Published online May 15, 2021. doi: 10.4251/wjgo.v13.i5.453
Peer-review started: November 27, 2020
First decision: February 14, 2021
Revised: February 22, 2021
Accepted: April 13, 2021
Article in press: April 13, 2021
Published online: May 15, 2021
Processing time: 160 Days and 9.9 Hours
The results of previous meta-analyses evaluating the association between the alcohol intake and gastric cancer risk have reported that a statistical significance only for men.
To investigate the different association between alcohol intake and gastric cancer risk between men and women.
The selection criteria included a prospective cohort study for evaluating alcohol intake and gastric cancer risk, with relative risks adjusted for potential confounders. Adjusted relative risk (RR) for the potential confounders and its 95% confidence interval (CI) in the highest vs lowest level were extracted from each study and a random-effects meta-analysis was conducted. Subgroup analyses by region, level of adjustment for smoking status, adjusting for body mass index, and year of publication were conducted.
A meta-analysis of all 27 cohorts showed that alcohol intake increased the risk of gastric cancer (summary RR = 1.13, 95%CI: 1.04-1.23, I2 = 58.2%). Further, 13 men’s cohorts had higher summary RR while maintaining statistical significance, and only seven women’s cohorts had no statistical significance.
The present review suggests that alcohol consumption increases the risk of gastric cancer in men. These findings showed that the sex variable in the association between alcohol intake and gastric cancer risk seemed to be an effect modifier with an interaction term. It is necessary to re-estimate follow-up outcomes after stratifying for sex.
Core Tip: The present review suggests that alcohol consumption increases the risk of gastric cancer, especially in men. These findings showed that the sex variable in the association between alcohol intake and gastric cancer risk seemed to be an effect modifier with an interaction term. It is necessary to re-estimate follow-up outcomes after stratifying for sex.
- Citation: Bae JM. Sex as an effect modifier in the association between alcohol intake and gastric cancer risk. World J Gastrointest Oncol 2021; 13(5): 453-461
- URL: https://www.wjgnet.com/1948-5204/full/v13/i5/453.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v13.i5.453
Global cancer statistics 2018 reported that gastric cancer was the fifth most frequently diagnosed cancer and the third leading cause of cancer-related death[1]. As gastric cancer is known to be a multifactorial disease[2], modifiable risk factors such as Helicobacter pylori and Epstein–Barr virus infection, diet, smoking status, and alcohol intake have been identified[3-6].
Table 1 summarizes the results of three meta-analyses published in 2017, that evaluated the association between alcohol intake and gastric cancer risk[7-9]. All summary relative risk (sRR) was over 1, but the results of statistical significance conflicted with each other. Interestingly, all meta-analyses reported that the 95% confidence interval (CI) of sRR in men did not involve 1. This indicates a statistically significant association between alcohol intake and gastric cancer risk in men. However, women did not have statistical significance in any of the meta-analyses. In addition, He et al[8] reported that light alcohol intake was associated with a reduction in gastric cancer in women (sRR = 0.74, 95%CI: 0.57-0.98).
| Ref. | Searching | Selected studies (Cohort) | Group | Summary relative risk (95% confidence interval) | I2 (%) |
| Han et al[7], 2017 | Dec-16 | 23 | Both, HLL | 1.17 (1.00-1.34) | 79.6 |
| 7 | Men, HLL | 1.18 (1.06-1.30) | 0 | ||
| 1 | Women, HLL | 1.13 (0.79-2.25) | 0 | ||
| Wang et al[9], 2017 | Dec-16 | 17 | Both, HLL | 1.19 (1.06-1.34) | 37.6 |
| 34 | Men, HLL | 1.21 (1.06-1.37) | 68.2 | ||
| 12 | Women, HLL | 1.18 (0.95-1.47) | 26.2 | ||
| He et al[8], 2017 | Apr-17 | 22 | Both, HLL | 1.03 (0.99-1.08) | 21.9 |
| Men, heavy | 1.13 (1.06-1.22) | 28.1 | |||
| Women, heavy | 1.33 (0.79-2.24) | 2.4 |
Based on these findings, the author hypothesized that alcohol intake’s association with gastric cancer risk may differ between men and women. Thus, the aim was to investigate the suggested hypothesis targeting three meta-analyses in Table 1 and Tramacere et al[10]’s study by performing a meta-epidemiological review[11].
