikova J, Sakitani K, Asfaha S, Renz BW, Dubeykovskaya ZA, Shibata W, Wang H, Westphalen CB, Chen X, Takemoto Y, Kim W, Khurana SS, Tailor Y, Nagar K, Tomita H, Hara A, Sepulveda AR, Setlik W, Gershon MD, Saha S, Ding L, Shen Z, Fox JG, Friedman RA, Konieczny SF, Worthley DL, Korinek V, Wang TC. Mist1 Expressing Gastric Stem Cells Maintain the Normal and Neoplastic Gastric Epithelium and Are Supported by a Perivascular Stem Cell Niche. Cancer Cell. 2015;28:800-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 252] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 43. | Yu T, Chen X, Lin T, Liu J, Li M, Zhang W, Xu X, Zhao W, Liu M, Napier DL, Wang C, Evers BM, Liu C. KLF4 deletion alters gastric cell lineage and induces MUC2 expression. Cell Death Dis. 2016;7:e2255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 44. | Barker N, Huch M, Kujala P, van de Wetering M, Snippert HJ, van Es JH, Sato T, Stange DE, Begthel H, van den Born M, Danenberg E, van den Brink S, Korving J, Abo A, Peters PJ, Wright N, Poulsom R, Clevers H. Lgr5(+ve) stem cells drive self-renewal in the stomach and build long-lived gastric units in vitro. Cell Stem Cell. 2010;6:25-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1056] [Cited by in RCA: 1194] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 45. | Stange DE, Koo BK, Huch M, Sibbel G, Basak O, Lyubimova A, Kujala P, Bartfeld S, Koster J, Geahlen JH, Peters PJ, van Es JH, van de Wetering M, Mills JC, Clevers H. Differentiated Troy+ chief cells act as reserve stem cells to generate all lineages of the stomach epithelium. Cell. 2013;155:357-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 419] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 46. | Leushacke M, Tan SH, Wong A, Swathi Y, Hajamohideen A, Tan LT, Goh J, Wong E, Denil SLIJ, Murakami K, Barker N. Lgr5-expressing chief cells drive epithelial regeneration and cancer in the oxyntic stomach. Nat Cell Biol. 2017;19:774-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 196] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 47. | Hayakawa Y, Chang W, Jin G, Wang TC. Gastrin and upper GI cancers. Curr Opin Pharmacol. 2016;31:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 48. | Arnold K, Sarkar A, Yram MA, Polo JM, Bronson R, Sengupta S, Seandel M, Geijsen N, Hochedlinger K. Sox2(+) adult stem and progenitor cells are important for tissue regeneration and survival of mice. Cell Stem Cell. 2011;9:317-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 627] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 49. | Schweiger PJ, Clement DL, Page ME, Schepeler T, Zou X, Sirokmány G, Watt FM, Jensen KB. Lrig1 marks a population of gastric epithelial cells capable of long-term tissue maintenance and growth in vitro. Sci Rep. 2018;8:15255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 50. | Lenti MV, Rugge M, Lahner E, Miceli E, Toh BH, Genta RM, De Block C, Hershko C, Di Sabatino A. Autoimmune gastritis. Nat Rev Dis Primers. 2020;6:56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 209] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 51. | Ansari S, Yamaoka Y. Helicobacter pylori Virulence Factors Exploiting Gastric Colonization and its Pathogenicity. Toxins (Basel). 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 189] [Cited by in RCA: 166] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 52. | Karam SM, Leblond CP. Dynamics of epithelial cells in the corpus of the mouse stomach. II. Outward migration of pit cells. Anat Rec. 1993;236:280-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 136] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 53. | Goldenring JR, Nam KT. Oxyntic atrophy, metaplasia, and gastric cancer. Prog Mol Biol Transl Sci. 2010;96:117-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 54. | Tan VP, Wong BC. Helicobacter pylori and gastritis: Untangling a complex relationship 27 years on. J Gastroenterol Hepatol. 