The selection criterion for this meta-epidemiological study was as follows: A prospective cohort study for evaluating alcohol intake and gastric cancer risk showing RR adjusted for potential confounders.
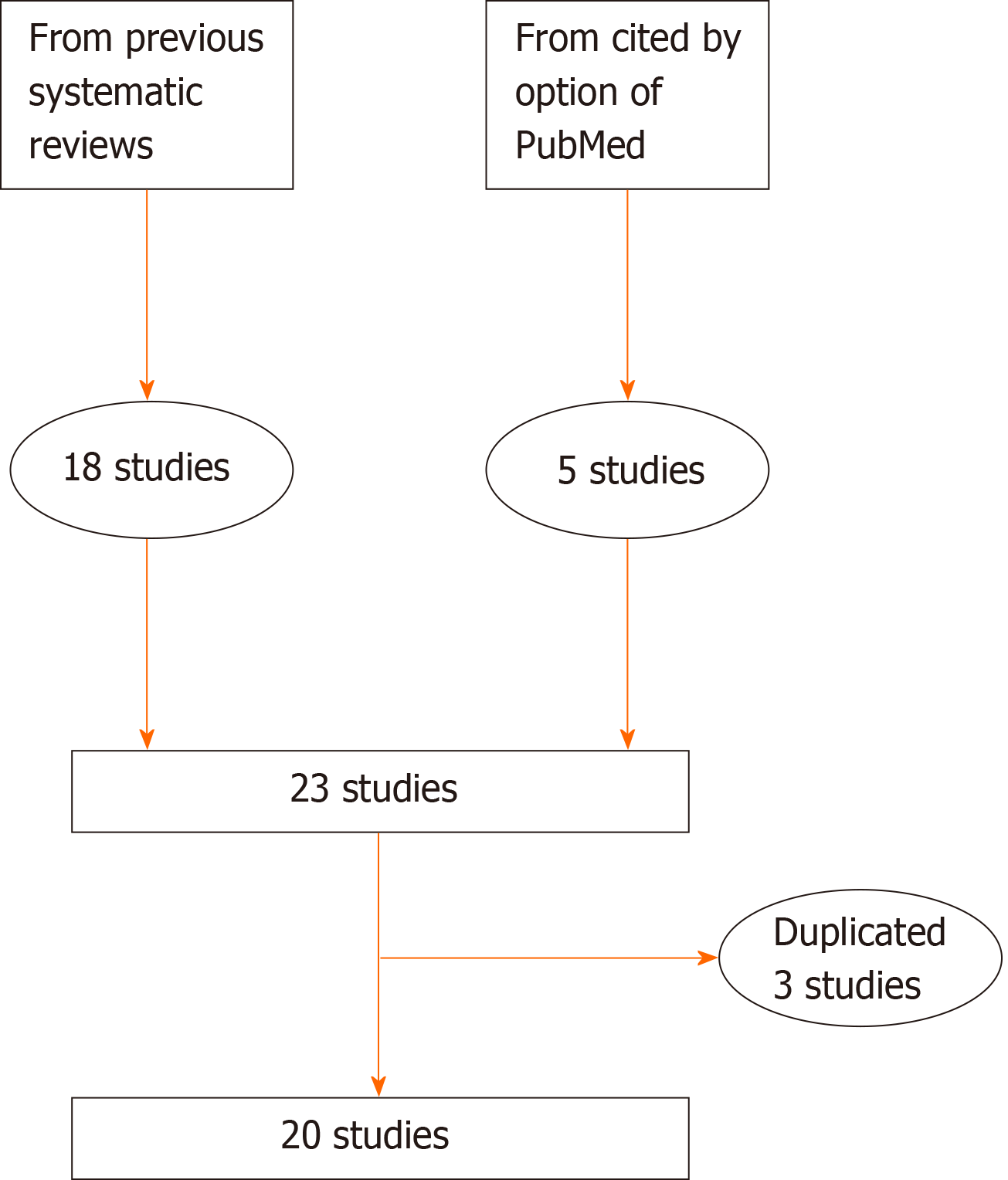
Of the cohort studies selected for conducting meta-analysis by four existing systematic reviews[7-10], a total of 18 studies met the selection criteria[12-29]. Since the latest year of publication, of the 18 studies, was 2015[29], cohort studies published until July 31, 2020 were needed. The articles that cited the 18 selected studies was listed using the “cited by” option on PubMed[30]. From this, additional cohort studies meeting the selection criteria were secured. After checking for duplication of cohort participants among the selected cohort studies, a study with more gastric cancer patients was selected between duplicate studies.