2011;26 Suppl 1:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 55. | Sipponen P, Maaroos HI. Chronic gastritis. Scand J Gastroenterol. 2015;50:657-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 187] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 56. | Fang JY, Du YQ, Liu WZ, Ren JL, Li YQ, Chen XY, Lv NH, Chen YX, Lv B; Chinese Society of Gastroenterology, Chinese Medical Association. Chinese consensus on chronic gastritis (2017, Shanghai). J Dig Dis. 2018;19:182-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 57. | Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol. 1996;20:1161-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3221] [Cited by in RCA: 3550] [Article Influence: 122.4] [Reference Citation Analysis (3)] |
| 58. | Matysiak-Budnik T, Mégraud F. Helicobacter pylori infection and gastric cancer. Eur J Cancer. 2006;42:708-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 59. | Kim YJ, Lee SY, Yang H, Kim JH, Sung IK, Park HS. [Nodular Gastritis as a Precursor Lesion of Atrophic and Metaplastic Gastritis]. Korean J Gastroenterol. 2019;73:332-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 60. | Rugge M, Correa P, Dixon MF, Fiocca R, Hattori T, Lechago J, Leandro G, Price AB, Sipponen P, Solcia E, Watanabe H, Genta RM. Gastric mucosal atrophy: interobserver consistency using new criteria for classification and grading. Aliment Pharmacol Ther. 2002;16:1249-1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 265] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 61. | Neumann WL, Coss E, Rugge M, Genta RM. Autoimmune atrophic gastritis--pathogenesis, pathology and management. Nat Rev Gastroenterol Hepatol. 2013;10:529-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 283] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 62. | Varbanova M, Frauenschläger K, Malfertheiner P. Chronic gastritis - an update. Best Pract Res Clin Gastroenterol. 2014;28:1031-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 63. | Lahner E, Conti L, Annibale B, Corleto VD. Current Perspectives in Atrophic Gastritis. Curr Gastroenterol Rep. 2020;22:38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 64. | Lahner E, Zagari RM, Zullo A, Di Sabatino A, Meggio A, Cesaro P, Lenti MV, Annibale B, Corazza GR. Chronic atrophic gastritis: Natural history, diagnosis and therapeutic management. A position paper by the Italian Society of Hospital Gastroenterologists and Digestive Endoscopists [AIGO], the Italian Society of Digestive Endoscopy [SIED], the Italian Society of Gastroenterology [SIGE], and the Italian Society of Internal Medicine [SIMI]. Dig Liver Dis. 2019;51:1621-1632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 126] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 65. | Cazzato M, Esposito G, Galli G, Pilozzi E, Lahner E, Corleto VD, Zullo A, Di Giulio E, Annibale B. Diagnostic Accuracy of EndoFaster® and Narrow-Band Imaging Endoscopy in Patients with Impaired Gastric Acid Secretion: A Real-Time Prospective Study. Gastroenterol Res Pract. 2021;2021:6616334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 66. | Botezatu A, Bodrug N. Chronic atrophic gastritis: an update on diagnosis. Med Pharm Rep. 2021;94:7-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 67. | Liu T, Zheng H, Gong W, Chen C, Jiang B. The accuracy of confocal laser endomicroscopy, narrow band imaging, and chromoendoscopy for the detection of atrophic gastritis. J Clin Gastroenterol. 