Adjusted RR for potential confounders and its 95%CI in the highest vs lowest level were extracted by sex from each study. As the reference group of Buckland et al[27] was the moderate/high-intake group, the adjusted RR of the study was taken by the reciprocal of the adjusted RR of the no/low-intake group. The level of adjustment for smoking status and the adjustment for body mass index in each cohort study were evaluated. A high level of smoking status was defined as ≥ 3 in the definition suggested by Thomas and Hodges[31]. They defined three levels as adjustments with less than four categories based on smoking status and intensity.
The level of heterogeneity among cohorts was evaluated using the I-squared value, and a random-effects model meta-analysis was performed[32]. In addition, subgroup analyses by region, level of adjustment for smoking status, adjusting for body mass index, and year of publication were conducted to evaluate the effects of potential confounders. The level of statistical significance was set at P < 0.05.
The list made using the “cited by” option on PubMed on July 31, 2020 contained a total of 411 articles. Five cohort studies meeting the selection criteria were obtained from the list[33-37]. While checking for duplication of cohort participants, the author found that three studies of the Honolulu Heart Program[12,15], two of the European Prospective Investigation into Cancer and Nutrition cohort[13,27], and two of the NIH-AARP diet and health cohort[14,36] had the same cohort participants, respectively. Thus Nomura et al[12], Duell et al[13], and Freedman et al[14] were excluded based on the number of gastric cancer patients. Finally, 20 cohort studies with a total of 26864280 participants were selected (Figure 1)[15-29,33-37]. There were 10 Asian, 7 European, and 3 American studies in the regional distribution. They consisted of 27 cohorts by sex: 13 men’s, 7 women’s, and 7 adjusted for sex.
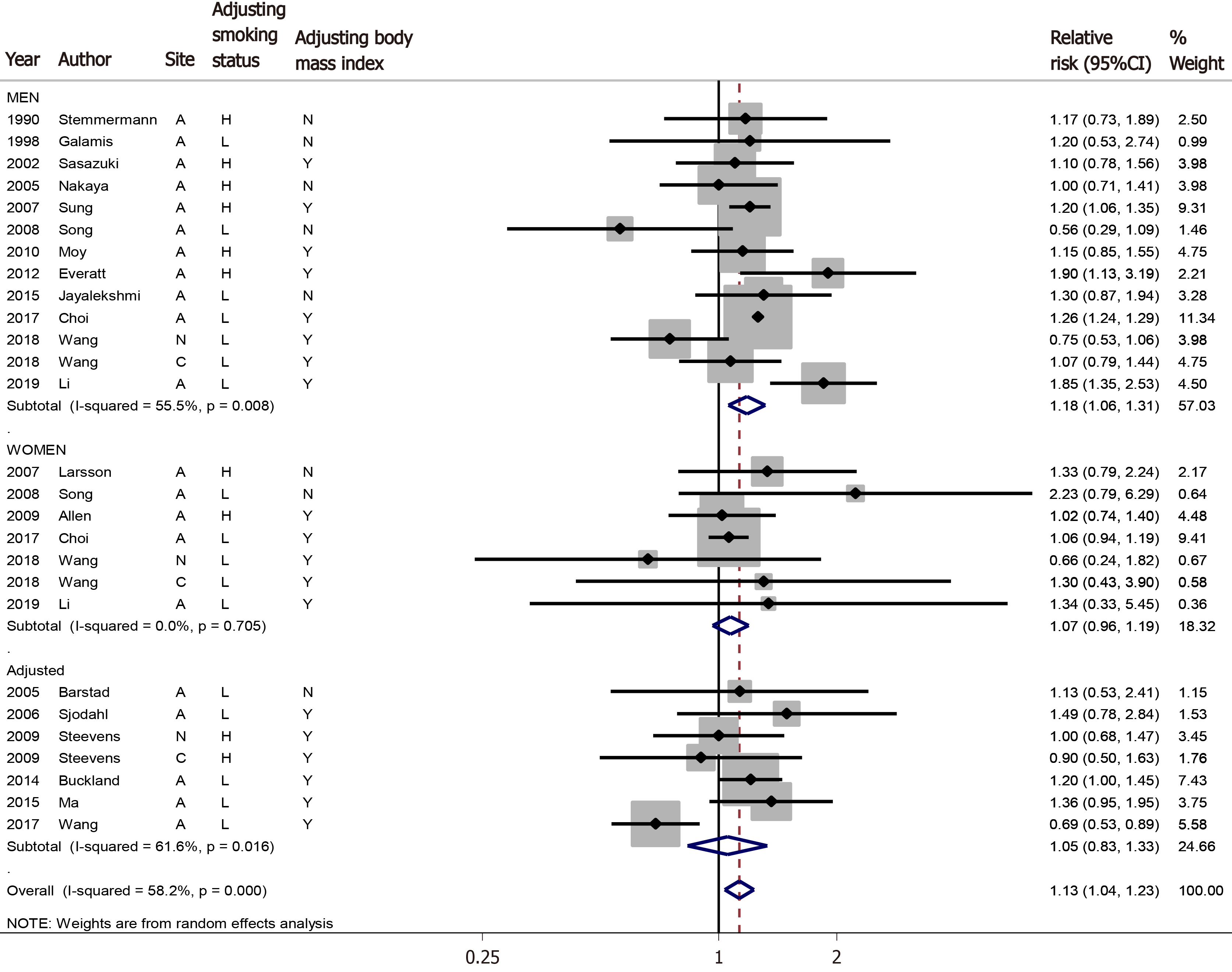