2015;49:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 68. | Zhang Y, Li F, Yuan F, Zhang K, Huo L, Dong Z, Lang Y, Zhang Y, Wang M, Gao Z, Qin Z, Shen L. Diagnosing chronic atrophic gastritis by gastroscopy using artificial intelligence. Dig Liver Dis. 2020;52:566-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 69. | Franklin MM, Schultz FA, Tafoya MA, Kerwin AA, Broehm CJ, Fischer EG, Gullapalli RR, Clark DP, Hanson JA, Martin DR. A Deep Learning Convolutional Neural Network Can Differentiate Between Helicobacter Pylori Gastritis and Autoimmune Gastritis With Results Comparable to Gastrointestinal Pathologists. Arch Pathol Lab Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 70. | Horiuchi Y, Aoyama K, Tokai Y, Hirasawa T, Yoshimizu S, Ishiyama A, Yoshio T, Tsuchida T, Fujisaki J, Tada T. Convolutional Neural Network for Differentiating Gastric Cancer from Gastritis Using Magnified Endoscopy with Narrow Band Imaging. Dig Dis Sci. 2020;65:1355-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (1)] |
| 71. | Massironi S, Zilli A, Elvevi A, Invernizzi P. The changing face of chronic autoimmune atrophic gastritis: an updated comprehensive perspective. Autoimmun Rev. 2019;18:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 72. | de Vries AC, van Grieken NC, Looman CW, Casparie MK, de Vries E, Meijer GA, Kuipers EJ. Gastric cancer risk in patients with premalignant gastric lesions: a nationwide cohort study in the Netherlands. Gastroenterology. 2008;134:945-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 585] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 73. | Malfertheiner P. Gastric atrophy reversible or irreversible after Helicobacter pylori eradication - an open question. Digestion. 2011;83:250-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 74. | Hwang YJ, Kim N, Lee HS, Lee JB, Choi YJ, Yoon H, Shin CM, Park YS, Lee DH. Reversibility of atrophic gastritis and intestinal metaplasia after Helicobacter pylori eradication - a prospective study for up to 10 years. Aliment Pharmacol Ther. 2018;47:380-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 132] [Article Influence: 18.9] [Reference Citation Analysis (1)] |
| 75. | Toyokawa T, Suwaki K, Miyake Y, Nakatsu M, Ando M. Eradication of Helicobacter pylori infection improved gastric mucosal atrophy and prevented progression of intestinal metaplasia, especially in the elderly population: a long-term prospective cohort study. J Gastroenterol Hepatol. 2010;25:544-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 76. | Tian G, Wu C, Li J, Liang B, Zhang F, Fan X, Li Z, Wang Y, Liu D, Lai-Han Leung E, Chen J. Network pharmacology based investigation into the effect and mechanism of Modified Sijunzi Decoction against the subtypes of chronic atrophic gastritis. Pharmacol Res. 2019;144:158-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 77. | Yi Y, Hu Z, Li R, Chen L, Zhang H, Li H, Wu M, Liu W. Effectiveness of Banxia Xiexin Decoction in the treatment of precancerous lesions: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e25607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 78. | Garg A, Rodriguez A, Lewis JT, Bansal R, Brahmbhatt B. Energy Drinks: A Reversible Risk Factor for Atrophic Gastritis and Gastric Intestinal Metaplasia. Cureus. 2020;12:e12298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 79. | Tahara T, Shibata T, Horiguchi N, Kawamura T, Okubo M, Ishizuka T, Nagasaka M, Nakagawa Y, Ohmiya N. A Possible Link between Gastric Mucosal Atrophy and Gastric Cancer after Helicobacter pylori Eradication. PLoS One. 2016;11:e0163700. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 80. | Take S, Mizuno M, Ishiki K, Kusumoto C, Imada T, Hamada F, Yoshida T, Yokota K, Mitsuhashi T, Okada H. Risk of gastric cancer in the second decade of follow-up after Helicobacter pylori eradication. J Gastroenterol. 2020;55:281-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 81. | Yan LR, Lv Z, Jing JJ, Yuan Y, Xu Q. Single nucleotide polymorphisms of whole genes and atrophic gastritis susceptibility:a systematic review and meta-analysis. Gene. 2021;782:145543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 82. | Dargiene G, Streleckiene G, Skieceviciene J, Leja M, Link A, Wex T, Kupcinskas L, Malfertheiner P, Kupcinskas J. TLR1 and PRKAA1 Gene Polymorphisms in the Development of Atrophic Gastritis and Gastric Cancer. J Gastrointestin Liver Dis. 2018;27:363-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 83. | Liu S, Liu JW, Sun LP, Gong YH, Xu Q, Jing JJ, Yuan Y. Association of IL10 gene promoter polymorphisms with risks of gastric cancer and atrophic gastritis. J Int Med Res. 2018;46:5155-5166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 84. | Otsuka T, Tahara T, Nakamura M, Jing W, Ota M, Nomura T, Hayashi R, Shimasaki T, Shibata T, Arisawa T. Polymorphism rs7521584 in miR429 is associated with the severity of atrophic gastritis in patients with Helicobacter pylori infection. Mol Med Rep. 2018;18:2381-2386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 85. | Oda T, Murakami K, Nishizono A, Kodama M, Nasu M, Fujioka T. Long-term Helicobacter pylori infection in Japanese monkeys induces atrophic gastritis and accumulation of mutations in the p53 tumor suppressor gene. Helicobacter. 2002;7:143-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 86. | Arita S, Inagaki-Ohara K. High-fat-diet-induced modulations of leptin signaling and gastric microbiota drive precancerous lesions in the stomach. Nutrition. 2019;67-68:110556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 87. | Sayols S, Klassek J, Werner C, Möckel S, Ritz S, Mendez-Lago M, Soshnikova N. Signalling codes for the maintenance and lineage commitment of embryonic gastric epithelial progenitors. Development. 2020;147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 88. | Meyer AR, Goldenring JR. Injury, repair, inflammation and metaplasia in the stomach. J Physiol. 2018;596:3861-3867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 89. | Goldenring JR. Pyloric metaplasia, pseudopyloric metaplasia, ulcer-associated cell lineage and spasmolytic polypeptide-expressing metaplasia: reparative lineages in the gastrointestinal mucosa. J Pathol. 2018;245:132-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 90. | Wada Y, Kushima R, Kodama M, Fukuda M, Fukuda K, Okamoto K, Ogawa R, Mizukami K, Okimoto T, Murakami K. Histological changes associated with pyloric and pseudopyloric metaplasia after Helicobacter pylori eradication. Virchows Arch. 2020;477:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 91. | Wada Y, Nakajima S, Kushima R, Takemura S, Mori N, Hasegawa H, Nakayama T, Mukaisho KI, Yoshida A, Umano S, Yamamoto K, Sugihara H, Murakami K. Pyloric, pseudopyloric, and spasmolytic polypeptide-expressing metaplasias in autoimmune gastritis: a case series of 22 Japanese patients. Virchows Arch. 2021;479:169-178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 92. | Weis VG, Goldenring JR. Current understanding of SPEM and its standing in the preneoplastic process. Gastric Cancer. 2009;12:189-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 93. | Saenz JB, Burclaff J, Mills JC. Modeling Murine Gastric Metaplasia Through Tamoxifen-Induced Acute Parietal Cell Loss. Methods Mol Biol. 2016;1422:329-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 94. | Li Q, Karam SM, Gordon JI. Diphtheria toxin-mediated ablation of parietal cells in the stomach of transgenic mice. J Biol Chem. 1996;271:3671-3676. [PubMed] |