A meta-analysis of all 27 cohorts showed that alcohol intake increased the risk of gastric cancer (sRR = 1.13, 95%CI: 1.04-1.23, I2= 58.2%) (Figure 2). When subgroup analysis by sex was performed, the 13 men’s cohorts had higher sRR while maintaining statistical significance (sRR = 1.18, 95%CI: 1.06-1.32, I2= 55.5%), but the seven women’s cohorts (sRR = 1.07, 95%CI: 0.96-1.19, I2= 0.0%) and seven cohorts adjusted for sex (sRR = 1.05, 95%CI: 0.83-1.33, I2= 61.6%) had no statistical significance.
The subgroup analysis of the 13 men’s cohorts showed that there was statistical significance in Asians, in the group with a high level of adjustment for smoking status, in the group with the adjustment for body mass index, and in more recently published studies (Table 2). These results were not found in the seven women’s cohorts.
| Men | Women | Both | ||
| All | 1.18 (1.06-1.32) [13] | 1.07 (0.95-1.19) [7] | 1.13 (1.04-1.23) [27] | |
| Region | ||||
| Asia | 1.22 (1.09-1.36) [8] | 1.09 (0.91-1.29) [3] | 1.43 (1.02-1.28) [13] | |
| Non-Asia | 1.12 (0.83-1.50) [5] | 1.07 (0.83-1.38) [4] | 1.11 (0.99-1.24) [14] | |
| Level of adjustment of smoking status | ||||
| Low | 1.14 (0.91-1.41) [7] | 1.07 (0.95-1.20) [5] | 1.16 (1.06-1.27) [10] | |
| High | 1.19 (1.08-1.31) [6] | 1.09 (0.84-1.43) [2] | 1.12 (0.98-1.27) [17] | |
| Adjustment of body mass index | ||||
| No | 1.05 (0.83-1.34) [5] | 1.48 (0.93-2.36) [2] | 1.12 (0.92-1.36) [8] | |
| Yes | 1.22 (1.08-1.37) [8] | 1.05 (0.96-1.17) [5] | 1.13 (1.03-1.24) [19] | |
| Year of publication | ||||
| Approximately 2005 | 1.08 (0.88-1.33) [4] | [0] | 1.08 (0.89-1.33) [5] | |
| 2006-2010 | 1.07 (0.81-1.41) [3] | 1.48 (0.93-2.36) [2] | 1.14 (0.98-1.32) [8] | |
| 2011- | 1.26 (1.02-1.56) [6] | 1.05 (0.95-1.17) [5] | 1.14 (1.00-1.29) [14] | |
| Site | ||||
| Cardia | 1.07 (0.79-1.44) [1] | 1.30 (0.43-3.90) [1] | 1.05 (0.81-1.35) [3] | |
| Non-cardia | 0.75 (0.53-1.06) [1] | 0.66 (0.24-1.82) [1] | 0.84 (0.65-1.08) [3] | |
The results show that alcohol intake increased the risk of gastric cancer, especially in men. However, this association was not seen in women.
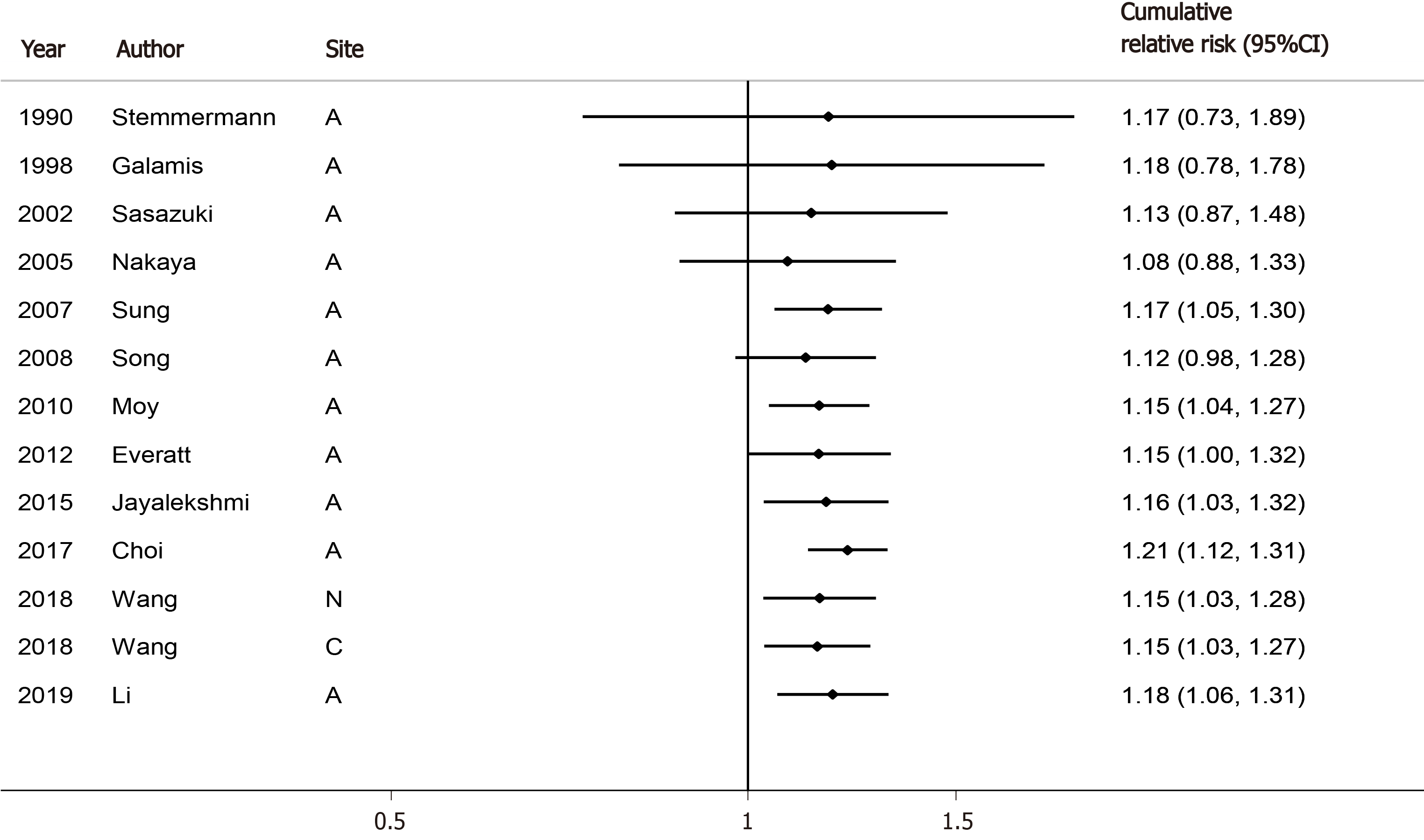
Compared to the sRR of 1.21 in men’s cohorts of Wang et al[9] in Table 1, the sRR of 1.13 estimated from 13 cohorts was the almost the same level, but the CI was narrower. The sRR of men’s cohorts published more recently was the highest and was statistically significant. Cumulative meta-analysis showed that the sRR converged as it moved from the past to the present (Figure 3).