| 95. | Karam SM. Cell lineage relationship in the stomach of normal and genetically manipulated mice. Braz J Med Biol Res. 1998;31:271-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 96. | Nozaki K, Weis V, Wang TC, Falus A, Goldenring JR. Altered gastric chief cell lineage differentiation in histamine-deficient mice. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1211-G1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 97. | Sáenz JB, Mills JC. Acid and the basis for cellular plasticity and reprogramming in gastric repair and cancer. Nat Rev Gastroenterol Hepatol. 2018;15:257-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 97] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 98. | Weis VG, Petersen CP, Mills JC, Tuma PL, Whitehead RH, Goldenring JR. Establishment of novel in vitro mouse chief cell and SPEM cultures identifies MAL2 as a marker of metaplasia in the stomach. Am J Physiol Gastrointest Liver Physiol. 2014;307:G777-G792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 99. | Sáenz JB. Follow the Metaplasia: Characteristics and Oncogenic Implications of Metaplasia's Pattern of Spread Throughout the Stomach. Front Cell Dev Biol. 2021;9:741574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 100. | Teal E, Dua-Awereh M, Hirshorn ST, Zavros Y. Role of metaplasia during gastric regeneration. Am J Physiol Cell Physiol. 2020;319:C947-C954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 101. | Lee HW, Yang DH, Kim HK, Lee BH, Choi KC, Choi YH, Park YE. Expression of MUC2 in gastric carcinomas and background mucosae. J Gastroenterol Hepatol. 2007;22:1336-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 102. | Pyo JS, Sohn JH, Kang G, Kim DH, Kim K, Do IG. MUC2 Expression Is Correlated with Tumor Differentiation and Inhibits Tumor Invasion in Gastric Carcinomas: A Systematic Review and Meta-analysis. J Pathol Transl Med. 2015;49:249-256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 103. | Babu SD, Jayanthi V, Devaraj N, Reis CA, Devaraj H. Expression profile of mucins (MUC2, MUC5AC and MUC6) in Helicobacter pylori infected pre-neoplastic and neoplastic human gastric epithelium. Mol Cancer. 2006;5:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 104. | Hoffmann W. Trefoil Factor Family (TFF) Peptides and Their Links to Inflammation: A Re-evaluation and New Medical Perspectives. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (1)] |
| 105. | Hoffmann W. Trefoil Factor Family (TFF) Peptides and Their Diverse Molecular Functions in Mucus Barrier Protection and More: Changing the Paradigm. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 106. | Ge H, Gardner J, Wu X, Rulifson I, Wang J, Xiong Y, Ye J, Belouski E, Cao P, Tang J, Lee KJ, Coberly S, Gupte J, Miao L, Yang L, Nguyen N, Shan B, Yeh WC, Véniant MM, Li Y, Baribault H. Trefoil Factor 3 (TFF3) Is Regulated by Food Intake, Improves Glucose Tolerance and Induces Mucinous Metaplasia. PLoS One. 2015;10:e0126924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 107. | Huang Z, Zhang X, Lu H, Wu L, Wang D, Zhang Q, Ding H. Serum trefoil factor 3 is a promising non-invasive biomarker for gastric cancer screening: a monocentric cohort study in China. BMC Gastroenterol. 2014;14:74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 108. | Kaise M, Miwa J, Tashiro J, Ohmoto Y, Morimoto S, Kato M, Urashima M, Ikegami M, Tajiri H. The combination of serum trefoil factor 3 and pepsinogen testing is a valid non-endoscopic biomarker for predicting the presence of gastric cancer: a new marker for gastric cancer risk. J Gastroenterol. 2011;46:736-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 109. | Kaise M, Miwa J, Fujimoto A, Tashiro J, Tagami D, Sano H, Ohmoto Y. Influence of Helicobacter pylori status and eradication on the serum levels of trefoil factors and pepsinogen test: serum trefoil factor 3 is a stable biomarker. Gastric Cancer. 2013;16:329-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 110. | Xu CC, Yue L, Wei HJ, Zhao WW, Sui AH, Wang XM, Qiu WS. Significance of TFF3 protein and Her-2/neu status in patients with gastric adenocarcinoma. Pathol Res Pract. 