However, the results of the women’s cohorts showed that alcohol intake might not increase the risk of gastric cancer. This finding can be supported by the results of He et al[8], who reported that light alcohol intake was associated with a reduction in gastric cancer in women (sRR = 0.74, 95%CI: 0.57-0.98). In addition, incidence rates are two-fold higher in men than in women[1]. Thus, the sex variable in the association between alcohol intake and gastric cancer risk seems not to be a simple confounder but be an effect modifier having an interaction term[38]. In other words, seven cohorts adjusted for sex need to re-estimate outcomes stratified by sex.
The subgroup analysis of 13 men’s cohorts indicated that there was statistical significance in Asians, in the group with the high level of adjustment for smoking status, and in the group adjusted for body mass index. Interestingly, the statistical significance was not shown in the group with a low level of adjustment for smoking status, and in the group not adjusted for body mass index. This is because a RR generally shifts to null as the potential confounder is strengthened. These phenomena strongly support the hypothesis that alcohol intake increases the risk of gastric cancer in men.
The main limitation is that the category of alcohol intake varies in each study, such as times per week, amount consumed per day, none/moderate/heavy, or never/ former/current drinker. Therefore, the author extracted the results of the highest and lowest levels from each study and applied a random effect model. Another limitation is that the author could not perform subgroup analysis for cardia and non-cardia because only three cohorts were selected. Thus, the author could not evaluate the argument by sex that “intestinal non-cardia carcinoma was accompanied by heavy alcohol consumption”[3].
In conclusion, the present study suggests that alcohol consumption increases the risk of gastric cancer in men. It is necessary to re-estimate the follow-up outcomes by stratification for sex to determine whether there is a sex difference in the association between alcohol intake and gastric cancer risk.
The previous systematic reviews showed a statistically significant association between alcohol intake and gastric cancer risk in men. However, women did not have statistical significance in any of the meta-analyses.
The author hypothesized that alcohol intake’s association with gastric cancer risk may differ between men and women.
The aim was to investigate the suggested hypothesis targeting four previous meta-analyses by performing a meta-epidemiological review.
After securing additional cohort studies meeting the selection criteria, updated meta-analysis and subgroup analysis by sex were conducted.
The subgroup analysis of the 13 men’s cohorts showed that there was statistical significance in Asians, in the group with a high level of adjustment for smoking status, in the group with the adjustment for body mass index, and in more recently published studies. These results were not found in the seven women’s cohorts.
The present study suggests that alcohol consumption increases the risk of gastric cancer in men.
It is necessary to re-estimate the follow-up outcomes by stratification for sex to determine whether there is a sex difference in the association between alcohol intake and gastric cancer risk.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yu PF S-Editor: Fan JR L-Editor: A P-Editor: Li JH
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55742] [Article Influence: 7963.1] [Reference Citation Analysis (132)] |
| 2. |
Yusefi AR, Bagheri Lankarani K, Bastani P, Radinmanesh M, Kavosi Z.
Risk Factors for Gastric Cancer: A Systematic Review |
| 3. | Machlowska J, Baj J, Sitarz M, Maciejewski R, Sitarz R. Gastric Cancer: Epidemiology, Risk Factors, Classification, Genomic Characteristics and Treatment Strategies. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 897] [Cited by in RCA: 846] [Article Influence: 169.2] [Reference Citation Analysis (0)] |