2013;209:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 111. | Kang JM, Lee BH, Kim N, Lee HS, Lee HE, Park JH, Kim JS, Jung HC, Song IS. CDX1 and CDX2 expression in intestinal metaplasia, dysplasia and gastric cancer. J Korean Med Sci. 2011;26:647-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 112. | Grainger S, Hryniuk A, Lohnes D. Cdx1 and Cdx2 exhibit transcriptional specificity in the intestine. PLoS One. 2013;8:e54757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 113. | Almeida R, Silva E, Santos-Silva F, Silberg DG, Wang J, De Bolós C, David L. Expression of intestine-specific transcription factors, CDX1 and CDX2, in intestinal metaplasia and gastric carcinomas. J Pathol. 2003;199:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 210] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 114. | Rau TT, Rogler A, Frischauf M, Jung A, Konturek PC, Dimmler A, Faller G, Sehnert B, El-Rifai W, Hartmann A, Voll RE, Schneider-Stock R. Methylation-dependent activation of CDX1 through NF-κB: a link from inflammation to intestinal metaplasia in the human stomach. Am J Pathol. 2012;181:487-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 115. | Asano N, Imatani A, Watanabe T, Fushiya J, Kondo Y, Jin X, Ara N, Uno K, Iijima K, Koike T, Strober W, Shimosegawa T. Cdx2 Expression and Intestinal Metaplasia Induced by H. pylori Infection of Gastric Cells Is Regulated by NOD1-Mediated Innate Immune Responses. Cancer Res. 2016;76:1135-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 116. | Shin CM, Kim N, Chang H, Kim JS, Lee DH, Jung HC. Follow-Up Study on CDX1 and CDX2 mRNA Expression in Noncancerous Gastric Mucosae After Helicobacter pylori Eradication. Dig Dis Sci. 2016;61:1051-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 117. | Yu JH, Zheng JB, Qi J, Yang K, Wu YH, Wang K, Wang CB, Sun XJ. Bile acids promote gastric intestinal metaplasia by upregulating CDX2 and MUC2 expression via the FXR/NF-κB signalling pathway. Int J Oncol. 2019;54:879-892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 118. | Camilo V, Garrido M, Valente P, Ricardo S, Amaral AL, Barros R, Chaves P, Carneiro F, David L, Almeida R. Differentiation reprogramming in gastric intestinal metaplasia and dysplasia: role of SOX2 and CDX2. Histopathology. 2015;66:343-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 119. | Jonaitis P, Kupcinskas L, Kupcinskas J. Molecular Alterations in Gastric Intestinal Metaplasia. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 120. | Huang KK, Ramnarayanan K, Zhu F, Srivastava S, Xu C, Tan ALK, Lee M, Tay S, Das K, Xing M, Fatehullah A, Alkaff SMF, Lim TKH, Lee J, Ho KY, Rozen SG, Teh BT, Barker N, Chia CK, Khor C, Ooi CJ, Fock KM, So J, Lim WC, Ling KL, Ang TL, Wong A, Rao J, Rajnakova A, Lim LG, Yap WM, Teh M, Yeoh KG, Tan P. Genomic and Epigenomic Profiling of High-Risk Intestinal Metaplasia Reveals Molecular Determinants of Progression to Gastric Cancer. Cancer Cell. 2018;33:137-150.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 182] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 121. | Sugimoto R, Habano W, Yanagawa N, Akasaka R, Toya Y, Sasaki A, Matsumoto T, Sugai T. Molecular alterations in gastric cancer and the surrounding intestinal metaplastic mucosa: an analysis of isolated glands. Gastric Cancer. 2021;24:382-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 122. | Nieuwenburg SAV, Mommersteeg MC, Eikenboom EL, Yu B, den Hollander WJ, Holster IL, den Hoed CM, Capelle LG, Tang TJ, Anten MP, Prytz-Berset I, Witteman EM, Ter Borg F, Burger JPW, Bruno MJ, Fuhler GM, Peppelenbosch MP, Doukas M, Kuipers EJ, Spaander MCW. Factors associated with the progression of gastric intestinal metaplasia: a multicenter, prospective cohort study. Endosc Int Open. 2021;9:E297-E305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 123. | Mills JC, Goldenring JR. Metaplasia in the Stomach Arises From Gastric Chief Cells. Cell Mol Gastroenterol Hepatol. 2017;4:85-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 124. | Hayakawa Y, Fox JG, Wang TC. Isthmus Stem Cells Are the Origins of Metaplasia in the Gastric Corpus. Cell Mol Gastroenterol Hepatol. 2017;4:89-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 125. | Yoshizawa N, Takenaka Y, Yamaguchi H, Tetsuya T, Tanaka H, Tatematsu M, Nomura S, Goldenring JR, Kaminishi M. Emergence of spasmolytic polypeptide-expressing metaplasia in Mongolian gerbils infected with Helicobacter pylori. Lab Invest. 2007;87:1265-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 126. | Can N, Oz Puyan F, Altaner S, Ozyilmaz F, Tokuc B, Pehlivanoglu Z, Kutlu KA. Mucins, trefoil factors and pancreatic duodenal homeobox 1 expression in spasmolytic polypeptide expressing metaplasia and intestinal metaplasia adjacent to gastric carcinomas. Arch Med Sci. 2020;16:1402-1410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 127. | Kinoshita H, Hayakawa Y, Niu Z, Konishi M, Hata M, Tsuboi M, Hayata Y, Hikiba Y, Ihara S, Nakagawa H, Hirata Y, Wang TC, Koike K. Mature gastric chief cells are not required for the development of metaplasia. Am J Physiol Gastrointest Liver Physiol. 2018;314:G583-G596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 128. | Correa P, Piazuelo MB, Wilson KT. Pathology of gastric intestinal metaplasia: clinical implications. Am J Gastroenterol. 2010;105:493-498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 290] [Cited by in RCA: 286] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 129. | Gawron AJ, Shah SC, Altayar O, Davitkov P, Morgan D, Turner K, Mustafa RA. AGA Technical Review on Gastric Intestinal Metaplasia-Natural History and Clinical Outcomes. Gastroenterology. 2020;158:705-731.e5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 130. | Li D, Bautista MC, Jiang SF, Daryani P, Brackett M, Armstrong MA, Hung YY, Postlethwaite D, Ladabaum U. Risks and Predictors of Gastric Adenocarcinoma in Patients with Gastric Intestinal Metaplasia and Dysplasia: A Population-Based Study. Am J Gastroenterol. 2016;111:1104-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 131. | den Hoed CM, Holster IL, Capelle LG, de Vries AC, den Hartog B, Ter Borg F, Biermann K, Kuipers EJ. Follow-up of premalignant lesions in patients at risk for progression to gastric cancer. Endoscopy. 2013;45:249-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 132. | Banks M, Graham D, Jansen M, Gotoda T, Coda S, di Pietro M, Uedo N, Bhandari P, Pritchard DM, Kuipers EJ, Rodriguez-Justo M, Novelli MR, Ragunath K, Shepherd N, Dinis-Ribeiro M. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;68:1545-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 425] [Cited by in RCA: 405] [Article Influence: 67.5] [Reference Citation Analysis (1)] |
| 133. | Xu M, Zhou W, Wu L, Zhang J, Wang J, Mu G, Huang X, Li Y, Yuan J, Zeng Z, Wang Y, Huang L, Liu J, Yu H. Artificial intelligence in the diagnosis of gastric precancerous conditions by image-enhanced endoscopy: a multicenter, diagnostic study (with video). Gastrointest Endosc. 2021;94:540-548.