| 4. | Wang C, Yuan Y, Hunt RH. The association between Helicobacter pylori infection and early gastric cancer: a meta-analysis. Am J Gastroenterol. 2007;102:1789-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Bae JM, Kim EH. Epstein-Barr Virus and Gastric Cancer Risk: A Meta-analysis With Meta-regression of Case-control Studies. J Prev Med Public Health. 2016;49:97-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Bae JM, Kim EH. Dietary intakes of citrus fruit and risk of gastric cancer incidence: an adaptive meta-analysis of cohort studies. Epidemiol Health. 2016;38:e2016034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Han X, Xiao L, Yu Y, Chen Y, Shu HH. Alcohol consumption and gastric cancer risk: a meta-analysis of prospective cohort studies. Oncotarget. 2017;8:83237-83245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | He Z, Zhao TT, Xu HM, Wang ZN, Xu YY, Song YX, Ni ZR, Xu H, Yin SC, Liu XY, Miao ZF. Association between alcohol consumption and the risk of gastric cancer: a meta-analysis of prospective cohort studies. Oncotarget. 2017;8:84459-84472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Wang PL, Xiao FT, Gong BC, Liu FN. Alcohol drinking and gastric cancer risk: a meta-analysis of observational studies. Oncotarget. 2017;8:99013-99023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Tramacere I, Negri E, Pelucchi C, Bagnardi V, Rota M, Scotti L, Islami F, Corrao G, La Vecchia C, Boffetta P. A meta-analysis on alcohol drinking and gastric cancer risk. Ann Oncol. 2012;23:28-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 215] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 11. | Murad MH, Wang Z. Guidelines for reporting meta-epidemiological methodology research. Evid Based Med. 2017;22:139-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 301] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 12. | Nomura A, Grove JS, Stemmermann GN, Severson RK. A prospective study of stomach cancer and its relation to diet, cigarettes, and alcohol consumption. Cancer Res. 1990;50:627-631. [PubMed] |
| 13. | Duell EJ, Travier N, Lujan-Barroso L, Clavel-Chapelon F, Boutron-Ruault MC, Morois S, Palli D, Krogh V, Panico S, Tumino R, Sacerdote C, Quirós JR, Sánchez-Cantalejo E, Navarro C, Gurrea AB, Dorronsoro M, Khaw KT, Allen NE, Key TJ, Bueno-de-Mesquita HB, Ros MM, Numans ME, Peeters PH, Trichopoulou A, Naska A, Dilis V, Teucher B, Kaaks R, Boeing H, Schütze M, Regner S, Lindkvist B, Johansson I, Hallmans G, Overvad K, Egeberg R, Tjønneland A, Lund E, Weiderpass E, Braaten T, Romieu I, Ferrari P, Jenab M, Stenling R, Aune D, Norat T, Riboli E, González CA. Alcohol consumption and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Am J Clin Nutr. 2011;94:1266-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Freedman ND, Abnet CC, Leitzmann MF, Mouw T, Subar AF, Hollenbeck AR, Schatzkin A. A prospective study of tobacco, alcohol, and the risk of esophageal and gastric cancer subtypes. Am J Epidemiol. 2007;165:1424-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 269] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 15. | Stemmermann GN, Nomura AM, Chyou PH, Yoshizawa C. Prospective study of alcohol intake and large bowel cancer. Dig Dis Sci. 1990;35:1414-1420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Galanis DJ, Kolonel LN, Lee J, Nomura A. Intakes of selected foods and beverages and the incidence of gastric cancer among the Japanese residents of Hawaii: a prospective study. Int J Epidemiol. 1998;27:173-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 131] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Sasazuki S, Sasaki S, Tsugane S; Japan Public Health Center Study Group. Cigarette smoking, alcohol consumption and subsequent gastric cancer risk by subsite and histologic type. Int J Cancer. 2002;101:560-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 118] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Barstad B, Sørensen TI, Tjønneland A, Johansen D, Becker U, Andersen IB, Grønbaek M. Intake of wine, beer and spirits and risk of gastric cancer. Eur J Cancer Prev. 2005;14:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Nakaya N, Tsubono Y, Kuriyama S, Hozawa A, Shimazu T, Kurashima K, Fukudo S, Shibuya D, Tsuji I. Alcohol consumption and the risk of cancer in Japanese men: the Miyagi cohort study. Eur J Cancer Prev. 2005;14:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Sjödahl K, Lu Y, Nilsen TI, Ye W, Hveem K, Vatten L, Lagergren J. Smoking and alcohol drinking in relation to risk of gastric cancer: a population-based, prospective cohort study. Int J Cancer. 2007;120:128-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Larsson SC, Giovannucci E, Wolk A. Alcoholic beverage consumption and gastric cancer risk: a prospective population-based study in women. Int J Cancer. 2007;120:373-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Sung NY, Choi KS, Park EC, Park K, Lee SY, Lee AK, Choi IJ, Jung KW, Won YJ, Shin HR. Smoking, alcohol and gastric cancer risk in Korean men: the National Health Insurance Corporation Study. Br J Cancer. 