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 134. | Yan T, Wong PK, Choi IC, Vong CM, Yu HH. Intelligent diagnosis of gastric intestinal metaplasia based on convolutional neural network and limited number of endoscopic images. Comput Biol Med. 2020;126:104026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 135. | Yang HB, Cheng HC, Sheu BS, Hung KH, Liou MF, Wu JJ. Chronic celecoxib users more often show regression of gastric intestinal metaplasia after Helicobacter pylori eradication. Aliment Pharmacol Ther. 2007;25:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 136. | Lu W, Ni Z, Jiang S, Tong M, Zhang J, Zhao J, Feng C, Jia Q, Wang J, Yao T, Ning H, Shi Y. Resveratrol inhibits bile acid-induced gastric intestinal metaplasia via the PI3K/AKT/p-FoxO4 signalling pathway. Phytother Res. 2021;35:1495-1507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 137. | Forté E, Petit B, Walter T, Lépilliez V, Vanbiervliet G, Rostain F, Barsic N, Albeniz E, Gete GG, Gabriel JCM, Cuadrado-Tiemblo C, Ratone JP, Jacques J, Wallenhorst T, Subtil F, Albouys J, Giovannini M, Chaussade S, Landel V, Ponchon T, Saurin JC, Barret M, Pioche M. Risk of neoplastic change in large gastric hyperplastic polyps and recurrence after endoscopic resection. Endoscopy. 2020;52:444-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 138. | Choi E, Means AL, Coffey RJ, Goldenring JR. Active Kras Expression in Gastric Isthmal Progenitor Cells Induces Foveolar Hyperplasia but Not Metaplasia. Cell Mol Gastroenterol Hepatol. 2019;7:251-253.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 139. | Carmack SW, Genta RM, Graham DY, Lauwers GY. Management of gastric polyps: a pathology-based guide for gastroenterologists. Nat Rev Gastroenterol Hepatol. 2009;6:331-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (1)] |
| 140. | Markowski AR, Markowska A, Guzinska-Ustymowicz K. Pathophysiological and clinical aspects of gastric hyperplastic polyps. World J Gastroenterol. 2016;22:8883-8891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (3)] |
| 141. | Castro R, Pimentel-Nunes P, Dinis-Ribeiro M. Evaluation and management of gastric epithelial polyps. Best Pract Res Clin Gastroenterol. 2017;31:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 142. | Goddard AF, Badreldin R, Pritchard DM, Walker MM, Warren B; British Society of Gastroenterology. The management of gastric polyps. Gut. 2010;59:1270-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 143. | Jain R, Chetty R. Gastric hyperplastic polyps: a review. Dig Dis Sci. 2009;54:1839-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 144. | Shaib YH, Rugge M, Graham DY, Genta RM. Management of gastric polyps: an endoscopy-based approach. Clin Gastroenterol Hepatol. 2013;11:1374-1384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 145. | Ouyang Y, Zhang W, Huang Y, Wang Y, Shao Q, Wu X, Lu N, Xie C. Effect of Helicobacter pylori eradication on hyperplastic gastric polyps: A systematic review and meta-analysis. Helicobacter. 2021;26:e12838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 146. | Obayashi Y, Kawano S, Sakae H, Abe M, Kono Y, Kanzaki H, Iwamuro M, Kawahara Y, Tanaka T, Yanai H, Okada H. Risk Factors for Gastric Cancer after the Eradication of Helicobacter pylori Evaluated Based on the Background Gastric Mucosa: A Propensity Score-matched Case-control Study. Intern Med. 2021;60:969-976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 147. | Kudo Y, Morohashi S, Takasugi K, Tsutsumi S, Ogasawara H, Hanabata N, Yoshimura T, Sato F, Fukuda S, Kijima H. Histopathological phenotypes of early gastric cancer and its background mucosa. Biomed Res. 2011;32:127-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 148. | Ohkusa T, Takashimizu I, Fujiki K, Suzuki S, Shimoi K, Horiuchi T, Sakurazawa T, Ariake K, Ishii K, Kumagai J, Tanizawa T. Disappearance of hyperplastic polyps in the stomach after eradication of Helicobacter pylori. A randomized, clinical trial. Ann Intern Med. 1998;129:712-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 86] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 149. | Bradai S, Khsiba A, Mahmoudi M, Ben Mohamed A, Medhioub M, Hamzaoui L, Azzouz MM. Hyperplastic Gastric Polyps: About 74 Cases. 2021. |