2007;97:700-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Song HJ, Kim HJ, Choi NK, Hahn S, Cho YJ, Park BJ. Gender differences in gastric cancer incidence in elderly former drinkers. Alcohol. 2008;42:363-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Steevens J, Schouten LJ, Goldbohm RA, van den Brandt PA. Alcohol consumption, cigarette smoking and risk of subtypes of oesophageal and gastric cancer: a prospective cohort study. Gut. 2010;59:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 171] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 25. | Moy KA, Fan Y, Wang R, Gao YT, Yu MC, Yuan JM. Alcohol and tobacco use in relation to gastric cancer: a prospective study of men in Shanghai, China. Cancer Epidemiol Biomarkers Prev. 2010;19:2287-2297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 26. | Everatt R, Tamosiunas A, Kuzmickiene I, Virviciute D, Radisauskas R, Reklaitiene R, Milinaviciene E. Alcohol consumption and risk of gastric cancer: a cohort study of men in Kaunas, Lithuania, with up to 30 years follow-up. BMC Cancer. 2012;12:475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Buckland G, Travier N, Huerta JM, Bueno-de-Mesquita HB, Siersema PD, Skeie G, Weiderpass E, Engeset D, Ericson U, Ohlsson B, Agudo A, Romieu I, Ferrari P, Freisling H, Colorado-Yohar S, Li K, Kaaks R, Pala V, Cross AJ, Riboli E, Trichopoulou A, Lagiou P, Bamia C, Boutron-Ruault MC, Fagherazzi G, Dartois L, May AM, Peeters PH, Panico S, Johansson M, Wallner B, Palli D, Key TJ, Khaw KT, Ardanaz E, Overvad K, Tjønneland A, Dorronsoro M, Sánchez MJ, Quirós JR, Naccarati A, Tumino R, Boeing H, Gonzalez CA. Healthy lifestyle index and risk of gastric adenocarcinoma in the EPIC cohort study. Int J Cancer. 2015;137:598-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 28. | Jayalekshmi PA, Hassani S, Nandakumar A, Koriyama C, Sebastian P, Akiba S. Gastric cancer risk in relation to tobacco use and alcohol drinking in Kerala, India--Karunagappally cohort study. World J Gastroenterol. 2015;21:12676-12685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Ma SH, Jung W, Weiderpass E, Jang J, Hwang Y, Ahn C, Ko KP, Chang SH, Shin HR, Yoo KY, Park SK. Impact of alcohol drinking on gastric cancer development according to Helicobacter pylori infection status. Br J Cancer. 2015;113:1381-1388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 30. | Bae JM, Kim EH. Citation Discovery Tools for Conducting Adaptive Meta-analyses to Update Systematic Reviews. J Prev Med Public Health. 2016;49:129-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Thomas DR, Hodges ID. Dietary Research on Coffee: Improving Adjustment for Confounding. Curr Dev Nutr. 2020;4:nzz142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. metan: Fixed- and random-effects meta-analysis. Stata J. 2008;8:3-28. [DOI] [Full Text] |
| 33. | Allen NE, Beral V, Casabonne D, Kan SW, Reeves GK, Brown A, Green J; Million Women Study Collaborators. Moderate alcohol intake and cancer incidence in women. J Natl Cancer Inst. 2009;101:296-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 409] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 34. | Choi YJ, Lee DH, Han KD, Kim HS, Yoon H, Shin CM, Park YS, Kim N. The relationship between drinking alcohol and esophageal, gastric or colorectal cancer: A nationwide population-based cohort study of South Korea. PLoS One. 2017;12:e0185778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 35. | Wang Z, Koh WP, Jin A, Wang R, Yuan JM. Composite protective lifestyle factors and risk of developing gastric adenocarcinoma: the Singapore Chinese Health Study. Br J Cancer. 2017;116:679-687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 36. | Wang S, Freedman ND, Loftfield E, Hua X, Abnet CC. Alcohol consumption and risk of gastric cardia adenocarcinoma and gastric noncardia adenocarcinoma: A 16-year prospective analysis from the NIH-AARP diet and health cohort. Int J Cancer. 2018;143:2749-2757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 37. | Li Y, Eshak ES, Shirai K, Liu K, Dong JY, Iso H, Tamakoshi A; JACC Study Group. Alcohol Consumption and Risk of Gastric Cancer: The Japan Collaborative Cohort Study. J Epidemiol. 2021;31:30-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 38. | Deandrea S, Foschi R, Galeone C, La Vecchia C, Negri E, Hu J. Is temperature an effect modifier of the association between green tea intake and gastric cancer risk? Eur J Cancer Prev. 2010;19:18-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |